Pituitary and hypothalamic diseases Dr Malith Kumarasinghe MBBS
Pituitary and hypothalamic diseases Dr. Malith Kumarasinghe MBBS( Colombo)
Overview n n n Anatomy and physiology Pituitary disorders Hypothalamic disorders
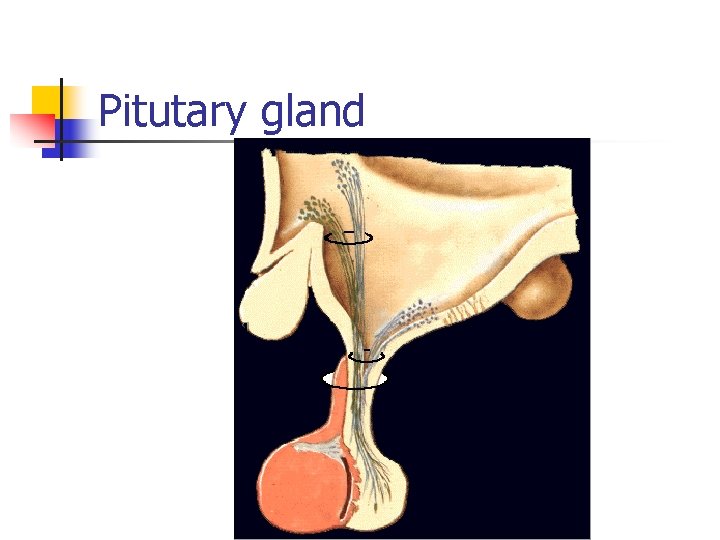
Pitutary gland
n Location n Sella turcica Floor of the brain Parts of the Pituitary Gland n n Anterior Pituitary Posterior Pituitary
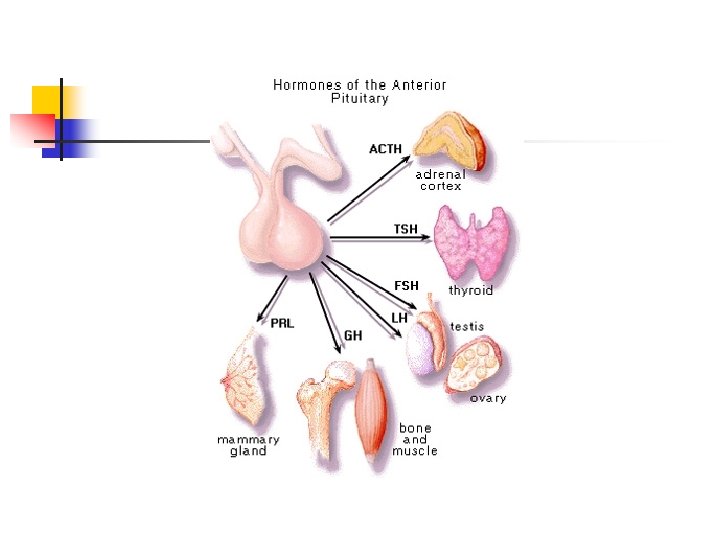
n Anterior Lobe Hormones n n n Growth Hormone Prolactin Thyroid Stimulating Hormone TSH Adreno. Cortico. Trophic Hormone ACTH Follicle Stimulating Hormone Lutenizing Hormone
Posterior pituitary hormones n Oxytocin n Milk ejection mechanism Uterine Contraction Vasopressin or ADH
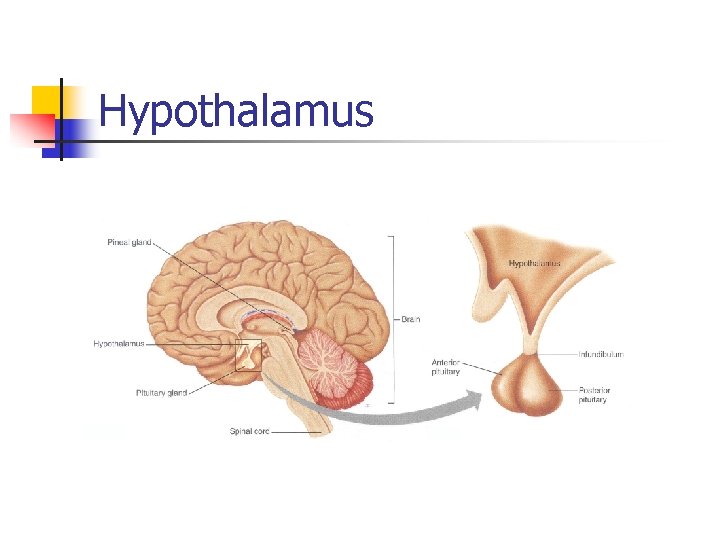
Hypothalamus
n Lies superior to the pituitary at the base of the brain
Hypothalamic functions n n homeostasis. controls the autonomic nervous system, regulates eating and drinking, controls body temperature controls pituitary gland secretions.
