Polypharmacy Anticoagulation AF meets PCI David J Moliterno
- Slides: 20
Polypharmacy Anticoagulation: AF meets PCI David J. Moliterno, MD Professor and Chairman Department of Internal Medicine The University of Kentucky Linda and Jack Gill Heart Institute
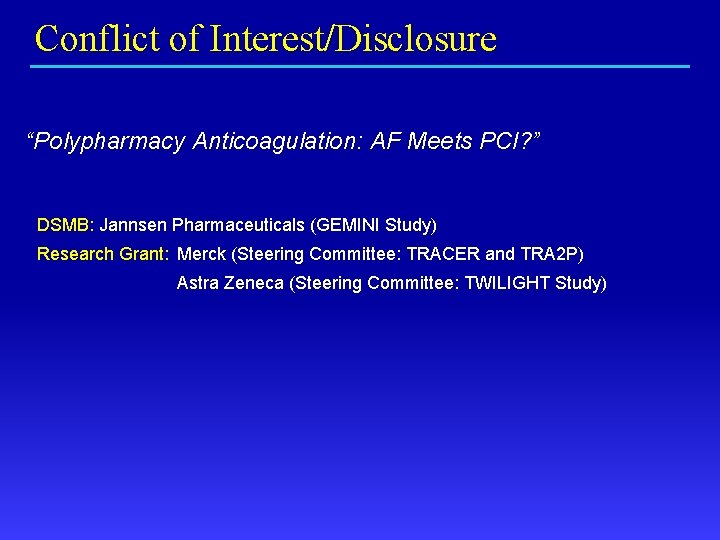
Conflict of Interest/Disclosure “Polypharmacy Anticoagulation: AF Meets PCI? ” DSMB: Jannsen Pharmaceuticals (GEMINI Study) Research Grant: Merck (Steering Committee: TRACER and TRA 2 P) Astra Zeneca (Steering Committee: TWILIGHT Study)
Optimal Anticoagulation—does it exist? Bleeding Thrombosis intensity x duration
Atrial Fibrillation § Most common sustained cardiac arrhythmia § Currently affects nearly 2. 3 million Americans, or 1% of US population § Prevalence expected to increase 2. 5 x by 2050 § Lifetime risk of developing AF: 1 in 4 for men and women ≥ 40 years of age § Among ACS-PCI patients, ~5% have AF § AF best managed with OAC among those needing antithrombotic therapy
