Radiological Category Thoracic Chest Principal Modality 1 General
- Slides: 21
Radiological Category: Thoracic Chest Principal Modality (1): General Radiography Principal Modality (2): Fluoroscopy Case Report #0485 Submitted by: Malisa Lester, M. D. Faculty reviewer: Chitra Chandrasekhar, M. D. Date accepted: 14 March 2008
Case History 46 year old male presents to the ER with chest pain.
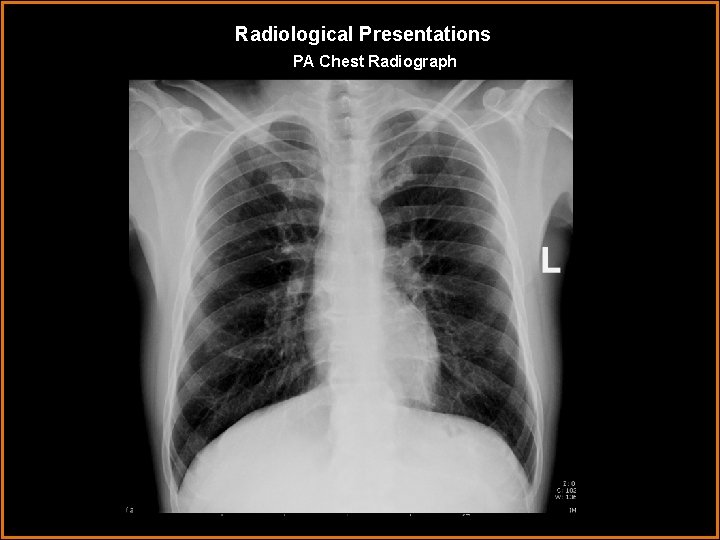
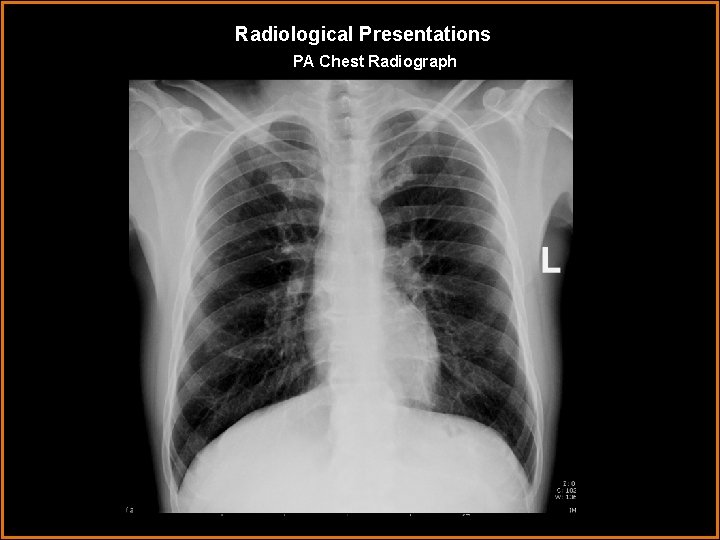
Radiological Presentations PA Chest Radiograph
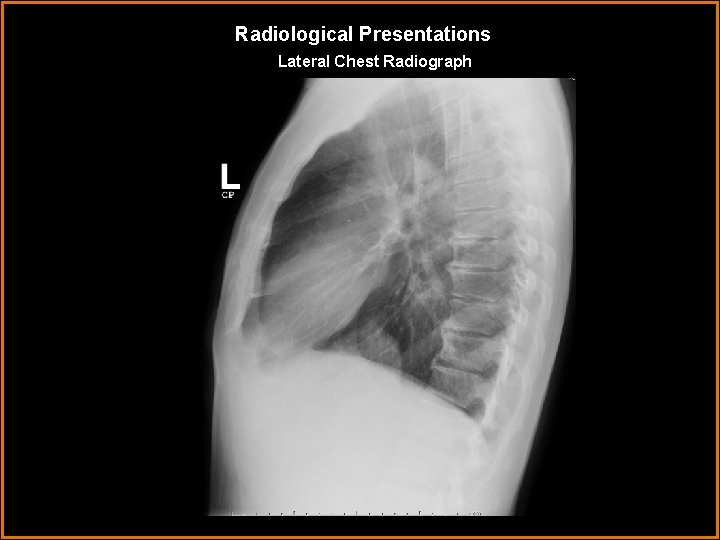
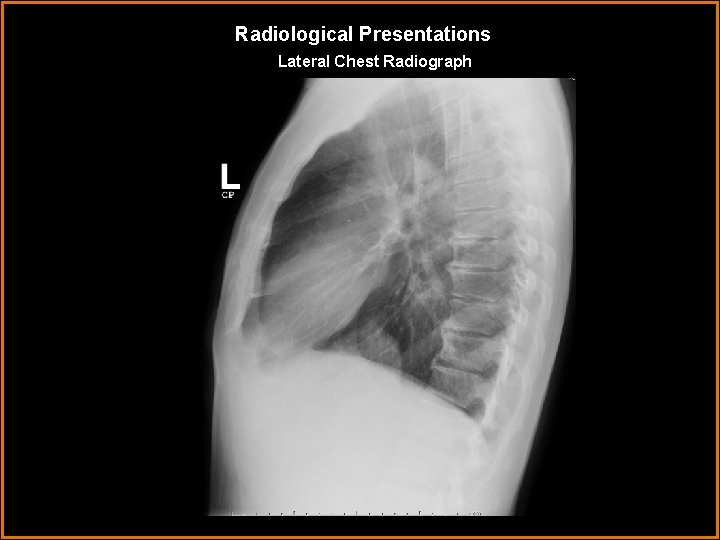
Radiological Presentations Lateral Chest Radiograph
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Hiatal hernia • Pericardial cyst • GI tract duplication cyst • Lymphadenopathy • Neurenteric cyst • Bochdalek hernia • Bronchogenic cyst • Aortic aneurysm • Lymphoma
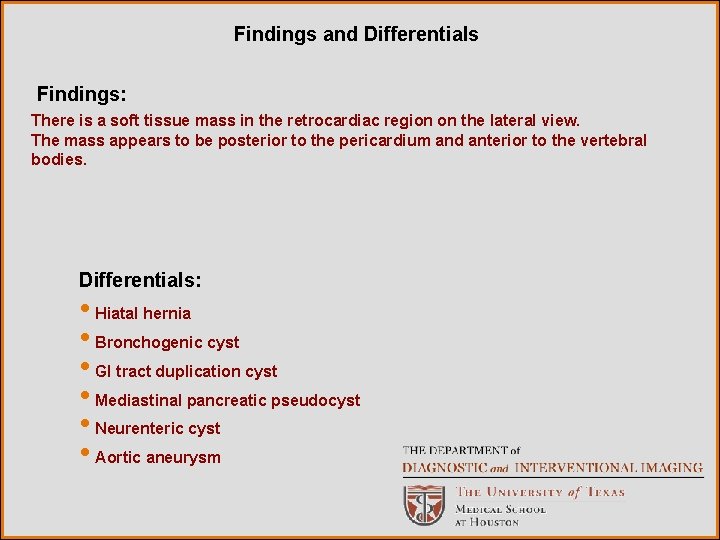
Findings and Differentials Findings: There is a soft tissue mass in the retrocardiac region on the lateral view. The mass appears to be posterior to the pericardium and anterior to the vertebral bodies. Differentials: • Hiatal hernia • Bronchogenic cyst • GI tract duplication cyst • Mediastinal pancreatic pseudocyst • Neurenteric cyst • Aortic aneurysm
Discussion The most probable location for the mass based on the lateral chest radiograph is within the posterior mediastinum according to the modified Fraser and Pare classification system, which defines the boundaries of the posterior mediastinum as “the posterior margins of the pericardium and great vessels anteriorly and the thoracic vertebral bodies posteriorly”. According to this classification system, normal structures within the posterior mediastium include the descending thoracic aorta, esophagus, thoracic duct, axygous/hemiazygous, autonomic nerves, lymph nodes, and fat. This helps narrow the differential diagnosis to “posterior mediastinal masses”, including: • neurogenic tumors • esophageal lesions • vascular lesions • foregut cysts • adenopathy • mediastinal pancreatic pseudocyst • paravertebral lesions.
