Preparation of the patient for dental proceduresurgery Veronika








- Slides: 36
Preparation of the patient for dental procedure/surgery Veronika Pokorna, MD, Ph. D. , MPH
Preoperative evalution • Medical history – Focus on risk factors: • Smoking • Family history - CVS diseases, VTE
Preoperative evalution • Medical history – Past medical history • Arterial hypertension, DM, atherosclerosis
Preoperative evalution • Actual health status: – Chest pain – Breathing problems – Palpitations – Acute infection • Physical examination
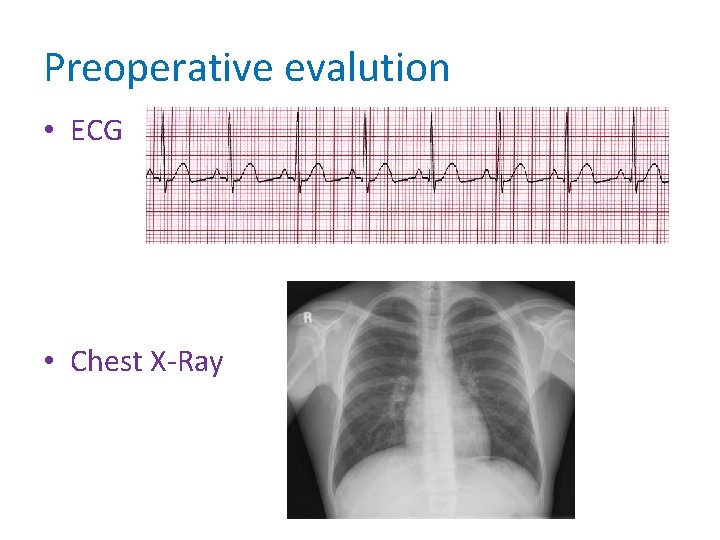
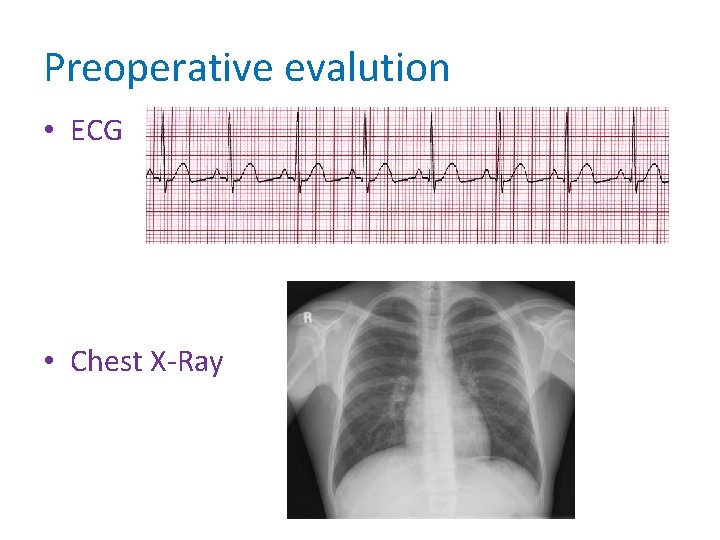