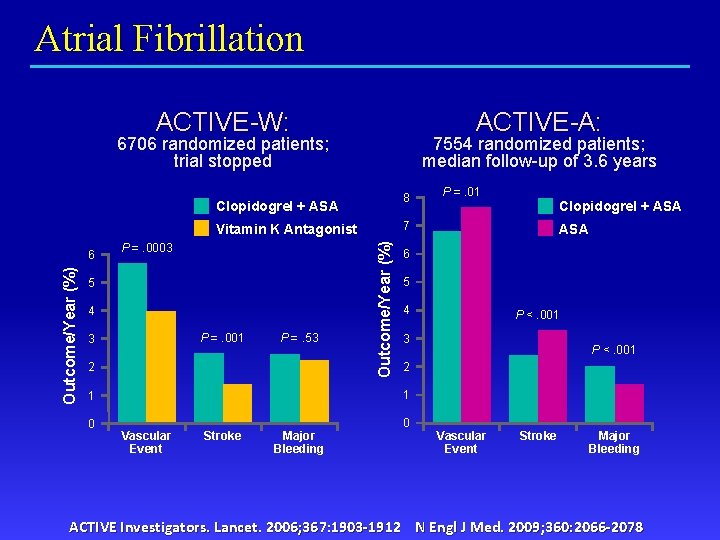
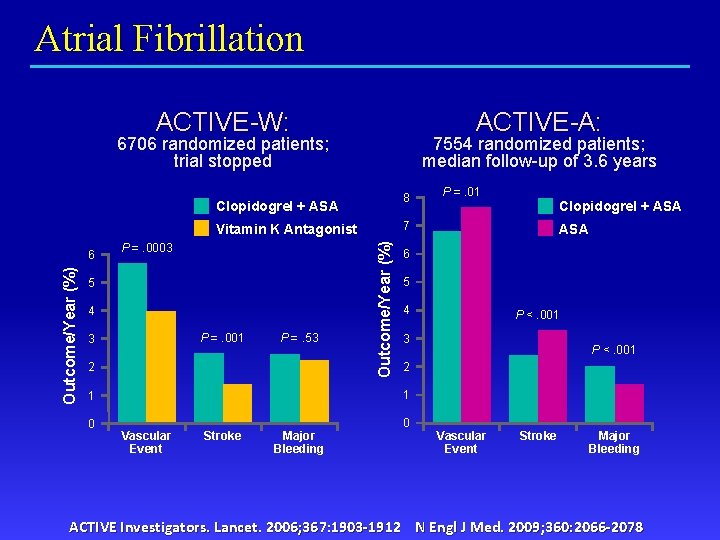
Atrial Fibrillation ACTIVE-W: ACTIVE-A: 6706 randomized patients; trial stopped 7554 randomized patients; median follow-up of 3. 6 years 8 Clopidogrel + ASA 5 4 P =. 001 3 P =. 53 2 Outcome/Year (%) P =. 0003 5 4 P <. 001 2 0 0 Major Bleeding P <. 001 3 1 Stroke ASA 6 1 Vascular Event Clopidogrel + ASA 7 Vitamin K Antagonist 6 P =. 01 Vascular Event Stroke Major Bleeding ACTIVE Investigators. Lancet. 2006; 367: 1903 -1912 N Engl J Med. 2009; 360: 2066 -2078
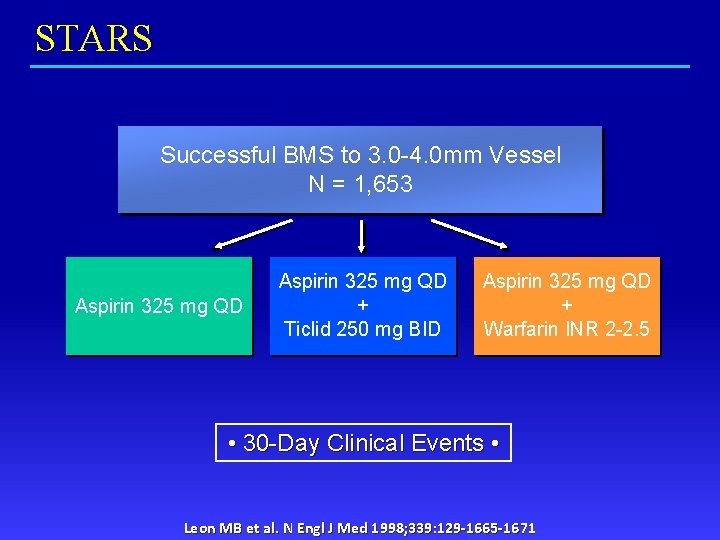
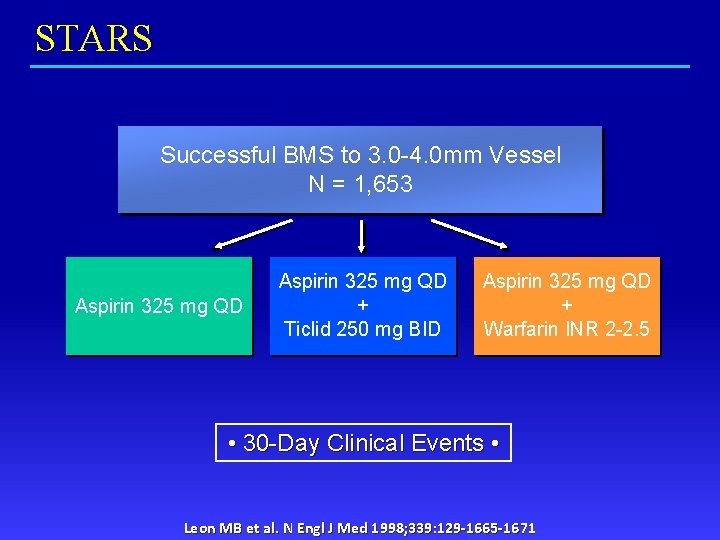
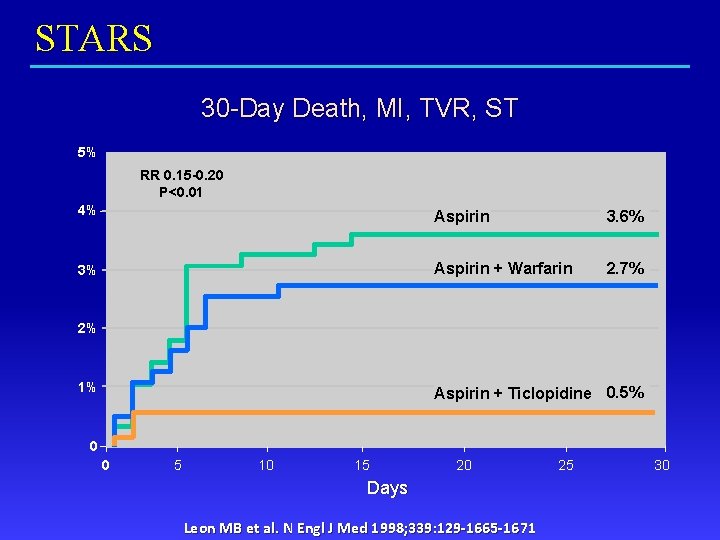
STARS Successful BMS to 3. 0 -4. 0 mm Vessel N = 1, 653 Aspirin 325 mg QD + Ticlid 250 mg BID Aspirin 325 mg QD + Warfarin INR 2 -2. 5 • 30 -Day Clinical Events • Leon MB et al. N Engl J Med 1998; 339: 129 -1665 -1671
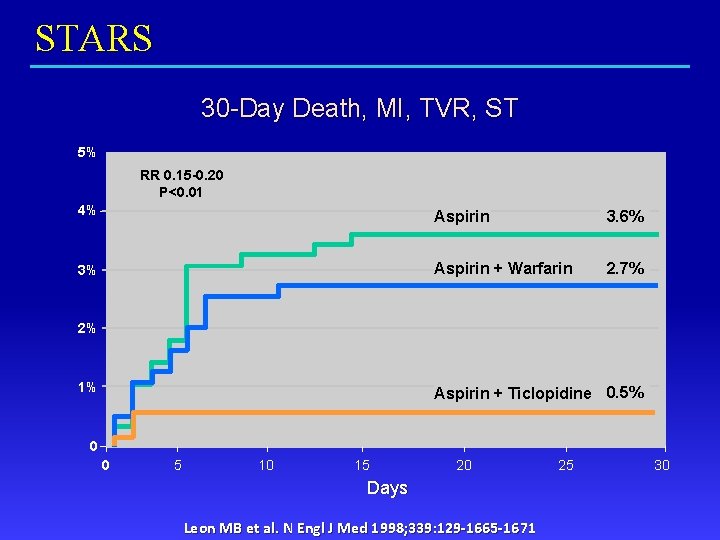
