Radiological Category Thoracic Chest Principal Modality 1 General
- Slides: 10
Radiological Category: Thoracic Chest Principal Modality (1): General Radiography Principal Modality (2): CT Case Report #0262 Submitted by: Gustav Blomquist, M. D. Faculty reviewer: Emma Ferguson, M. D. Date accepted: 01 January 2006
Case History 34 year old white male with shortness of breath presents to the Emergency Room.
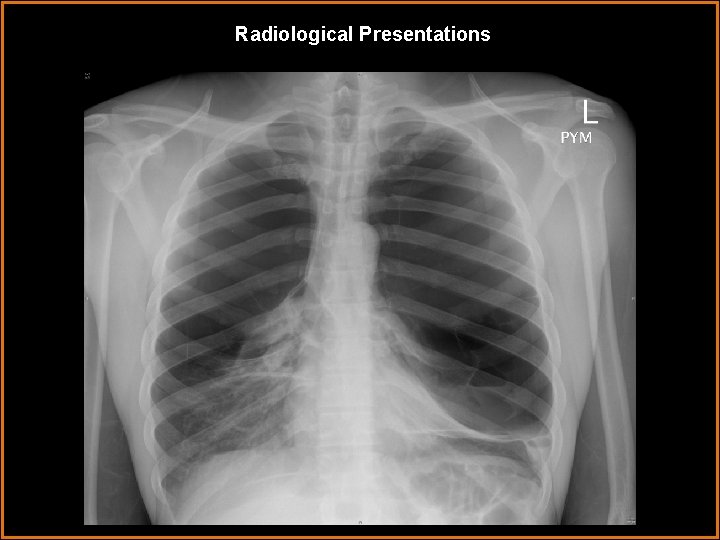
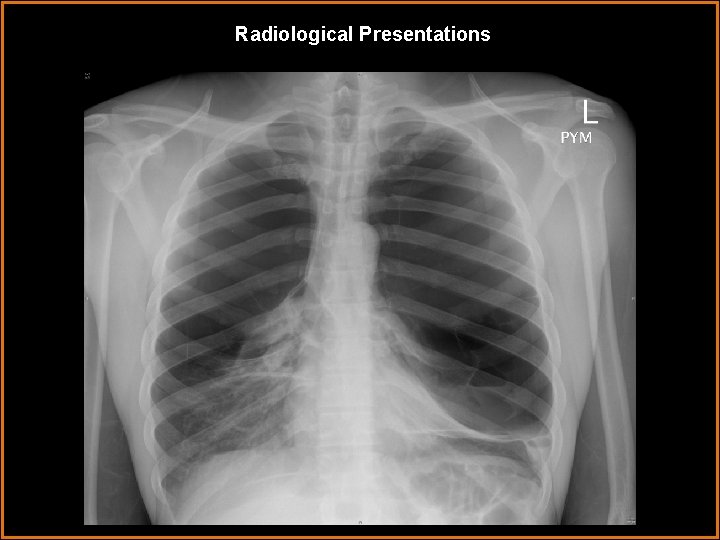
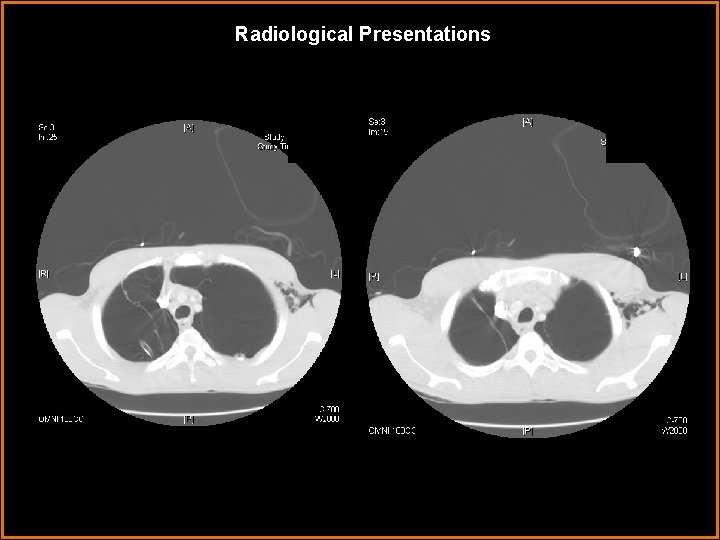
Radiological Presentations
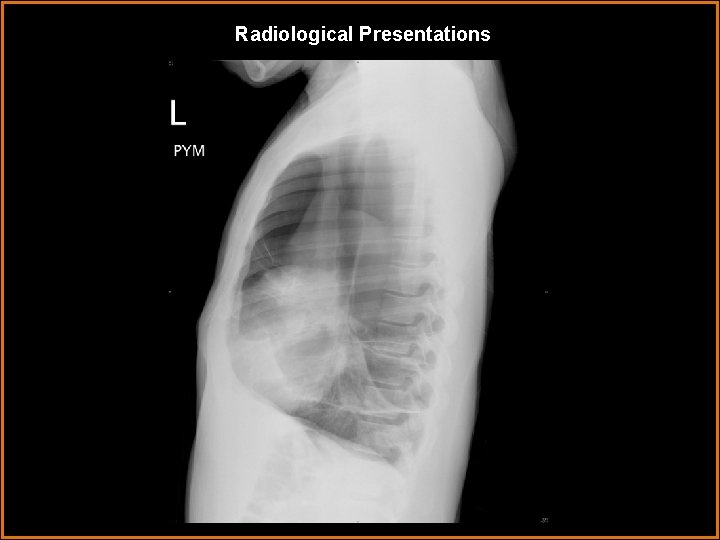
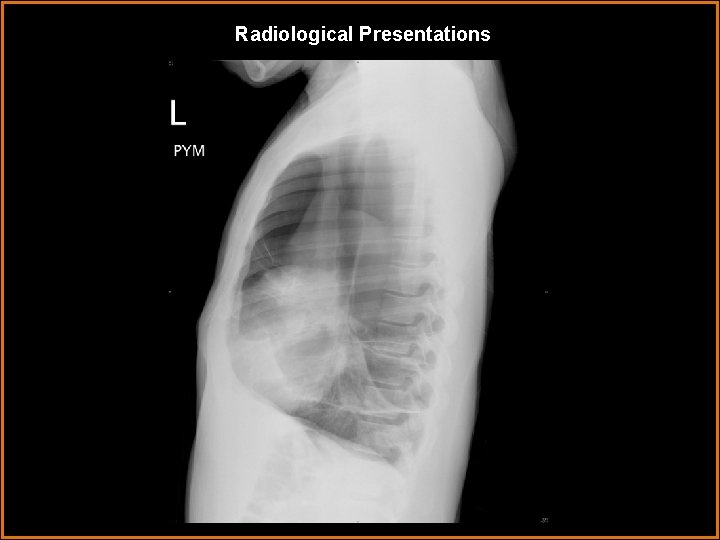
Radiological Presentations
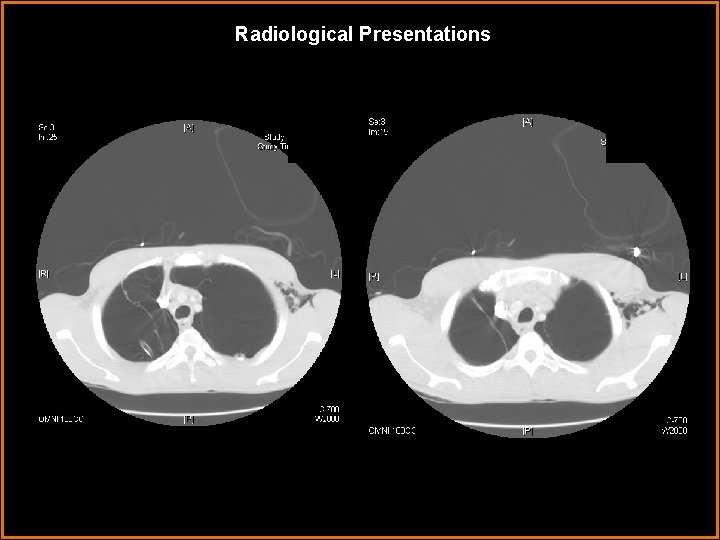
Radiological Presentations
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Bilateral Vanishing Lung • Bilateral Pneumothoraces • Atelectasis • Smithbauer-Loffler’s Syndrome • Pulmonary Atresia
Findings and Differentials Findings: CR: Increased lucenies in the top and middle thirds of the thorax with thin curved linear opacities running through the hemithoraces outlining cysts. No mediastinal shift. Bilateral crowding of vascular markings at the lung bases from atelectatic lung. CT: Linear lucenies in the lungs are thin curved opacities outlining giant cysts/bulla. No mediastinal shift. Evidence of bilateral pneumothoraces with bilateral chest tubes. Differentials: • Bilateral Vanishing Lung • Bilateral Pneumothoraces • Atelectasis
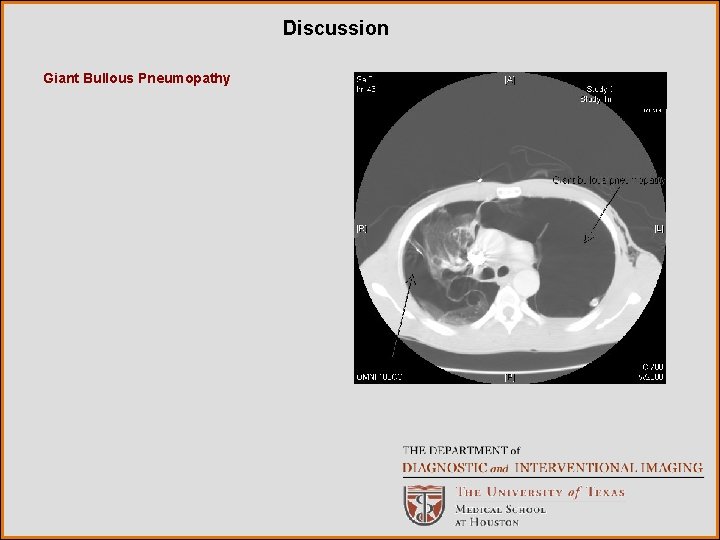