Preoperative evalution • ECG • Chest X-Ray
Preoperative evalution • Laboratory parameters – Blood count – Coagulation parameters – Biochemistry – glycemia, creatinine, Na, K, Cl, ALT – Serology – Blood group
Preoperative evalution • Summary of diagnosis • Recommendation on: – Peri-operative medication – Peri-operative management • Prevention of VTE

CVS assessment and management
CVS assessment and management


CVS assessment and management

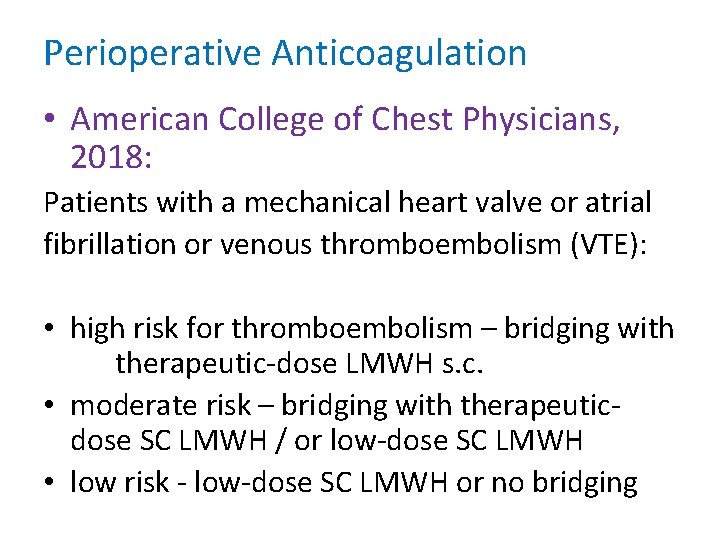
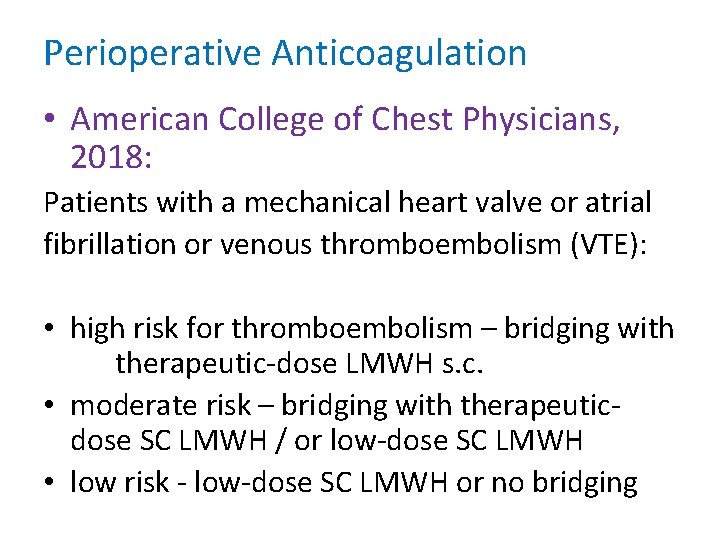
Perioperative Anticoagulation • American College of Chest Physicians, 2018: Patients with a mechanical heart valve or atrial fibrillation