PHM 226 Example Instructor Dr Jeffrey Henderson HEMOLYTIC
- Slides: 16
PHM 226, Example Instructor: Dr. Jeffrey Henderson HEMOLYTIC ANEMIA Presented by: Ally Dhalla ally_dhalla@hotmail. com Sandeep Gothi deepsand@hotmail. com Ujjwal Patel patel_ujjwal@hotmail. com Presented JAN 20 2004
What is hemolytic anemia? • Hemolytic anemia is a disorder in which the red blood cells are destroyed prematurely. • RBCs are destroyed faster than the bone marrow can produce them. • There are two types of hemolytic anemia: Extrinsic and Intrinsic
Types of Hemolytic Anemia • Extrinsic - red blood cells are produced healthy but are later destroyed by becoming trapped in the spleen, destroyed by infection, or destroyed from drugs that can affect red blood cells. • Intrinsic - the destruction of the red blood cells due to a defect within the red blood cells themselves. Intrinsic hemolytic anemia is often inherited, such as sickle cell anemia and Glucose-6 -Phosphate Dehydrogenase deficiency. (G 6 PD)
What is G 6 PD? • It is an X-linked recessive inheritance. (males usually affected and females are carriers) • Risk factors: being black, being male, or having a family history of G 6 PD deficiency. • G 6 PD enzyme functions in the Pentose-Monophosphate shunt and in the process, catalyzes the reduction of NADP+ to NADPH required in triggering a cascade of events that can detoxify the harmful oxidant H 2 O 2.
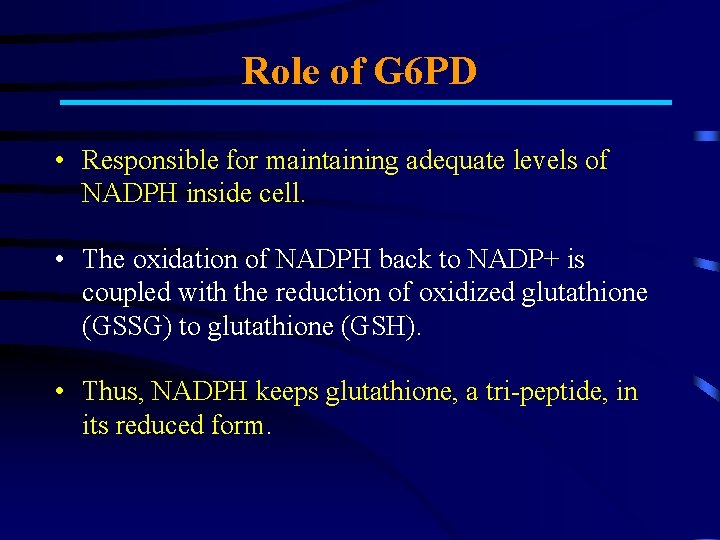
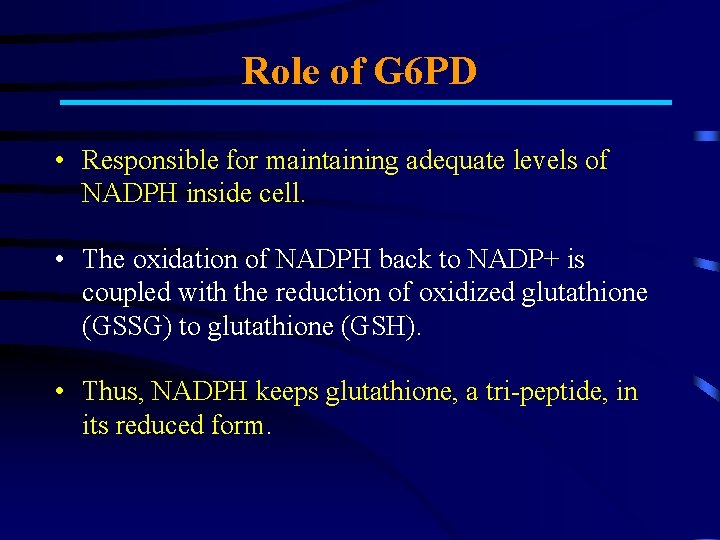
Role of G 6 PD • Responsible for maintaining adequate levels of NADPH inside cell. • The oxidation of NADPH back to NADP+ is coupled with the reduction of oxidized glutathione (GSSG) to glutathione (GSH). • Thus, NADPH keeps glutathione, a tri-peptide, in its reduced form.
