Population Health Management Concepts for Health Centers Module




- Slides: 22

Population Health Management Concepts for Health Centers Module 3 PHM Concepts for Health Centers Module 3 1
MODULE 3 A ROADMAP FOR IMPLEMENTING POPULATION HEALTH MANAGEMENT PHM Concepts for Health Centers Module 3 2
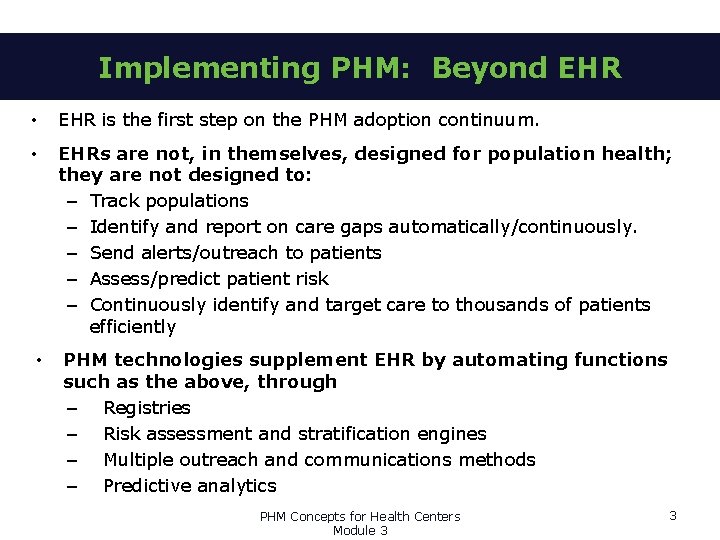
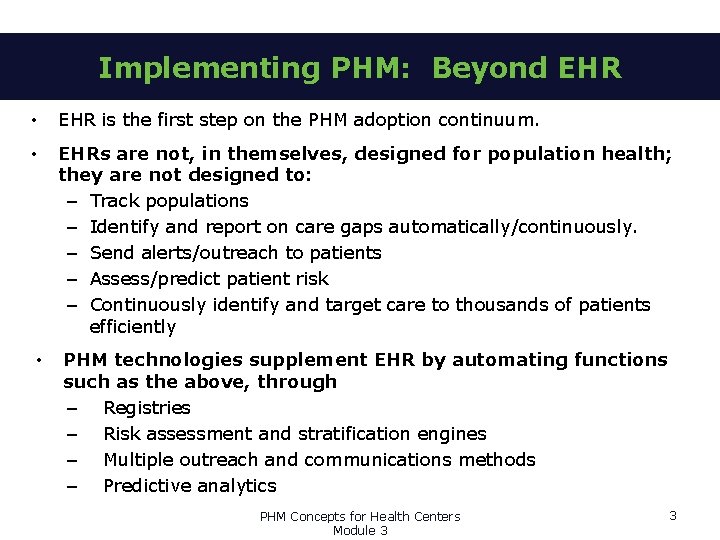
Implementing PHM: Beyond EHR • EHR is the first step on the PHM adoption continuum. • EHRs are not, in themselves, designed for population health; they are not designed to: – Track populations – Identify and report on care gaps automatically/continuously. – Send alerts/outreach to patients – Assess/predict patient risk – Continuously identify and target care to thousands of patients efficiently • PHM technologies supplement EHR by automating functions such as the above, through – Registries – Risk assessment and stratification engines – Multiple outreach and communications methods – Predictive analytics PHM Concepts for Health Centers Module 3 3
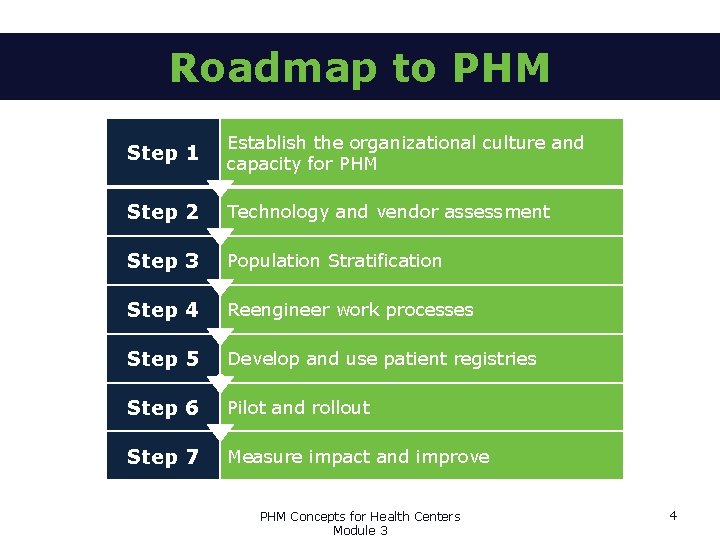
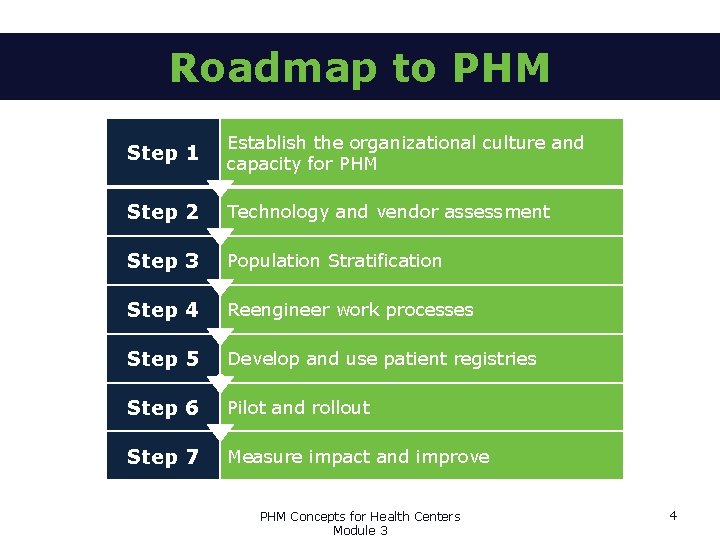
Roadmap to PHM Step 1 Establish the organizational culture and capacity for PHM Step 2 Technology and vendor assessment Step 3 Population Stratification Step 4 Reengineer work processes Step 5 Develop and use patient registries c Step 6 Pilot and rollout Step 7 Measure impact and improve PHM Concepts for Health Centers Module 3 4
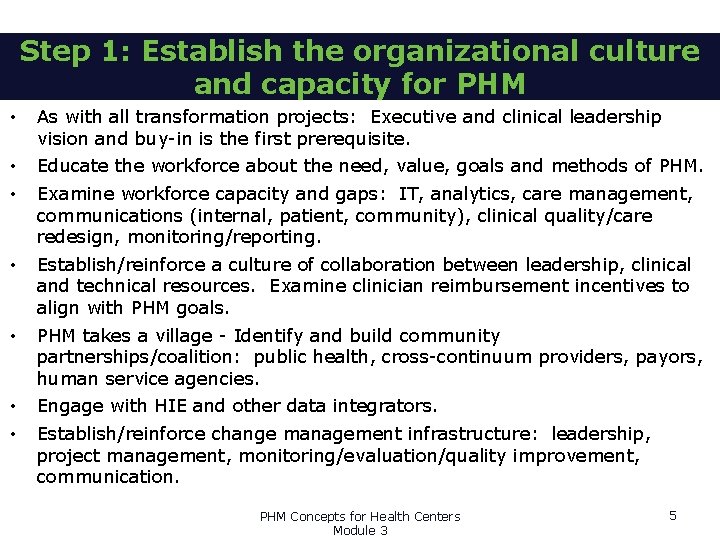
Step 1: Establish the organizational culture and capacity for PHM • As with all transformation projects: Executive and clinical leadership vision and buy-in is the first prerequisite. • • Educate the workforce about the need, value, goals and methods of PHM. • Establish/reinforce a culture of collaboration between leadership, clinical and technical resources. Examine clinician reimbursement incentives to align with PHM goals. • PHM takes a village - Identify and build community partnerships/coalition: public health, cross-continuum providers, payors, human service agencies. • • Engage with HIE and other data integrators. Examine workforce capacity and gaps: IT, analytics, care management, communications (internal, patient, community), clinical quality/care redesign, monitoring/reporting. Establish/reinforce change management infrastructure: leadership, project management, monitoring/evaluation/quality improvement, communication. PHM Concepts for Health Centers Module 3 5
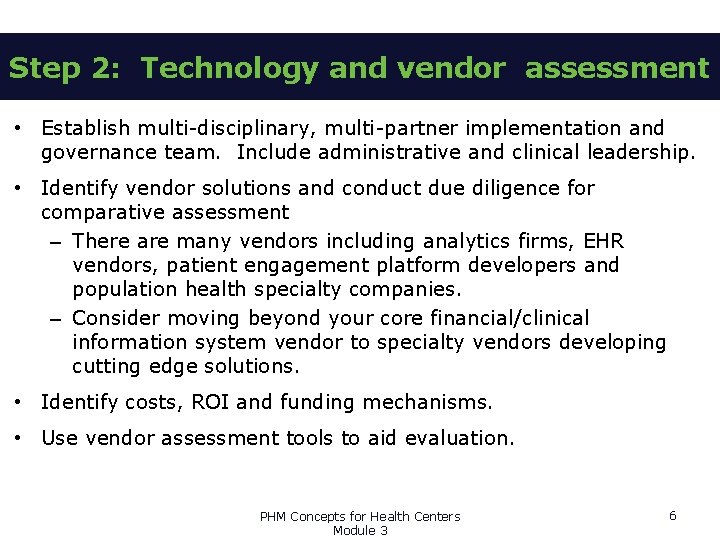
Step 2: Technology and vendor assessment • Establish multi-disciplinary, multi-partner implementation and governance team. Include administrative and clinical leadership. • Identify vendor solutions and conduct due diligence for comparative assessment – There are many vendors including analytics firms, EHR vendors, patient engagement platform developers and population health specialty companies. – Consider moving beyond your core financial/clinical information system vendor to specialty vendors developing cutting edge solutions. • Identify costs, ROI and funding mechanisms. • Use vendor assessment tools to aid evaluation. PHM Concepts for Health Centers Module 3 6
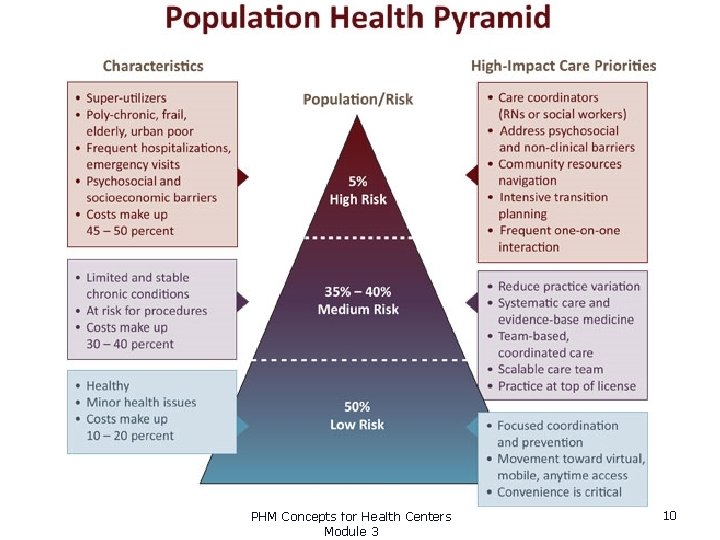
Step 3: Population Stratification • The heart of PHM is risk stratification of your health center’s panel to keep a patient population as healthy as possible to minimize expensive utilization and lower costs. • Risk stratification: assess all patients in your panel, grouping them into strata according to their risk of getting sick or sicker. • Theory is based on the Pareto principle – the 80/20 rule – the sickest 20% of the population is at highest risk to utilize 80% of high-cost services – Highest risk group includes people with multiple chronic diseases, Medicare and Medicaid population, people with disabilities, etc. – Highest risk patients pose highest financial risk to health centers with value-based reimbursement contracts. PHM Concepts for Health Centers Module 3 7