STARS 30 -Day Death, MI, TVR, ST 5% RR 0. 15 -0. 20 P<0. 01 4% Aspirin 3. 6% 3% Aspirin + Warfarin 2. 7% 2% 1% Aspirin + Ticlopidine 0. 5% 0 0 5 10 15 20 Days Leon MB et al. N Engl J Med 1998; 339: 129 -1665 -1671 25 30
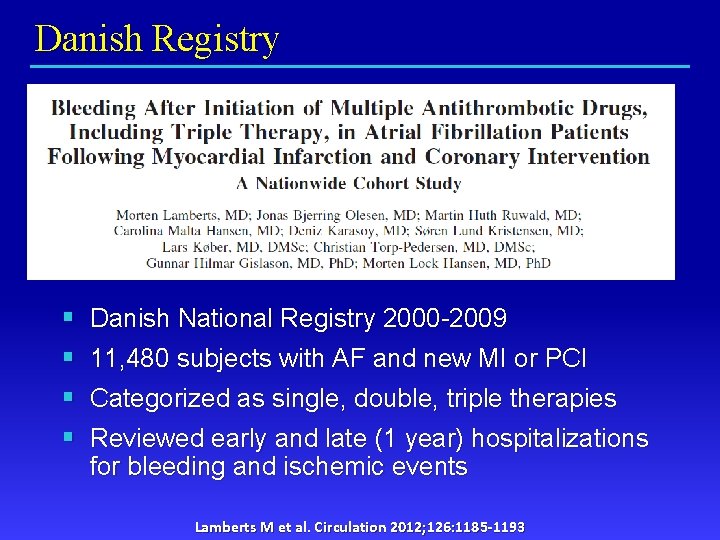
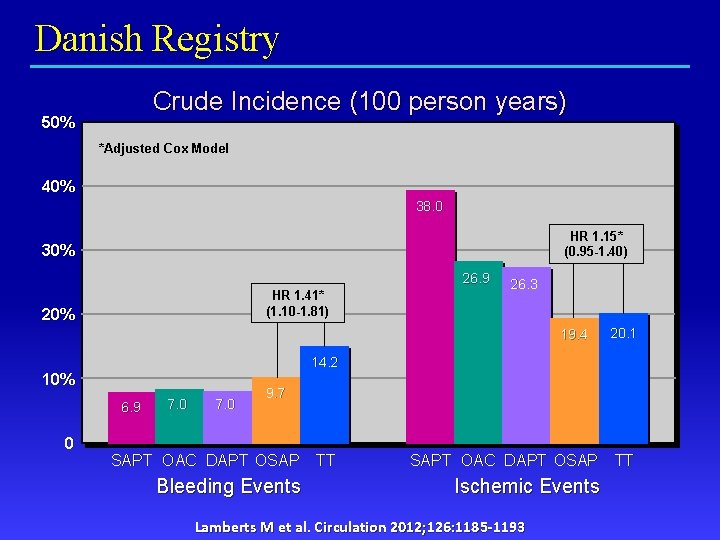
Danish Registry § § Danish National Registry 2000 -2009 11, 480 subjects with AF and new MI or PCI Categorized as single, double, triple therapies Reviewed early and late (1 year) hospitalizations for bleeding and ischemic events Lamberts M et al. Circulation 2012; 126: 1185 -1193
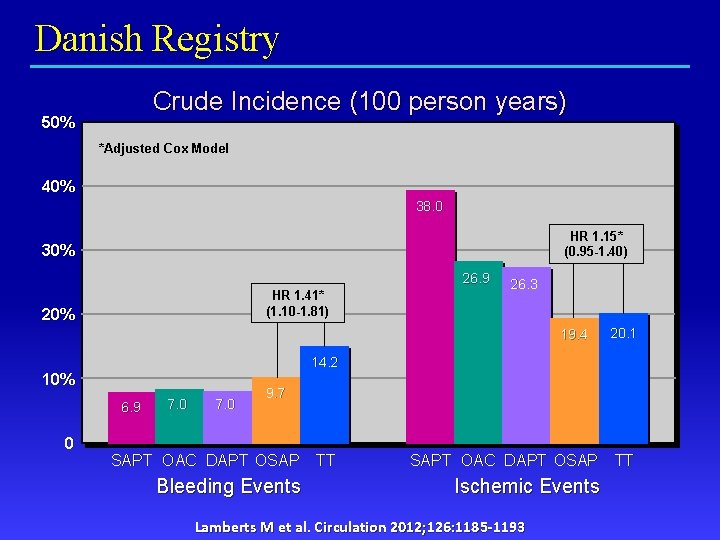
Danish Registry Crude Incidence (100 person years) 50% *Adjusted Cox Model 40% 38. 0 HR 1. 15* (0. 95 -1. 40) 30% 26. 9 HR 1. 41* (1. 10 -1. 81) 20% 26. 3 19. 4 20. 1 14. 2 10% 6. 9 0 7. 0 9. 7 SAPT OAC DAPT OSAP Bleeding Events TT SAPT OAC DAPT OSAP Ischemic Events Lamberts M et al. Circulation 2012; 126: 1185 -1193 TT
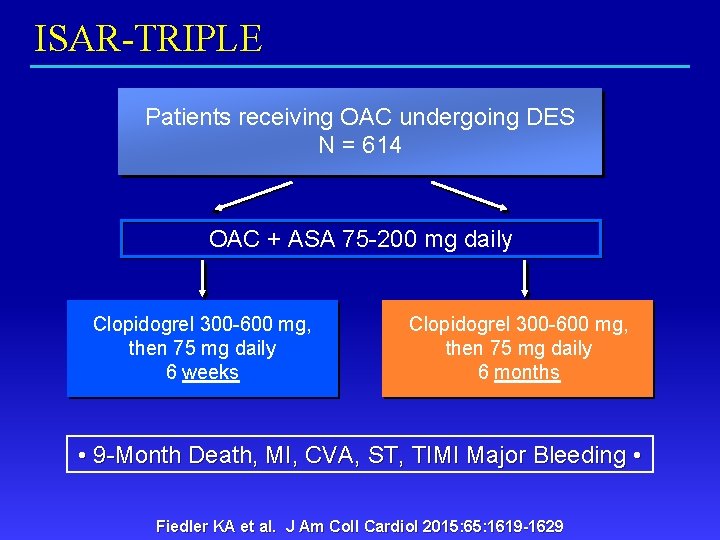
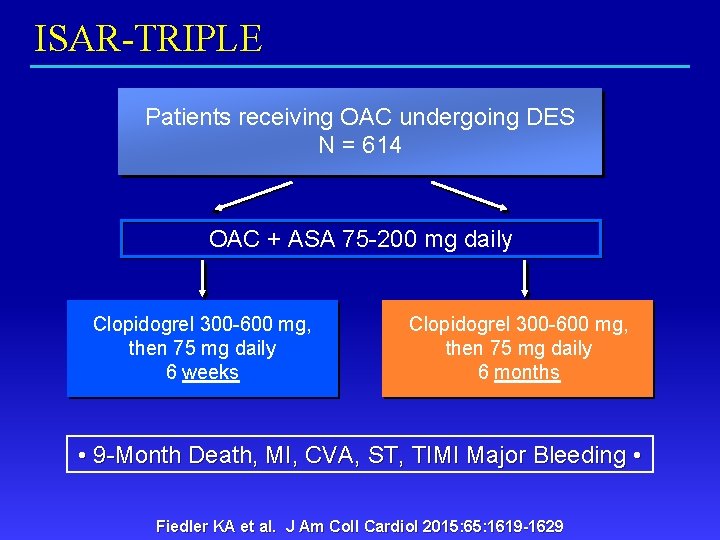
