Recent Advances in IOP measurements Dr Deepak Megur
- Slides: 17
Recent Advances in IOP measurements Dr Deepak Megur Cataract and Glaucoma services Megur Eye Care Centre Bidar Karnataka
Tonometry Why…? • Because…. – “IOP is the only modifiable risk factor in Glaucoma” – Most frequently examined parameter in the follow up of a glaucoma pt.
What to use…? • Goldmann Applanation Tonometry • Gold Standard Tono. Pen: Acceptable (SEAGIG Asia Pacific Glaucoma guidelines)
Factors affecting measured IOP. • Central Corneal Thickness: – Thicker Corneas: Artificially elevated IOP – Thinner Cornea: Artificially decreased IOP – Correction nomogram: • 525 Micron • 1 -3 mm hg per 40 micron deviation. ( SEAGIG Asia Pacific Guidelines 2004)
Central Corneal Thickness • Measurement – Ultrasonic Pachymeter – Measured along / Before GAT – Time of measurement, waking hours • CCT – Predicting Risk factor – Prognostic significance – Response to drugs
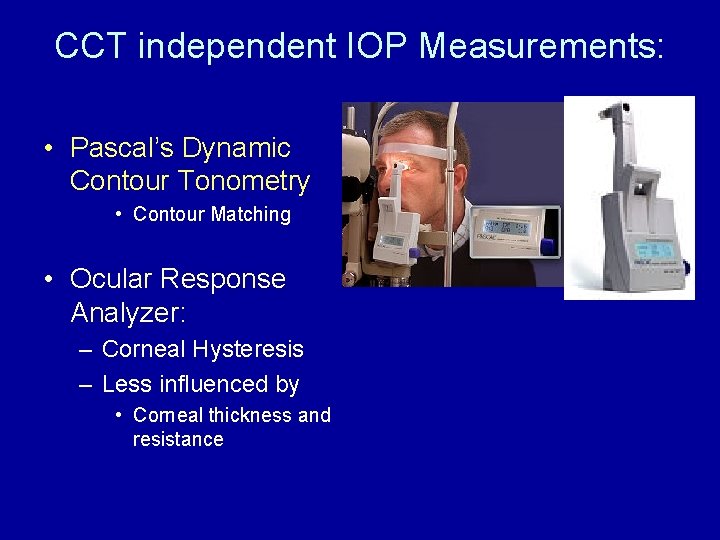
CCT independent IOP Measurements: • Pascal’s Dynamic Contour Tonometry • Contour Matching • Ocular Response Analyzer: – Corneal Hysteresis – Less influenced by • Corneal thickness and resistance
Pascal’s Dynamic Contour Tonometry. • Slitlamp-mounted. . • Direct measurement of pressure - no systematic errors from force-to-pressure conversion. • Numerical display of result. • No mechanical calibration required; self-calibrating. • Convenient disposable tip prevents contamination and potential infection • Battery operated - no cabling. • Visual control of eye/tip interface through transparent Sensor. Tip. • Single button operation.
Pascal’s Dynamic Contour Tonometry • Dynamic contour tonometry (DCT) is a novel method which uses principle of contour matching instead of applanation. • This is designed to reduce the influence of biomechanical properties of the cornea on measurement. • These include corneal thickness, rigidity, curvature, and elastic properties. • It is less influenced by corneal thickness but more influenced by corneal curvature than the Goldmann tonometer