Discussion Giant bullous lung disease is an uncommon cause of respiratory distress. In patients with severe emphysema, discrete emphysematous bullae have been shown to functionally impair pulmonary mechanics and result in diminished exercise capacity and even acute respiratory distress. Most patients with bullae have a significant cigarette smoking history, although cocaine smoking, pulmonary sarcoidosis, 1 -antitrypsin deficiency, 1 -antichymotrypsin deficiency, Marfan’s syndrome, Ehlers-Danlos syndrome and inhaled fiberglass exposure have been shown to be associated with emphysematous lung bullae. Bullae which enlarge enough to compress adjacent lung tissue are best diagnosed by CT. A “double-wall sign” on chest CT, demonstrating air on both sides of the bulla wall, signifies an associated pneumothorax with the bulla. In addition to chest CT, these patients should undergo ABGs and PFTs, The decision to operate is often a challenging one. Patients should undergo surgical resection when they have incapacitating dyspnea with large bullae that fill more than 30% of the hemithorax and result in the compression of healthy adjacent lung tissue. In addition, operation is indicated for patients who have complications related to bullous disease such as infection or pneumothorax. There are two surgical approaches for resecting giant lung bullae. Stapling resection of the entire bulla, either through a VATS or open approach, is the most common technique. Pericardial strips can be used along the staple line to assist in control of air leaks since the surrounding lung tissue is often diseased. Another operative approach is the modified Monaldi technique, which involves opening the bulla, placing a purse-string suture