Radiological Category Thoracic Chest Principal Modality 1 General
- Slides: 18
Radiological Category: Thoracic Chest Principal Modality (1): General Radiography Principal Modality (2): PET/CT Case Report #0512 Submitted by: Patricia Franco, M. D. Faculty reviewer: Jeremy Erasmus, M. D. Date accepted: 11 April 2008
Case History 58 year old male with progressive shortness of breath and weight loss.
Radiological Presentation Figure 1
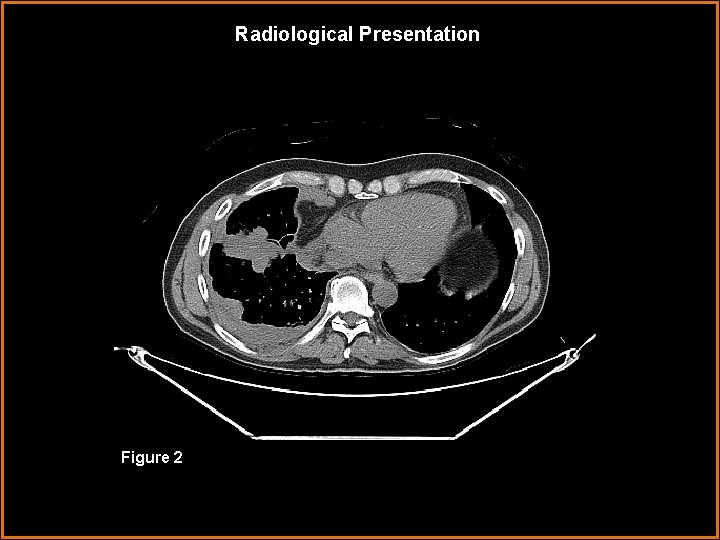
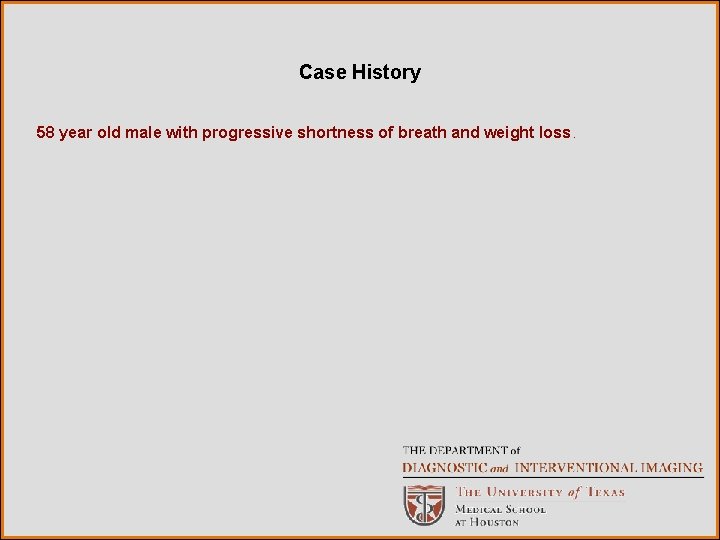
Radiological Presentation Figure 2
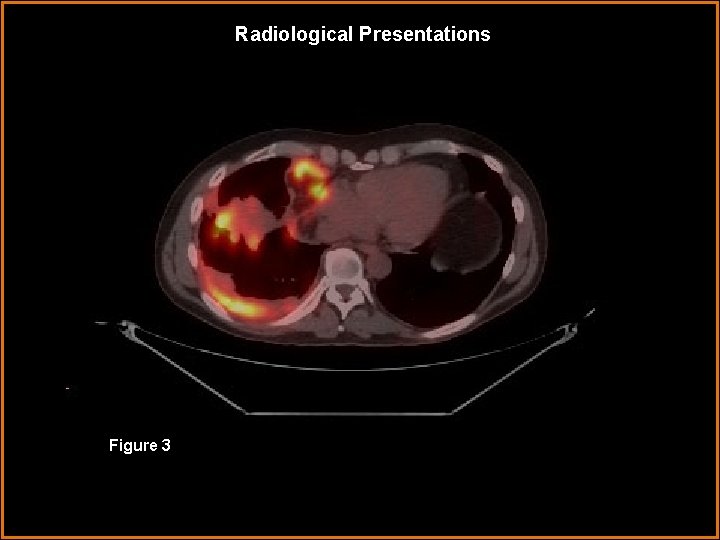
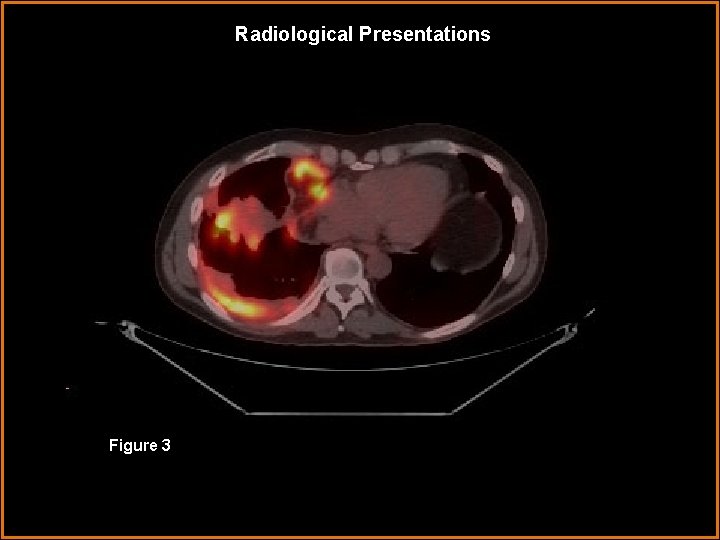
Radiological Presentations Figure 3
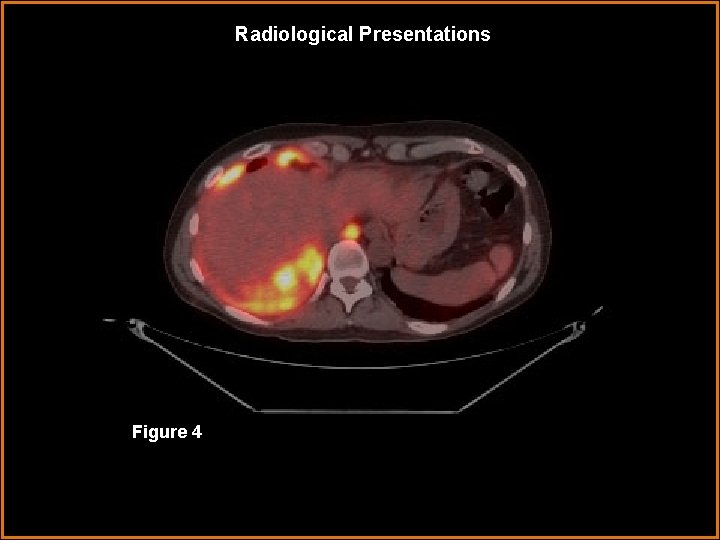
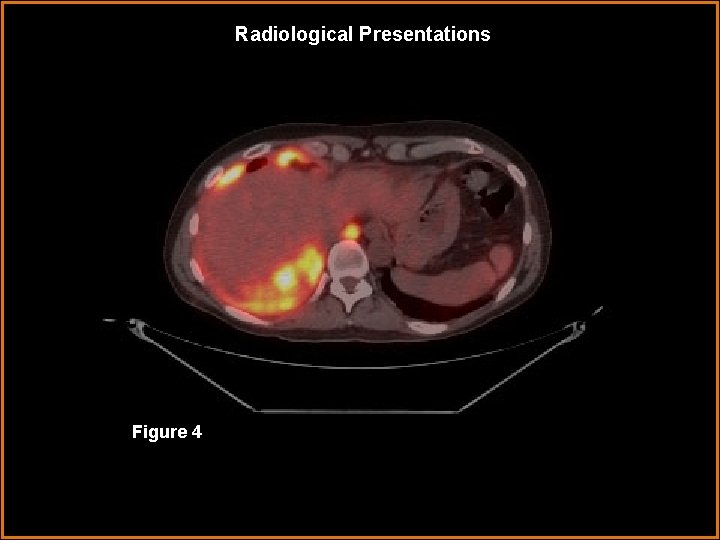
Radiological Presentations Figure 4
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Metastatic adenocarcioma of the pleura • Fibrosarcoma of the pleura • Malignant Mesothelioma • Fibrous Tumor of the pleura