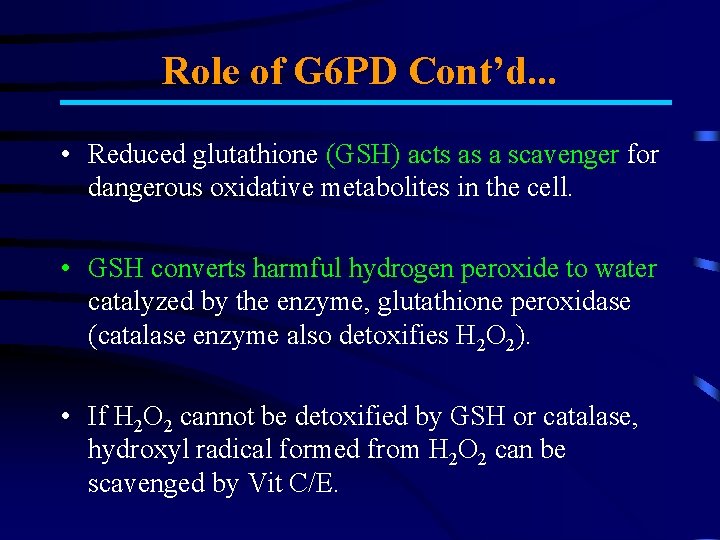
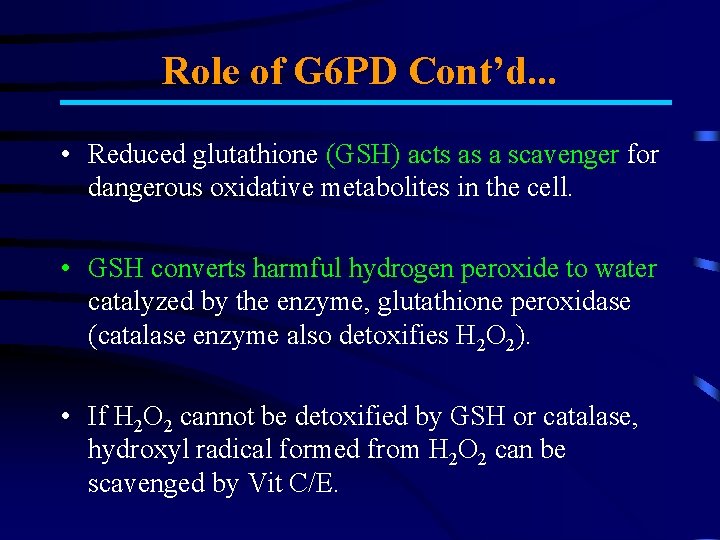
Role of G 6 PD Cont’d. . . • Reduced glutathione (GSH) acts as a scavenger for dangerous oxidative metabolites in the cell. • GSH converts harmful hydrogen peroxide to water catalyzed by the enzyme, glutathione peroxidase (catalase enzyme also detoxifies H 2 O 2). • If H 2 O 2 cannot be detoxified by GSH or catalase, hydroxyl radical formed from H 2 O 2 can be scavenged by Vit C/E.
