Postoperative care Introduction Postoperative complications are the most
- Slides: 23
Postoperative care
Introduction �Postoperative complications are the most important factors in determining outcome in the first 72 hours following surgery �It is critical to monitor basic physiological parameters such as renal, cardiovascular and respiratory functions
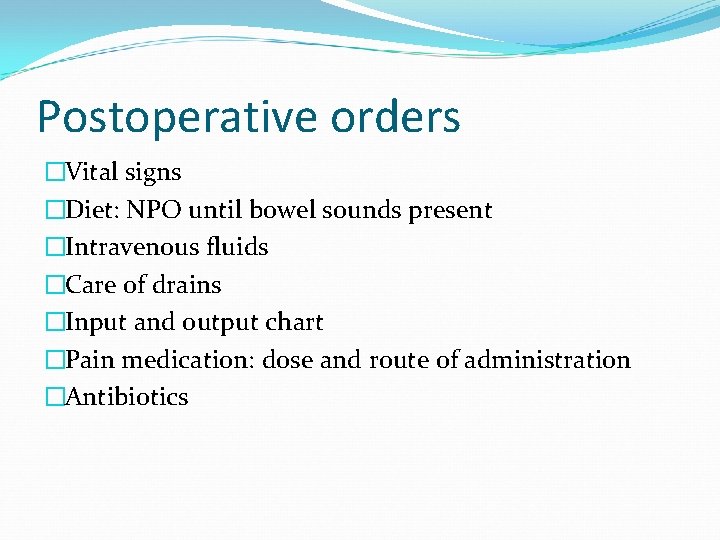
Postoperative orders �Vital signs �Diet: NPO until bowel sounds present �Intravenous fluids �Care of drains �Input and output chart �Pain medication: dose and route of administration �Antibiotics
Postoperative orders �Venous thrombosis prophylaxis �Other medications
Postoperative vascular complications �Venous thromboembolism (VTE) includes DVT and PE and are a major but preventable cause of morbidity and mortality
Pulmonary embolism �Has few definite symptoms �But onset of respiratory distress with hypotension, chest pain and cardiac arrhythmias may be harbingers of impending death �Can convert a successful operation into a postoperative fatality
Prevention of VTE �Unfractionated heparin �LMWH �Graduated compression stockings �Intermittent pneumatic compression stockings
Risk factors of postop thrombosis �Virchow’s triad: hypercoagulability, stasis, trauma to vessels
Diagnosis of VTE �Venography �Impedence plethysmography �Doppler ultrasound �MRI/MRI Venography
Treatment of VTE �UFH �LMWH
Postoperative pulmonary complications �Atelectasis �Pneumonia �Respiratory failure �Pulmonary thromboembolic disease
Risk factors for PPCs �Age > 60 years �Cancer �Congestive cardiac failure �Smoking (within 8 weeks of surgery) �Upper abdominal incision �Vertical incision �Incision length > 20 cm
Atelectasis �Definition not uniform in clinical studies �Generally accepted criteria include: �impaired oxygenation in a clinical setting where atelectasis is likely �Unexplained fever > 38 o. C �CXR evidence of volume loss or new airspace opacity
Risk factors for atelectasis �Advanced age �Obesity �Intraperitoneal atelectasis �Prolonged anaesthesia time �NG tube placement �Smoking
Prevention of atelectasis �Cessation of smoking (6 -8 weeks before surgery) �Laporoscopic procedure �Deep breathing exercises �Mobilization �Adequate analgesia (epidural or PCA preferred) �Selective gastric decompression
Postoperative pneumonia �Hospital-acquired pneumonia (HAP) is pneumonia that develops 48 hours or more after hospital admission because of an organism that was not incubating at the time of hospitalization �HAP after abdominal surgery increases mortality, hospital stay and hospital charges �Caused by a wide range of bacteria. Also by viruses and fungi in immunosuppressed patients
Pathogens causing early onset (<4 days) HAP �Strep pneumonia �MS Staph aureus �H influenza �E coli �K pneumonia �Enterobacter spp. �Proteus spp. �Serratia marcescens