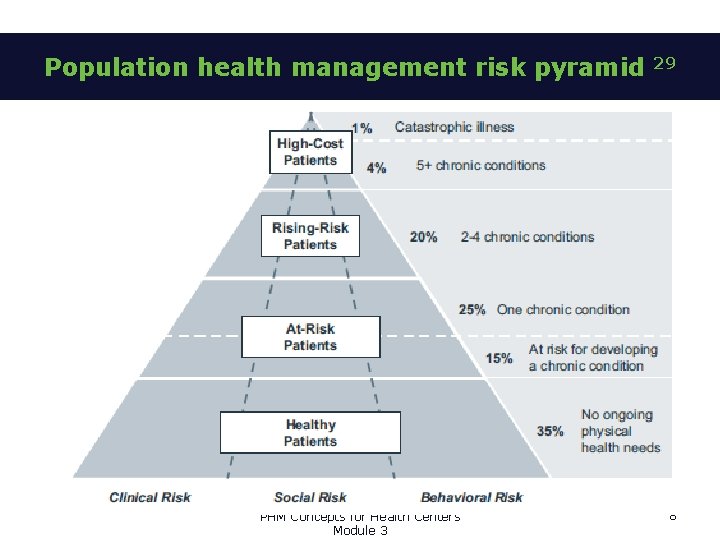
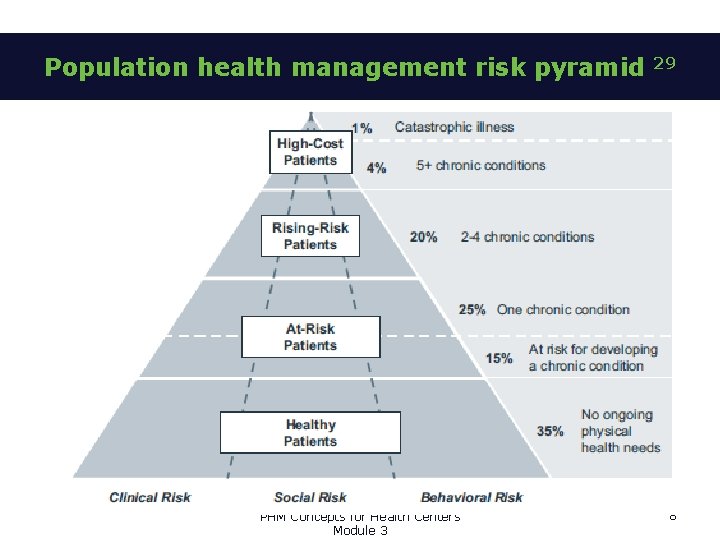
Population health management risk pyramid PHM Concepts for Health Centers Module 3 29 8
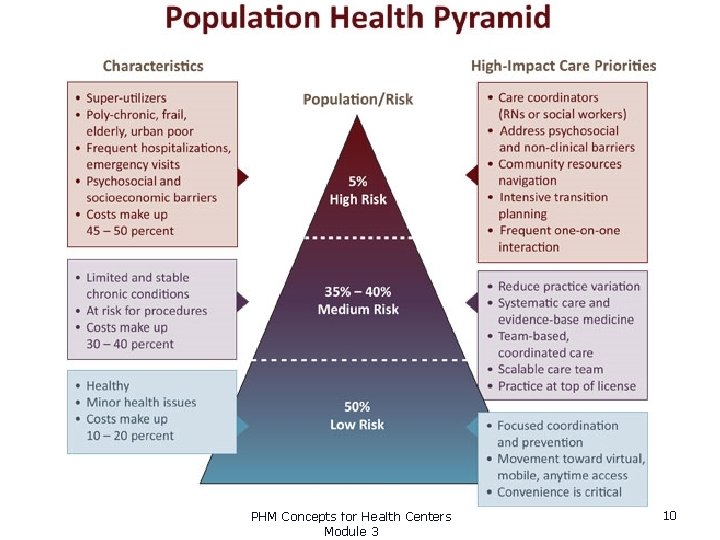
Population risk stratification • It’s not about focusing on the sickest to the exclusion of the healthy, it’s about all patients: – Target specific care to high-risk patients, while – Systematically addressing the preventive and chronic care needs of every patient, and – Monitor health of all patients • UNLIKE disease management which grouped patients by diagnosis, risk stratification identifies and groups patients by relative health risk that translates to care and resources required, for example: – Patients sick enough to require ongoing care management – Patients with chronic conditions needing intervention to prevent exacerbation – Healthy patients, need preventive care/education, positive health behavior reinforcement – By social determinants, health status, behavioral risk, financial risk that can be addressed PHM Concepts for Health Centers Module 3 9
30 PHM Concepts for Health Centers Module 3 10
Now that your population is stratified: PHM Methods • Apply care management and automated engagement to reduce utilization among the high risk 20%. • Health promotion/prevention focus to keep all patients from rising in risk • Critical success factors: – Patient engagement to encourage prevention and prevent leakage where at risk for total cost of care. – Network partnerships to collaborate to keep patients well. – Reengineering/care redesign is necessary to optimize and align work processes. PHM Concepts for Health Centers Module 3 11