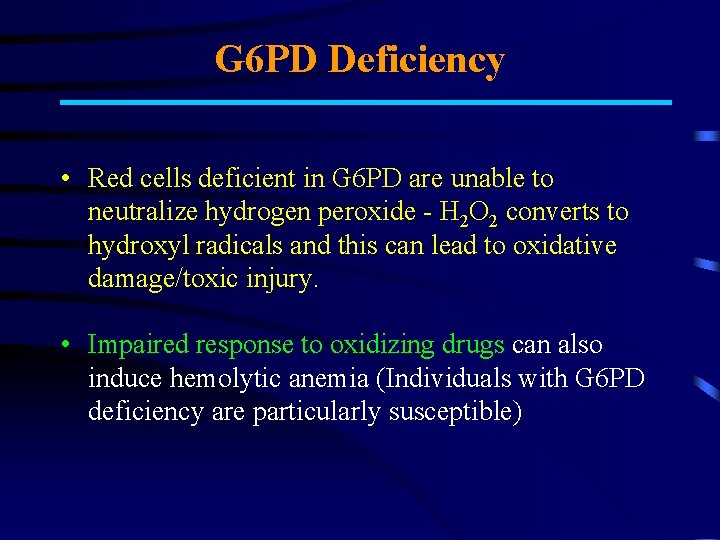
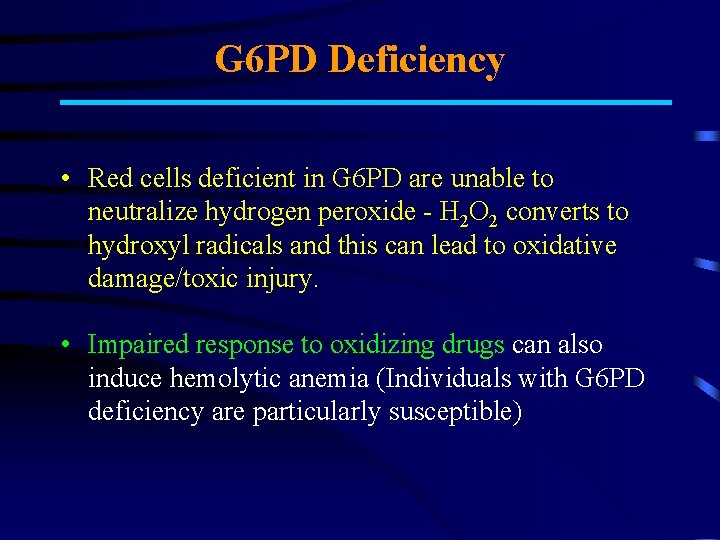
G 6 PD Deficiency • Red cells deficient in G 6 PD are unable to neutralize hydrogen peroxide - H 2 O 2 converts to hydroxyl radicals and this can lead to oxidative damage/toxic injury. • Impaired response to oxidizing drugs can also induce hemolytic anemia (Individuals with G 6 PD deficiency are particularly susceptible)
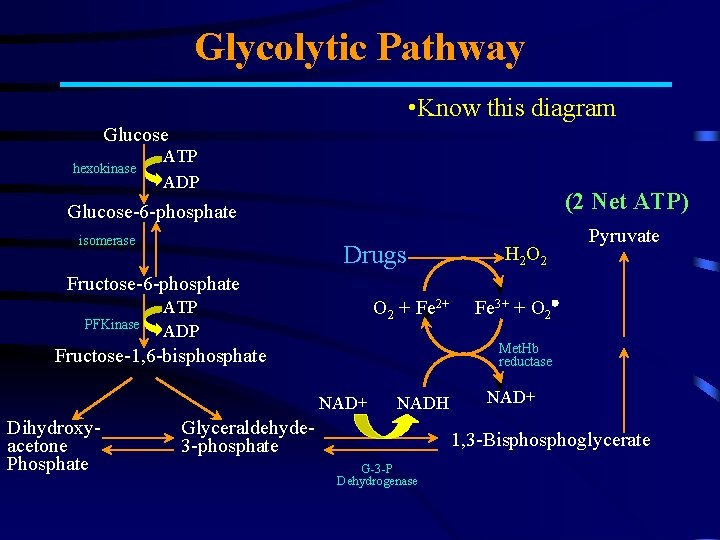
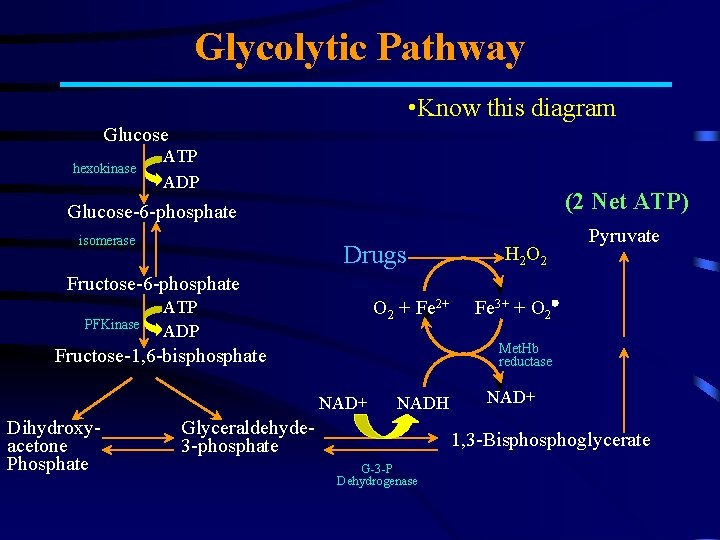
Glycolytic Pathway • Know this diagram Glucose hexokinase ATP ADP (2 Net ATP) Glucose-6 -phosphate isomerase Drugs H 2 O 2 Pyruvate Fructose-6 -phosphate PFKinase O 2 + Fe 2+ ATP ADP Met. Hb reductase Fructose-1, 6 -bisphosphate NAD+ Dihydroxyacetone Phosphate Fe 3+ + O 2 NADH Glyceraldehyde 3 -phosphate NAD+ 1, 3 -Bisphoglycerate G-3 -P Dehydrogenase
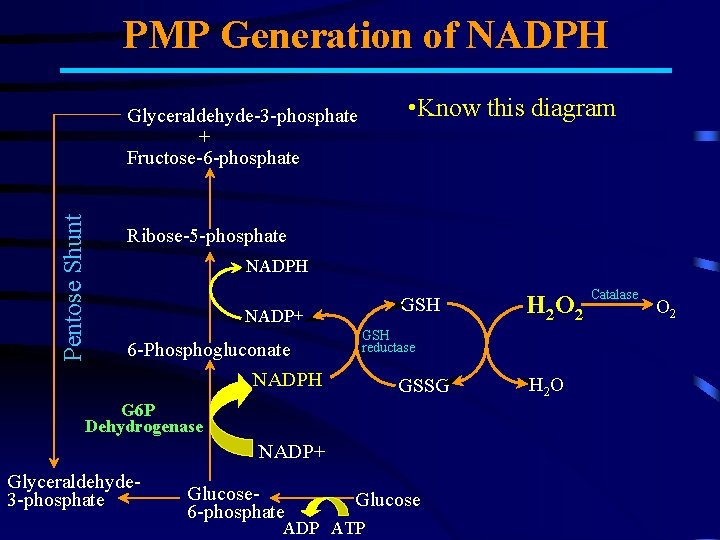
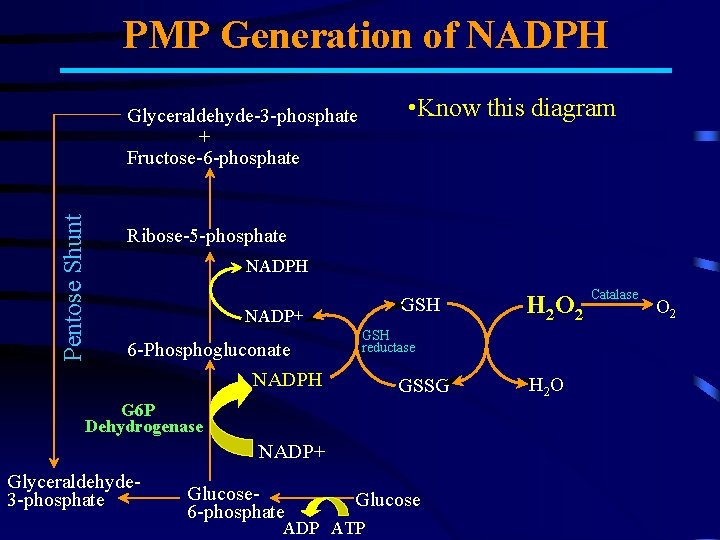
PMP Generation of NADPH • Know this diagram Pentose Shunt Glyceraldehyde-3 -phosphate + Fructose-6 -phosphate Ribose-5 -phosphate NADPH GSH NADP+ 6 -Phosphogluconate NADPH GSH reductase GSSG G 6 P Dehydrogenase NADP+ Glyceraldehyde 3 -phosphate Glucose 6 -phosphate H 2 O 2 Glucose ADP ATP H 2 O Catalase O 2