or venous thromboembolism (VTE): • high risk for thromboembolism – bridging with therapeutic-dose LMWH s. c. • moderate risk – bridging with therapeuticdose SC LMWH / or low-dose SC LMWH • low risk - low-dose SC LMWH or no bridging
Perioperative Anticoagulation • American College of Chest Physicians, 2018: In patients on VKAs who are undergoing minor dental procedures, continue the VKAs around the time of the procedure as well a coadminister an oral prohemostatic agent.
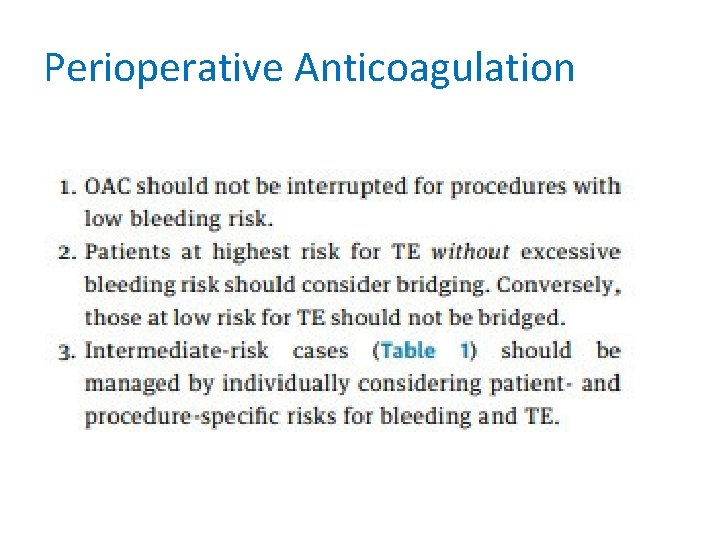
Perioperative Anticoagulation • American Heart Association, American College of Cardiology, Heart Rhythm Society, and American College of Chest Physicians:
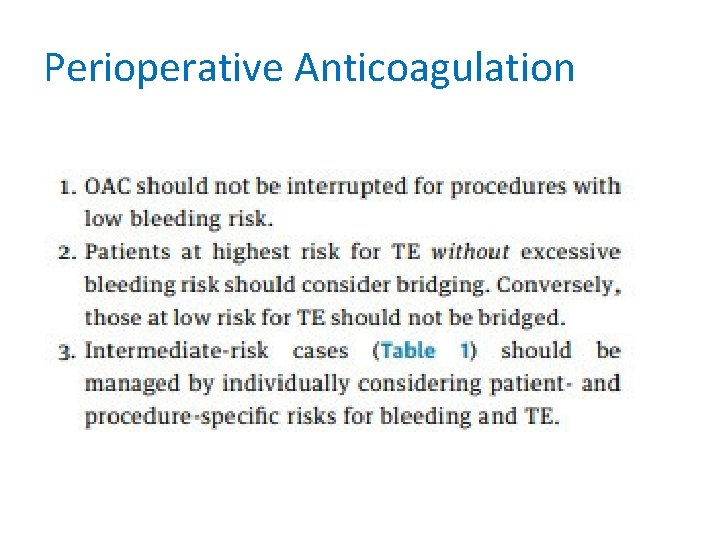
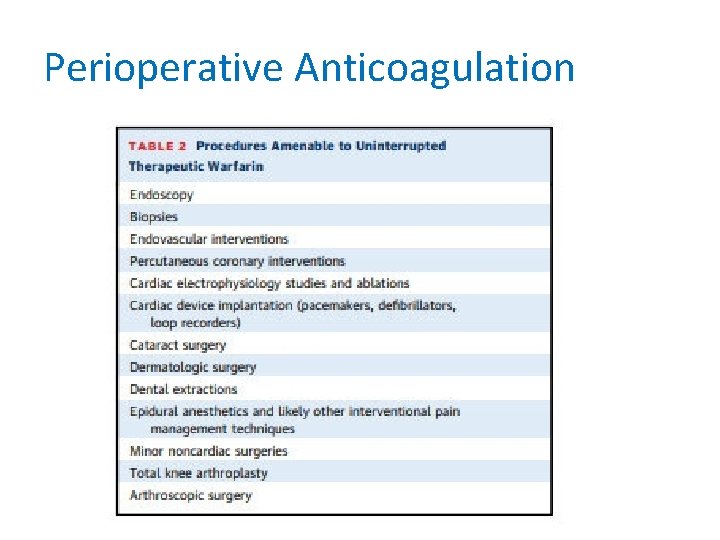
Perioperative Anticoagulation
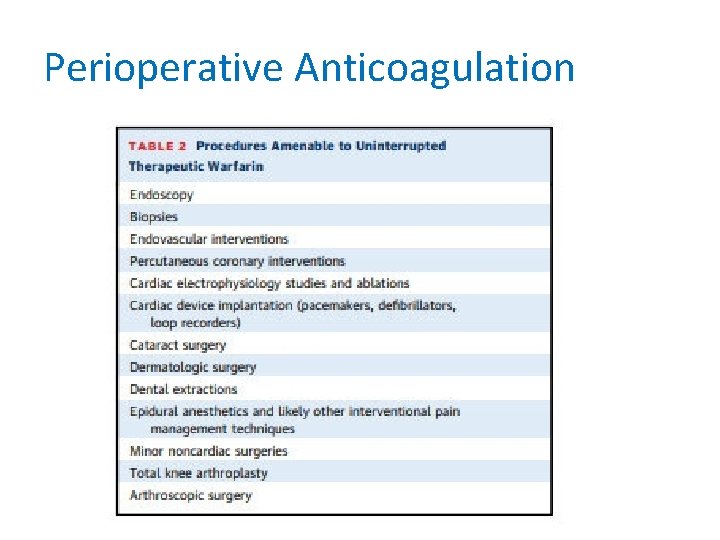
Perioperative Anticoagulation
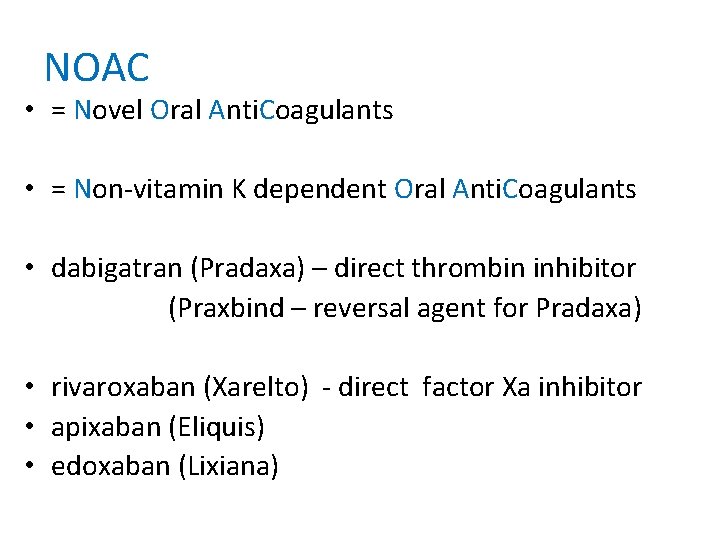
NOAC • = Novel Oral Anti. Coagulants • = Non-vitamin K dependent Oral Anti. Coagulants • dabigatran (Pradaxa) – direct thrombin inhibitor (Praxbind – reversal agent for Pradaxa) • rivaroxaban (Xarelto) - direct factor Xa inhibitor • apixaban (Eliquis) • edoxaban (Lixiana)
NOAC • Circulation, 2017
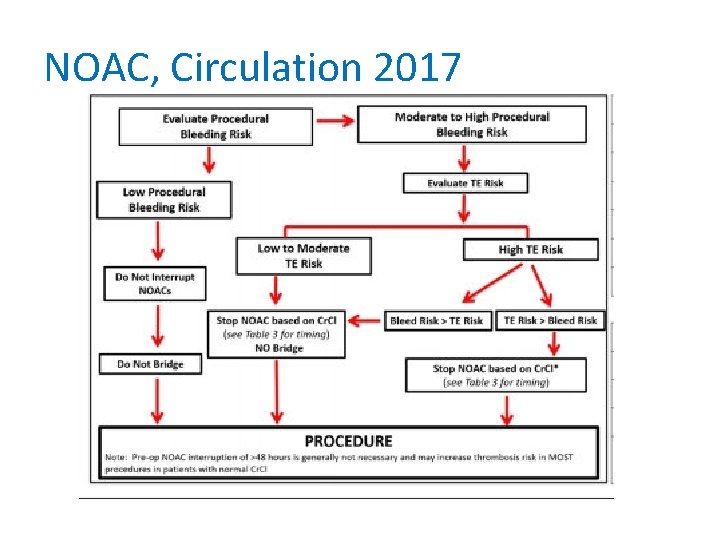
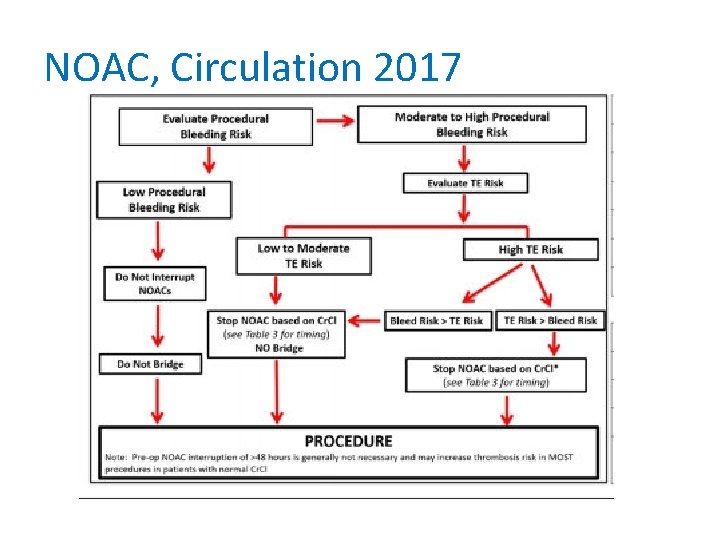