Step 4: Reengineer work processes • Three Clinical pillars of PHM enabled by analytics and automation: – Multidisciplinary care teams to extend the reach of the PCP and engage the patient; – Reach out to patients and populations beyond the walls of the clinic; – Optimize patient visits. • Data-driven Quality Improvement to make work processes more efficient – Utilize data-driven QI processes and tools; – Use Lean/Six Sigma efficiency improvement methods where possible; – Refer to HITEQ Data-Driven Quality Improvement Resource Set for resources and tools. • Team-based care, and reaching lives through automated care management and patient engagement tools to make care more targeted and effective – Enhanced access to primary care; – A communications engine can provide automated patient outreach and alerts to maintain contact with patients and support self-management • For health centers, especially important to use technology to stay in contact with vulnerable populations who often have less frequent contact with providers. – Focus on health behavior and lifestyle, integration of behavioral health; – Care management of high-risk patients; – Coordination across the continuum of care. PHM Concepts for Health Centers Module 3 12
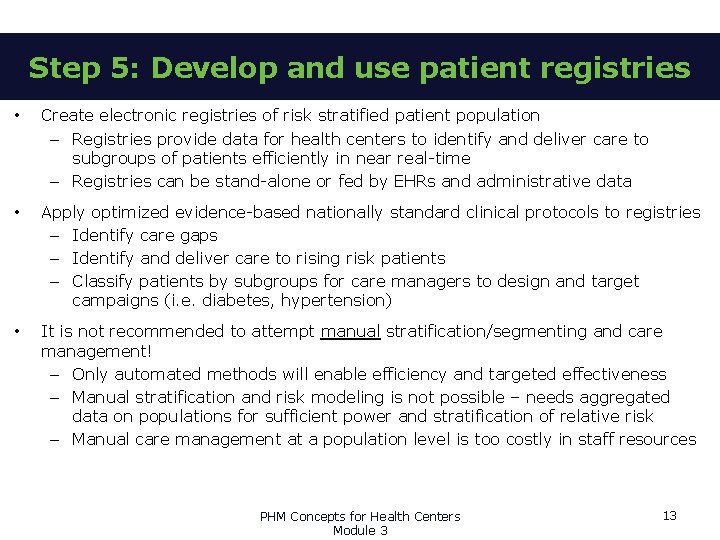
Step 5: Develop and use patient registries • Create electronic registries of risk stratified patient population – Registries provide data for health centers to identify and deliver care to subgroups of patients efficiently in near real-time – Registries can be stand-alone or fed by EHRs and administrative data • Apply optimized evidence-based nationally standard clinical protocols to registries – Identify care gaps – Identify and deliver care to rising risk patients – Classify patients by subgroups for care managers to design and target campaigns (i. e. diabetes, hypertension) • It is not recommended to attempt manual stratification/segmenting and care management! – Only automated methods will enable efficiency and targeted effectiveness – Manual stratification and risk modeling is not possible – needs aggregated data on populations for sufficient power and stratification of relative risk – Manual care management at a population level is too costly in staff resources PHM Concepts for Health Centers Module 3 13