Findings and Differentials Findings: PA view of the chest shows diffuse pleural thickening forming a rind of tumor that encases the right lung. There is volume loss with mild elevation of the right hemidiaphragm and a small pleural effusion ( Fig 1 ). Contrast-enhanced chest CT shows this multifocal nodular pleural thickening extending into the major fissure and the small pleural effusion ( Fig 2 ). On PET-CT, the nodules extend from the apex down to the anterior and posterior pleural recesses and have increased FDG uptake (max SUV 11. 3) No left-sided pleural or parenchymal FDG avid lesions are demonstrated. Additionally, an enlarged node adjacent to the descending aorta has low-grade increased metabolic activity suggests metastatic disease (maximum SUV 3. 4). ( Figs 3 and 4 ) Differential Diagnosis: • Metastatic adenocarcinoma of pleura • Malignant mesothelioma
Diagnosis: Malignant Pleural Mesothelioma (MPM)
Discussion Distinguishing malignant mesothelioma from metastatic adenocarcinoma and pleural sarcomas is difficult and usually requires a large amount of tissue in the pleural biopsy sample (3). Malignant pleural mesothelioma (MPM) is an uncommon neoplasm. It occurs more frequently in men than women with a ratio of 2 -6: 1. The peak of incidence occurs in the sixth and seventh decades of life and is associated with a history of occupational exposure to asbestos in 40% to 80% of patients (1, 2, 4). Patients typically present with chest pain and shortness of breath, and the diagnosis of mesothelioma is usually first suggested by imaging evaluation (4). Consequently, it has an essential role in the diagnosis and staging of patients with malignant mesothelioma (1, 2, 4)
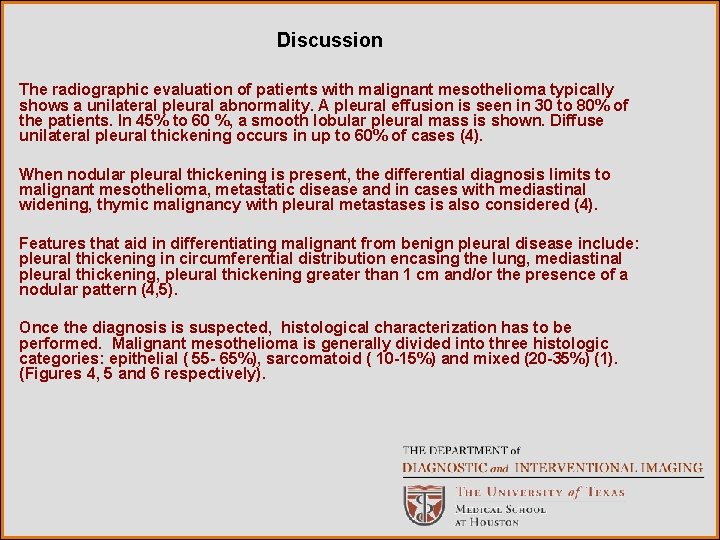
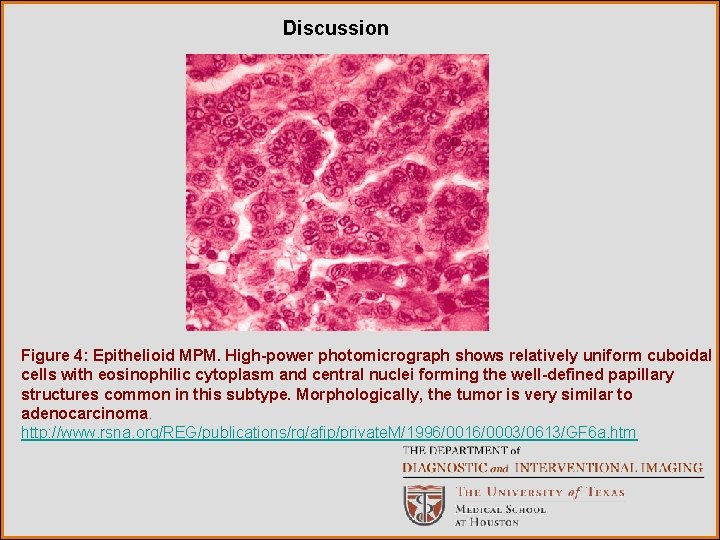
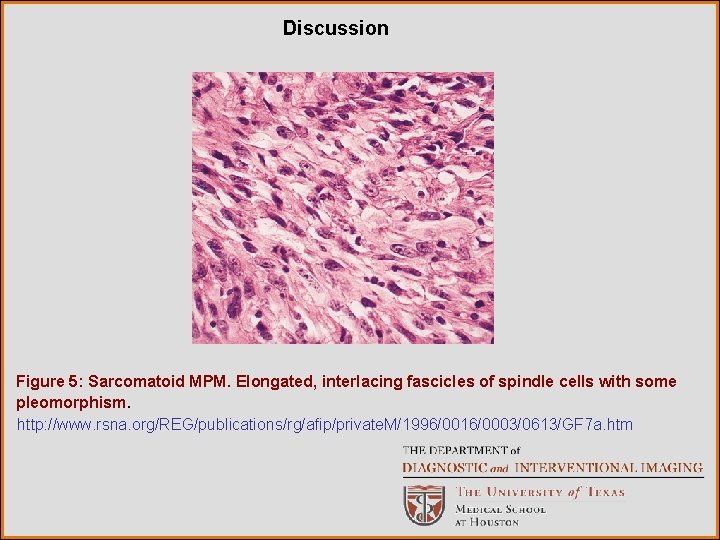
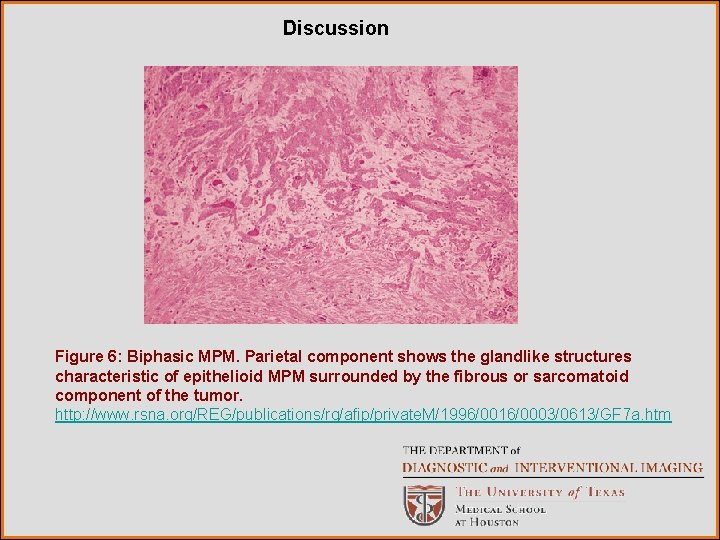
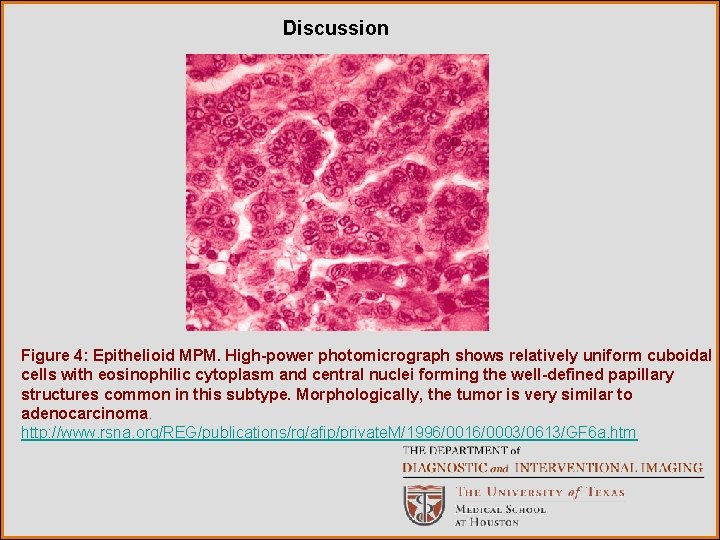
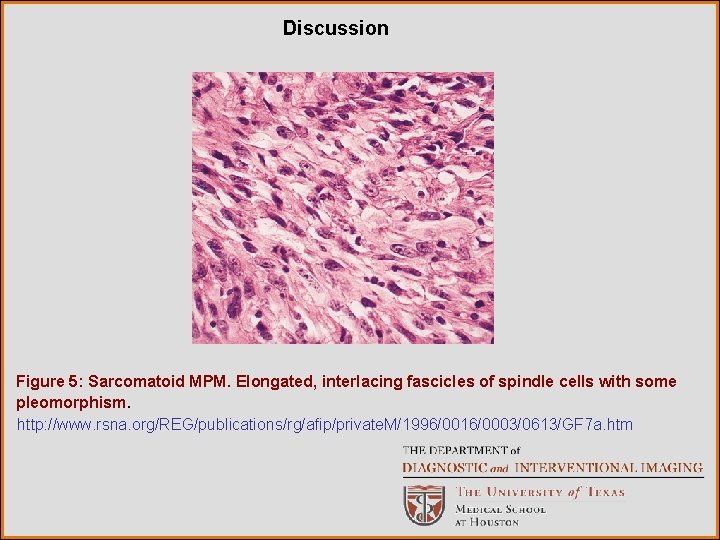
Discussion The radiographic evaluation of patients with malignant mesothelioma typically shows a unilateral pleural abnormality. A pleural effusion is seen in 30 to 80% of the patients. In 45% to 60 %, a smooth lobular pleural mass is shown. Diffuse unilateral pleural thickening occurs in up to 60% of cases (4). When nodular pleural thickening is present, the differential diagnosis limits to malignant mesothelioma, metastatic disease and in cases with mediastinal widening, thymic malignancy with pleural metastases is also considered (4). Features that aid in differentiating malignant from benign pleural disease include: pleural thickening in circumferential distribution encasing the lung, mediastinal pleural thickening, pleural thickening greater than 1 cm and/or the presence of a nodular pattern (4, 5). Once the diagnosis is suspected, histological characterization has to be performed. Malignant mesothelioma is generally divided into three histologic categories: epithelial ( 55 - 65%), sarcomatoid ( 10 -15%) and mixed (20 -35%) (1). (Figures 4, 5 and 6 respectively).