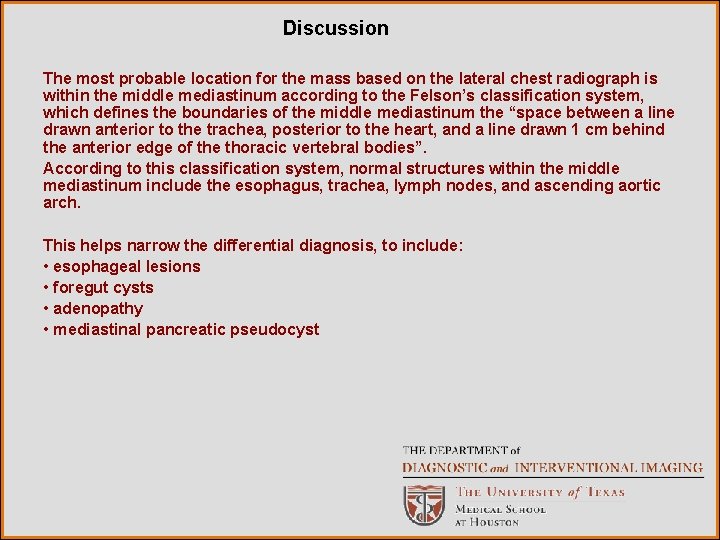
Discussion The most probable location for the mass based on the lateral chest radiograph is within the middle mediastinum according to the Felson’s classification system, which defines the boundaries of the middle mediastinum the “space between a line drawn anterior to the trachea, posterior to the heart, and a line drawn 1 cm behind the anterior edge of the thoracic vertebral bodies”. According to this classification system, normal structures within the middle mediastinum include the esophagus, trachea, lymph nodes, and ascending aortic arch. This helps narrow the differential diagnosis, to include: • esophageal lesions • foregut cysts • adenopathy • mediastinal pancreatic pseudocyst
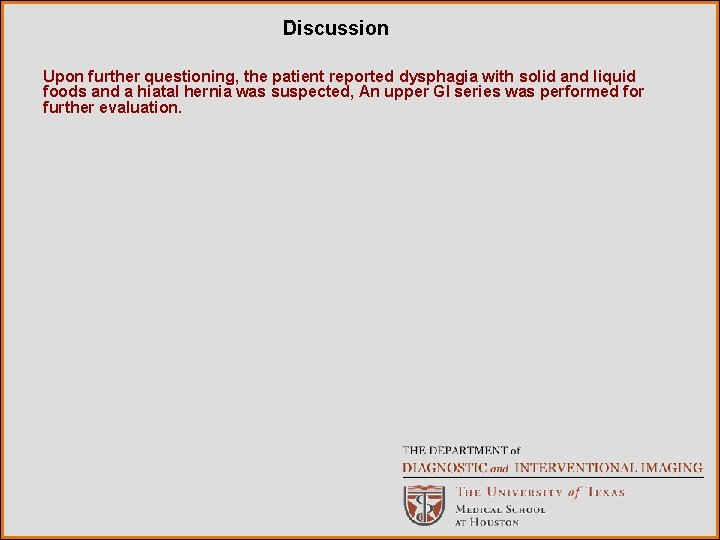
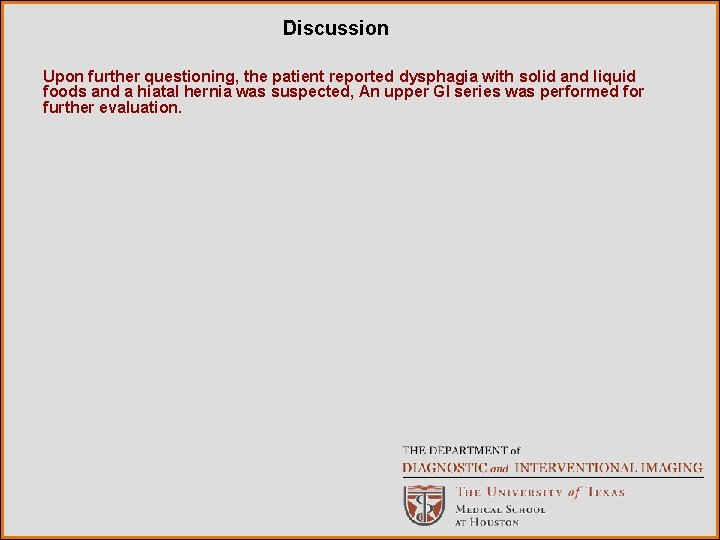
Discussion Upon further questioning, the patient reported dysphagia with solid and liquid foods and a hiatal hernia was suspected, An upper GI series was performed for further evaluation.