NOAC, Circulation 2017
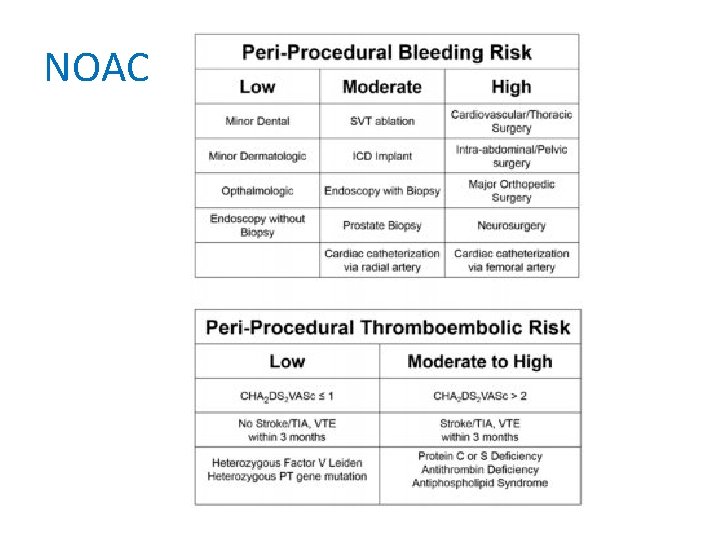
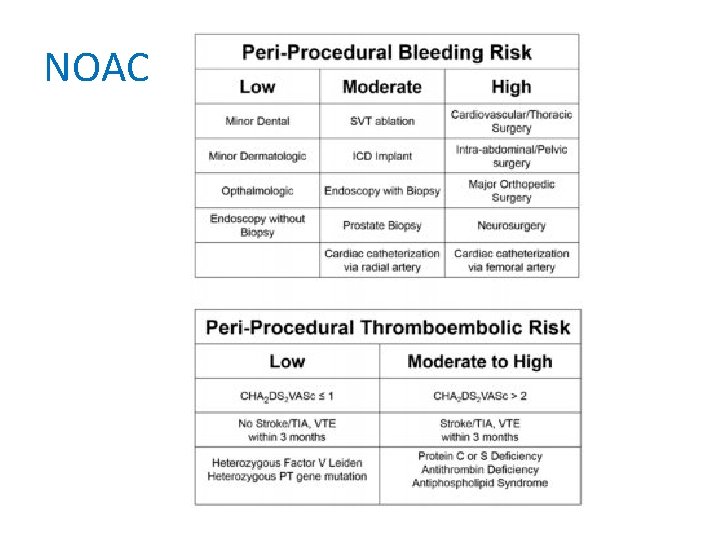
NOAC


Infective Endocarditis • Infective Endocarditis (Guidelines on Prevention, Diagnosis and Treatment of) ESC Clinical Practice Guidelines • ESC 2015 • www. escardio. org
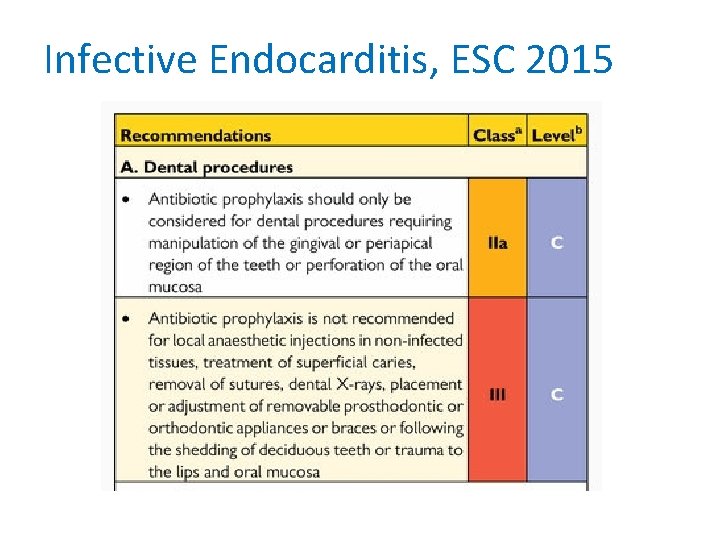
Infective Endocarditis, ESC 2015 • The restriction of indications for antibiotic prophylaxis was initiated in 2002 • Low-grade but repeated bacteraemia occurs more frequently during daily routine activities such as toothbrushing, flossing or chewing, and even more frequently in patients with poor dental health.