DCT -Principles • It uses a miniature pressure sensor embedded within a tonometer tip contour-matched to the shape of the cornea. • The tonometer tip rests on the cornea with a constant appositional force of one gram. • When the sensor is subjected to a change in pressure, the electrical resistance is altered and the PASCAL's computer calculates a change in pressure in concordance with the change in resistance
• The contour matched tip has a concave surface of radius 10. 5 mm, which approximates to the shape of a normal cornea when the pressure on both sides is equal. • The probe is placed adjacent to the central cornea. • The integrated piezoresistive pressure sensor automatically begins to acquire data, measuring IOP 100 times per second. • A complete measurement cycle requires about 8 seconds of contact time. • The device also measures the variation in pressure that occurs with the cardiac cycle. (Ocular pulse Amplitude)
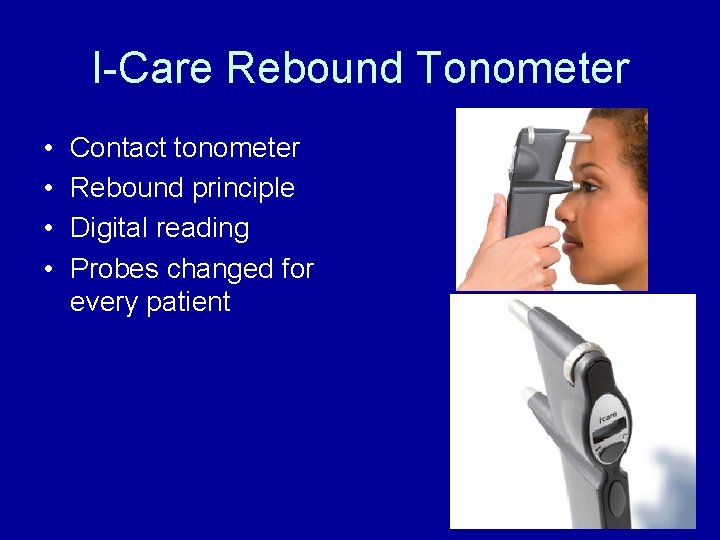
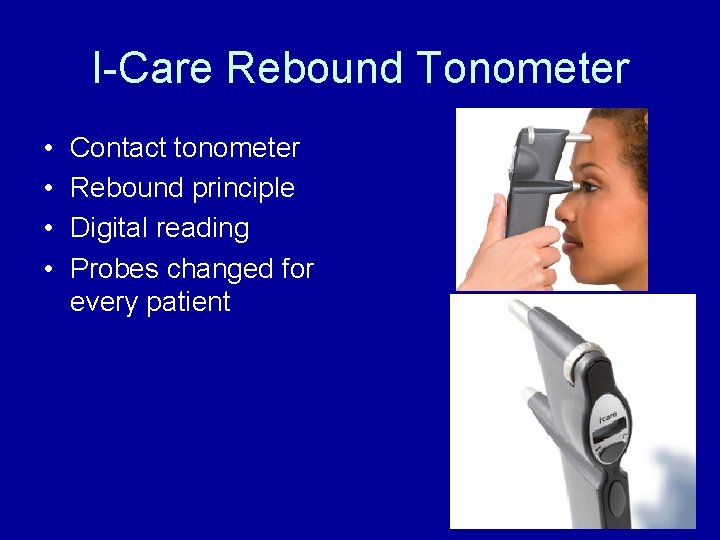
I-Care Rebound Tonometer • • Contact tonometer Rebound principle Digital reading Probes changed for every patient
Rebound Tonometers Principle • Determine IOP by bouncing a small plastic tipped metal probe against the cornea. • The device uses an induction coil to magnetise the probe and fire it against the cornea. • As the probe bounces against the cornea and back in to the device it creates an induction current from which the intraocular pressure is calculated.
I-Care Rebound Tonometer • Advantages: – Fast – No Anaesthetic required – Pt friendly – children • Affected by corneal properties. – Thickness – Hysteresis
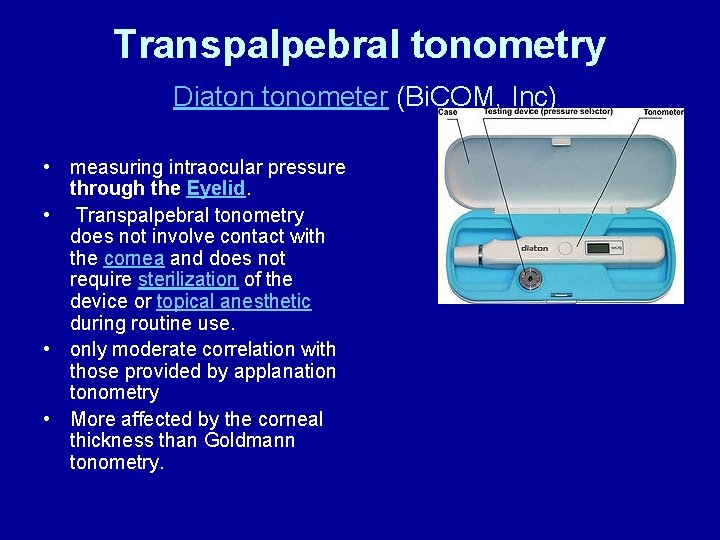
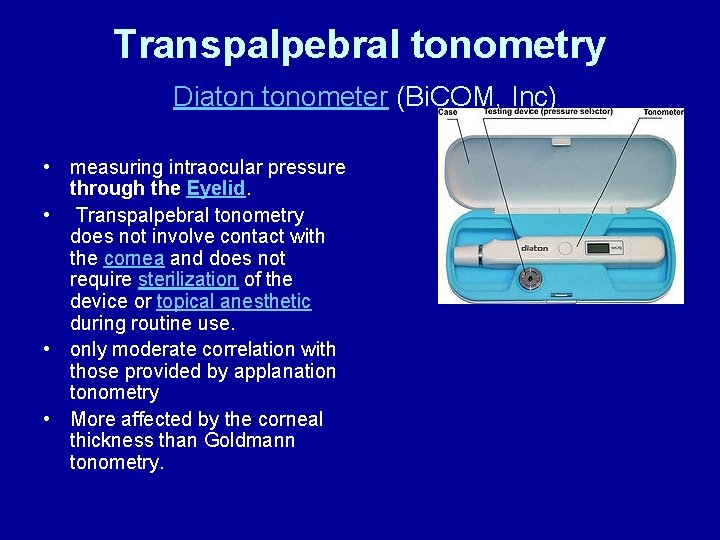
Transpalpebral tonometry Diaton tonometer (Bi. COM, Inc) • measuring intraocular pressure through the Eyelid. • Transpalpebral tonometry does not involve contact with the cornea and does not require sterilization of the device or topical anesthetic during routine use. • only moderate correlation with those provided by applanation tonometry • More affected by the corneal thickness than Goldmann tonometry.
