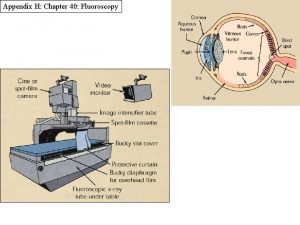
Radiological Category Gastrointestinal Principal Modality 1 Fluoroscopy Principal
- Slides: 15
Radiological Category: Gastrointestinal Principal Modality (1): Fluoroscopy Principal Modality (2): CT Case Report #0616 Submitted by: Miguel Fabrega, M. D. Faculty reviewer: Verghese George, M. D. Date accepted: 14 April 2009
Case History 35 year old woman with history of AIDS, complaining of dysphagia, odynophagia and progressive cough for 2 weeks – presents for a flouroscopic upper GI study.
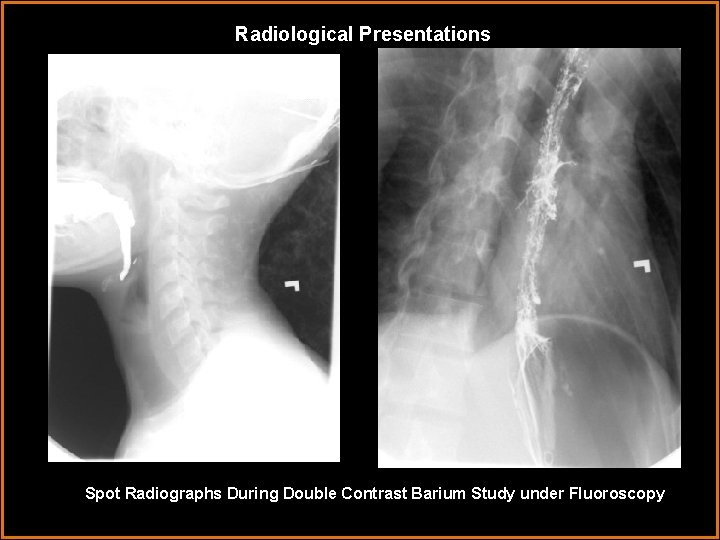
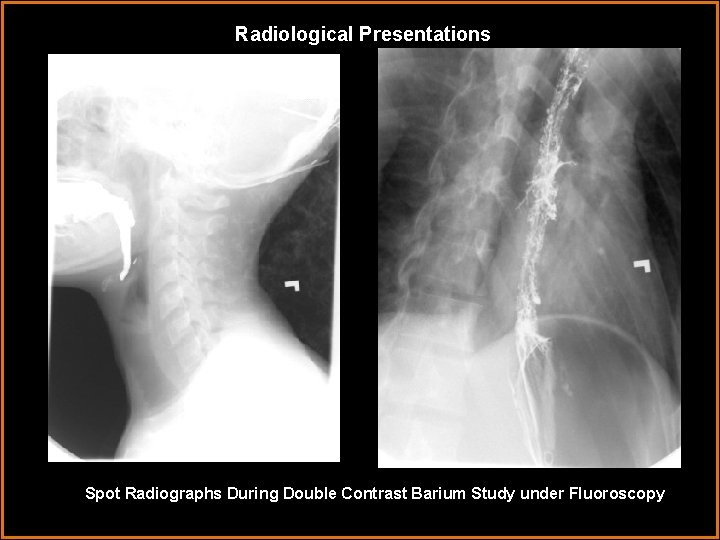
Radiological Presentations Spot Radiographs During Double Contrast Barium Study under Fluoroscopy
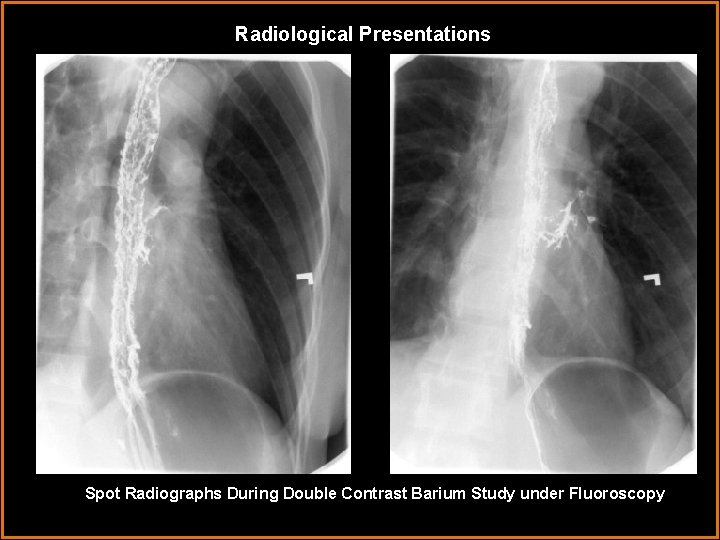
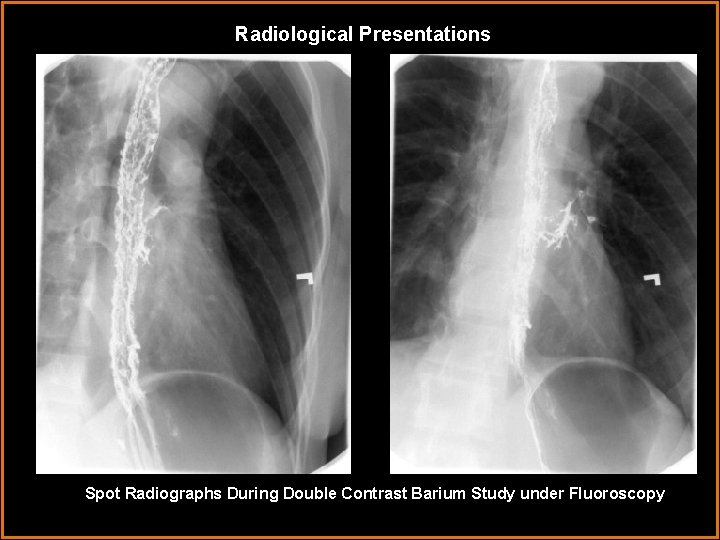
Radiological Presentations Spot Radiographs During Double Contrast Barium Study under Fluoroscopy
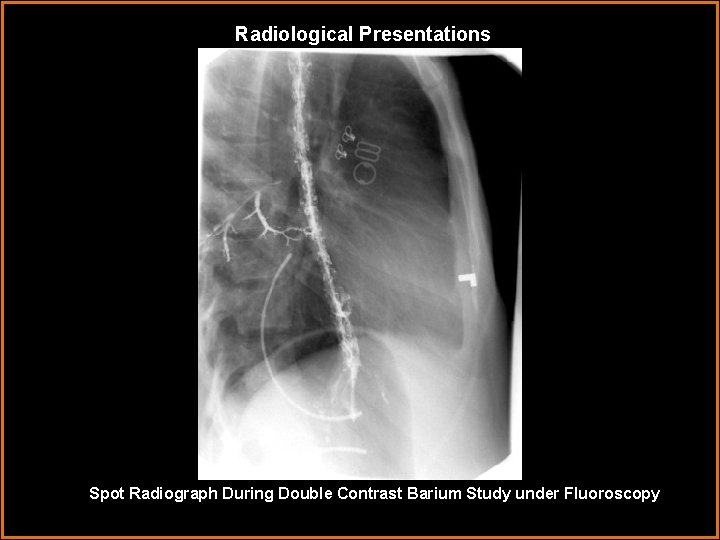
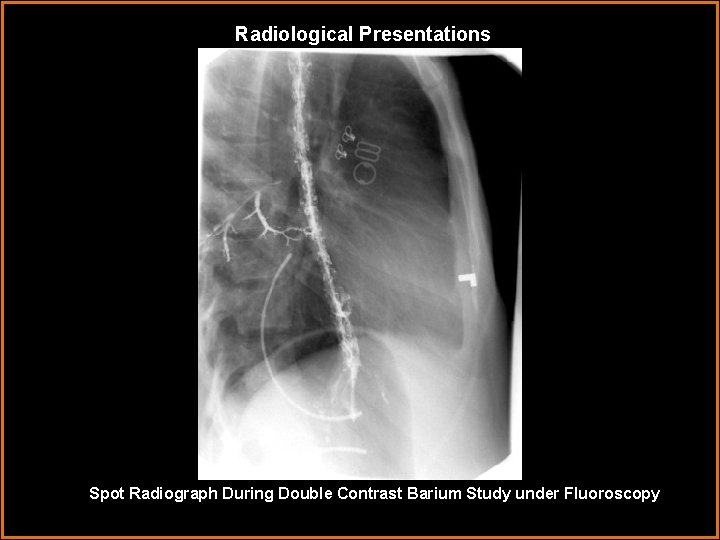
Radiological Presentations Spot Radiograph During Double Contrast Barium Study under Fluoroscopy
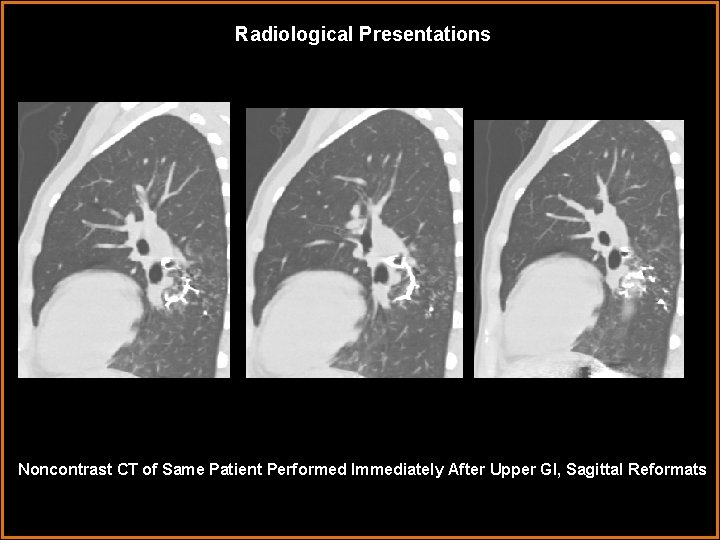
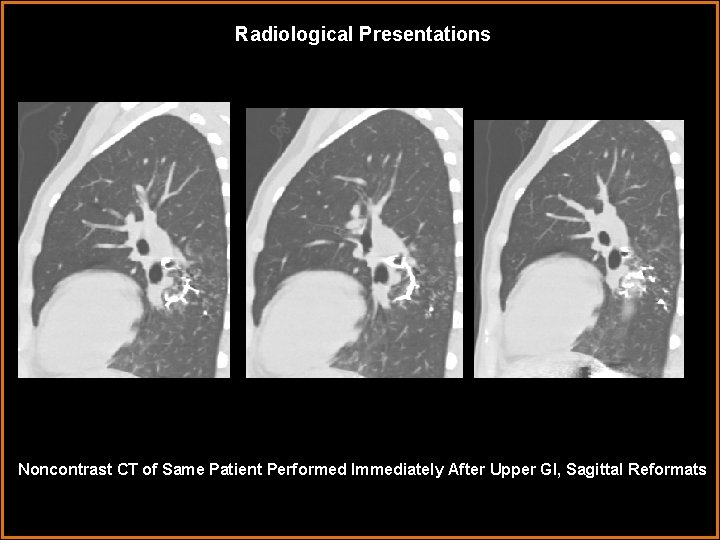
Radiological Presentations Noncontrast CT of Same Patient Performed Immediately After Upper GI, Sagittal Reformats
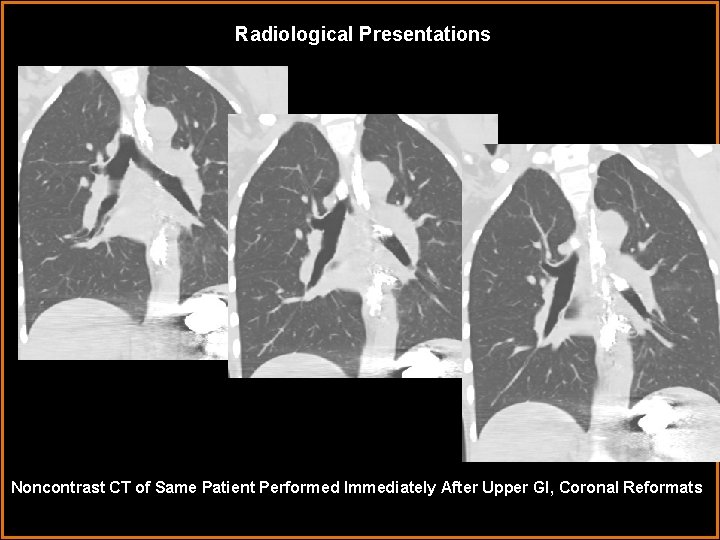
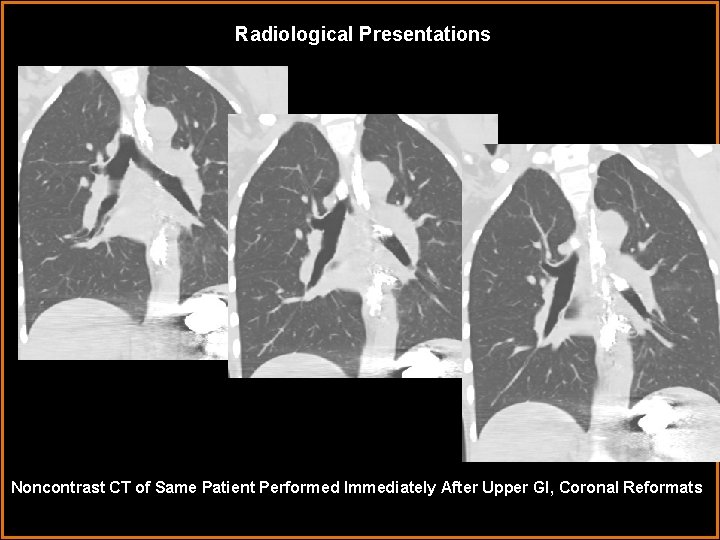