Hypothalamic actions on the pituitary Posterior pituitary The hypothalamic nuclei produce ADH and oxytocin. These move down the axon and are stored in the posterior pituitary. Following stimulation of the hypothalamus these hormones are then released into the bloodstream.
Anterior pituitary the hypothalamus is linked to the anterior pituitary by a network of microcapillaries Control is maintained by release of hypothalamic hormones, some of which stimulate release and others inhibit release of pituitary hormones
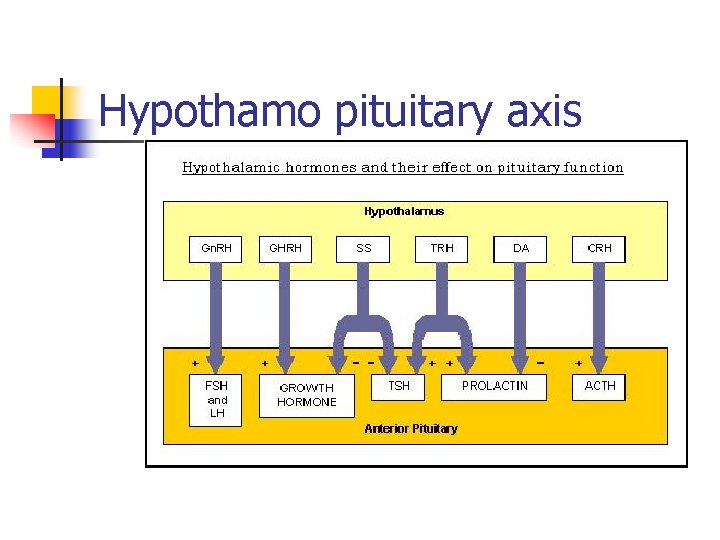
Hypothamo pituitary axis
Pituitary disorders Tumors primary benign non functional adenomas macroadenoma/microadenoma malignant secondary n
n n n Infections Infiltrative diseases TB Vascular disorders Sheehans syndrome
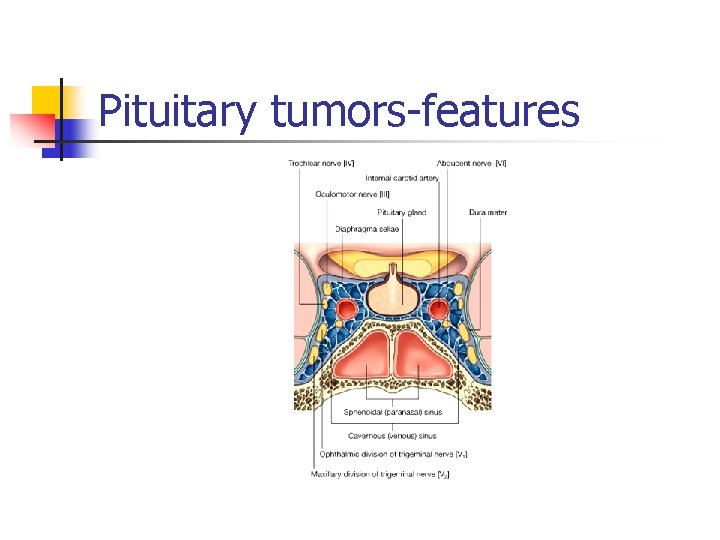
Pituitary tumors features
Pituitary tumors features n n Pituitary tumors may produce one or more hormones causing endocrine dysfunction Some pituitary tumors compress rest of the gland causing deficiency of hormones