Infective Endocarditis, ESC 2015 • The estimated risk of IE following dental procedures is very low. • Antibiotic administration carries a small risk of anaphylaxis. • Widespread use of antibiotics may result in the emergence of resistant microorganisms.
Infective Endocarditis, ESC 2015 • Patients with the highest risk of IE can be placed in 3 categories: 1. Patients with a prosthetic valve or with prosthetic material used for cardiac valve repair, this also applies to transcatheterimplanted prostheses and homografts.
Infective Endocarditis, ESC 2015 • Patients with the highest risk of IE can be placed in 3 categories: 2. Patients with previous IE
Infective Endocarditis, ESC 2015 • Patients with the highest risk of IE can be placed in 3 categories: 3. Patients with untreated cyanotic congenital heart disease (CHD) and those with CHD who have postoperative palliative shunts, conduits or other prostheses.

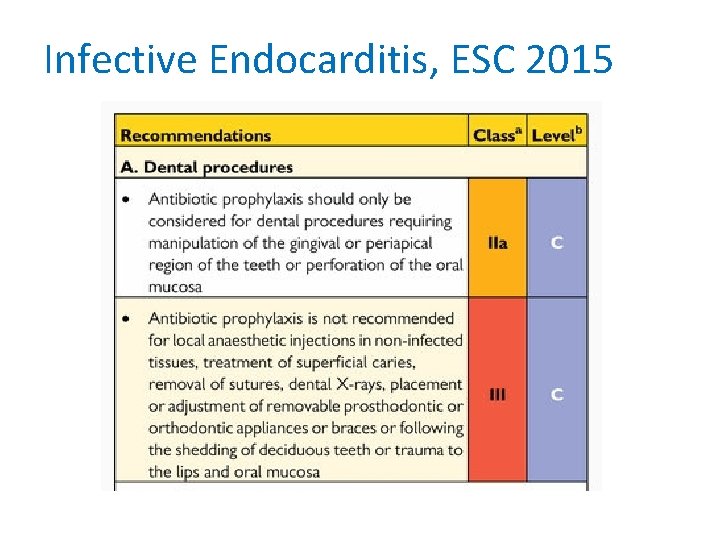
Infective Endocarditis, ESC 2015
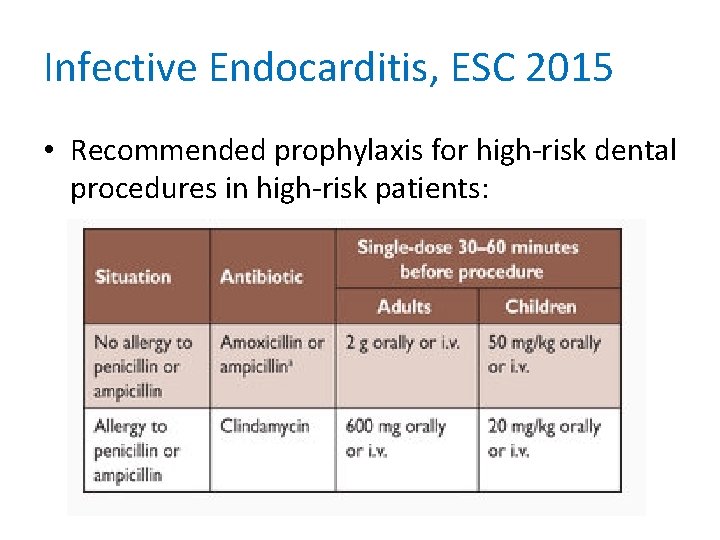
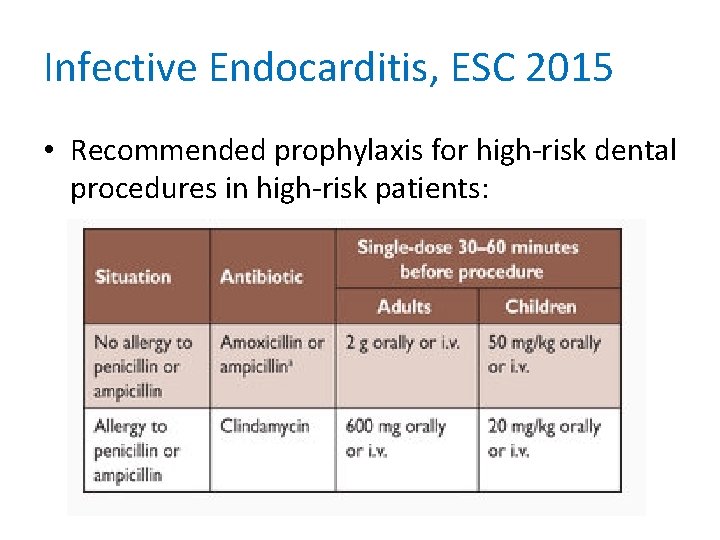
Infective Endocarditis, ESC 2015 • Recommended prophylaxis for high-risk dental procedures in high-risk patients:
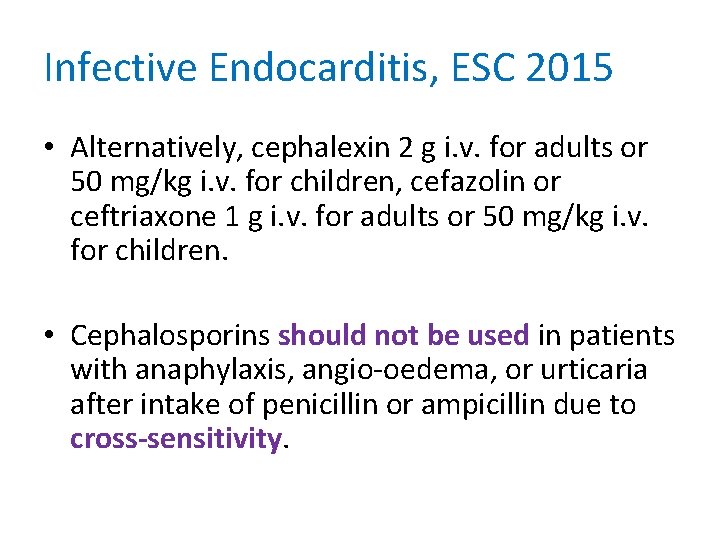
Infective Endocarditis, ESC 2015 • Alternatively, cephalexin 2 g i. v. for adults or 50 mg/kg i. v. for children, cefazolin or ceftriaxone 1 g i. v. for adults or 50 mg/kg i. v. for children. • Cephalosporins should not be used in patients with anaphylaxis, angio-oedema, or urticaria after intake of penicillin or ampicillin due to cross-sensitivity.