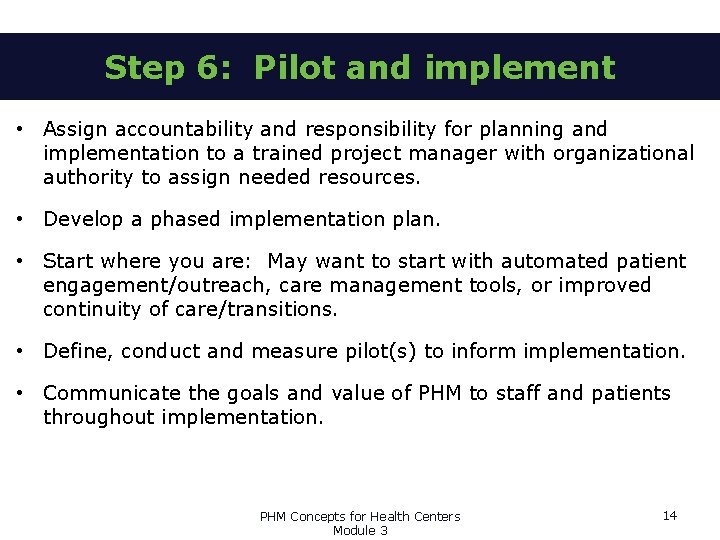
Step 6: Pilot and implement • Assign accountability and responsibility for planning and implementation to a trained project manager with organizational authority to assign needed resources. • Develop a phased implementation plan. • Start where you are: May want to start with automated patient engagement/outreach, care management tools, or improved continuity of care/transitions. • Define, conduct and measure pilot(s) to inform implementation. • Communicate the goals and value of PHM to staff and patients throughout implementation. PHM Concepts for Health Centers Module 3 14
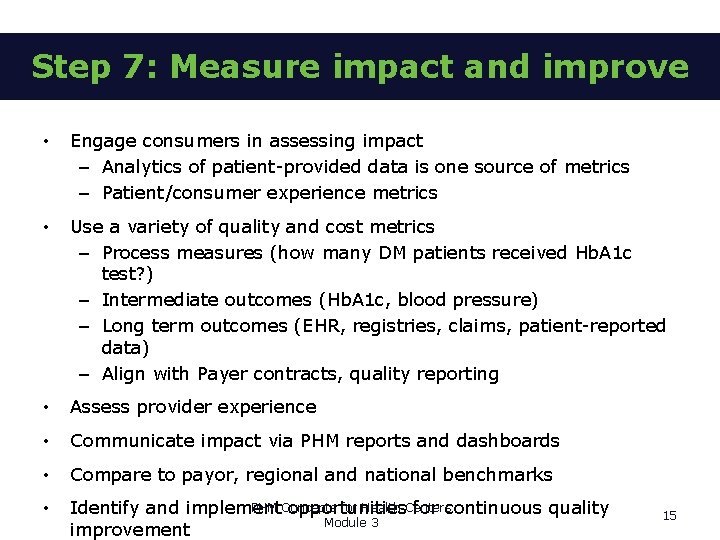
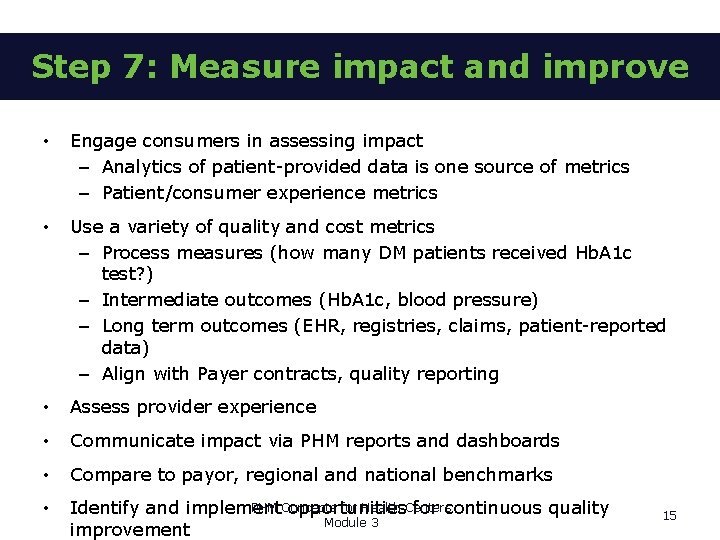
Step 7: Measure impact and improve • Engage consumers in assessing impact – Analytics of patient-provided data is one source of metrics – Patient/consumer experience metrics • Use a variety of quality and cost metrics – Process measures (how many DM patients received Hb. A 1 c test? ) – Intermediate outcomes (Hb. A 1 c, blood pressure) – Long term outcomes (EHR, registries, claims, patient-reported data) – Align with Payer contracts, quality reporting • Assess provider experience • Communicate impact via PHM reports and dashboards • Compare to payor, regional and national benchmarks • PHM Concepts for Health Centers Identify and implement opportunities for continuous quality Module 3 improvement 15
IMPLEMENTATION CHALLENGES PHM Concepts for Health Centers Module 3 16
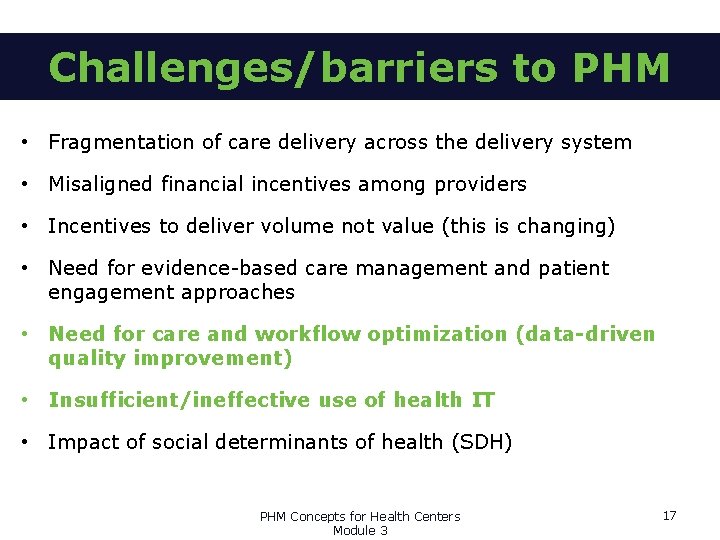
Challenges/barriers to PHM • Fragmentation of care delivery across the delivery system • Misaligned financial incentives among providers • Incentives to deliver volume not value (this is changing) • Need for evidence-based care management and patient engagement approaches • Need for care and workflow optimization (data-driven quality improvement) • Insufficient/ineffective use of health IT • Impact of social determinants of health (SDH) PHM Concepts for Health Centers Module 3 17

