Hemolytic Anemia Dr Sommanikhone PHANGMANIXAY Pediatrician General Pediatrics











- Slides: 21
Hemolytic Anemia ເລອດຈາງຈາກການແຕກຂອງເ ມດ ເລອດແດງ Dr. Sommanikhone PHANGMANIXAY Pediatrician General Pediatrics
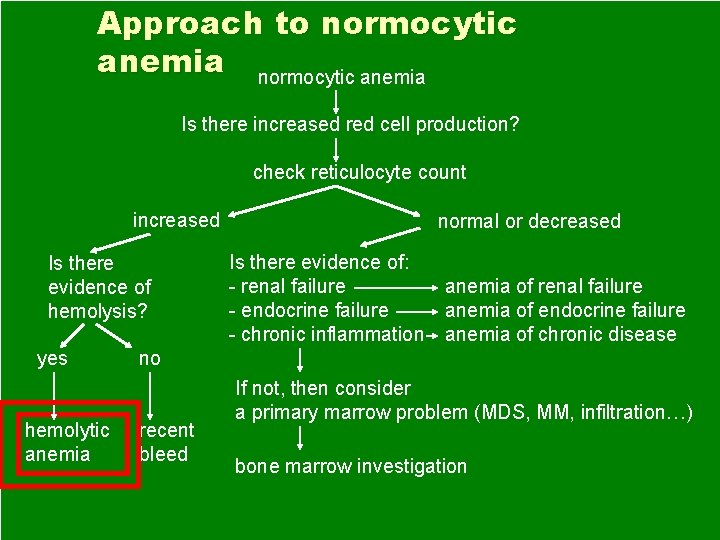
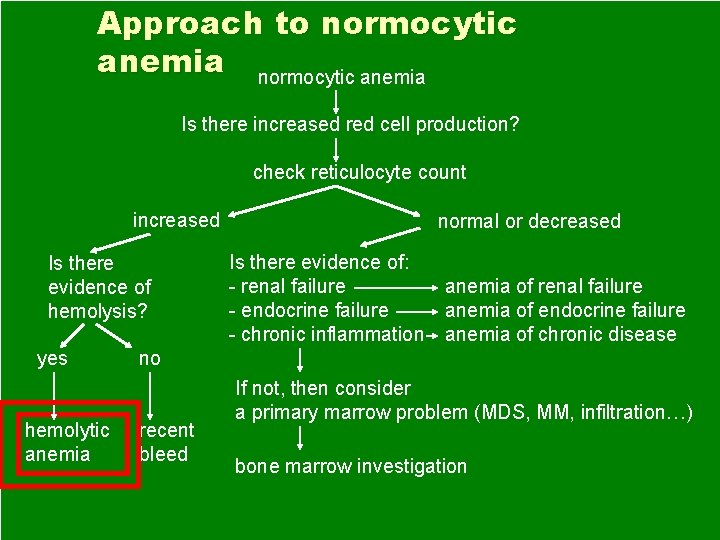
Approach to normocytic anemia Is there increased red cell production? check reticulocyte count increased Is there evidence of hemolysis? yes hemolytic anemia normal or decreased Is there evidence of: - renal failure - endocrine failure - chronic inflammation anemia of renal failure anemia of endocrine failure anemia of chronic disease no recent bleed If not, then consider a primary marrow problem (MDS, MM, infiltration…) bone marrow investigation


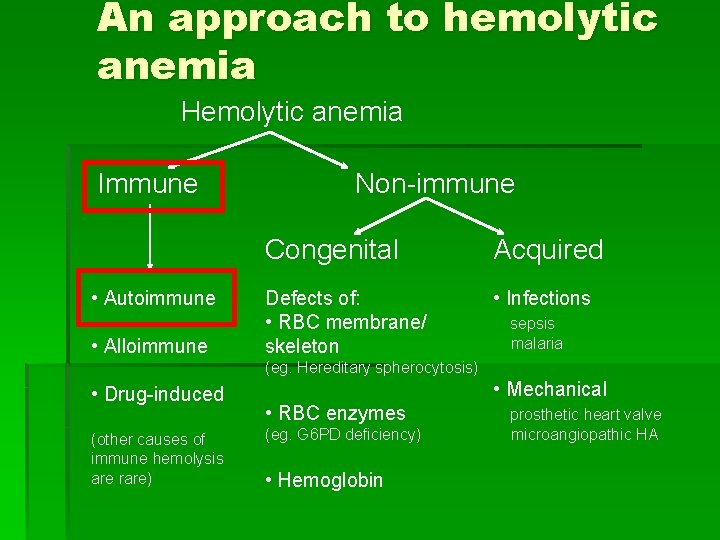
