Recruitment and Retention in DSMES Rural Healthcare Rules



- Slides: 39
Recruitment and Retention in DSMES Rural Healthcare Rules Kristine Kilen, RD, CDE Diabetes Educator and Program Coordinator Billings Clinic Miles City ~ Miles City, MT
Objectives • Identify and address barriers to engaging patients in DSMES • Implement strategies that support rural providers and programs in reaching and teaching DSMES • Engage in use of tools to support growing DSMES programs
I know where I want to go…. . And, it looks like I can get there.
Benefits associated with DSMES: • Improved health outcomes – Reduced A 1 c by as much as. 88% – Reduced onset and/or advancement of complications – Reduced hospital admissions and readmissions • More healthful eating patterns and regular activity • Enhanced self-efficacy and empowerment, increased healthy coping, and improved quality of life Powers MA et al. DSME/S Position Statement 2015 Diabetes Care, The Diabetes Educator, Journal of Academy of Nutrition and Dietetics
Benefits associated with DSMES: NOTE: 1) Benefits of education decrease over time 2) Sustained improvement requires time and follow-up 3) Effectiveness directly correlated to amount of time spent with educator Powers MA et al. DSME/S Position Statement 2015 Diabetes Care, The Diabetes Educator, Journal of Academy of Nutrition and Dietetics

CDC: Diabetes is more prevalent in disadvantaged groups • Remote counties • Populations that have less education • Populations with higher rates of unemployment *** • Diabetes prevalence is 15 -17% higher in rural areas than in urban areas (CDC MMWR data) • Rural America has a disproportionately high number of diabetes-related hospital deaths compared to urban America (most pronounced in the South and Midwest)