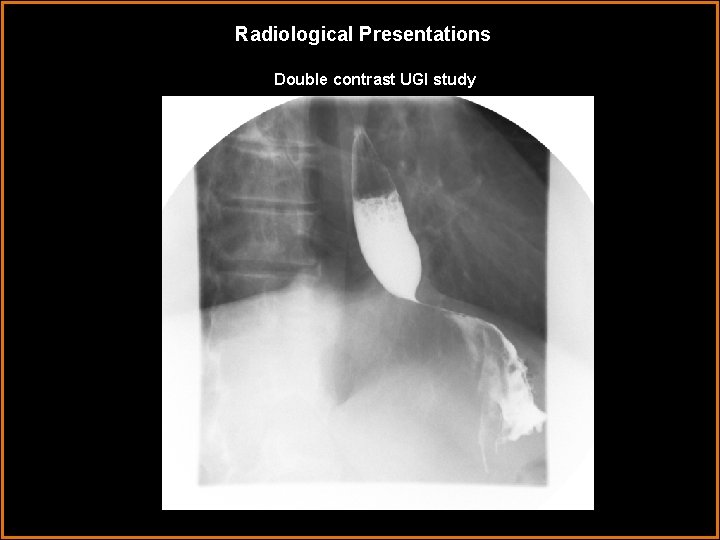
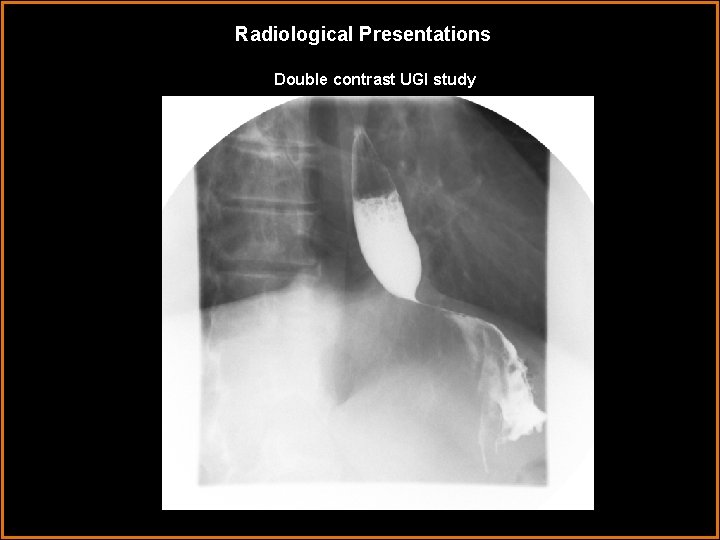
Radiological Presentations Double contrast UGI study
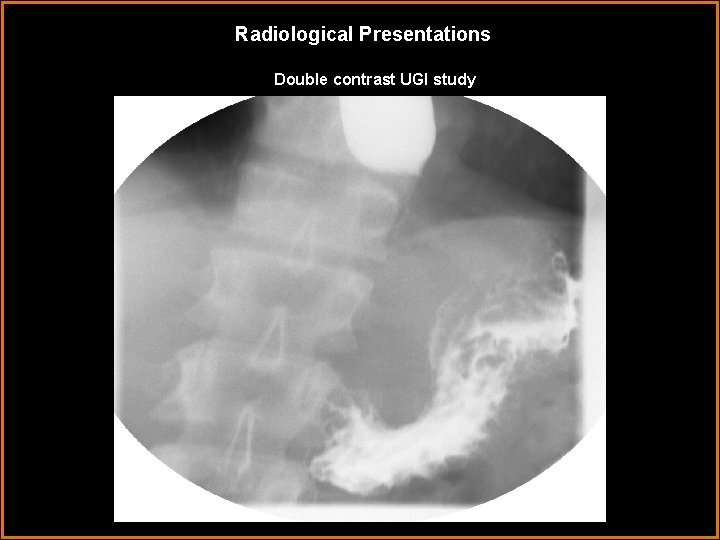
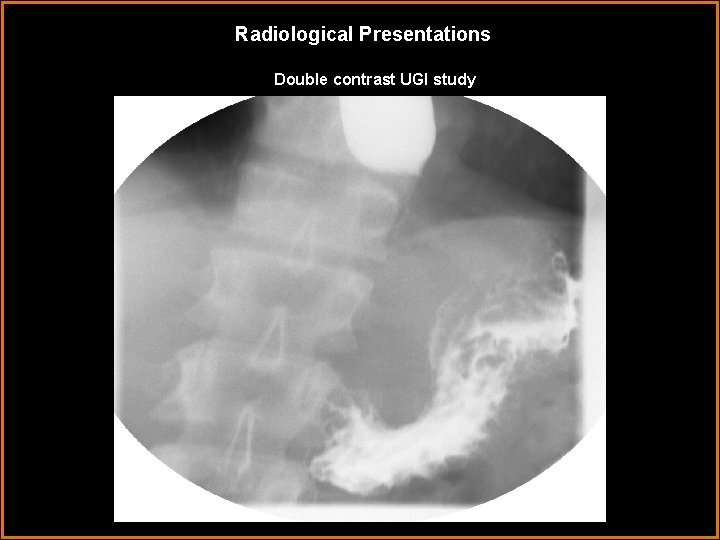
Radiological Presentations Double contrast UGI study
Discussion No hiatal hernia is demonstrated on the upper GI series. Near complete obstruction of the gastroesophageal junction by what appeared to be an extrinsic mass compressing the gastric fundus and the GE junction was demonstrated, indicating that the mass was both within the mediastinum and abdomen. Further clinical evaluation revealed a history of pancreatitis and small pancreatic pseudocyst. A CT of the abdomen/pelvis was then performed.
