Radiological Category Thoracic Chest Principal Modality 1 MRI
- Slides: 16
Radiological Category: Thoracic Chest Principal Modality (1): MRI Principal Modality (2): None Case Report #0515 Submitted by: Paul S. Lee, M. D. Faculty reviewer: Sandra Oldham, M. D. Date accepted: 15 April 2008
Case History A previously-healthy 57 y/o woman experienced 6 months of exercise dyspnea while biking up hills, then while hiking and walking. Her physician heard a murmur and arranged additional evaluation. A cardiac MRI was performed in her workup where a mass was discovered. She was then transferred to our tertiary care center for further management. On admission, her physical exam showed a heart rate of 76 bpm, blood pressure of 138/92. A Grade III/VI harsh systolic murmur was heard all along the left sternal border, which increased with inspiration.
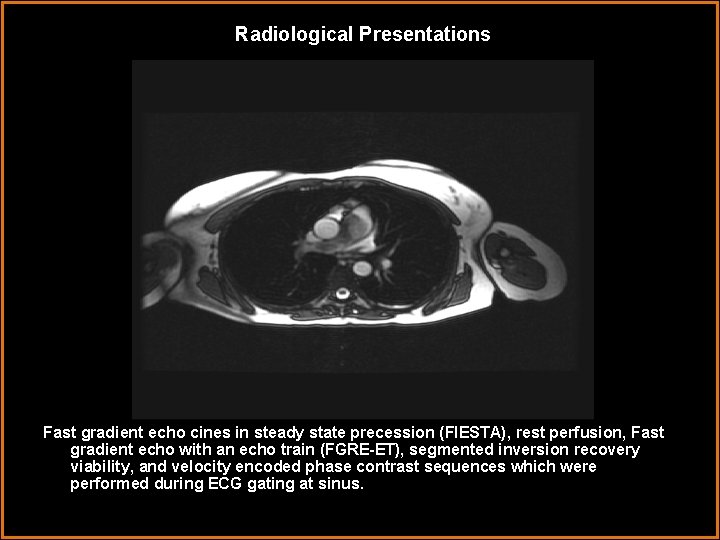
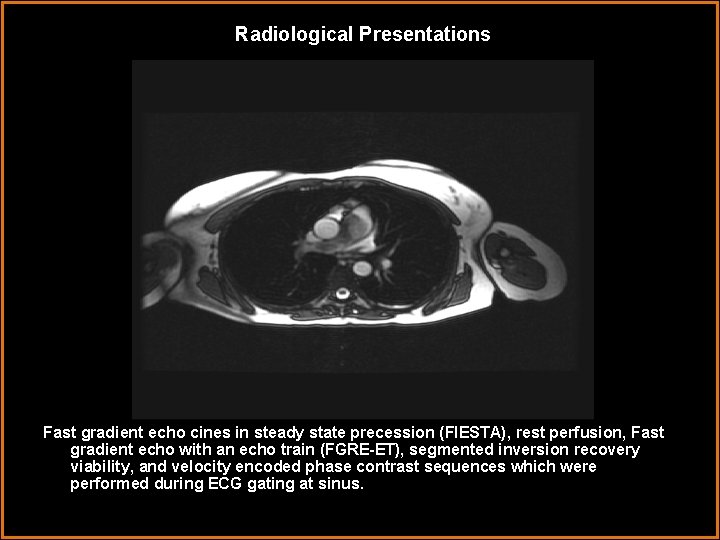
Radiological Presentations Fast gradient echo cines in steady state precession (FIESTA), rest perfusion, Fast gradient echo with an echo train (FGRE-ET), segmented inversion recovery viability, and velocity encoded phase contrast sequences which were performed during ECG gating at sinus.