Rural barriers to accessing healthcare and health education • Shortage of physicians and providers in rural areas • Low health literacy of residents • Inadequate access to health insurance to cover medical appointments, medications and diabetes supplies • Low incomes that result in deferring care for financial reasons • Limited access to transportation to travel to appointments with primary or specialty care providers *** Int J Environ Res Public Health 2017, 14, 464
Barriers to DSMES in rural areas: – Fewer DSMES programs due to shortage of accredited service providers – Cost of service – Current reimbursement model limits accessibility – Transportation issues/distance to service – Independent nature of rural areas – Provider and medical community service availability
The ‘rural patient experience’ – providing DSMES in rural areas of need and what works: • Find resources that target the needs of low-income populations – poverty in rural areas is a huge challenge • For culturally diverse populations, employ bilingual and/or culturally competent staff • Provide education appropriate to age, culture, and literacy level • Create an advisory or stakeholder group that represents the diversity of the community
Challenges and strategies to overcome them: • Transportation issues – help coordinate transportation, minimize travel, use flexible scheduling • Timing of classes often doesn’t fit rural schedules – be flexible, offer alternate timing • Provider challenges in rural areas – help promote ongoing provider education, participate in a learning collaborative • Implement team approach to support providers and decrease burnout

ICAHN
Illinois Diabetes Action Plan Strategic Priority Areas 1. 34 million DM 3. 6 million pre DM 1. Data and Health Information Technology Support for existing and invest in new systems 2. Finance and Reimbursement increase access, reduce burden (social, economic, cultural, geographic) 3. Community and Clinical Links strengthening care coordination mechanisms and referrals What can DSMES Programs Do