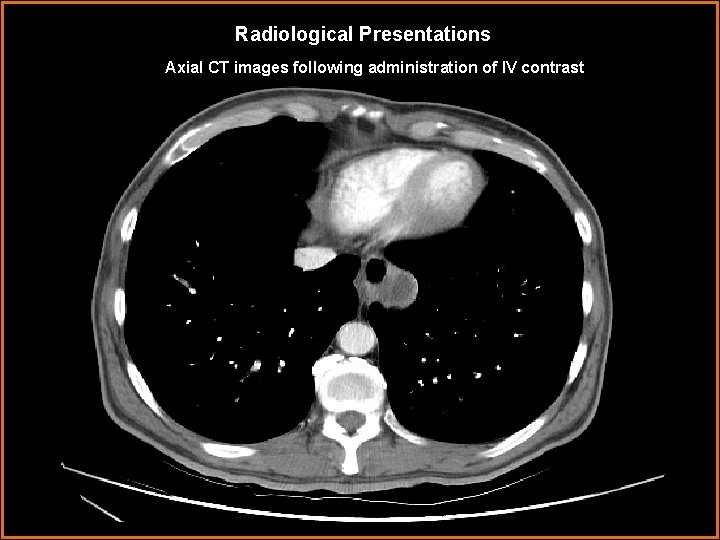
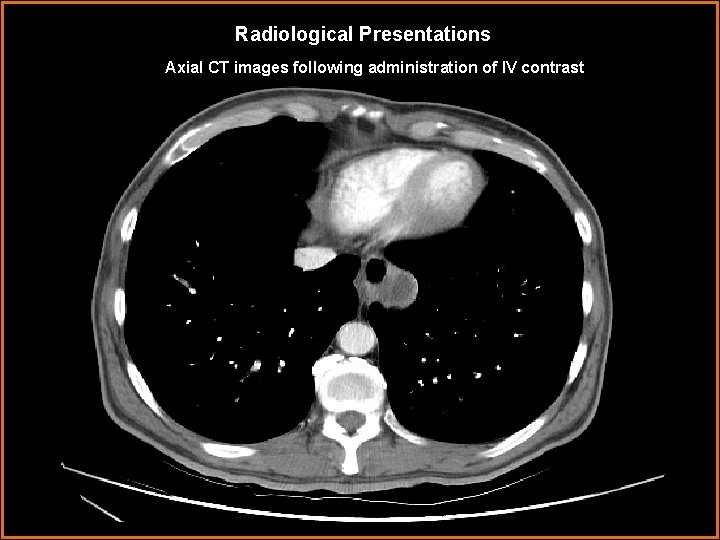
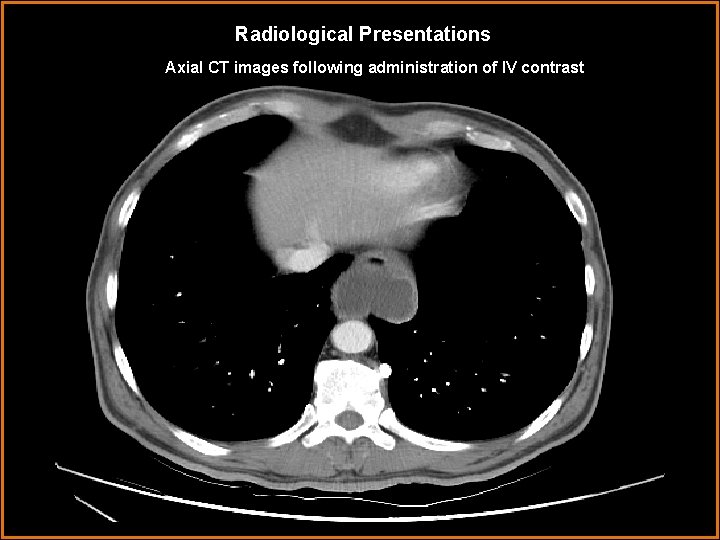
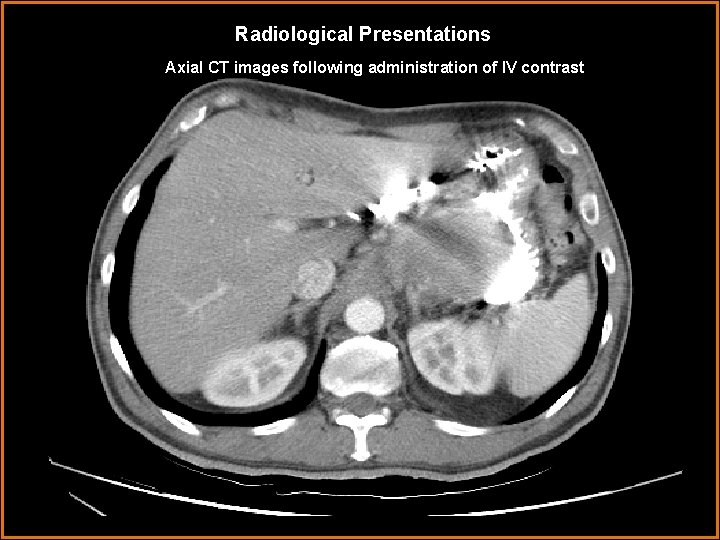
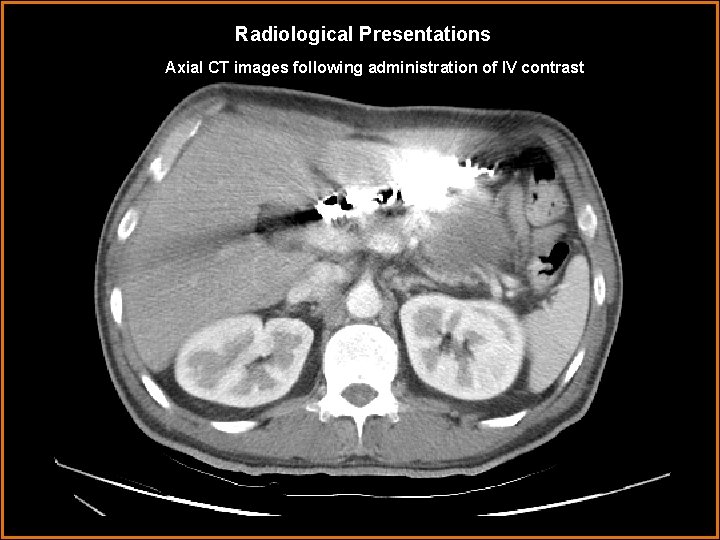
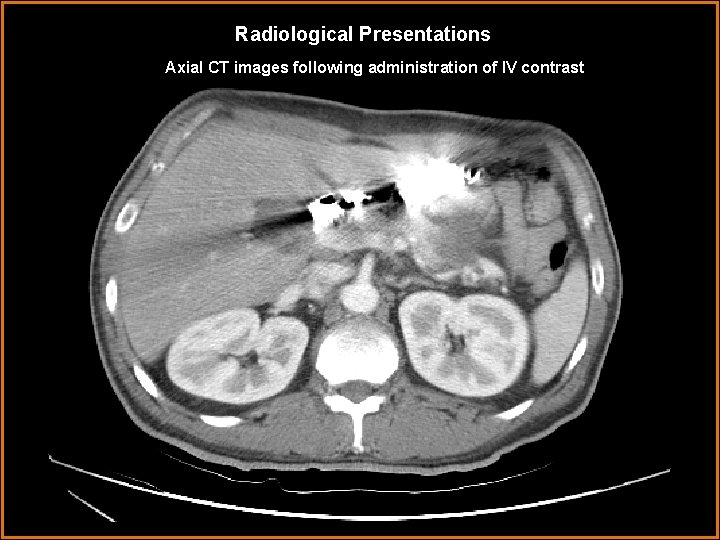
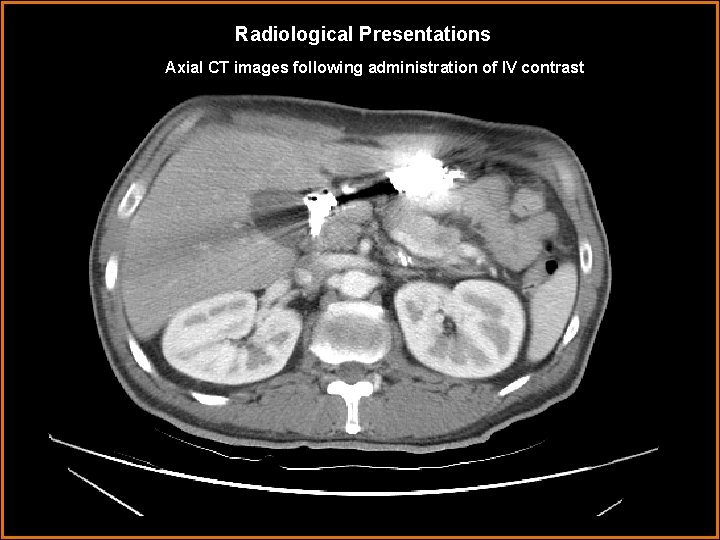
Radiological Presentations Axial CT images following administration of IV contrast
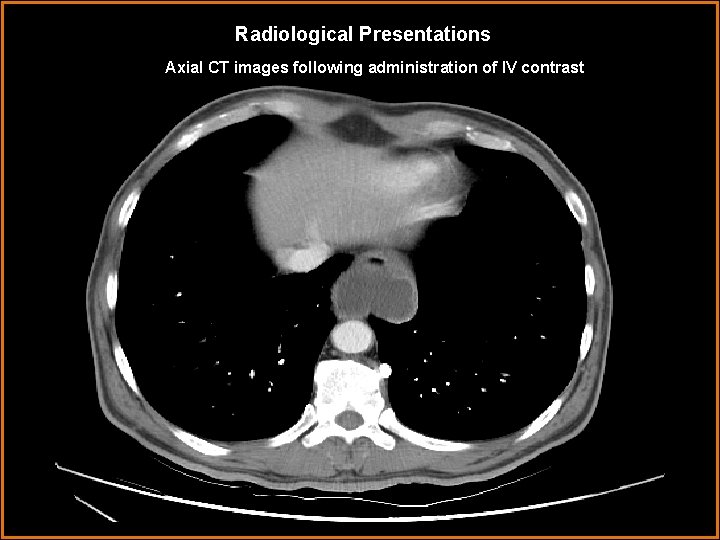
Radiological Presentations Axial CT images following administration of IV contrast
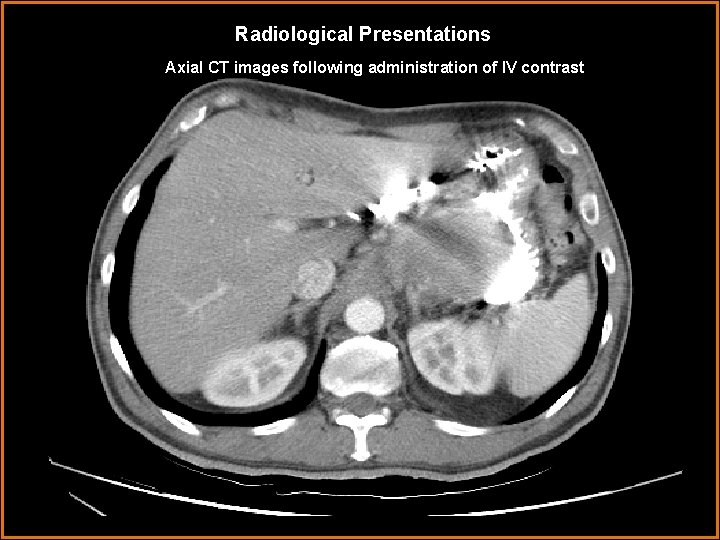
Radiological Presentations Axial CT images following administration of IV contrast
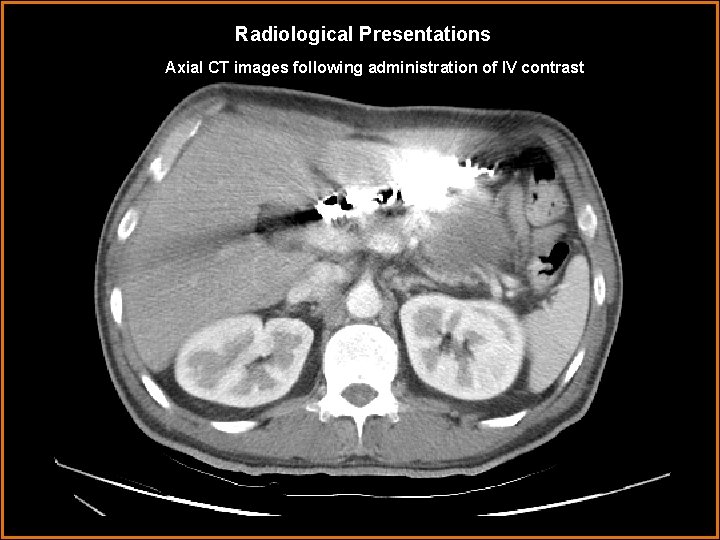
Radiological Presentations Axial CT images following administration of IV contrast