at the neck of the bulla and closing the overlying bulluous sac with a running back-and-forth plicating stitch. Both techniques have been shown to be effective. Smoking cessation and aggressive pulmonary rehabilitation are also important for successful treatment of patients with bullous lung disease.
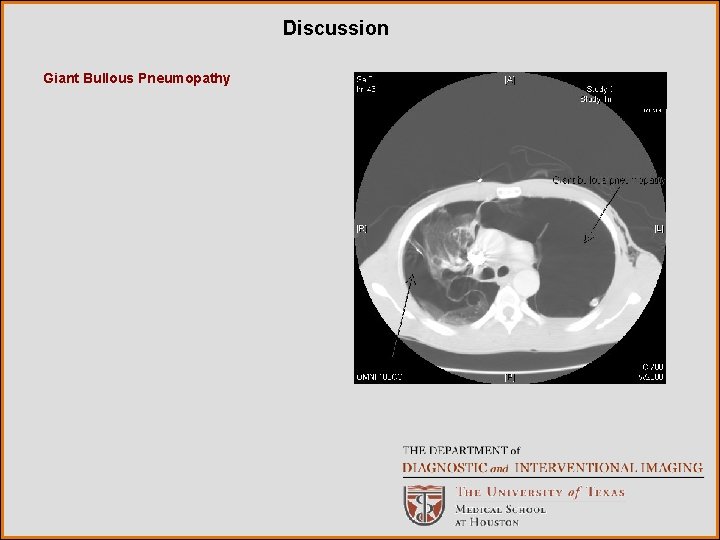
Discussion Giant Bullous Pneumopathy
Bibliography • • • http: //www. ctsnet. org/sections/clinicalresources/clinicalcases/article-1. html Greenberg JA, Singhal S, Kaiser LR. Giant bullous lung disease: evaluation, selection, techniques, and outcomes. Chest Surg Clin N Am 2003; 13: 631 -49. Van der Klooster JM, Grootendorst AF. Severe bullous emphysema associated with cocaine smoking. Thorax 2001; 56: 982 -3. Zar HJ, Cole RP. Bullous emphysema occurring in pulmonary sarcoidosis. Respiration 1995; 62: 290 -3. Vigneswaran WT, Townsend ER, Fountain SW. Surgery for bullous disease of the lung. Eur J Cardiothorac Surg 1992; 6: 427 -30. De Giacomo T, Rendina EA, Venuta F, et al. Bullectomy is comparable to lung volume reduction in patients with end-stage emphysema. Eur J Cardiothorac Surg 2002; 22: 35762. Waitches GM, Stern EJ, Dubinsky TJ. Usefulness of the double-wall sign in detecting pneumothorax in patients with giant bullous emphysema. Am J Roentgenol 2000; 174: 1765 -8. Snider GL. Reduction pneumoplasty for giant bullous emphysema. Implications for surgical treatment of nonbullous emphysema. Chest. 1996; 109: 540 -8. Shah SS, Goldstraw P. Surgical treatment of bullous emphysema: experience with the Brompton technique. Ann Thorac Surg 1994; 58: 1452 -6.