Drugs that affect it • Drugs that can precipitate this reaction include: · anti-malarial agents · sulfonamides (antibiotic) · aspirin · non-steroidal anti-inflammatory drugs (NSAIDs) · nitrofurantoin · quinidine · quinine · others • Also: exposure to certain chemicals such as those in mothballs and flava beans.
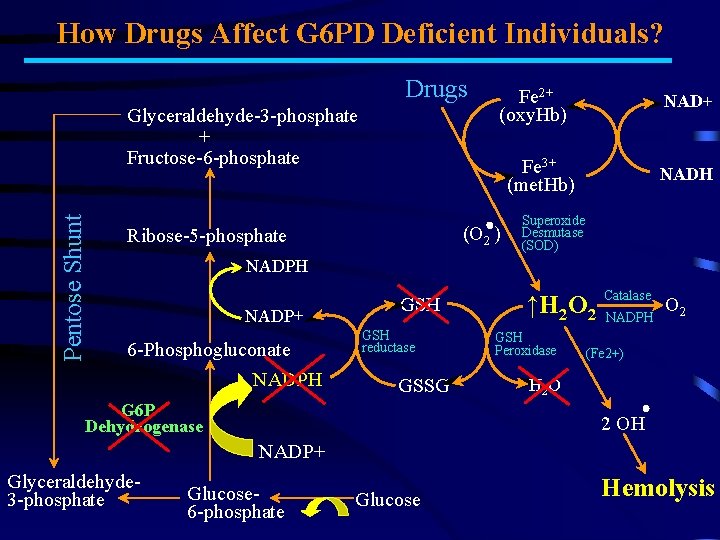
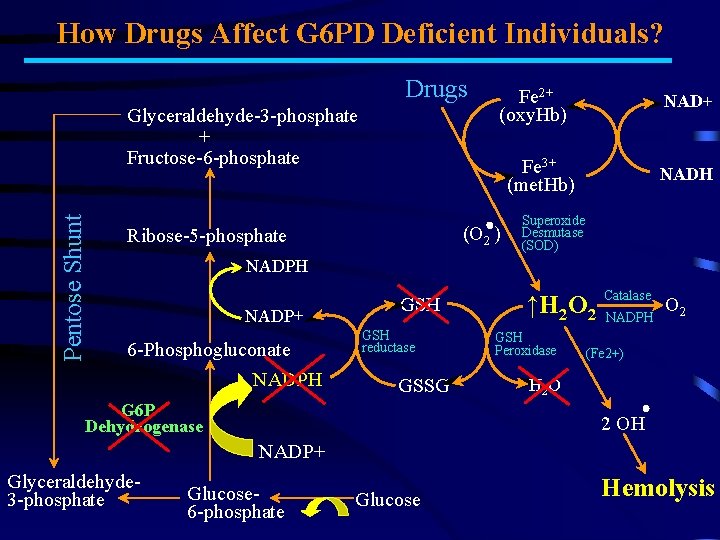
How Drugs Affect G 6 PD Deficient Individuals? Drugs Pentose Shunt Glyceraldehyde-3 -phosphate + Fructose-6 -phosphate Fe 2+ (oxy. Hb) NAD+ Fe 3+ (met. Hb) (O 2 ) Ribose-5 -phosphate NADH Superoxide Desmutase (SOD) NADPH NADP+ 6 -Phosphogluconate NADPH GSH reductase GSSG G 6 P Dehydrogenase ↑H 2 O 2 GSH Peroxidase Catalase NADPH O 2 (Fe 2+) H 2 OH NADP+ Glyceraldehyde 3 -phosphate Glucose 6 -phosphate Glucose Hemolysis
What are the symptoms? • The most common symptoms include: – – – – abnormal paleness or lack of color of the skin jaundice, or yellowing of the skin, eyes, and mouth dark color to urine fever weakness dizziness confusion intolerance to physical activity
Signs of anemia include: • • pale skin and fingernails rapid pulse heart murmur Enlarged spleen and liver