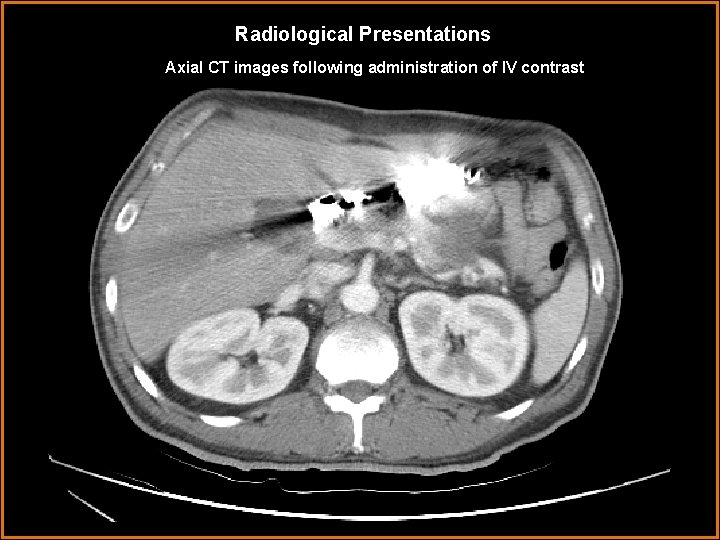
Radiological Presentations Axial CT images following administration of IV contrast
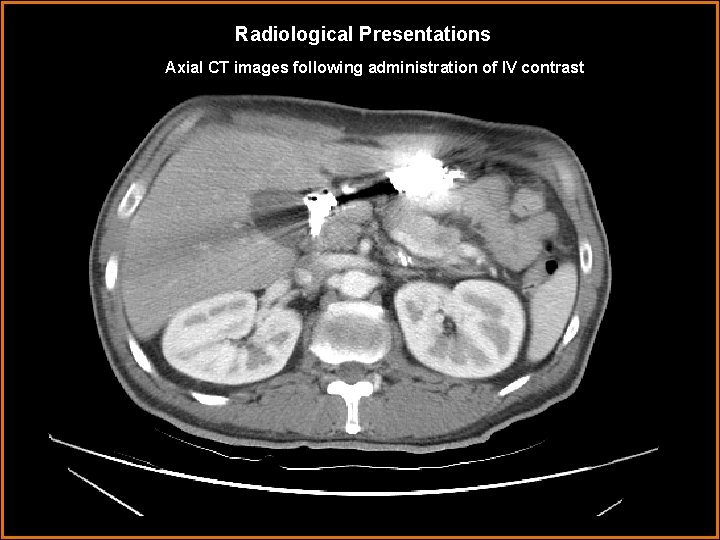
Radiological Presentations Axial CT images following administration of IV contrast
Discussion The CT demonstrates a large fluid collection extending from the pancreatic tail, along the lesser curvature, to the GE junction and above the level of the diaphragm, causing obstruction at the GE junction, most compatible with a pancreatic pseudocyst. The hyperdense material within the GI tract is barium from the UGI study. A pancreatic pseudocyst is a collection of pancreatic secretions, blood, and cellular debris which organizes and develops a fibrous capsule. They can be located within