Radiological Presentations Noncontrast CT of Same Patient Performed Immediately After Upper GI, Coronal Reformats
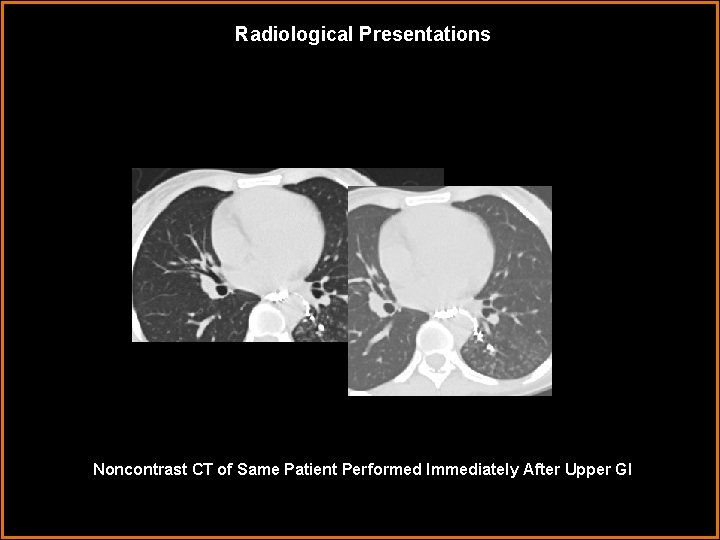
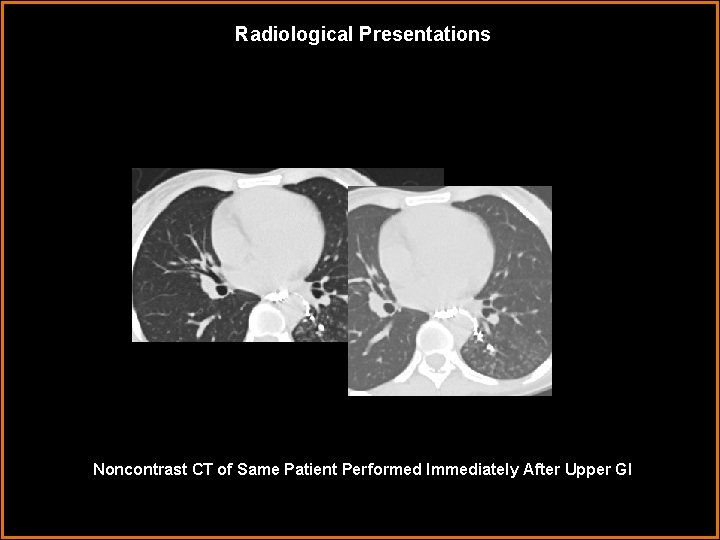
Radiological Presentations Noncontrast CT of Same Patient Performed Immediately After Upper GI
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Esophageal rupture • Esophageal varices with opacification of mediastinal veins • Squamous cell carcinoma of the esophagus with malignant fistula • Esophageal candidiasis with esophagobronchial fistula • Esophagovenous fistula • Aspiration of barium
Findings and Differentials Findings: - Diffuse ulceration of esophageal mucosa, as evidenced by its shaggy appearance - Opacified branching structure posterolateral to and communicating with esophagus (spot films) - Contrast within left main bronchus and segmental bronchi of the left lower lobe ( sagittal and coronal CT reformats) - Narrow tract of contrast between the esophagus and airway (axial CT) - Tree in bud opacities in left lower lobe of lung (axial CT) Differentials: • Esophageal candidiasis with esophagobronchial fistula • Esophageal candidiasis with esophagovenous fistula • Squamous cell carcinoma with associated fistula • Aspiration