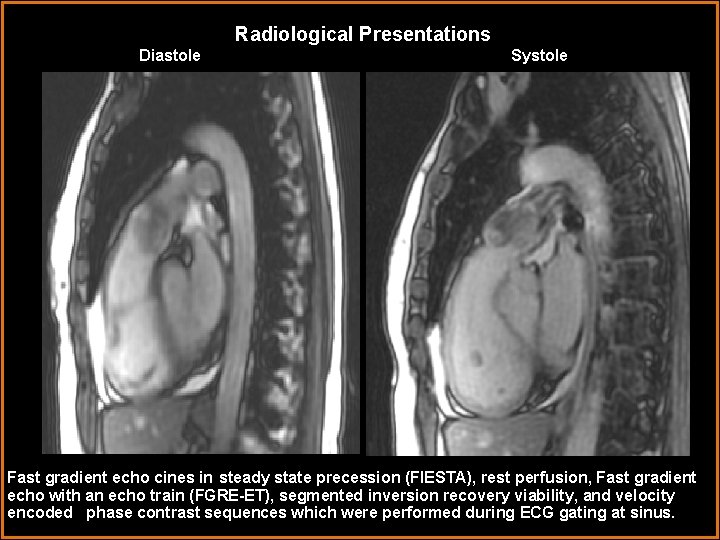
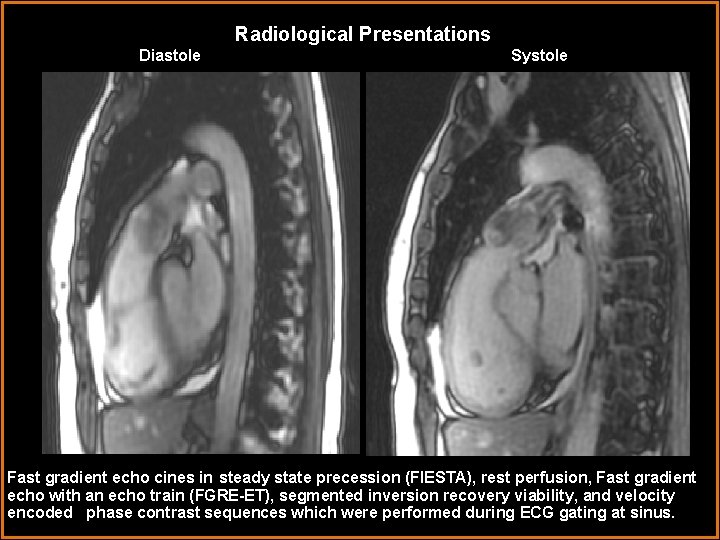
Radiological Presentations Diastole Systole Fast gradient echo cines in steady state precession (FIESTA), rest perfusion, Fast gradient echo with an echo train (FGRE-ET), segmented inversion recovery viability, and velocity encoded phase contrast sequences which were performed during ECG gating at sinus.
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Cardiac Myxoma • Pulmonary Embolism • Pulmonary Artery Sarcoma • Flow artifact • Fibroelastoma
Differential Why is this not flow artifact? Why is this not a pulmonary embolism? • This was a mass attached to the main pulmonary valve and right pulmonary artery. • This mass was mobile and displaced into the main pulmonary artery during systole and prolapsed into the RV during diastole. This “ball valve” motion has been noted in pulmonary artery sarcoma and would be unusual for an embolism.
Findings and Differentials Findings: Large multi-lobed, elongated, irregular mass extending from pulmonic valve, attached to walls of main pulmonary artery and right pulmonary artery. The mass was mobile, being displaced into the main pulmonary artery during systole(arrowhead), prolapsing back into the RV during diastole(arrow). It showed substantial distal displacement (1. 5 cm) with systole into the pulmonary artery and prolapse into the Right Ventricular Outflow Tract with diastole. A fragmented turbulent flow jet was noted through and around the mass during systole. The mass was relatively avascular and signal attenuated. Right ventricular ejection fraction was 49%. Differentials: • Pulmonary Embolism • Pulmonary artery sarcoma • Cardiac Myxoma • Fibroelastoma
Discussion • • Operative findings revealed that the pulmonary artery was firm with an intervascular mass involving the pulmonary valve and extending partly into the right pulmonary artery. However, a second mass was present in the right pulmonary artery behind the superior vena cava (SVC) extending into the hilum of the lung from the proximal right pulmonary artery. A resection of the main pulmonary artery, proximal left pulmonary artery and right pulmonary artery with resection of the pulmonary valve and right ventricular outflow tract was performed. The pulmonary valve, RVOT and right and left pulmonary arteries were reconstructed with homograft. Resection of the mediastinal mass and tricuspid valve annuloplasty were also performed.