the pancreatic parenchyma, or outside of it, and are most commonly found within the lesser sac. The incidence of pancreatic pseudocysts is greater in patients with chronic pancreatitis versus acute. A pancreatic pseudocyst with mediastinal extension is a relatively rare entity with only approximately 50 cases reported in the literature. An enlarging pseudocyst dissects along the planes of least resistance, and can enter the mediastinum through the esophageal or aortic hiatus. Other less common routes of entrance include the foramen of Morgagni, the inferior vena cava hiatus, and direct penetration of the diaphragm. Once inside the mediastinum, pancreatic pseudocysts may rupture into the pleural space to produce an effusion or may extend superiorly into the neck. Patients with mediastinal pancreatic pseudocysts may complain of back pain, dysphagia, gastroesophageal reflux, or be asymptomatic. Management of pancreatic pseudocysts can include medical, endosurgical, and surgical interventions, however is typically conservative initially.
Diagnosis Mediastinal extension of a pancreatic pseudocyst.
References Goodman, Lawrence R. Felson’s principles of chest roentgenology, a programmed text, 2 nd Ed. Philadelphia. Saunders. 1999. Mc. Loud, Theresa C. Thoracic radiology: the requisites. St. Louis. Mosby. 1998. Sadat, Umar et al. Mediastinal extension of a complicated pancreatic pseudocyst; a case report and literature review. Journal of Medical Case Reports. 2007; 1: 12 -14.