Radiological Category Thoracic Chest Principal Modality 1 CT
- Slides: 13
Radiological Category: Thoracic Chest Principal Modality (1): CT Principal Modality (2): None Case Report #0286 Submitted by: Davis Teichgraeber, M. D. Faculty reviewer: John Bruzzi, M. D. Date accepted: 15 April 2006
Case History 59 year old female presented to her physician with a two month history of facial swelling and erythema with dysphagia. The patient has a past medical history of myasthenia gravis that was diagnosed 4 years earlier. Initial chest x-ray (not available) at the time of diagnosis was reported as normal without evidence of a mediastinal mass. She was treated with IV immunoglobulin and high dose steroids over a period of several years then weaned off.
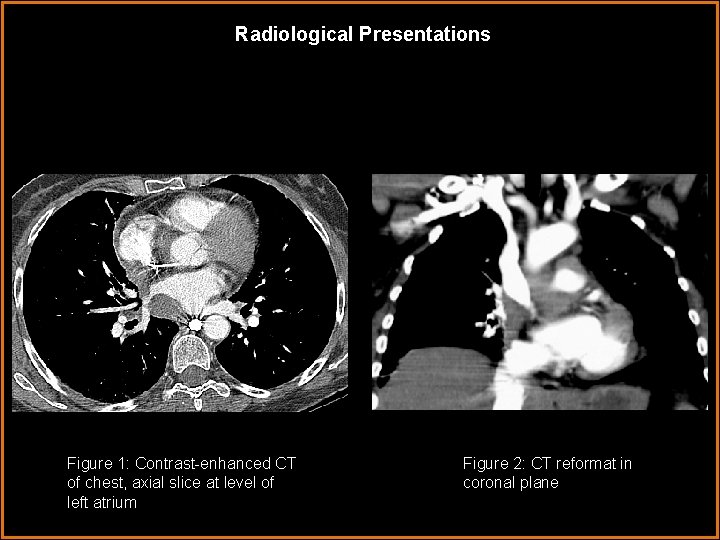
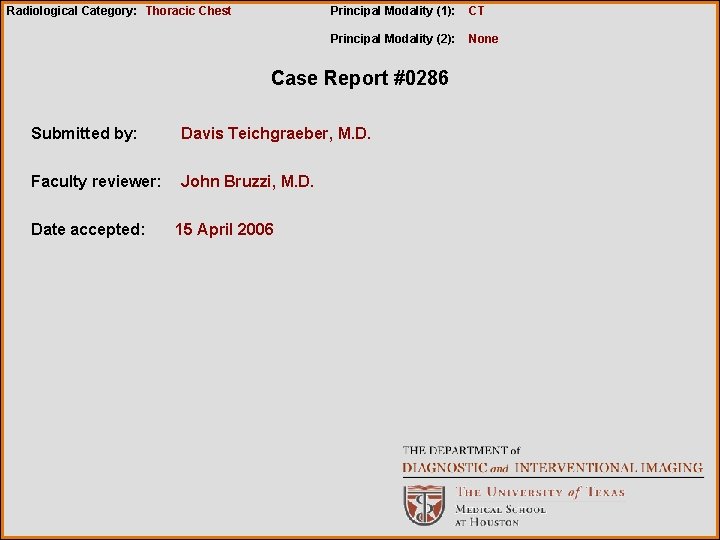
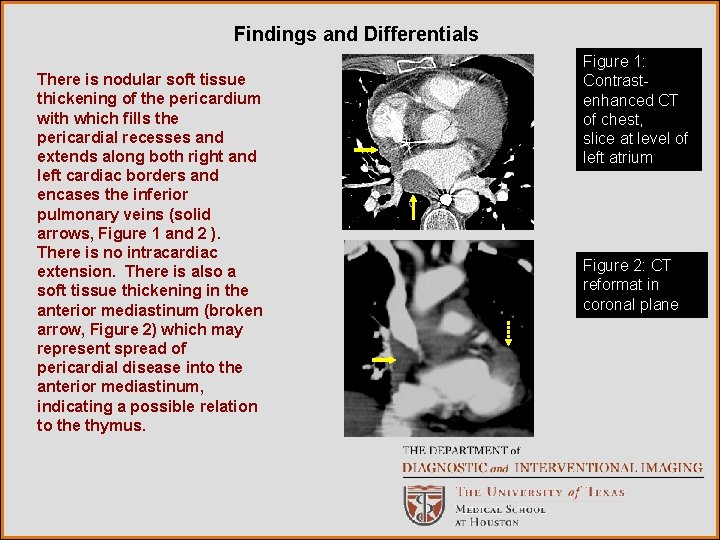
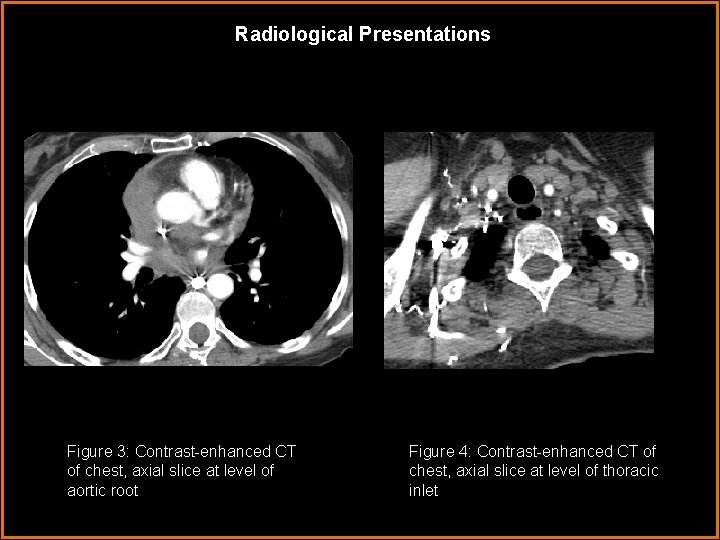
Radiological Presentations Figure 1: Contrast-enhanced CT of chest, axial slice at level of left atrium Figure 2: CT reformat in coronal plane
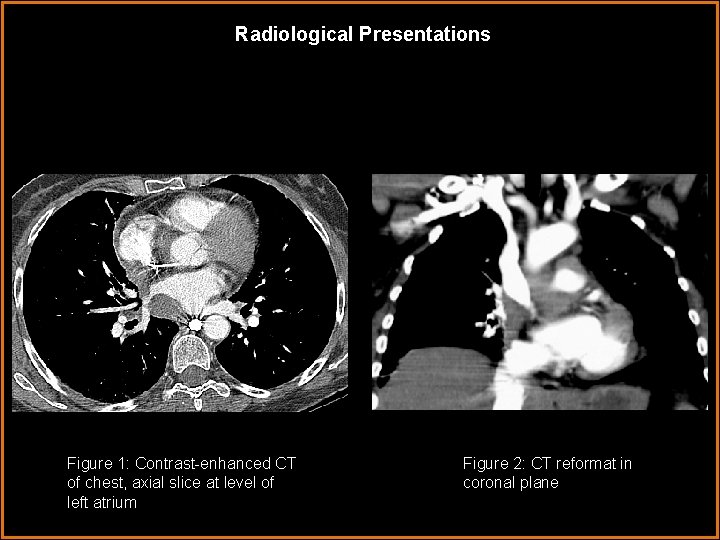
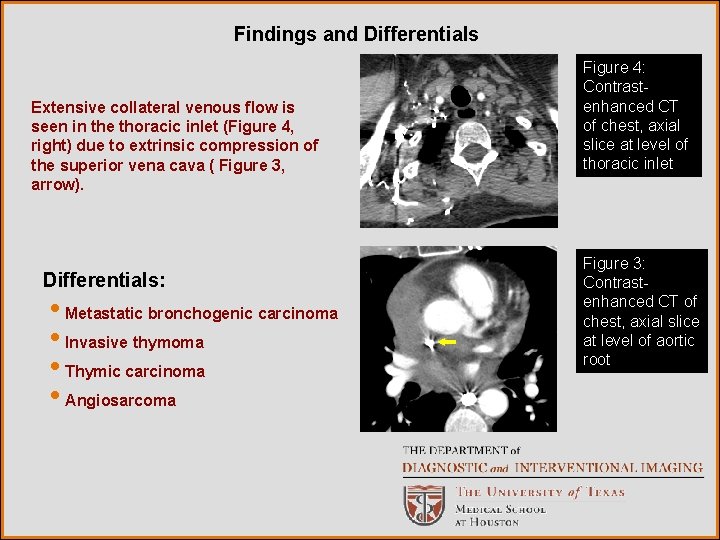
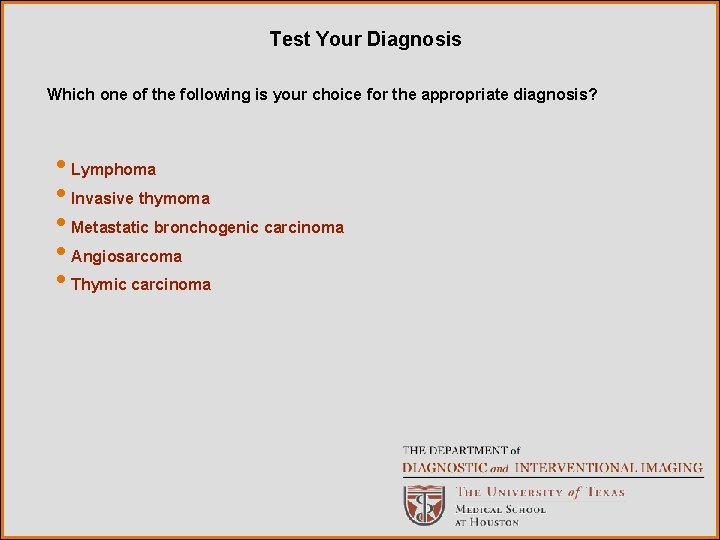
Radiological Presentations Figure 3: Contrast-enhanced CT of chest, axial slice at level of aortic root Figure 4: Contrast-enhanced CT of chest, axial slice at level of thoracic inlet