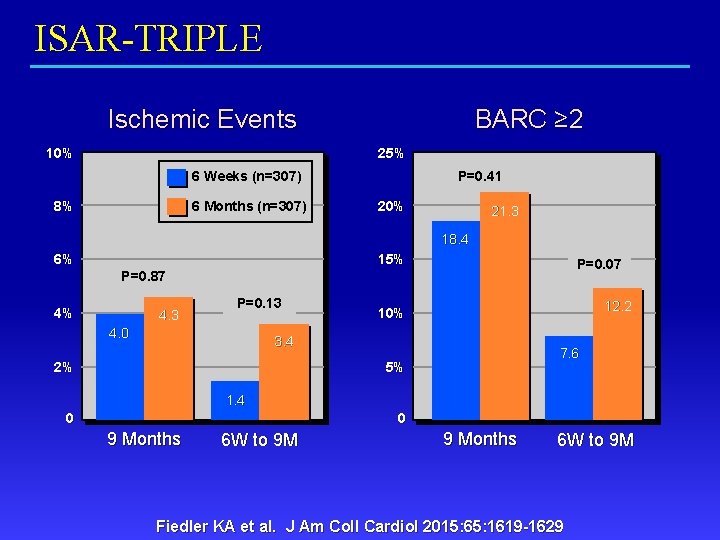
ISAR-TRIPLE Patients receiving OAC undergoing DES N = 614 OAC + ASA 75 -200 mg daily Clopidogrel 300 -600 mg, then 75 mg daily 6 weeks Clopidogrel 300 -600 mg, then 75 mg daily 6 months • 9 -Month Death, MI, CVA, ST, TIMI Major Bleeding • Fiedler KA et al. J Am Coll Cardiol 2015: 65: 1619 -1629
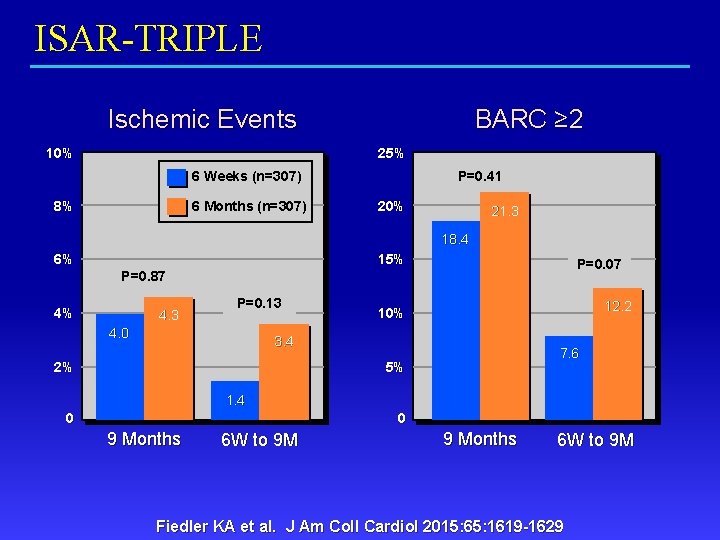
ISAR-TRIPLE Ischemic Events 10% BARC ≥ 2 25% 6 Weeks (n=307) 8% 6 Months (n=307) P=0. 41 20% 21. 3 18. 4 6% 15% P=0. 07 P=0. 87 4% 4. 3 P=0. 13 4. 0 12. 2 10% 3. 4 2% 7. 6 5% 1. 4 0 0 9 Months 6 W to 9 M Fiedler KA et al. J Am Coll Cardiol 2015: 65: 1619 -1629
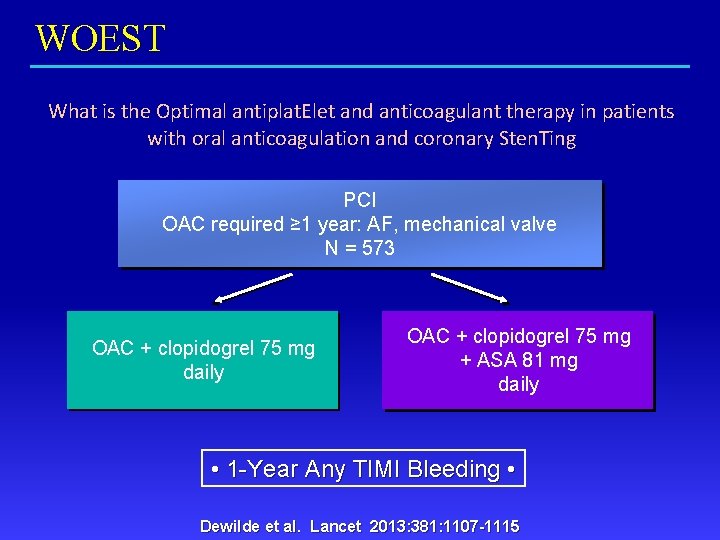
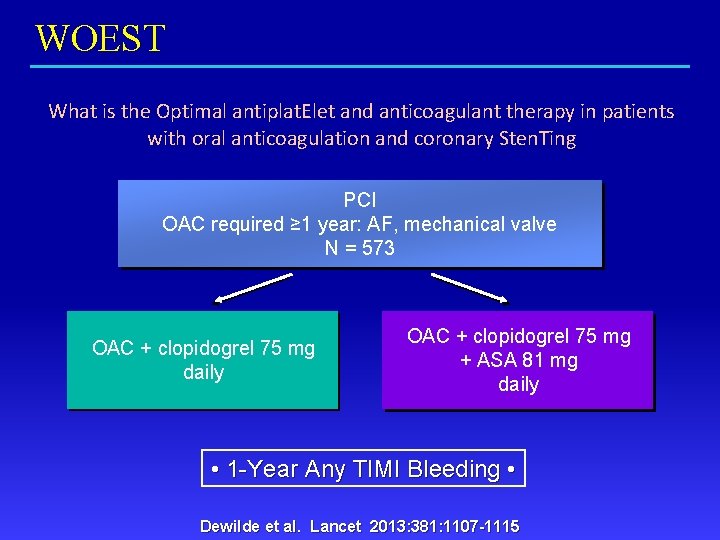
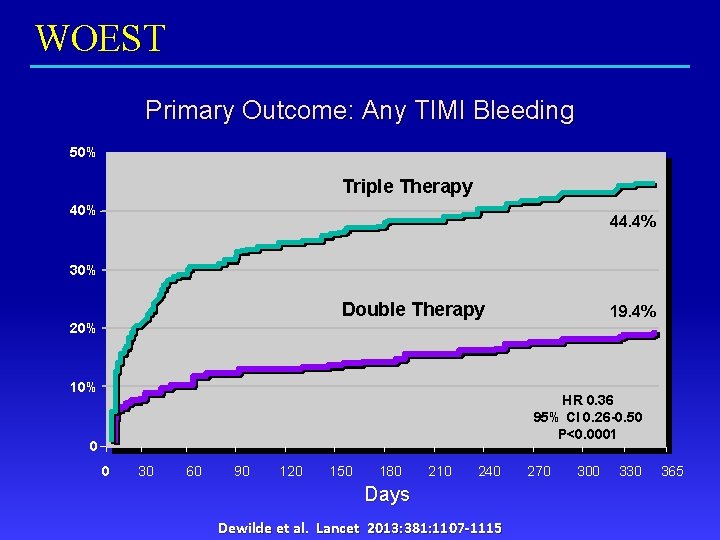
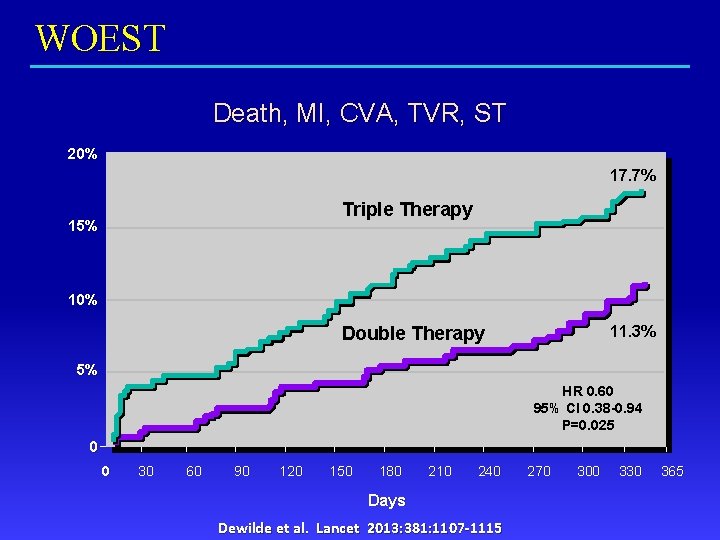
WOEST What is the Optimal antiplat. Elet and anticoagulant therapy in patients with oral anticoagulation and coronary Sten. Ting PCI OAC required ≥ 1 year: AF, mechanical valve N = 573 OAC + clopidogrel 75 mg daily OAC + clopidogrel 75 mg + ASA 81 mg daily • 1 -Year Any TIMI Bleeding • Dewilde et al. Lancet 2013: 381: 1107 -1115
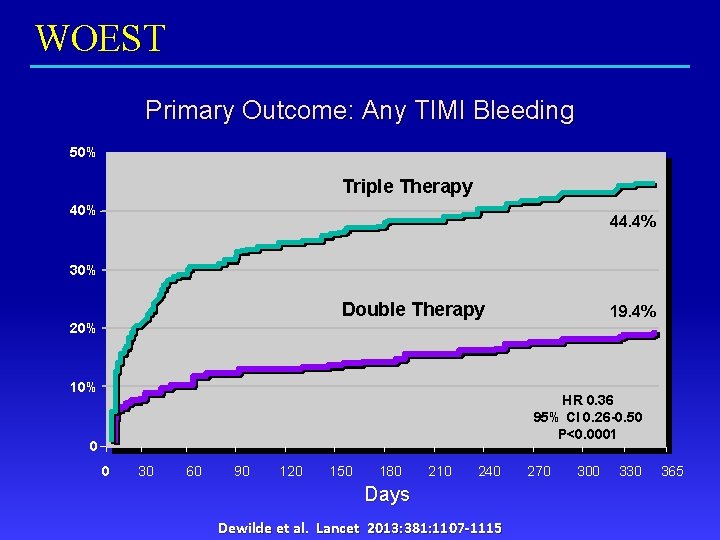
WOEST Primary Outcome: Any TIMI Bleeding 50% Triple Therapy 40% 44. 4% 30% Double Therapy 19. 4% 20% 10% HR 0. 36 95% CI 0. 26 -0. 50 P<0. 0001 0 0 30 60 90 120 150 180 210 240 Days Dewilde et al. Lancet 2013: 381: 1107 -1115 270 300 330 365
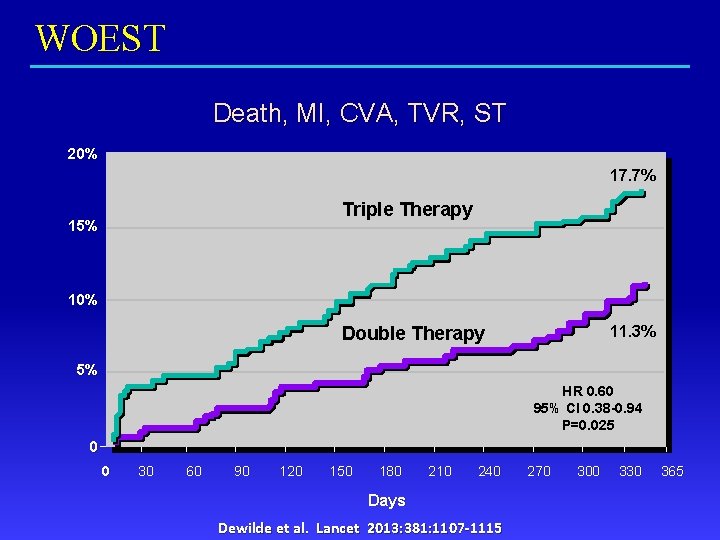
WOEST Death, MI, CVA, TVR, ST 20% 17. 7% Triple Therapy 15% 10% 11. 3% Double Therapy 5% HR 0. 60 95% CI 0. 38 -0. 94 P=0. 025 0 0 30 60 90 120 150 180 210 240 Days Dewilde et al. Lancet 2013: 381: 1107 -1115 270 300 330 365
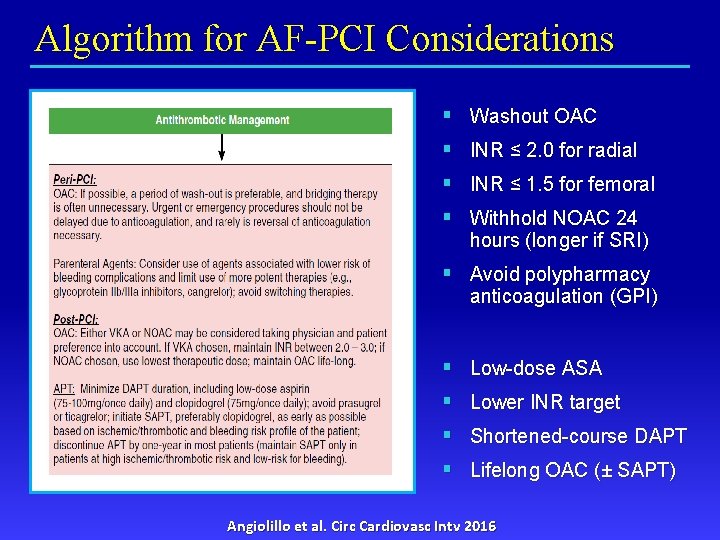
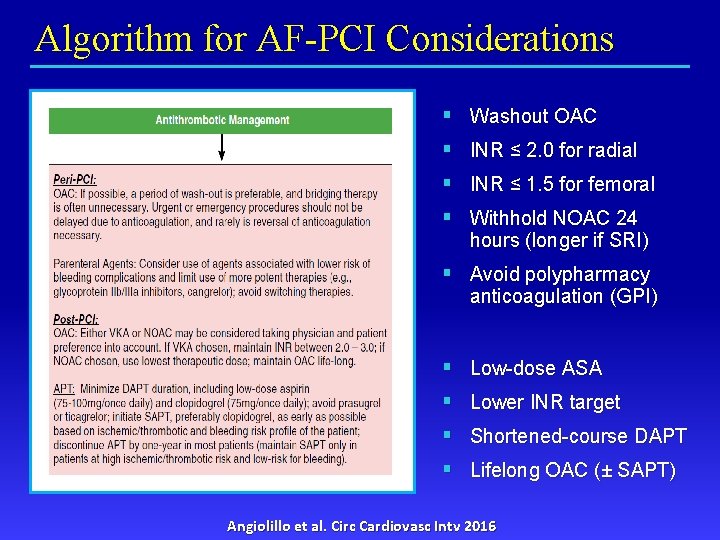
Algorithm for AF-PCI Considerations § Washout OAC § INR ≤ 2. 0 for radial § INR ≤ 1. 5 for femoral § Withhold NOAC 24 hours (longer if SRI) § Avoid polypharmacy anticoagulation (GPI) § Low-dose ASA § Lower INR target § Shortened-course DAPT § Lifelong OAC (± SAPT) Angiolillo et al. Circ Cardiovasc Intv 2016