Insurance Link: supporting referral • Insurance companies offering wellness incentivization • Partner with commercial insurance to be linked for access in community • Work with patients to better understand their benefits and technology
Technology Applications • Investigate remote monitoring platforms and CMS new reimbursement rules • Possible options: mysugr, onetouch revel, glooko • Investment in equipment • Population health management to identify patients for participation • Staff remote monitor and contact incident to treating healthcare provider • CPT coding and revenue generation
Additional Service Lines to DSMES • Medical Nutrition Therapy (MNT) Registered Dietitian on DSMES team can offer individual or class interventions • Intensive Behavioral Therapy (IBT) for obesity management: staff (RD) can offer incident to provider and CMS covers with no co-pay or deductible • National Diabetes Prevention Program Lifestyle Program for pre-diabetes, may include newly diagnosed diabetes to support program
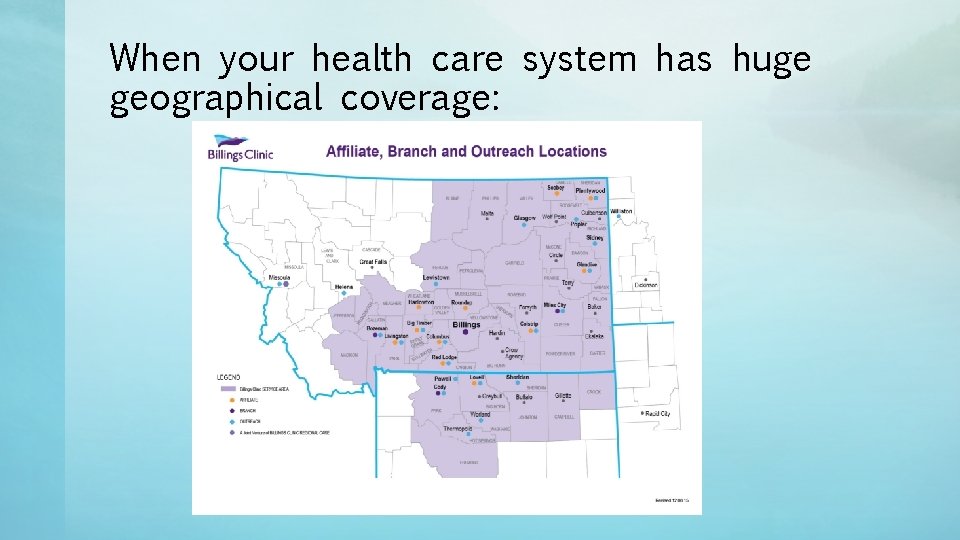
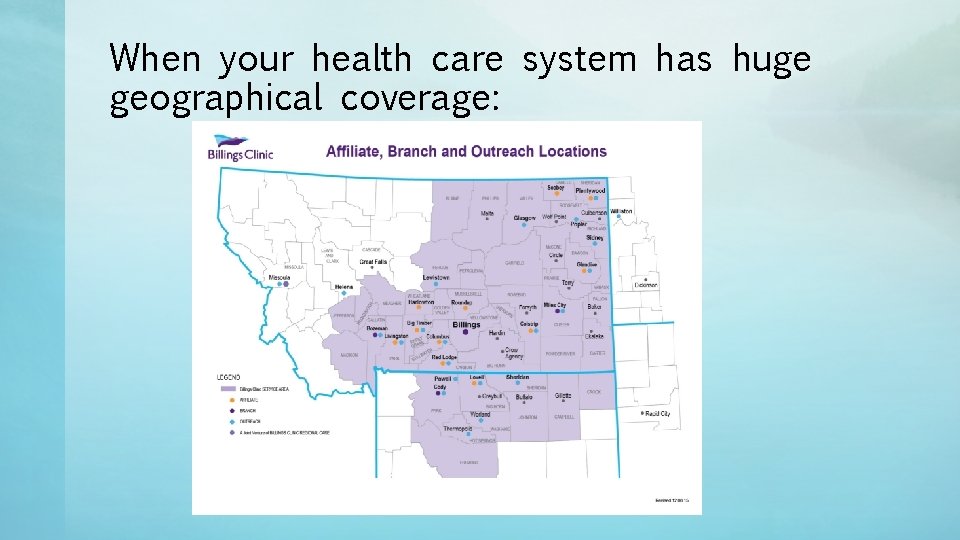
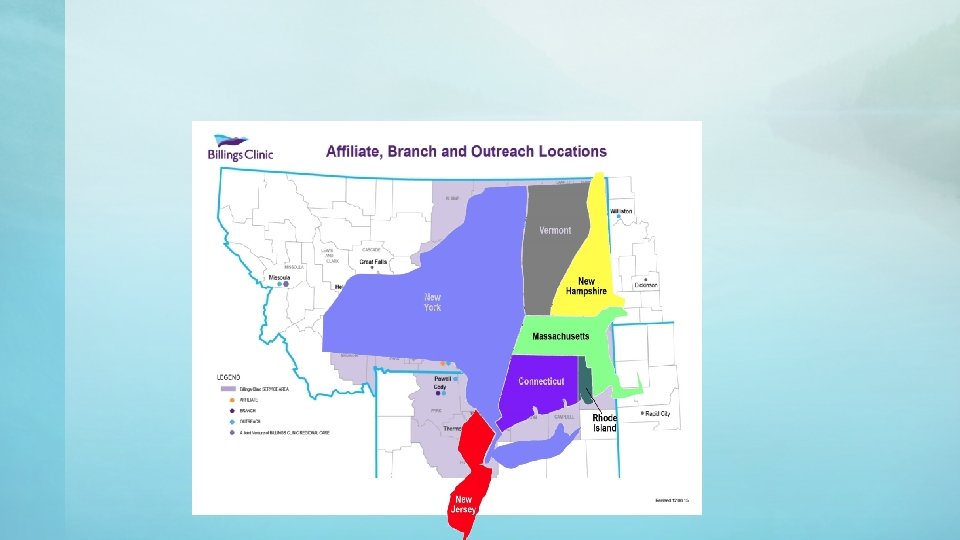
When your health care system has huge geographical coverage:
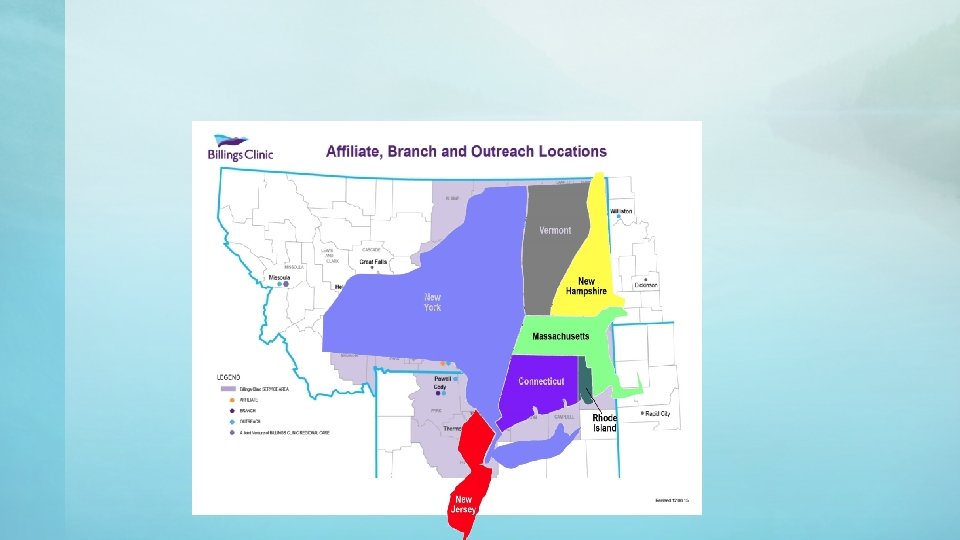
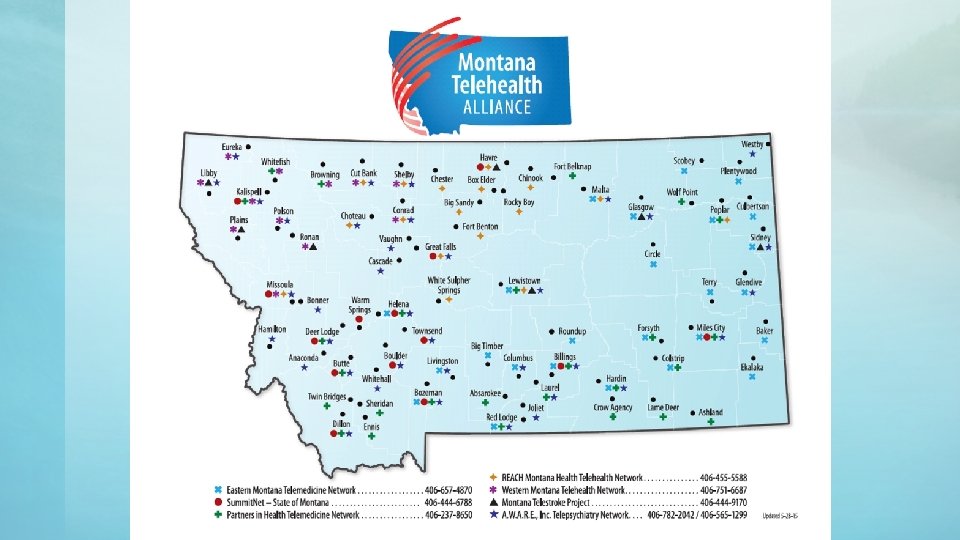
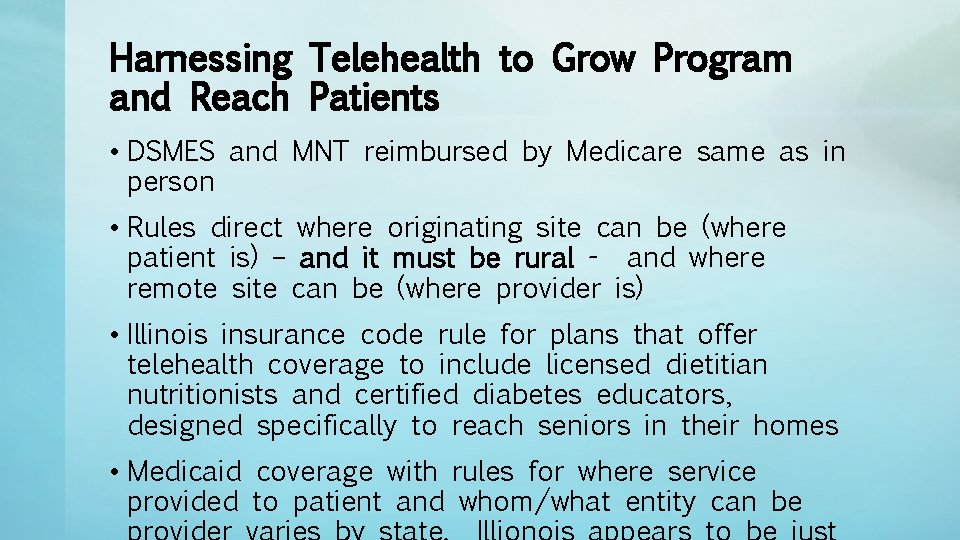
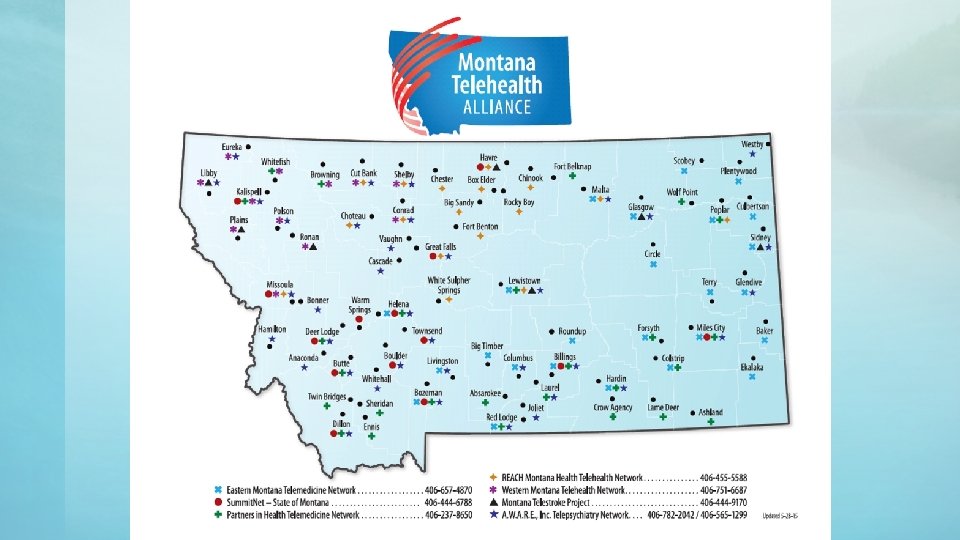
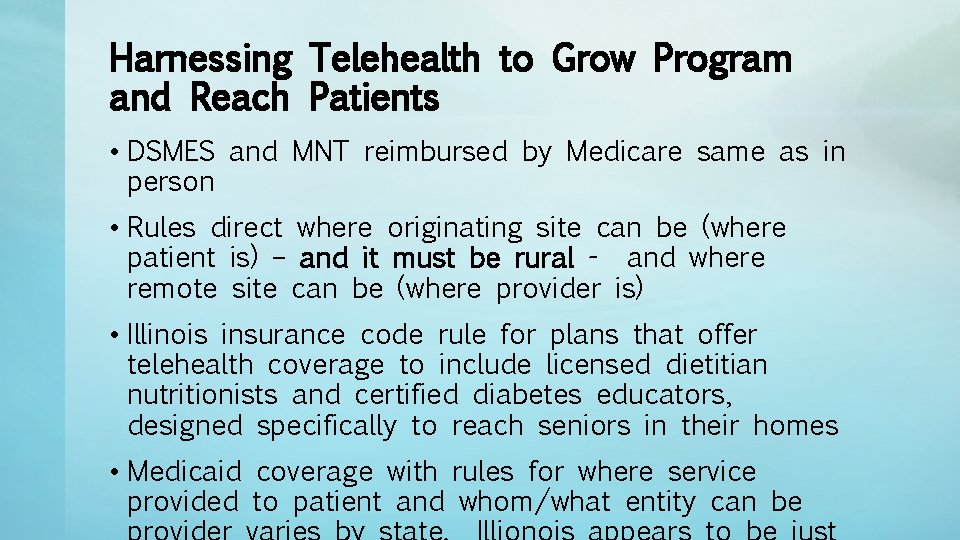
Harnessing Telehealth to Grow Program and Reach Patients • DSMES and MNT reimbursed by Medicare same as in person • Rules direct where originating site can be (where patient is) – and it must be rural - and where remote site can be (where provider is) • Illinois insurance code rule for plans that offer telehealth coverage to include licensed dietitian nutritionists and certified diabetes educators, designed specifically to reach seniors in their homes • Medicaid coverage with rules for where service provided to patient and whom/what entity can be