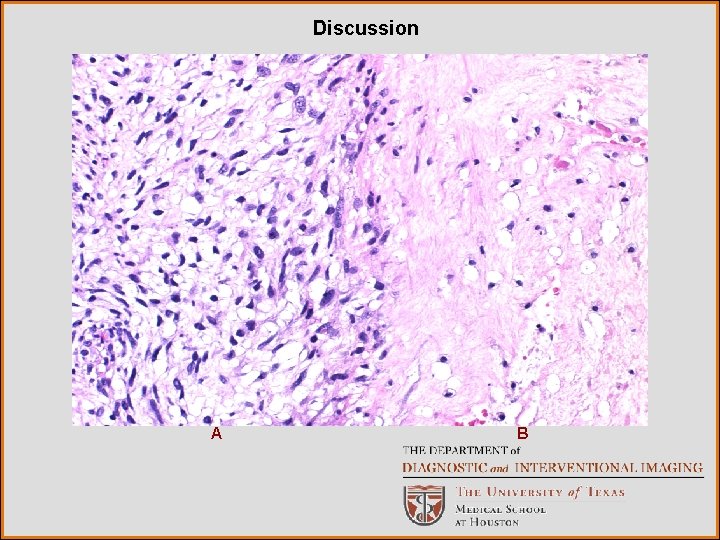
Findings Gross patholologic findings demonstrated two masses: The first was mass a fungating firm, pink tan lesion nodular lesion 5. 5 X 3. 0 X 2. 9 cm found in the valvular segment. The second was a soft pink tan nodular lesion 2. 5 X 1. 3 cm found at the birfurcation. Microscopic examination revealed 2 different histiologic patterns. (A) In other areas the lesion was cellular and composed of spindle cells with elongated nuclei with tapered ends, moderate nuclear pleomorphism and occasional mitotic figures(22 per 10 HPF). (B) Most of the mass was hypocellular with few vessels and demonstrated background fibrosis with myxoid change.
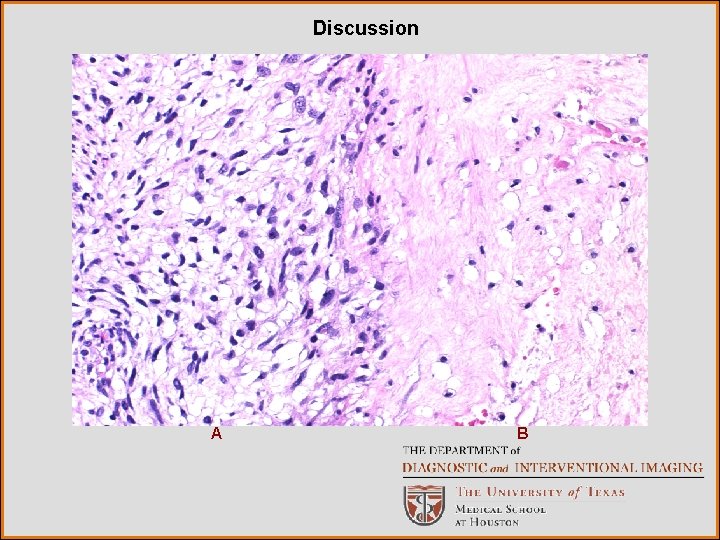
Discussion A B
Discussion Immunohistochemical stains: • Revealed that a small subset of spindled cells were positive for muscle specific actin and desmin. • It was rarely positive for smooth muscle actin and CD 31 and very rarely positive for myogenin. • Cytokeratin AE 1/AE 3, Cam 5. 2, S 100, and CD 34 were negative in the cells of interest. • CD 31 and CD 34 highlight the background vasculature.