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? • Lymphoma • Invasive thymoma • Metastatic bronchogenic carcinoma • Angiosarcoma • Thymic carcinoma
Findings and Differentials There is nodular soft tissue thickening of the pericardium with which fills the pericardial recesses and extends along both right and left cardiac borders and encases the inferior pulmonary veins (solid arrows, Figure 1 and 2 ). There is no intracardiac extension. There is also a soft tissue thickening in the anterior mediastinum (broken arrow, Figure 2) which may represent spread of pericardial disease into the anterior mediastinum, indicating a possible relation to the thymus. Figure 1: Contrastenhanced CT of chest, axial slice at level of left atrium Figure 2: CT reformat in coronal plane
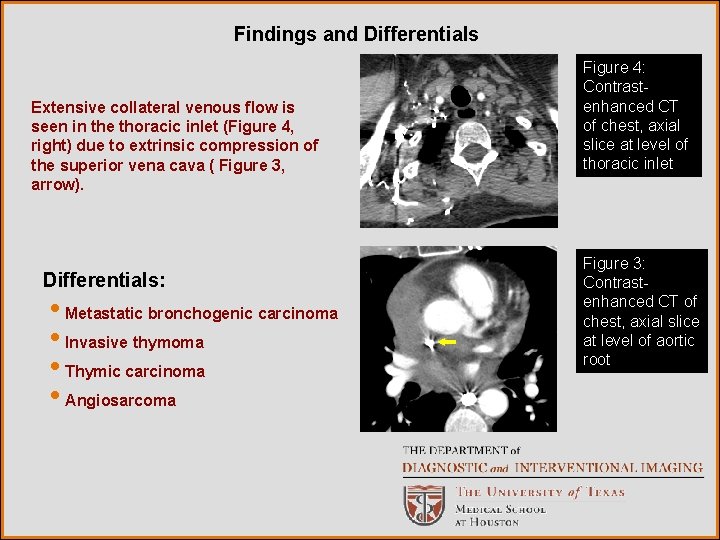
Findings and Differentials Extensive collateral venous flow is seen in the thoracic inlet (Figure 4, right) due to extrinsic compression of the superior vena cava ( Figure 3, arrow). Differentials: • Metastatic bronchogenic carcinoma • Invasive thymoma • Thymic carcinoma • Angiosarcoma Figure 4: Contrastenhanced CT of chest, axial slice at level of thoracic inlet Figure 3: Contrastenhanced CT of chest, axial slice at level of aortic root