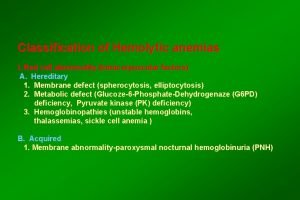
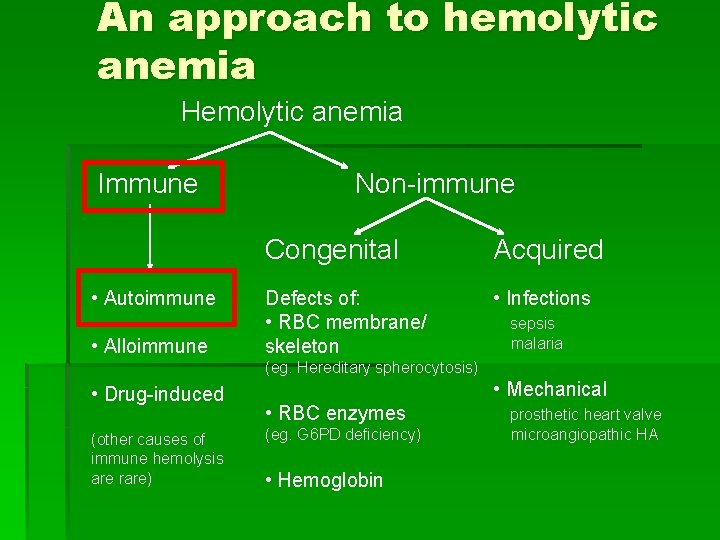
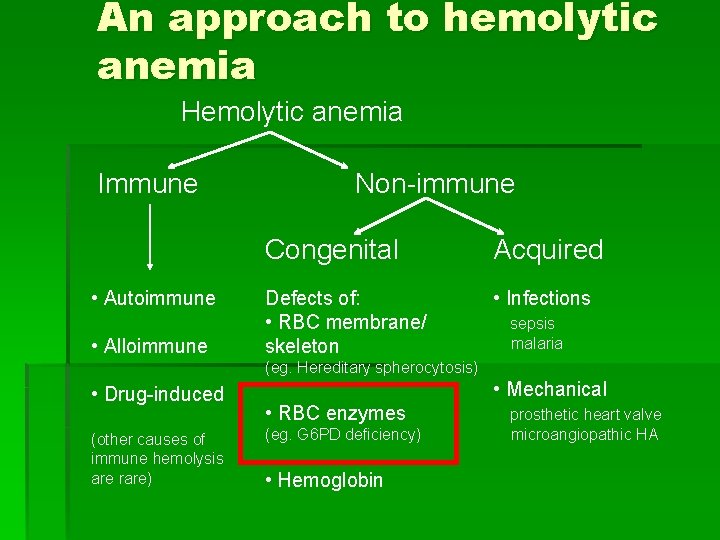
An approach to hemolytic anemia Hemolytic anemia Immune • Autoimmune • Alloimmune Non-immune Congenital Acquired Defects of: • RBC membrane/ skeleton • Infections sepsis malaria (eg. Hereditary spherocytosis) • Drug-induced (other causes of immune hemolysis are rare) • Mechanical • RBC enzymes (eg. G 6 PD deficiency) • Hemoglobin prosthetic heart valve microangiopathic HA

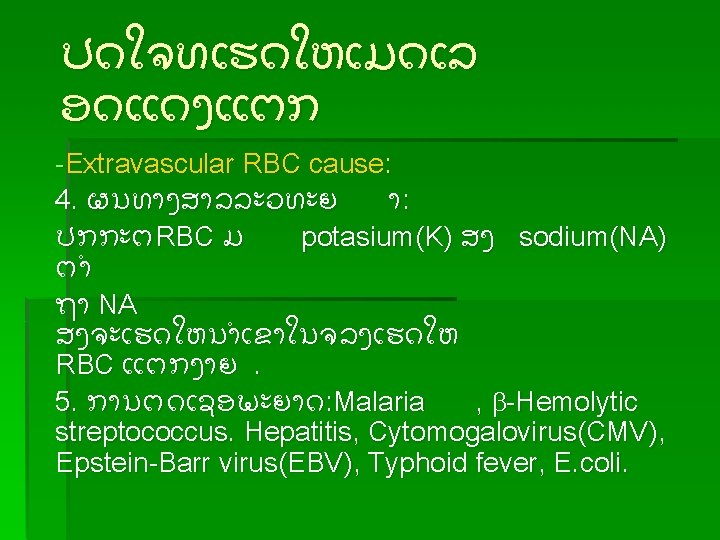
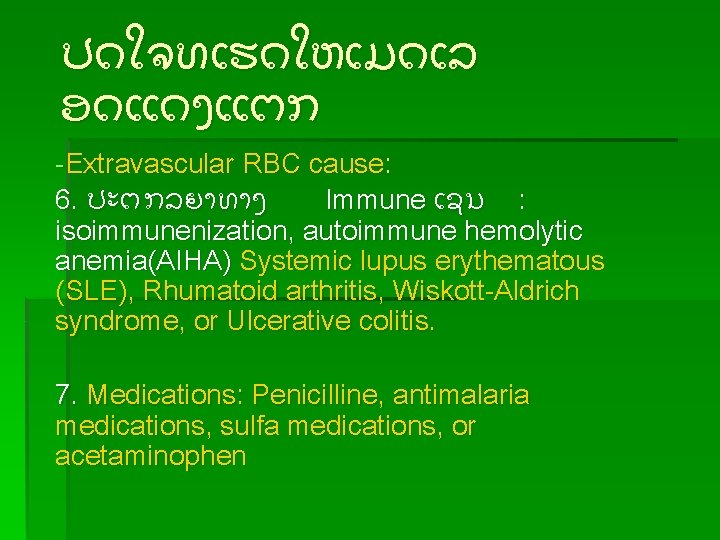
ປດໃຈທເຮດໃຫເມດເລ ອດແດງແຕກ -Extravascular RBC cause: 6. ປະຕກລຍາທາງ Immune ເຊນ : isoimmunenization, autoimmune hemolytic anemia(AIHA) Systemic lupus erythematous (SLE), Rhumatoid arthritis, Wiskott-Aldrich syndrome, or Ulcerative colitis. 