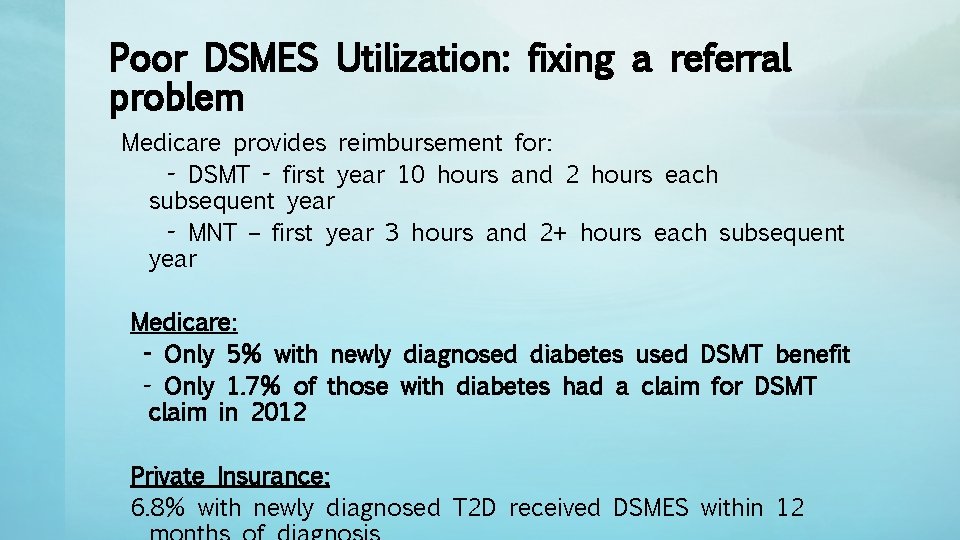
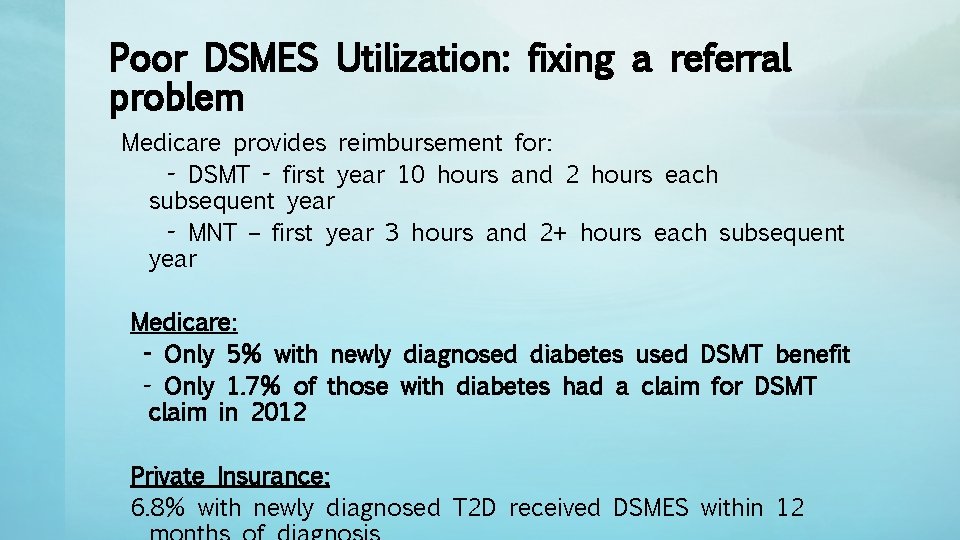
Poor DSMES Utilization: fixing a referral problem Medicare provides reimbursement for: - DSMT - first year 10 hours and 2 hours each subsequent year - MNT – first year 3 hours and 2+ hours each subsequent year Medicare: - Only 5% with newly diagnosed diabetes used DSMT benefit - Only 1. 7% of those with diabetes had a claim for DSMT claim in 2012 Private Insurance: 6. 8% with newly diagnosed T 2 D received DSMES within 12
How can DSMES Programs Engage and Support Providers in reaching patients • Create network with providers and staff • Carve out time to see and be seen…or heard • Provide tools that will support referrals • Create methods and scripting for all clinic and program staff • Ask what you and your program can do
Making the Most of your Program • Make your program patient centered and promote that to your audiences • Remember – and talk about – that your patient is First a human, second a person with diabetes • You and your program are marketing tools
Share with providers your DSMES script • “your provider cares about giving you the highest quality health care” • “when you see us for healthcare, we feel you are hiring us for only the best, and Diabetes Self Management Education is an absolute standard of the best in medical care for diabetes” • “we are all working as a team to give you the best care to keep you safe and at your healthiest”
Ask provider to consider scripting • “part of my caring for your diabetes is giving you knowledge; because they have more time and expertise with the many components of self care for diabetes, you need to have diabetes education” • “our clinic uses a team approach to your diabetes care, and as your provider I have a diabetes program that I work with for part of your care” • “we have a diabetes expert in the building and I am sending you to her/him”