Be sure your PHM and SDH tools play well together… • There are different approaches to implementing PHM: – Add-on functionality/module to existing EHR – PHM specialty system – “Homegrown” tools or different systems “cobbled” together. These components/systems may not play well together. • Avoid a “morass of different systems that become difficult to manage”. 31 • Avoid disparate systems that don’t interoperate nor add value to each other. 31 • For some institutions: “…chasing shiny objects is very common” 31…. avoid this! PHM Concepts for Health Centers Module 3 18
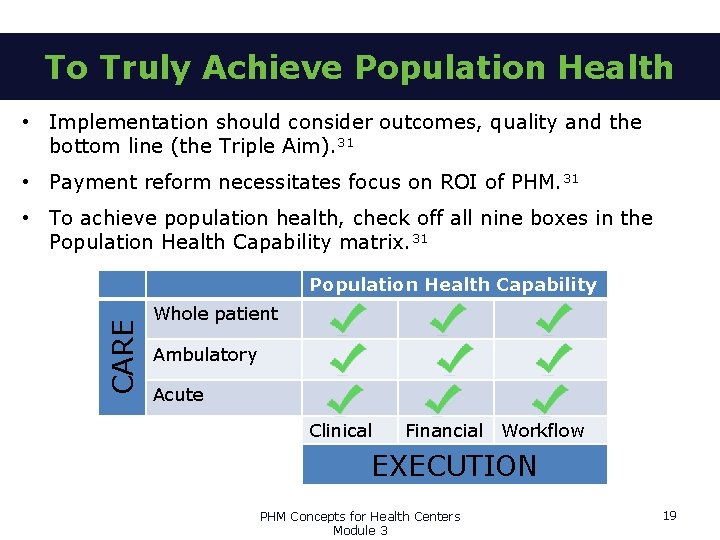
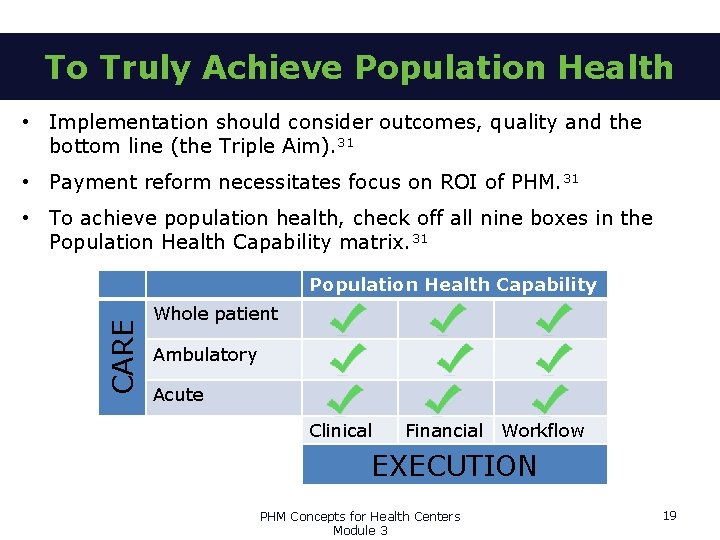
To Truly Achieve Population Health • Implementation should consider outcomes, quality and the bottom line (the Triple Aim). 31 • Payment reform necessitates focus on ROI of PHM. 31 • To achieve population health, check off all nine boxes in the Population Health Capability matrix. 31 CARE Population Health Capability Whole patient Ambulatory Acute Clinical Financial Workflow EXECUTION PHM Concepts for Health Centers Module 3 19

References 1. 2. Kindig, D and Stoddart, G. What is Population Health? American Journal of Public Health. 2003; 93, 3. 4. 5. Dr. John Frank, scientific director, Canada Institute of Population and Public Health. 6. Schroeder, S. A. (2007). We can do better—Improving the health of the American people. The New England Journal of Medicine, 357(12), 1221– 1228. 7. 8. 9. 10. National Association of Community Health Centers. PRAPARE. http: //nachc. org/research-and-data/prapare/. 2016. Dartmouth-Hitchcock. What is Population Health? http: //www. dartmouthhitchcock. org/about_dh/what_is_population_health. html. 2016. Young, TK. Population Health: Concepts and Methods. New York, NY: Oxford University press; 1998. World Health Organization. “Social Determinants of Health. ” http: //www. who. int/social_determinants/thecommission/finalreport/key_concepts/en/. 