Diagnosis -The morphologic and immunophenotypic features were most consistent with intimal sarcoma. -Based on poor differentiation, high mitotic activity and the presence of focal necrosis, this was considered a high-grade sarcoma FNCLCC grade 3. -This case was reviewed by three other pathologists, who concurred with the diagnosis.
Discussion Biologic aggressiveness is often predicted based on histologic grade. Two of the most commonly employed grading systems are the -US National Cancer Institute (NCI) system developed by Costa and colleagues -Federation Nationale des Centres de Lutte Contre le Cancer (FNCLCC) Sarcoma Group. (I, III) FNCLCC system employs a score generated by the evaluation of three parameters: -tumor differentiation, -mitotic rate -amount of tumor necrosis.
Discussion • • • Pulmonary Artery Sarcomas (PAS) are rare tumors, only a few hundred cases are reported in the literature. Those involving the pulmonary valve as in our case are even more rare. Pulmonary artery sarcomas are the most common type of primary neoplasm found in the pulmonary artery. (1) As a group pulmonary artery neoplasms have a poor prognosis. Therefore early diagnosis and treatment is essential to patient favorable outcome. Review literature from both the 1990’s and current journals, convey the same information about PAS. Due to the nonspecific symptoms they are most often misdiagnosed as chronic pulmonary embolus and treated with anticoagulation. According to the most review articles done in the 1990’s which examined 138 cases the mean age of diagnosis was 49. 3 years (range 13 -81). Some literature reports a roughly equal sex distribution while others report a slightly female predominance. (1)
Discussion • Treatment is usually surgical with or without adjuvant chemotherapy or radiation therapy. However, the results of adjuvant therapy while encouraging have yet to demonstrate a clear improvement in mortality. • These patients as a whole have a poor prognosis. The average survival with surgical resection is 12 months after diagnosis and 1. 5 months without treatment. • A recent article by Huo et al. (3) discusses 12 cases of pulmonary artery sarcomas at MD Anderson between 1990 -2004. The longest survival document recently was 68 months. The cases reviewed by Huo et al. concluded that patients with leiomyosarcoma had the longest survival and the worst prognosis with rhabdomyosarcoma , whereas patients the diagnosis of high grade sarcoma fell somewhere in between. (3) • However, in contrast to intimal sarcomas which are thought to arise from pluripotent intimal cells, leimyosarcomas originate from the media of the vessel are generally referred to as mural sarcomas and considered distinct from each other. (3, 1)
References (1) Yi ES. Tumors of the pulmonary vasculature. Cardiology Clinics 22. 2004 431440. (2) Bloomberg RD, Butany JW, Cusimano RJ, Leask RL. Primary cardiac sarcoma involving the pulmonary artery and valve. Canadian J Cardiology. 2003 Jun; 19(7): 843 -7 (3)Huo L, Moran CA, Fuller GN, Gladdish G, Suster S. Pulmonary Artery Sarcoma. A Clinicopathologic and Immunohistochemical Study of 12 Cases. American Journal of Clinical Pathology 2006; 125: 419 -424 (4) Cox JE, Chiles C, Aquino SL, Savage P, Oaks T. Pulmonary Atery Sarcomas: a Review of Clinical and Radiographic Features. Journal of Computer Assisted Tomography. 1997; Vol 21(5), Sept. /Oct. pp 750 -755 (5) Sparrow PJ, Kurian JB, Jones TR, Sivananthan MU. MR Imaging of Cardiac Tumors. Radiographics. 2005; Volume 25(5) pp 1255 -1276 (6) Parish JM, Rosenow EC, Swensen SJ, Crotty TB. Pulmonary Artery Sarcoma Clinical Feature. Chest 1996 Vol. 110(6) Dec. pp 1480 -1488