And even some scripting for staff • Nurses: “we all work together to care for you and the diabetes program will teach and support you and work with us” • Scheduling/support staff: “if you have questions about how your care with Diabetes Education will go we can connect you” • All Clinic: “all components of your health care important and we all work together to keep you safe”
Shared Appointments/Diabetes Appointments • Shared appointments can be created in a clinic to have many patients scheduled for same time and a session lead by CDE • Provider sees patient briefly but with intervention supported by CDE is able to up-code • Can be valuable if clinic engages in a "diabetes day" or partial day and more than one provider uses system • CDE leads a visit on a parameter of self care such as foot care, sick day management, etc
CDE supported medical visits • CDE sees patients with provider for a day or partial day • Works when able to concentrate "diabetes days" for provider(s) in clinic • CDE triages medication, data, tech use • Is not coded as DSMES, but translates to smooth follow up scheduling for DSMES • High provider and patient satisfaction
Engaging PWD – rural or otherwise! • Go where people with diabetes in rural communities gather: – School: offer education for T 1 DM, PIR days – Church: partner with parish nurse? – Community or senior centers – Coffee shop or local café – Work-related sites (? grain elevator, mine, etc) – Grocery store or farmers market – Library – Gym/Work-out Club
Marketing your diabetes education services in rural communities • Where does your target audience get their information? ASK THEM! – Newspaper – Online or social media: this is big and growing – Radio: PSA? – TV – Local ‘tidbit’ type of newsletters – Word of mouth – usually BIG in rural communities – Parish Health/Nurses – Any time someone asks for support. . . local gym, trainers ALWAYS make time to talk and support