Discussion Differential Diagnosis: -Aspiration: although this would explain the tree in bud opacities seen on CT, and may explain the barium seen in the bronchial tree on the upper GI and CT, it would not explain the fistulous tract between the esophagus and respiratory tract. -Esophageal malignancy with esophagobronchial fistula (EBF): although malignancy is the most common reason for non-congenital EBF, the appearance of the esophagus is not characteristic. Esophageal carcinoma appears as an annular stricture, polypoid intraluminal filling defects, or an ulcerated mass. The diffuse irregularity of mucosa seen here is more consistent with extensive ulcerations associated with esophagitis. -Esophageal candidiasis: the typical appearance of esophageal candidiasis, which is a relatively common complication in patients with AIDS, is that of discrete mucosal plaques that may become confluent and form a cobblestone pattern or shaggy esophageal border. The imaging description and clinical profile match those of this case.
Discussion Differential Diagnosis: Esophagial candidiasis (continued): Additional consideration into the nature of the fistula must also be made. The opaque branching structure seen under fluoroscopy may be venous, as a low pressure system may allow for intravasation and persistent visualization of contrast ( as opposed to arterial, where the contrast would be swiftly dissipated). However, a follow up non contrast CT performed immediately after the Upper GI study clearly shows contrast within the left main bronchus and segmental bronchi. This makes esophagovenous fistula and varices unlikely. Esophageal rupture is also unlikely as the only contrast not contained within the esophagus communicates with the bronchial tree. No free contrast is seen. (continued next slide)
Discussion Differential Diagnosis: Esophagobronchial fistula (EBF): non-congenital esophagobronchial fistulas are uncommon. When they do occur, they are most often in association with malignancy. Benign EBF is even rarer. The symptoms are not as severe as tracheoesophageal fistulas (which are much more common), and may present as an indolent cough, though it can progress to pulmonary sepsis. Surgical intervention is often needed when present. Benign EBF is usually associated with instrumentation, intubation, foreign bodies, or granulomatous infections. The radiographic findings in the current case are consistent with EBF. A fistulous tract is clearly opacified with barium and communicates between the esophagus and respiratory tract. Barium in the respiratory tract then forms a “bronchogram”, which was the initial observation under fluoroscopy that prompted the CT for further characterization. Furthermore, the “tree in bud” opacities are likely the result of an