Pathogens causing late onset (>5 days) HAP �Pseudomonas aeruginosa �MDR K pneumonia �Acinetobacter spp
HAP: clinical definition �New opacity on CXR( PA and lat views preferred) plus 2 of the following: �Fever >38 o. C �Leukocytosis or leukopenia �Purulent respiratory secretions �Diagnosis should be supported by sample of lower resp tract secretions-bronchoscopy
HAP treatment �Initial therapy should be given IV �Combination therapy for those at risk of MDR pathogens �Monotherapy for those at low risk of MDR
Respiratory failure �Def: inability to maintain normal tissue oxygen transport or the normal excretion of carbon dioxide �Arterial PO 2 < 60 mm. Hg or arterial PCO 2 > 45 mm. Hg generally indicate significant respiratory compromise �Generally managed in ICU including endotracheal intubation
Postoperative care of the urinary bladder �Most common postop problem of female bladder is atony caused by overdistension and reluctance of the patient to initiate the voluntary phase of voiding �Urethral or suprapubic catheter is used � 7 -10 days postop postvoid residuals are evaluated �If >100 ml catheterization duration is extended �Once residuals are less than 100 ml on 2 successive voidings of >200 ml catheters can be removed
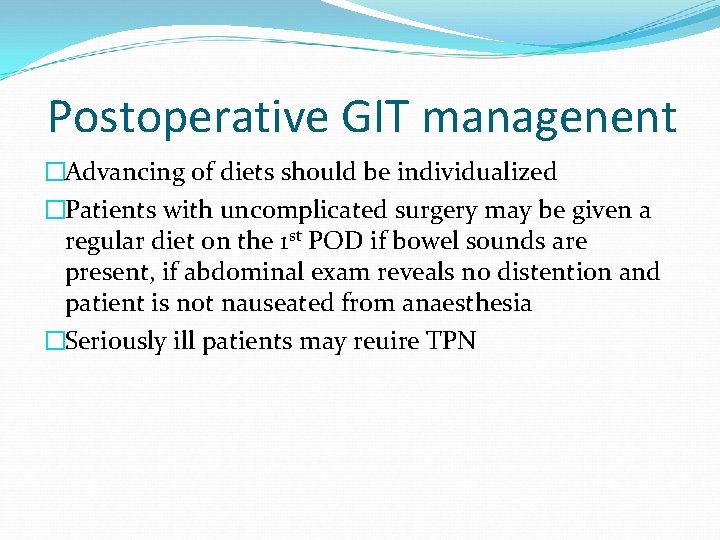
Postoperative GIT managenent �Advancing of diets should be individualized �Patients with uncomplicated surgery may be given a regular diet on the 1 st POD if bowel sounds are present, if abdominal exam reveals no distention and patient is not nauseated from anaesthesia �Seriously ill patients may reuire TPN
 Antigentest åre
Antigentest åre Nursing management of patient with cataract
Nursing management of patient with cataract Post operative nursing management
Post operative nursing management Levels of health care primary secondary tertiary
Levels of health care primary secondary tertiary Data klinis
Data klinis Postoperative shock
Postoperative shock Tsh
Tsh Eswl complications
Eswl complications C section complications
C section complications Duodenal switch complications
Duodenal switch complications Complications of shigellosis
Complications of shigellosis Double lumen tracheostomy
Double lumen tracheostomy Non atopic asthma
Non atopic asthma Cva complications
Cva complications Thoracentesis complications
Thoracentesis complications Complications of eclampsia
Complications of eclampsia Causes of post term pregnancy
Causes of post term pregnancy Post dated pregnancy complications
Post dated pregnancy complications قص العجان
قص العجان Massive transfusion protocol
Massive transfusion protocol Bronchoscopy complications
Bronchoscopy complications Rapamune
Rapamune Herpes zoster
Herpes zoster Bronchoscopy complications
Bronchoscopy complications