No to Lectures, Yes to Engaging educational tools • No More Didactic, ‘lecture-based’ or power pointbased classes • There are times to be serious, but there also times to HAVE FUN! How do we learn best? When we are engaged and enjoying the content and relationships we are building. • Hands on, interactive tools…don’t have to be expensive! Ex: Food labels, measuring cups/spoons, various plate sizes
Engaging Education Tools • Motivational Interviewing: – Helping people evoke their own ideas about and solutions for challenges they face in taking care of their diabetes • Storytelling: – Use of tales of personal problems, plans, execution, and positive outcomes of individuals faced with health challenges • Edu-taining – Making your own brand of information sharing based on audiences unique characteristics
Collaborative goal setting and support • Discuss what is important to the PWD, and allow him/her to set SMART goal that they can work on • Maybe call it a goal, or a plan, or a “what one thing could you change until we visit again and talk about how it went? ” • Follow Up on that goal, assess and evaluate, set goal again • Teaching to the person first, making sure they know that by coming to their medical appointments they are meeting a primary goal of caring for themselves. And it is a very positive decision and pathway we are on. – Dr. Vincent Montori – Mayo Clinic: “Minimally disruptive medicine” and the “patient revolution” concepts in caring for people
Adversity, when used properly, will buy you a ticket to a place you couldn't have gone any other way Tony Bennet, NCAA Champion Virginia Cavaliers men’s basketball coach

Thank you Kristine Kilen, RD, CDE kkilen@billingsclinic. org