2016. IBM Phytel Population Health Management. http: //www 3. phytel. com/our-platform/phytel-atmosphere About HRSA. http: //www. hrsa. gov/about/. March 2016. Healthy Communities, Healthy People: HRSA and the Affordable Care Act. https: //www. cms. gov/Outreach-and. Education/Outreach/Open. Door. Forums/Downloads/HRSAAffordable. Care. Act. Provisionsupdated. PPTSlides. pdf 11. HRSA Strategic Plan 2016 -2018. http: //www. hrsa. gov/about/strategicplan/index. html. March 2016. 12. HRSA Strategic Plan 2016 -2018. Goal 3: Build Healthy Communities. http: //www. hrsa. gov/about/strategicplan/goal 3. html. March 2016. 13. Centers for Disease Control and Prevention. Million Hearts®. http: //millionhearts. hhs. gov/. 14. Centers for Medicare & Medicaid Services. Million Hearts® Cardiovascular Disease Risk Reduction Model https: //innovation. cms. gov/initiatives/Million-Hearts-CVDRRM/. July 21, 2016. 15. Centers for Disease Control and Prevention. Million Hearts® Undiagnosed Hypertension. http: //millionhearts. hhs. gov/tools-protocols/hiding-plain-sight/index. html. Accessed November 28, 2016 16. Centers for Disease Control and Prevention. Million Hearts® Hypertension Prevalence Estimator Tool. https: //nccd. cdc. gov/Million. Hearts/Estimator/. Accessed November 28, 2016. 17. Health. IT. gov. EHR Incentives & Certification. https: //www. healthit. gov/providers-professionals/meaningful-use-definition -objectives. February 6, 2015. 18. Centers for Medicare & Medicaid Services. Electronic Health Records (EHR) Incentive Programs https: //www. cms. gov/Regulations-and. Guidance/Legislation/EHRIncentive. Programs/index. html? redirect=/EHRIncentive. Programs/. November 22, 2016. 19. Health. IT. gov. How can electronic health records improve public and population health outcomes? https: //www. healthit. gov/providers-professionals/faqs/how-can-electronic-health-records-improve-public-and-populationhealth-. January 15, 2013.