Required Tests • Blood tests are taken to measure levels of: – red cells, assess size and shape of red cells – measure the Hb level – determine the number of reticulocytes. • Other blood tests may include: Coombs' test (direct and indirect) — checks for hemolytic anemia caused by an abnormal immune reaction. Heinz body presentation — looks for a deficiency in amount of G 6 PD enzyme, which results in hemolysis if certain medications or foods are ingested.
Treatments may include • Stopping use of offending drug. • For more severe cases, treat with: • corticosteroids (e. g. prednisone) • intravenous immunoglobulin infusions • immunosuppressive (e. g. azathioprine (Imuran) and cyclophosphamide (Cytoxan) • Vitamin and mineral supplements (e. g. folic acid). • Change in diet. • If Hb levels ↓, treatment may include blood transfusion or splenectomy (surgical removal of the spleen). • If physical damage to RBC, then treat w/ blood transfusions or simple iron supplements. • Iron - Taken during pregnancy and when iron levels are low. • Erythropoietin (Procrit) - To increase RBC production in people w/ kidney problems.
References • Ezra E. W. Cohen, M. D. , Section of Hematology/Oncology, Department of Medicine, The University of Chicago, IL. 11 Jan 2004 <http: //www. nlm. nih. gov/medlineplus/ency/article/000571. htm > • Updated by: Corey