Pituitary tumors features Symptoms caused by pressure from a larger pituitary tumor n Headache n Visual changes n n Double vision Visual field loss
Hypopituitarism deficiency of pituitary hormones n Causes n n n Pituitary tumour Sheehan’s syndrome TB, sarcoidosis
GH deficiency n n n High body fat content fracture risk Fatigue, muscle weakness
Gonadotrophin deficiency n Male n n testicular volume Loss of facial & body hair sexual function and libido Female n n Amenorrhoea Vaginal dryness
ACTH deficiency n n n Weakness, tiredness Hypotension Vomiting Hypoglycaemia Hyponatraemia Myalgia
TSH deficiency n Features of hypothyroidism
Investigation of hypopituitarism
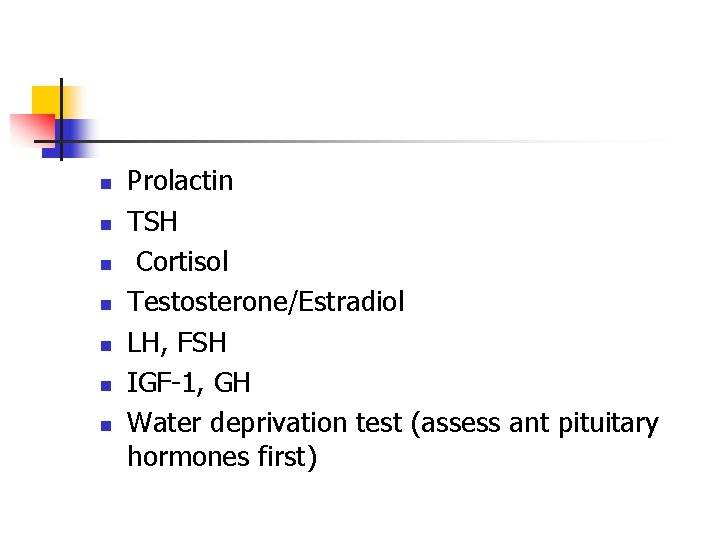
n n n n Prolactin TSH Cortisol Testosterone/Estradiol LH, FSH IGF 1, GH Water deprivation test (assess ant pituitary hormones first)
Treatment of hypopituitarism
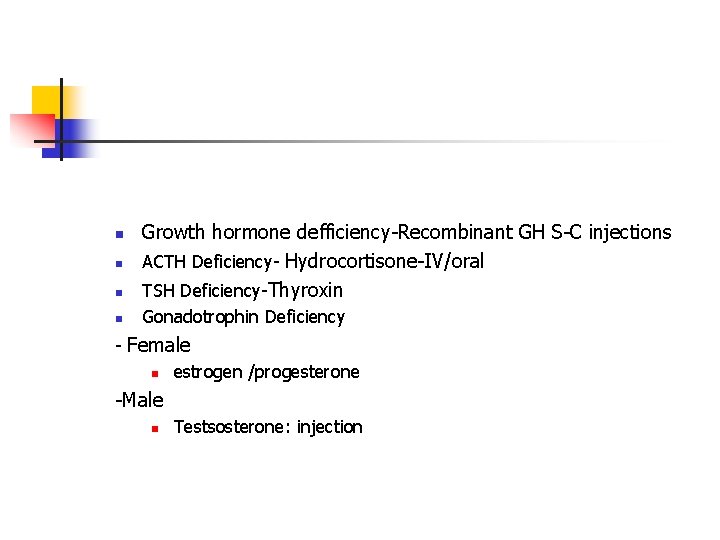