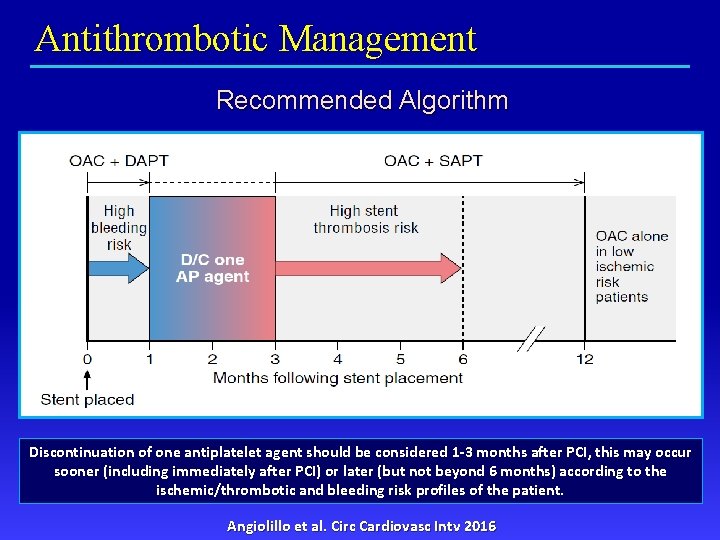
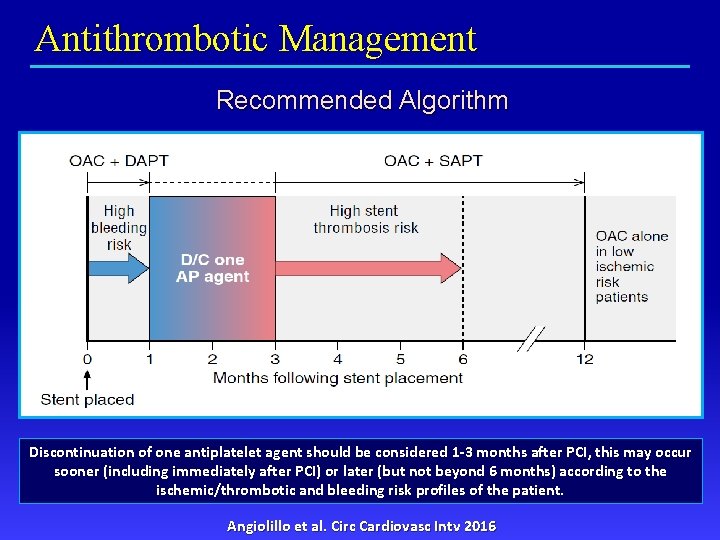
Antithrombotic Management Recommended Algorithm Discontinuation of one antiplatelet agent should be considered 1 -3 months after PCI, this may occur sooner (including immediately after PCI) or later (but not beyond 6 months) according to the ischemic/thrombotic and bleeding risk profiles of the patient. Angiolillo et al. Circ Cardiovasc Intv 2016
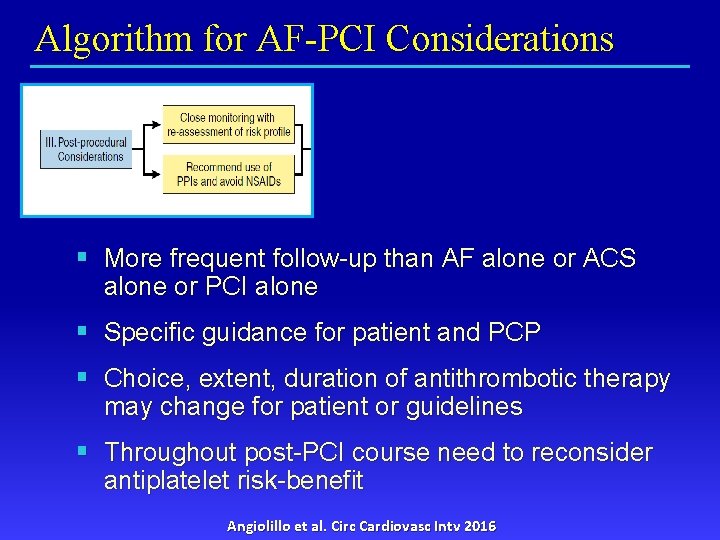
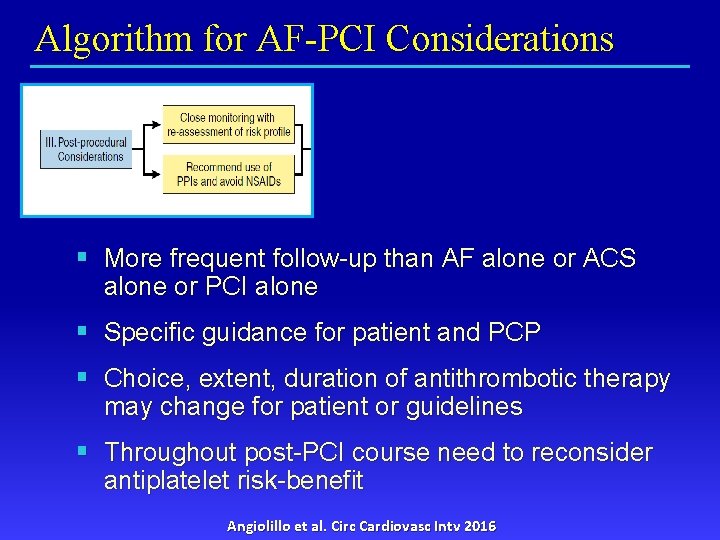
Algorithm for AF-PCI Considerations § More frequent follow-up than AF alone or ACS alone or PCI alone § Specific guidance for patient and PCP § Choice, extent, duration of antithrombotic therapy may change for patient or guidelines § Throughout post-PCI course need to reconsider antiplatelet risk-benefit Angiolillo et al. Circ Cardiovasc Intv 2016