References 20. Centers for Medicare & Medicaid Services. EHR Incentive Programs in 2015 through 2017 Public Health Reporting for Eligible Professionals in 2016. https: //www. cms. gov/Regulations-and. Guidance/Legislation/EHRIncentive. Programs/Downloads/2016_EPPublic. Health. Reporting. pdf. 2016. 21. HRSA Strategic Plan 2016 -2018. Goal 4: Improve Health Equity http: //www. hrsa. gov/about/strategicplan/goal 4. html. March 2016. 22. Whitehead M, Dahlgren G. Concepts and Principles for Tackling Social Inequities in Health: Levelling up, Part 1. World Health Organization, Regional Office for Europe; 2006. www. euro. who. int/__data/assets/pdf_file/0010/74737/E 89383. pdf 23. Laderman M, Whittington J. A framework for improving health equity. Healthcare Executive. 2016 May; 31(3): 82 -85 http: //www. ihi. org/resources/Pages/Publications/Framework-Improving-Health-Equity. aspx 24. The City of Portland, OR. The Problem with “Equality”. https: //www. portlandoregon. gov/oehr/article/449547? . 2016. 25. Gaskin DJ, La. Veist TA, Richard P. The State of Urban Health: Eliminating Health Disparities to Save Lives and Cut Costs. Washington, DC: National Urban League Policy Institute; December 2012. 26. Cohen SB. The Concentration of Health Care Expenditures and Related Expenses for Costly Medical Conditions, 2009. Agency for Healthcare Research and Quality, Statistical Brief #359. February 2012. http: //meps. ahrq. gov/mepsweb/data_files/publications/st 359/stat 359. pdf 27. Wyatt R, Laderman M, Botwinick L, Mate K, Whittington J. Achieving Health Equity: A Guide for Health Care Organizations. IHI White Paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2016. 28. Hodach, R. Provider-Led Population Health Management, Author. House, 2015 29. Arcadia Healthcare Solutions. Risk: It’s More Than a Number. http: //arcadiasolutions. com/risk-more-than-a-number/. April 9, 2014. Accessed September 19, 2016. 30. Clifton Larson Allen. Moving From Traditional Care Delivery Models to Population Health Management. http: //www. claconnect. com/Health-Care/Transition-From-Traditional-Care-Delivery-Models-to-Population-Health. Management. aspx. April 16, 2015. Accessed September 19, 2016. 31. Jeffrey Springer, VP Healthcare Solutions, Citius. Tech Inc. , Top 5 Emerging Trends in Population Health, September 2016 HIMSS and Healthcare IT New Pop Health Forum, Chicago, IL. http: //www. healthcareitnews. com/node/529146, accessed September 19, 2016. 32. Institute for Health Technology Transformation, Population Health Management: A Roadmap for Provider-Based Automation in a New Era of Healthcare. 2012. http: //www 3. phytel. com/docs/default-source/resources/a-roadmap-forprovider-based-automation-in-a-new-era-of-healthcare. pdf? sfvrsn=2 33. Stiefel M, Nolan K. A Guide to Measuring the Triple Aim: Population Health, Experience of Care, and Per Capita Cost. IHI Innovation Series white paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2012. 34. Stoto, M. Population Health in the Affordable Care Act Era. Academy. Health. February 21, 2013.
MODULE 3 COMPLETED Check Out Module 4: Data for Population Health Management Measuring Population Health Emerging Directions in Population Health PHM Concepts for Health Centers Module 3 22
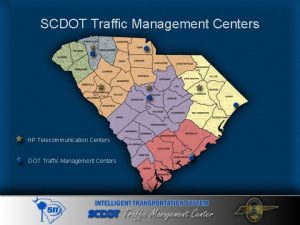
 Indiana council of community mental health centers
Indiana council of community mental health centers Health resource centers and libraries near pittsburg
Health resource centers and libraries near pittsburg Cloud os for virtualized data centers
Cloud os for virtualized data centers Social responsibility of management ppt
Social responsibility of management ppt Population ecology section 1 population dynamics answer key
Population ecology section 1 population dynamics answer key Population ecology section 1 population dynamics answer key
Population ecology section 1 population dynamics answer key Population ecology section 1 population dynamics
Population ecology section 1 population dynamics Chapter 4 section 1 population dynamics answer key
Chapter 4 section 1 population dynamics answer key Population health risk assessment and management
Population health risk assessment and management Stp manipulation attack
Stp manipulation attack Module 5 computer concepts skills training
Module 5 computer concepts skills training Module 5 computer concepts exam answers
Module 5 computer concepts exam answers Module 8 computer concepts skills training
Module 8 computer concepts skills training Module 4 computer concepts
Module 4 computer concepts Module 9 computer concepts
Module 9 computer concepts C device module module 1
C device module module 1 Kontinuitetshantering
Kontinuitetshantering Typiska drag för en novell
Typiska drag för en novell Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Kassaregister ideell förening
Kassaregister ideell förening