Resources • Guiciardi, et al; BMC Health Serv Res. 2016; 16: 249. Designing and delivering facilitated storytelling interventions for chronic disease self-management: a scoping review • Motivational Interviewing In Health Care – Helping Patients Change Behavior” by Rollnick, Miller, and Butler • “Motivational Interviewing in Diabetes Care” by Steinberg and Miller • “Building Motivational Interviewing Skills: A Practitioner’s Workbook” by Rosengren • Lifestyle Management: Standards of Medical Care in Diabetes — 2019 Diabetes Care 2019 Jan; 42 (Supplement 1): S 46 -S 60. https: //doi. org/10. 2337/dc 19 -S 005
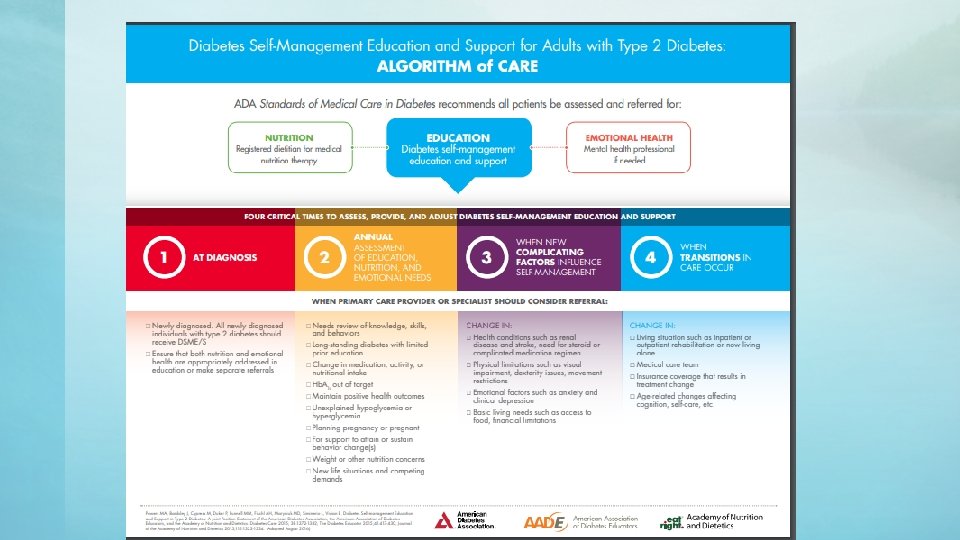
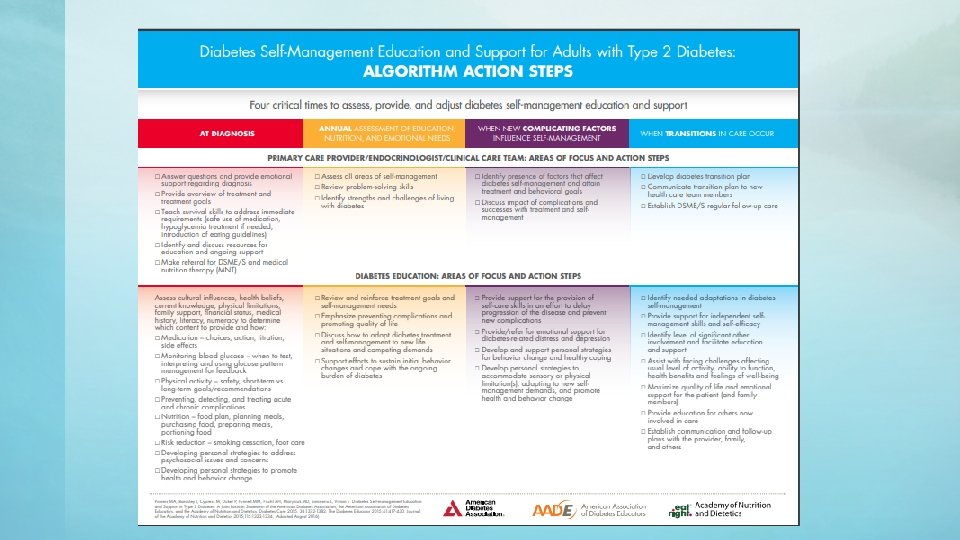
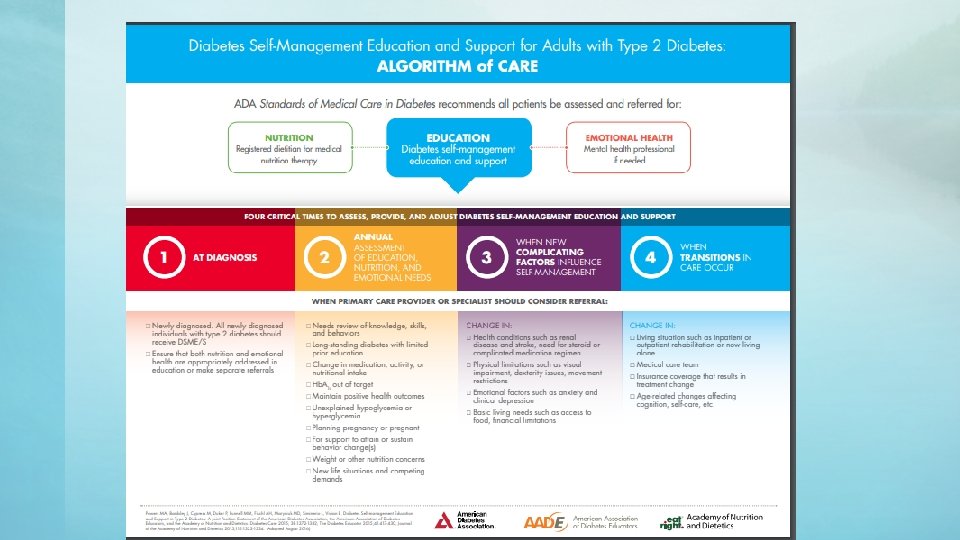
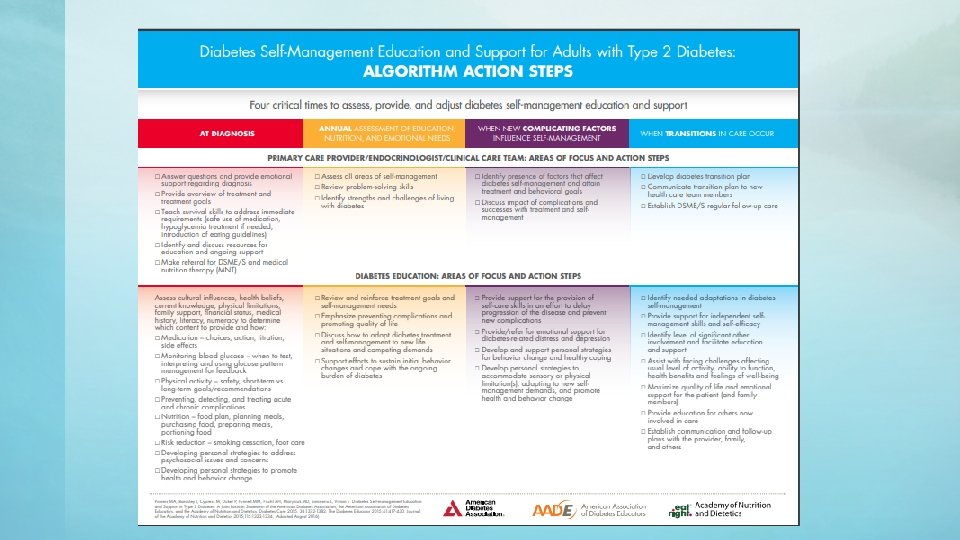
Resources • Improving Care and Promoting Health in Populations: Standards of Medical Care in Diabetes— 2019 Diabetes Care 2019 Jan; 42 (Supplement 1): S 7 -S 12. https: //doi. org/10. 2337/dc 19 -S 001 • Bardsley, J. , Baker, K. M. , & Powers, M. (2017). Diabetes Selfmanagement Education and Support Algorithm of Care: Tools for Use and Dissemination. AADE in Practice, 5(5), 22– 28. https: //doi. org/10. 1177/2325160317720184
 Rfmlp
Rfmlp Building a recruitment and retention plan
Building a recruitment and retention plan Physician recruitment onboarding and retention
Physician recruitment onboarding and retention What is recruitment
What is recruitment Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Heti rpr
Heti rpr Recruitment retention recovery
Recruitment retention recovery Colorado employee record retention requirements
Colorado employee record retention requirements Bsbhrm506
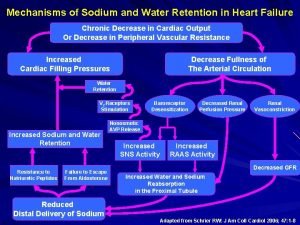
Bsbhrm506 Insulin and sodium retention
Insulin and sodium retention Ferris orientation
Ferris orientation Pathophysiology of sodium and water retention
Pathophysiology of sodium and water retention Urban rural difference