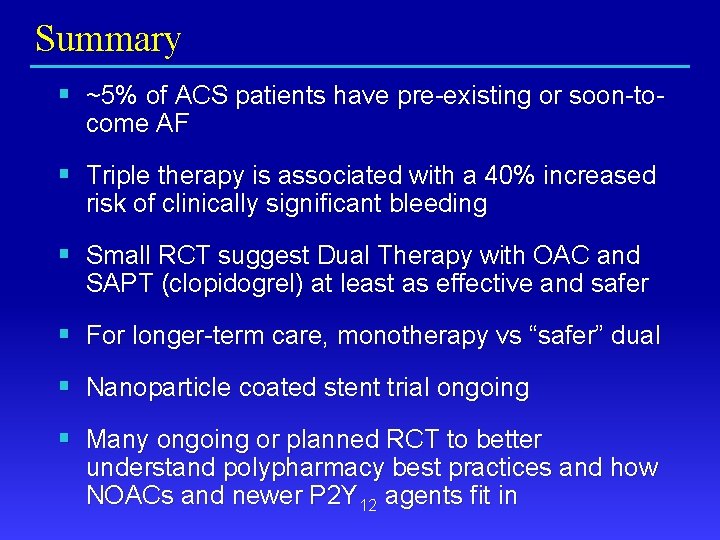
Summary § ~5% of ACS patients have pre-existing or soon-tocome AF § Triple therapy is associated with a 40% increased risk of clinically significant bleeding § Small RCT suggest Dual Therapy with OAC and SAPT (clopidogrel) at least as effective and safer § For longer-term care, monotherapy vs “safer” dual § Nanoparticle coated stent trial ongoing § Many ongoing or planned RCT to better understand polypharmacy best practices and how NOACs and newer P 2 Y 12 agents fit in
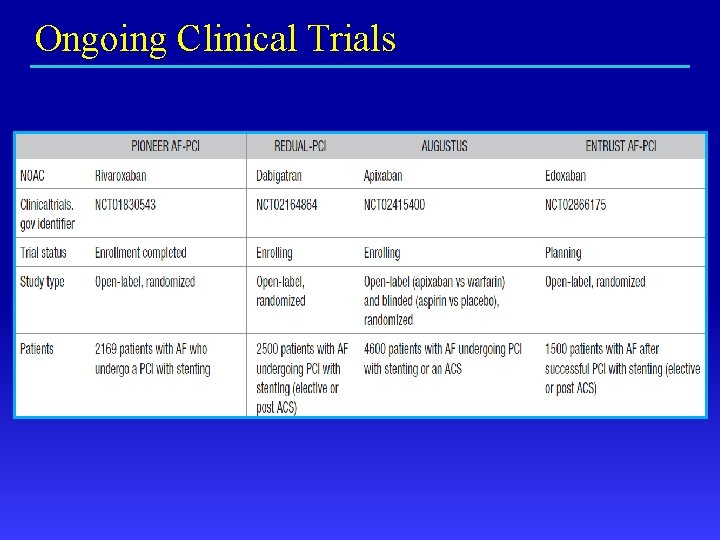
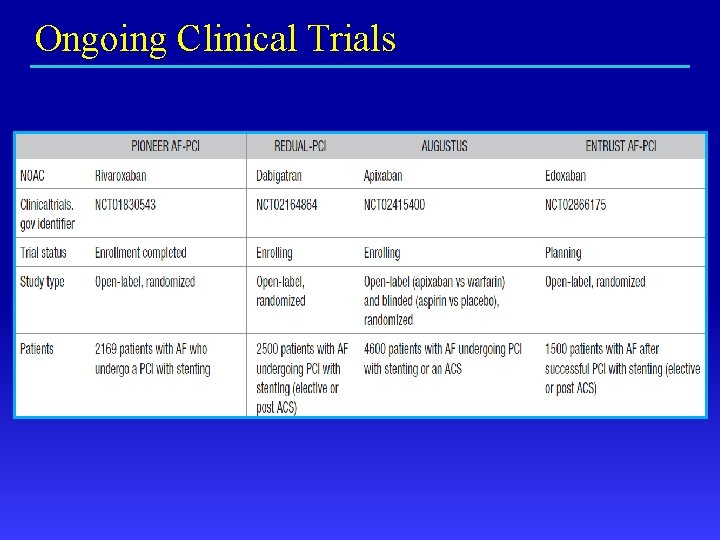
Ongoing Clinical Trials
Polypharmacy Anticoagulation: AF meets PCI David J. Moliterno, MD Professor and Chairman Department of Internal Medicine The University of Kentucky Linda and Jack Gill Heart Institute
 David moliterno md
David moliterno md Alison moliterno
Alison moliterno Warfarin dosing chart
Warfarin dosing chart Overlake anticoagulation clinic
Overlake anticoagulation clinic Coumadin clinic emory
Coumadin clinic emory Anticoagulation
Anticoagulation Lahey coumadin clinic
Lahey coumadin clinic Anticoagulation
Anticoagulation Pbs hospital medication chart
Pbs hospital medication chart Tripple therapy
Tripple therapy Cardioversion anticoagulation
Cardioversion anticoagulation Generally restful like the horizon where the sky meets land
Generally restful like the horizon where the sky meets land Newton meets buzz and woody
Newton meets buzz and woody Limnetic zone
Limnetic zone Death of achilles
Death of achilles The congress of vienna meets
The congress of vienna meets Approaches meets masters
Approaches meets masters Business intelligence in higher education
Business intelligence in higher education A generally restful like the horizon
A generally restful like the horizon Macbeth meets the witches
Macbeth meets the witches How does huck feel about not turning jim in
How does huck feel about not turning jim in