7. Medications: Penicilline, antimalaria medications, sulfa medications, or acetaminophen

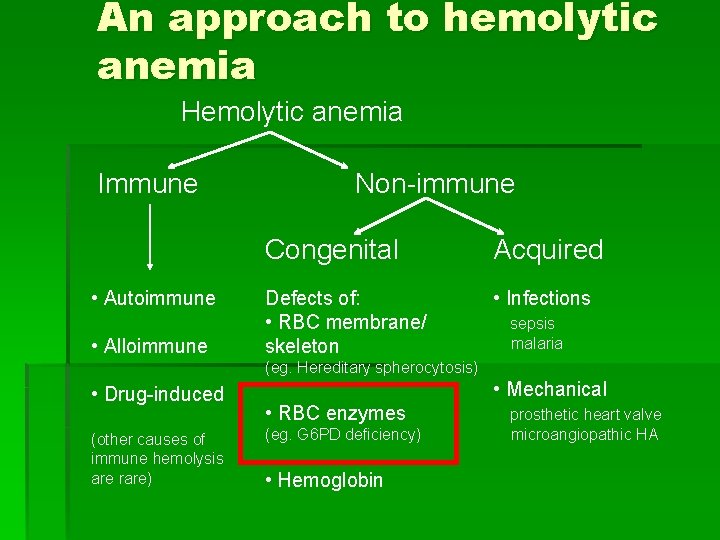
An approach to hemolytic anemia Hemolytic anemia Immune • Autoimmune • Alloimmune Non-immune Congenital Acquired Defects of: • RBC membrane/ skeleton • Infections sepsis malaria (eg. Hereditary spherocytosis) • Drug-induced (other causes of immune hemolysis are rare) • Mechanical • RBC enzymes (eg. G 6 PD deficiency) • Hemoglobin prosthetic heart valve microangiopathic HA

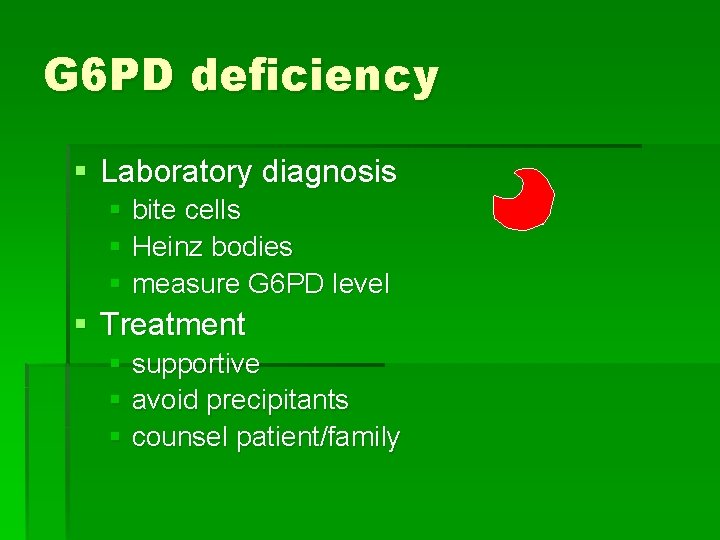
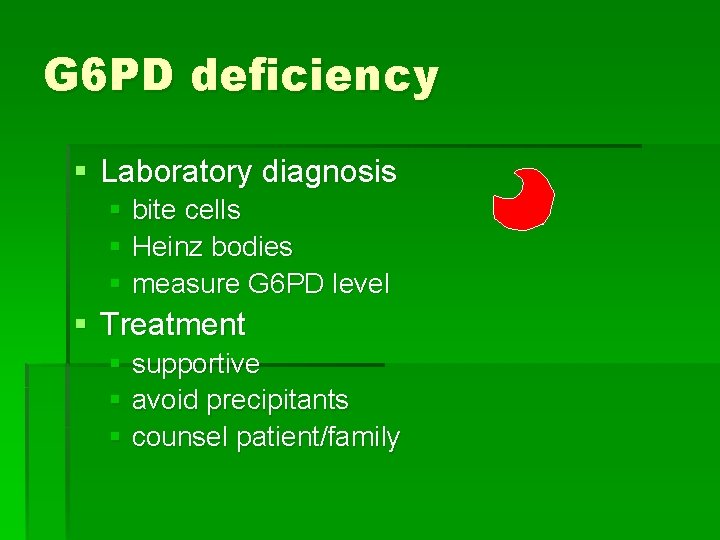
G 6 PD deficiency § Laboratory diagnosis § bite cells § Heinz bodies § measure G 6 PD level § Treatment § supportive § avoid precipitants § counsel patient/family