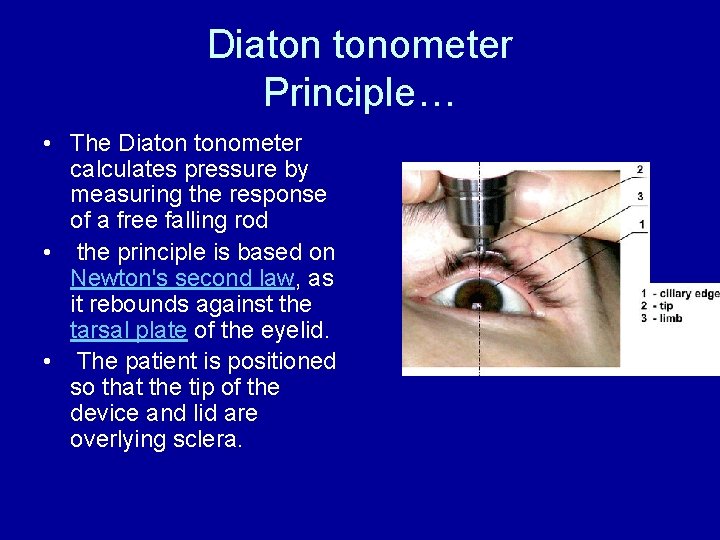
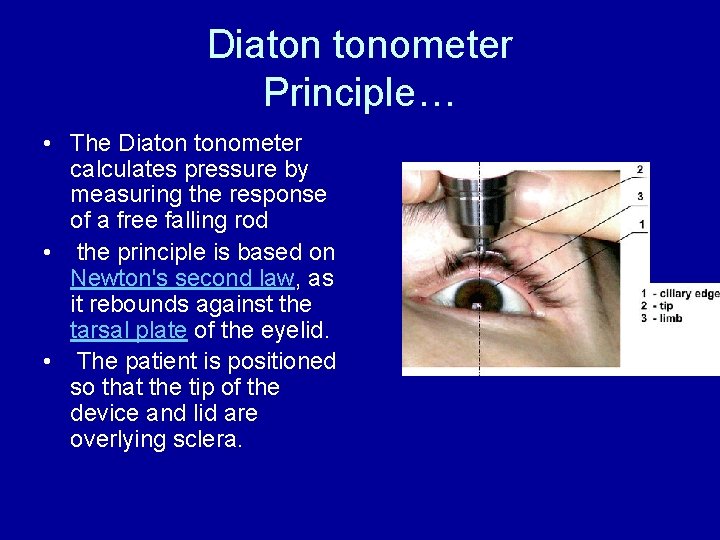
Diaton tonometer Principle… • The Diaton tonometer calculates pressure by measuring the response of a free falling rod • the principle is based on Newton's second law, as it rebounds against the tarsal plate of the eyelid. • The patient is positioned so that the tip of the device and lid are overlying sclera.
Non-contact tonometry or air-puff tonometry • Non-contact tonometry: • It uses a rapid air pulse to applanate the cornea. • Corneal applanation is detected via an electro-optical system. • Intraocular pressure is estimated by detecting the force of the air jet at the instance of applanation. •
Non-contact tonometry or air-puff tonometry • A fast and simple way to screen for high IOP. • However, modern non-contact tonometers have been shown to correlate well with Goldmann tonomtery measurements • Particularly useful – in children and other non-compliant patient groups. • non-contact tonometry – which reduces the potential for disease transmission…?
 Deepak megur
Deepak megur Deepak megur
Deepak megur Recent advances in dental ceramics
Recent advances in dental ceramics Coherent scattering
Coherent scattering Lurbinectedin posologie
Lurbinectedin posologie Advances in technology during wwii
Advances in technology during wwii Short term loans and advances
Short term loans and advances Advances in memory technology
Advances in memory technology Chapter 9 intellectual development in the first year
Chapter 9 intellectual development in the first year Opto-electronic advances
Opto-electronic advances Axis powers
Axis powers Advances in real-time rendering in games
Advances in real-time rendering in games Irac circular rbi
Irac circular rbi Loans and advances in tally
Loans and advances in tally Quick grammar review
Quick grammar review Iop
Iop Pravilnik o iopu
Pravilnik o iopu Pedagoški profil učenika primer
Pedagoški profil učenika primer