Discussion Cardiac neoplasms can be primary or secondary involving the heart muscle or pericardium. Of the malignant primary cardiac tumors, angiosarcomas and leiomyosarcoma are the most common. Myxomas, the most common primary benign tumor, typically occur in the left atrium and are solitary. Angiosarcomas are highly vascular tumors and frequently appear as a right atrial mass with accompanying hemopericardium. They often invade the pericardium resulting in hemorrhagic effusions sometimes leading to tamponade. They can also result in tumor emboli in the pulmonary vessels precipitating a progressive right sided heart failure 1, 2. On contrast CT, these masses are heterogeneous, irregular and hypodense. On MR T 1 WI and T 2 WI, angiosarcomas are bright hemorrhagic nodular areas against a background of intermediate intense heterogeneity creating and appearance likened to a cauliflower. Noncardiac tumors may invade the heart and pericardium by lymphangitic spread, hemotogenous dissemination, local extension or transvenous routes. Pericardial metastases occur late in the course of a neoplasm, usually as recurrent disease. Lung cancer, the most frequent cause of pericardial malignancy, accounts for 1/3 cases. Bronchogenic carcinoma may involve the heart and pericardium by direct extension or by a combination of lymphatic and hemotogenous dissemination. Breast cancer and lymphoma/leukemia are the second and third most common sources respectively. However, cardiac or pericardial locations are rarely the first site of malignant disease and the patient typically also has metastatic disease at other sites 3.