n Growth hormone defficiency Recombinant GH S C injections ACTH Deficiency Hydrocortisone IV/oral TSH Deficiency Thyroxin n Gonadotrophin Deficiency n n Female n estrogen /progesterone Male n Testsosterone: injection
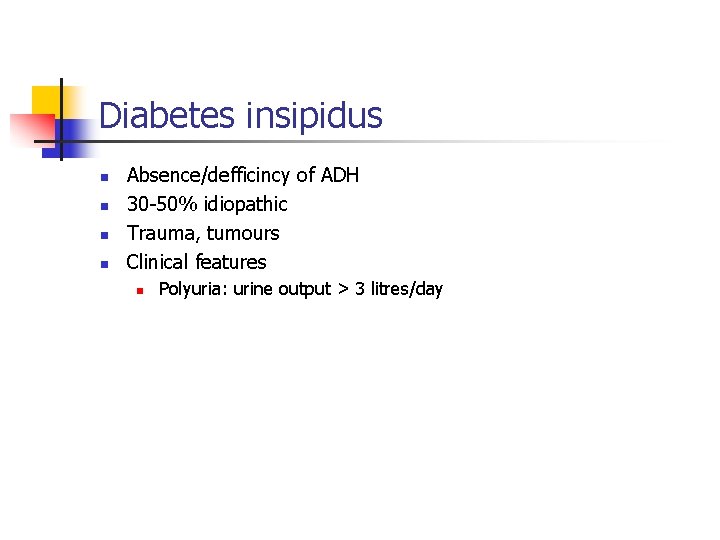
Diabetes insipidus n n Absence/defficincy of ADH 30 50% idiopathic Trauma, tumours Clinical features n Polyuria: urine output > 3 litres/day
Investigation, treatment n Water deprivation test n n n Normal: urine osmolality rises in water deprivation DI: Urine fails to concentrate ADH deficiency: urine osmolality with desmopressin Nephrogenic DI: no response to desmopressin Treatment n Desmopressin n Nasal fluid/aerosol, tablet
Pituitary hormone excess
GH excess n Causes n Pituitary tumour causing high secretion growth hormone
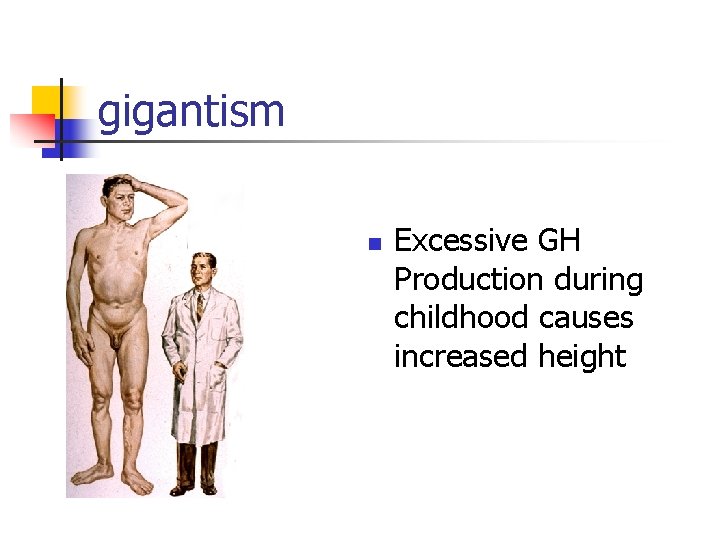
gigantism n Excessive GH Production during childhood causes increased height
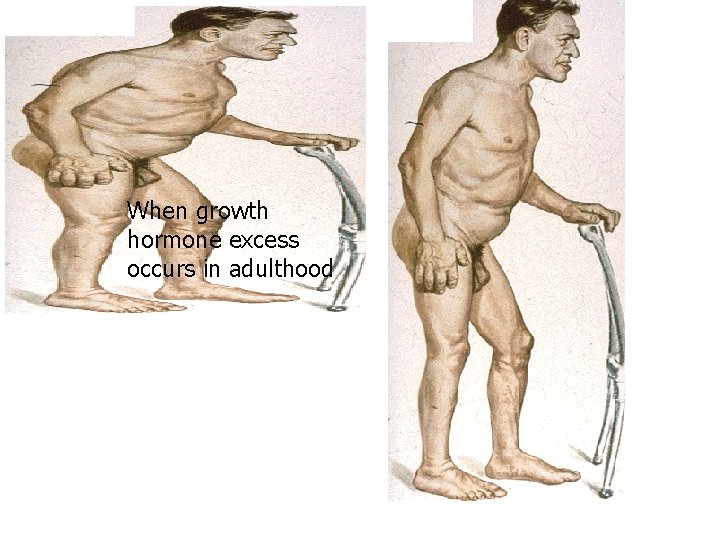
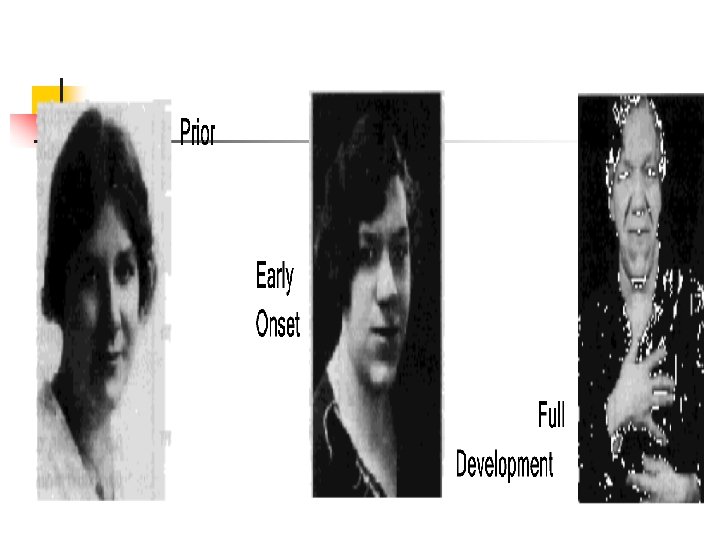
acromegaly When growth hormone excess occurs in adulthood