associated pneumonitis, localized only to the left lower lobe. In this patient, no malignancy is known or demonstrated radiographically. Benign EBF may have occurred due to prior EGD (concealed in history) or due to infection.
Diagnosis Esophageal candidiasis with benign esophagobronchial fistula and associated pneumonitis
References 1. Brant WE, Helms CA, eds. Fundamentals of Diagnostic Radiology. 3 rd Edition. PA: Lippincott Williams & Wilkins; 2000: 811 -812. 2. Pickhardt PJ, et al. Acquired Gastrointestinal Fistulas: Classification, Etiologies, and Imaging Evaluation. Radiology July 2002: 9 -23 3. Roberts Jr L, et al. Adult Esophageal Candidiasis: a radiographic spectrum. . Pneumomediastinum Revisited. Radio. Graphics 1987: volume 7: 289 -307
 Digital fluoroscopy vs conventional fluoroscopy
Digital fluoroscopy vs conventional fluoroscopy Erate category 1
Erate category 1 Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Carm fluoroscopy
Carm fluoroscopy Real time fluoroscopy
Real time fluoroscopy Aspurbi
Aspurbi Spot film device fluoroscopy
Spot film device fluoroscopy Metformin and constipation
Metformin and constipation Oral yol
Oral yol Embryology
Embryology Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Sistema digestorio função
Sistema digestorio função Gastrik inhibitör polipeptid
Gastrik inhibitör polipeptid