Discussion Figure 4: Epithelioid MPM. High-power photomicrograph shows relatively uniform cuboidal cells with eosinophilic cytoplasm and central nuclei forming the well-defined papillary structures common in this subtype. Morphologically, the tumor is very similar to adenocarcinoma. http: //www. rsna. org/REG/publications/rg/afip/private. M/1996/0016/0003/0613/GF 6 a. htm
Discussion Figure 5: Sarcomatoid MPM. Elongated, interlacing fascicles of spindle cells with some pleomorphism. http: //www. rsna. org/REG/publications/rg/afip/private. M/1996/0016/0003/0613/GF 7 a. htm
Discussion Figure 6: Biphasic MPM. Parietal component shows the glandlike structures characteristic of epithelioid MPM surrounded by the fibrous or sarcomatoid component of the tumor. http: //www. rsna. org/REG/publications/rg/afip/private. M/1996/0016/0003/0613/GF 7 a. htm
Discussion Treatment options depend on the stage of presentation. Multimodality regimens combining chemotherapy, radiotherapy, immunotherapy and surgery are being used more frequently in patient management. No single treatment has proven to be effective and death usually occurs within 12 to 17 months after diagnosis. (4) For patients with MPM of epithelial histology, early stage, negative nodes and adequate pulmonary function, extrapleural pneumonectomy (EPP) and adjuvant therapy are likely to prolong survival. The determination of local extent and identification of metastases with plain films is not sensitive or specific. CT is a better modality to use to evaluate the lung parenchyma and to assess the local extent and mediastinal invasion. MRI is used to address equivocal findings on CT concerning local extent of tumor. (4)
Discussion Both CT and MRI are suboptimal for the determination of mediastinal node disease. Complete nodal evaluation with mediastinoscopy, lacks the required sensitivity and specificity because not all nodal are accessible. (5) Integrated PET-CT increases the accuracy of overall staging and significantly improves the selection of patients being considered for EPP (6). Specifically, CT-PET detects more extensive disease involvement than that shown by other imaging modalities and is particularly useful in identifying occult distant metastases (5, 6). PET-CT may also aid in the determination of prognosis and treatment response (6). PET standardized uptake value (SUV) has been used as an indicator of prognosis and in the assessment of treatment response. The increment of FDG lesion uptake over time is a better predictor of aggressiveness than histologic grade (5).
References 1. Zhen J. Wang, Gautham P. Reddy, Michael B. Gotway, Charles B. Higgins, David M. Jablons, Mohan Ramaswamy, Randall A. Hawkins, and W. Richard Webb Malignant Pleural Mesothelioma: Evaluation with CT, MR Imaging, and PET Radio. Graphics 2004; 24: 105 -119. 2. MC Dynes, EM White, WA Fry, and GG Ghahremani. Imaging manifestations of pleural tumors. Radio. Graphics 1992; 12: 1191 -1201. 3. http: //www. education. auntminnie. com 4. Mylene T. Truong, Jeremy J. Erasmus, Edith M. Marom, and Reginald F. Munden. Imaging Evaluation in the Diagnosis and Staging of Malignant Pleural Mesothelioma. Seminars in Roentgenology, Vol 39, No 3 ( July ), 2004: pp 386 -396.
References 5. Mylene T. Truong, Edith M. Marom and Jeremy J. Erasmus. Preoperative Evaluation of Patients With Malignant Pleural Mesothelioma: Role of Integrated CT-PET Imaging. J Thorac Imaging. Volume 21, Number 2, May 2006. 6. Jeremy J. Erasmus, Mylene T. Truong, W. Roy Smythe, Reginald F. Munden, Edith M. Maron, et al. Integrated Computed Tomography-positron emission tomography in patients with potentially resectable malignant pleural mesothelioma: Staging Implications. J Thorac Cardiovasc Surg. 2005; 129: 1364 -70.