Urban rural difference Features of primary retention form
Features of primary retention form Grooves and coves
Grooves and coves Features of primary retention form
Features of primary retention form орнокард
орнокард Chapter 9 agricultural transformation and rural development
Chapter 9 agricultural transformation and rural development Chapter 9 agricultural transformation and rural development
Chapter 9 agricultural transformation and rural development How to build customer satisfaction value and retention
How to build customer satisfaction value and retention Urban and rural definition
Urban and rural definition Service and follow up for customer retention
Service and follow up for customer retention Reference and retention samples
Reference and retention samples Ministry of agriculture and rural development cameroon
Ministry of agriculture and rural development cameroon Induction in hrm
Induction in hrm Rural and urban settlements grade 12
Rural and urban settlements grade 12 Retention and disposal of gmp documents
Retention and disposal of gmp documents Employee separation and retention management
Employee separation and retention management Support retention and stability
Support retention and stability Ministry of agriculture and rural development vietnam
Ministry of agriculture and rural development vietnam Pre purchase evaluation of alternatives
Pre purchase evaluation of alternatives Business retention and expansion survey
Business retention and expansion survey Functional cusp bevel
Functional cusp bevel Managing careers and retention
Managing careers and retention Retention and drainage
Retention and drainage Retention and drainage
Retention and drainage Segmentation of rural market
Segmentation of rural market Building customer satisfaction value and retention
Building customer satisfaction value and retention Building customer satisfaction
Building customer satisfaction