Discussion Thymic neoplasms include thymomas, thyroid carcinoma, thymic hyperplasia, neuroendocrine tumors and thymic cysts. Both benign and malignant mediastinal tumors produce local effects compressing the airway, esophagus and, as in this case, the right heart and great vessels. Thymoma is the most common primary neoplasm of the anterior mediastinum and the most common tumor of the thymus. There are many classifications in the literature based on histologic and immunophenotypic resemblance to cortical or medullary areas of the thymus. However, the most benign thymoma (WHO type A, medullary) - while solid and encapsulated and lacking the malignant histological features of malignancy - can still invade the adjacent mediastinal fat, pleura, pericardium, great vessels, heart. Therefore, they are referred to as invasive but not malignant. Although they are usually found in the anterior mediastinum, thymomas can be located anywhere from the neck to the cardiophrenic angle and less commonly in other mediastinal compartments. They are associated with paraneoplastic syndromes such as myasthenia gravis, red blood cell aplasia, and hypogammoglobunemia. Thirty to fifty percent of patients with thymoma develop MG but only 15% of patients with MG have thymoma.
Discussion In thymomas, chest radiographs demonstrate a mass in the anterior mediastinum in 45 -80% of patients. CT is more definitive in the diagnosis of thymoma, in which they are typically well-defined, spherical, oval, or lobulated homogeneous soft tissue masses that enhance post contrast. They can also present with heterogeneous areas of low attenuation secondary to hemorrhage, necrosis, or cyst formation. Capsular invasion is suggested by irregular interface with adjacent lung, irregular tumor margins, midline crossing, encroachment of vascular structures, and encasement of mediastinal structures. Pleural effusion is uncommon. MRI signal is similar to normal thymus (intermediate, higher than skeletal muscle on T 1 WI and high signal approaching fat on T 2 WI) yet it can appear heterogeneous after gadolinium administration as a result off hemorrhage, necrosis, and cystic degneration 5. Thymic carcinomas are malignant epithelial tumor with loss of organ-typical features and cytologic atypia. A highly aggressive tumor, it has a tendency towards metastases to regional lymph nodes, distant sites (lung, bone, liver, brain) in addition to local invasion. It is rarely associated with paraneoplastic syndromes like MG. Radiological evaluation of thymic carcinomas may show a large poorly defined anterior mediastinal mass associated with intrathoracic adenopathy, vascular invasion and pleural or pericardial effusions. MRI findings are similar to thymoma.
Discussion On CT, the thymic carcinoma may appear to have more irregular margins than thymoma. They may also show areas of low attenuation secondary to necrosis, hemorrhage or cystic degeneration or curvilinear and punctate calcifications like some thymomas. Therefore, imaging cannot distinguish definitively between thymoma and thymic carcinoma 6. This patient had a biopsy of the pericardial masses performed at an outside referring facility and pathology examination (not available) confirmed a low grade epithelial neoplasm consistent with thymoma. This prompted reexamination of the patient’s first chest x-ray for any evidence of an anterior mediastinal mass that was present when the patient was first diagnosed with myasthenia gravis. No mass was detected on chest x-ray and the patient did not have a CT at that time. When the patient presented to our facility, the tumor was considered unresectable and the patient was referred for chemotherapy. The patient did not undergo MRI because surgical intervention was not being considered. The CT reformatted images in the coronal planes provided excellent depiction of the extent of tumor extension within the pericardial recesses. Because of its more superior contrast resolution, MRI allows more accurate tissue characterization and facilitates distinction between tumor, thrombus and blood flow artifact 3.
Diagnosis Intrapericardial thymoma (low grade epithelial type)
References 1. 2. 3. 4. 5. 6. Schwartzman PR, White RD. Imaging of cardiac and paracardiac masses. J Thorac Imaging. 2000; 15(4) 265 -73. Restrepo CS, Largoza A, Lemos DF, et al. CT and MR imaging findings of malignant cardiac tumors. Current Problems in Diagnostic Radiology. 2005; 34(1): 1 -11. Chiles C, Woodard PK, Gutierrez FR, Link KM. Metastatic involvement of the heart and pericardium: CT and MR imaging. Radiographics 2001; 21: 439449. Warren MH. Malignancies involving the pericardium. Sem Thor Cardiovasc Surg. 2000; 12(2)119 -29. Restrepo CS, Pandit M, Rojas IC, et al. Image findings of expansile lesions of the thymus. Curr Probl Diagn Radiol. 2005; : 22 -34. Strollo DC, Rosado-de-Christensen ML, Jett JR. Primary mediastinal tumors. Part 1 : tumors of anterior mediastinum. Chest 1997; 112: 511 -22