 Patient 2 patient
Patient 2 patient Procedure for admitting a patient
Procedure for admitting a patient Burs used in crown preparation
Burs used in crown preparation Veronika fuchsová
Veronika fuchsová Hi allow me to introduce myself
Hi allow me to introduce myself Veronika macků
Veronika macků Veronika grob
Veronika grob Veronika körner
Veronika körner Veronika braunisch
Veronika braunisch Veronika körner
Veronika körner Veronika duci
Veronika duci Veronika ruzickova porn
Veronika ruzickova porn Veronika martens
Veronika martens Hawaii tsunami 2012
Hawaii tsunami 2012 Veronika allas
Veronika allas Veronika opalova
Veronika opalova Veronika černohorská
Veronika černohorská Lisa roos nude
Lisa roos nude Andráczi tóth veronika
Andráczi tóth veronika Veronika logovinsky
Veronika logovinsky Veronika macků
Veronika macků Veronika bajt
Veronika bajt Dr. andráczi-tóth veronika
Dr. andráczi-tóth veronika Veronika margaret
Veronika margaret Musicians
Musicians Ivanova veronika
Ivanova veronika Youth in action programme
Youth in action programme Sztancsik veronika
Sztancsik veronika Unset message veronika
Unset message veronika Veronika pitova
Veronika pitova Veronika macků
Veronika macků Veronika velkova
Veronika velkova Defense mechanism mature
Defense mechanism mature Veronika körner
Veronika körner Veronika součková zpěv
Veronika součková zpěv Veronika liebl
Veronika liebl Kele veronika
Kele veronika