Culter, M. D. M. P. H. , F. R. C. P. C. , Department of Medical Oncology, Dana Farber Cancer INsitiute; Instructor of Medicine, Harvard University, Boston, MA. Review provided by Veri. Med Healthcare Network. Source: MEDLINEplus Medical Information. 11 Jan 2004 http: //www. hlm. nil. gov/medlineplus/ency/article/000528. htm • Ramez A. Ethnasios. An Introduction to G 6 PD Deficiency. 7 Jan 2004 <http: //www. rialto. com/g 6 pd/physiolo. htm> • Peggy Gulley, MD. Hemolytic Anemia Lecture. 9 Jan 2004 <http//: pathology. uthscsa. edu/MSII/Hemo. html> • Rebecca Elstrom, M. D. , Division of Hematology-Oncology, University of Pennsylvania Medical Center, Philadelphia, PA. Review provided by Veri. Med Healthcare Network. . 11 Jan 2004 <http: //www. umm. edu/blood/anehemol. htm> • Patrick Yorba, MD, Staff Physician, Department of Emergency Medicine, University of Virginia Health Sciences Center. 11 Jan 2004 http: //www. emedicinehealth. com/articles/4893 -6. asp? pd=1/11/2004%2010: 25: 15%20 PM • Faculty of Harvard Medical School © 1996 -2003 Aetna Inteli. Health Inc. 11 Jan 2004 <http: //www. intelihealth. com/IH/iht. IH/WSIHW 000/9339/21246. html> • Images taken from http: //health. allrefer. com/health/hemolytic-anemia-pictures-images. html>. 11 Jan 2004