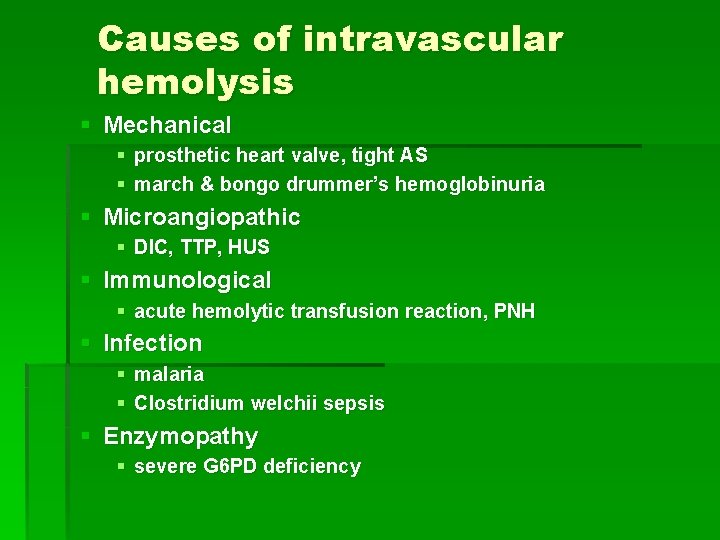
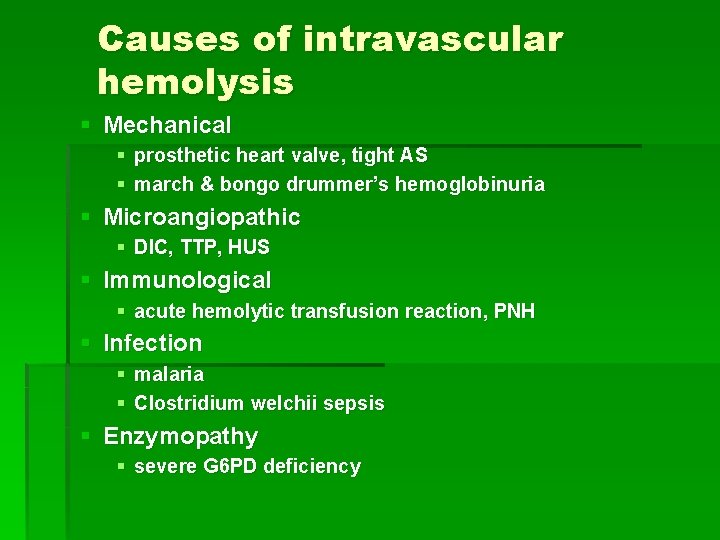
Causes of intravascular hemolysis § Mechanical § prosthetic heart valve, tight AS § march & bongo drummer’s hemoglobinuria § Microangiopathic § DIC, TTP, HUS § Immunological § acute hemolytic transfusion reaction, PNH § Infection § malaria § Clostridium welchii sepsis § Enzymopathy § severe G 6 PD deficiency

An approach to hemolytic anemia Hemolytic anemia Immune • Autoimmune • Alloimmune Non-immune Congenital Acquired Defects of: • RBC membrane/ skeleton • Infections sepsis malaria (eg. Hereditary spherocytosis) • Drug-induced (other causes of immune hemolysis are rare) • Mechanical • RBC enzymes (eg. G 6 PD deficiency) • Hemoglobin prosthetic heart valve microangiopathic HA