Clinical features n n n Enlargement of hands, altered shoe and ring size sweating Thyroid enlargement Sleep apnoea Diabetes, hypertension Colonic polyps, GI malignancies
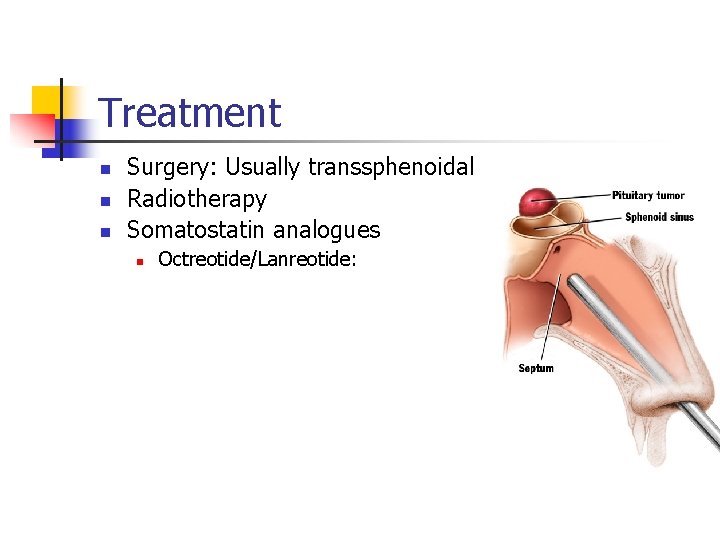
Treatment n n n Surgery: Usually transsphenoidal Radiotherapy Somatostatin analogues n Octreotide/Lanreotide:
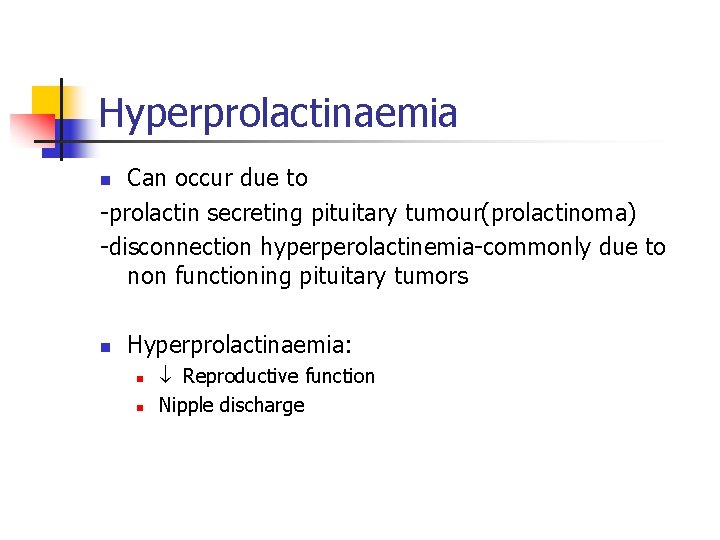
Hyperprolactinaemia Can occur due to prolactin secreting pituitary tumour(prolactinoma) disconnection hyperperolactinemia commonly due to non functioning pituitary tumors n n Hyperprolactinaemia: n n Reproductive function Nipple discharge
Treatment n Dopamine agonists: n Bromocriptine Surgery
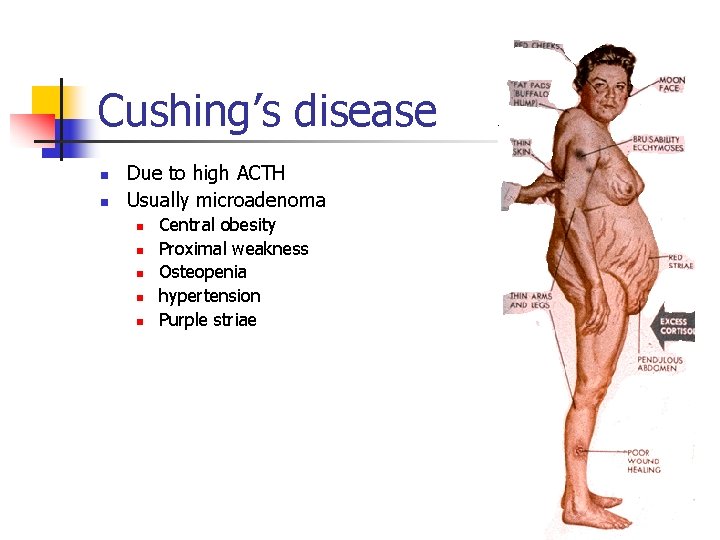
Cushing’s disease n n Due to high ACTH Usually microadenoma n n n Central obesity Proximal weakness Osteopenia hypertension Purple striae

Treatment n Pituitary surgery n Radiotherapy
Hypothalamic disorders Causes trauma malignancy malnutrition anorrexia nervosa n
Features n n n Endocrine dysfunction Eating disorders Problems related to autonomic control
Questions ….
- Slides: 43