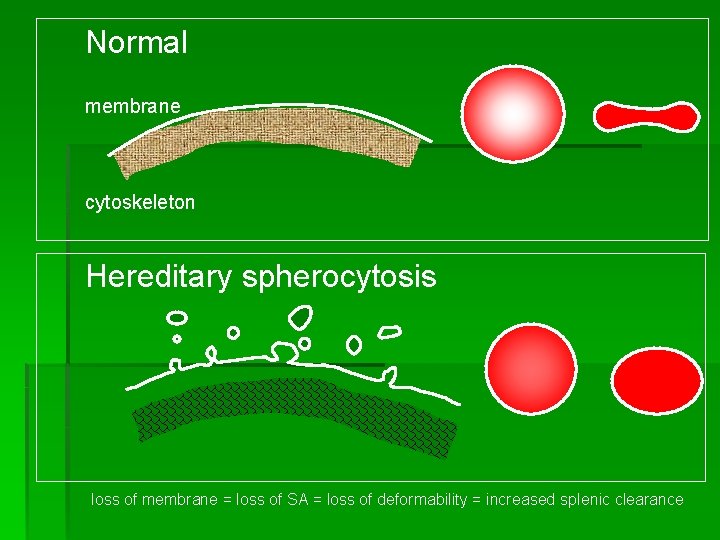
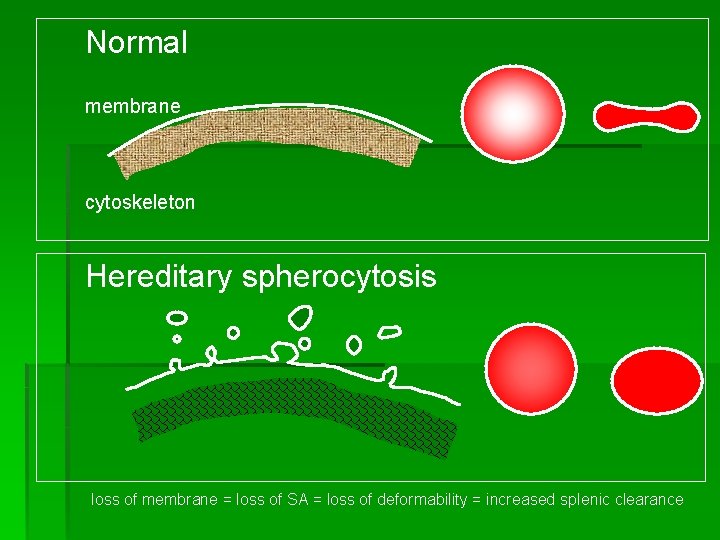
Normal membrane cytoskeleton Hereditary spherocytosis loss of membrane = loss of SA = loss of deformability = increased splenic clearance




 Hemolysis treatment
Hemolysis treatment Extracorpuscular hemolytic anemia
Extracorpuscular hemolytic anemia Types of hemolytic anemia
Types of hemolytic anemia Extrinsic hemolytic anemia
Extrinsic hemolytic anemia Treatment for hemolytic anemia
Treatment for hemolytic anemia Microangiopathic hemolytic anemia
Microangiopathic hemolytic anemia Causes of hemolysis
Causes of hemolysis Why splenomegaly in hemolytic anemia
Why splenomegaly in hemolytic anemia Intravascular hemolytic anemia
Intravascular hemolytic anemia Robert koch institute
Robert koch institute Evidence of hemolysis
Evidence of hemolysis Acquired hemolytic anemia
Acquired hemolytic anemia Extrinsic hemolytic anemia
Extrinsic hemolytic anemia Pathophysiology of anemia diagram
Pathophysiology of anemia diagram Megaloblastic anemia causes
Megaloblastic anemia causes Megaloblastic anemia vs pernicious anemia
Megaloblastic anemia vs pernicious anemia Causes of macrocytic anemia
Causes of macrocytic anemia Pediatrician
Pediatrician A pediatrician wishes to recruit 5 couples
A pediatrician wishes to recruit 5 couples Dr pushpa raj sharma
Dr pushpa raj sharma Advantages and disadvantages of being a pediatrician
Advantages and disadvantages of being a pediatrician Dr pushpa raj sharma
Dr pushpa raj sharma