pharyngitis Sayed Mostafa Hashemi MD 2 INTRODUCTION n




- Slides: 60

pharyngitis Sayed Mostafa Hashemi MD 2
INTRODUCTION n n n Pharyngitis is defined as inflammation of the pharynx. The anatomic region of the pharynx invariably affected in adults is the oropharynx. The predominant symptom is sore throat, which overall is the third most common chief complaint to physicians in an officebased practice. 3
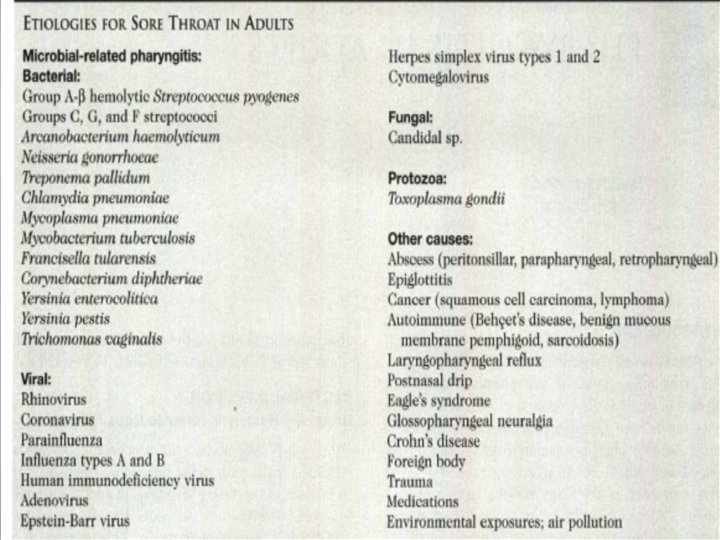
4
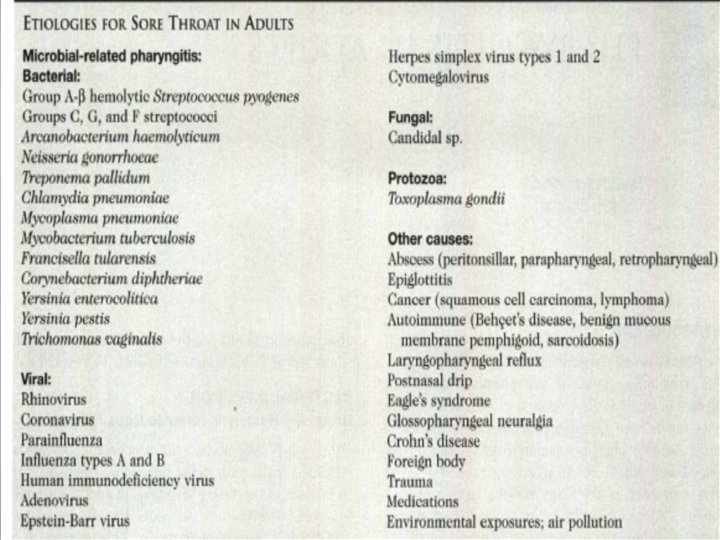
Pharyngitis n Pharyngeal mucosa exhibits an inflammatory response to many other agents n n n Opportunistic bacteria Fungi Environmental pollutants Neoplasm Granulomatous disease Chemical and physical irritants 5
Important disease mimic Pharyngitis n n Scc of the upper aerodigestive tract frequently presents with a history of chronic sore throat. Epiglottitis in adults commonly presents as a severe acute sore throat and odynophagia with a relatively normal oropharyngeal examination. postnasal drip and laryngopharyngeal reflux can cause an irritative pharyngitis. Occupational and environmental exposures can also be associated with an irritative pharyngitis and this has been demonstrated in many different populations, such as in the firefighters who have World Trade Center cough 6
Infectious causes of pharyngitis 7
Bacterial infection n Pharyngitis in adults is caused by a bacterial infection in approximately 5% to 10% of patients This is different than in children, where bacterial pharyngitis accounts for 30% to 40% of cases 8
Bacterial infection n Approximately 75% of adults presenting with a sore throat are prescribed antibiotics for a presumed bacterial pharyngitis even though this practice will only help a minority of the patients 9
n n n BASIC KWNOLAGE ABOUT GABHS is the pathogenic organism responsible for most cases of bacterial pharyngitis in adults. This organism is a gram positive cocci that grows in chains. Its natural reservoir is the skin and upper aerodigestive tract mucosa of the nasopharynx and oropharynx. The organism is a pathogen only in humans. Less than 5% of adults are asymptomatic carriers Spread occurs mostly through aerosolized microdroplets, less commonly by direct contact, and rarely through ingestion of contaminated nonpasteurized milk or food. Infections are more common in the autumn and winter 10
Symptoms & Signs n Symptoms are usually rapid in onset and include severe sore throat, odynophagia, cervical lymphadenopathy, fevers, chills, malaise, headache, mild neck stiffness, and anorexia. 11
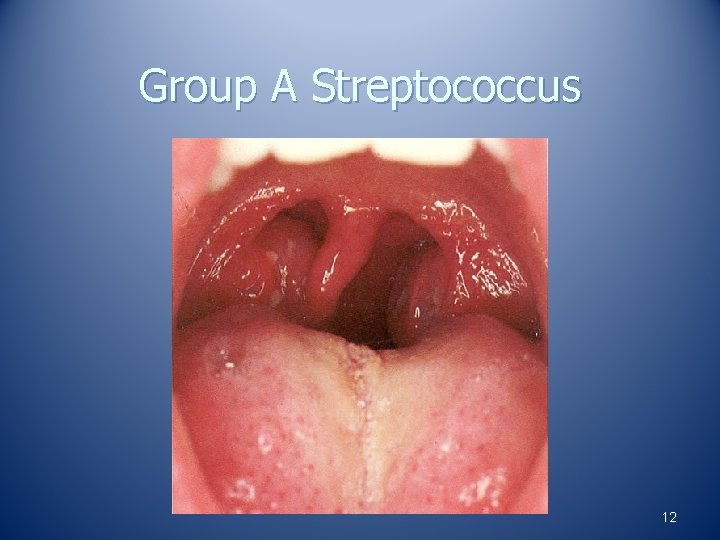
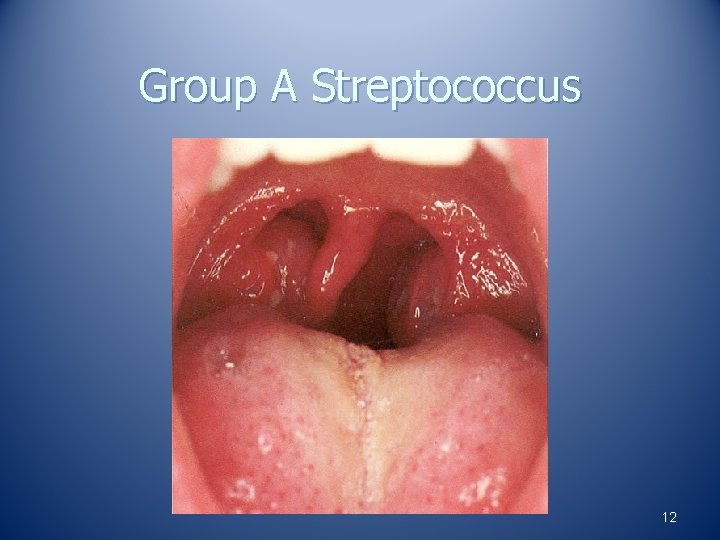
Group A Streptococcus 12

13
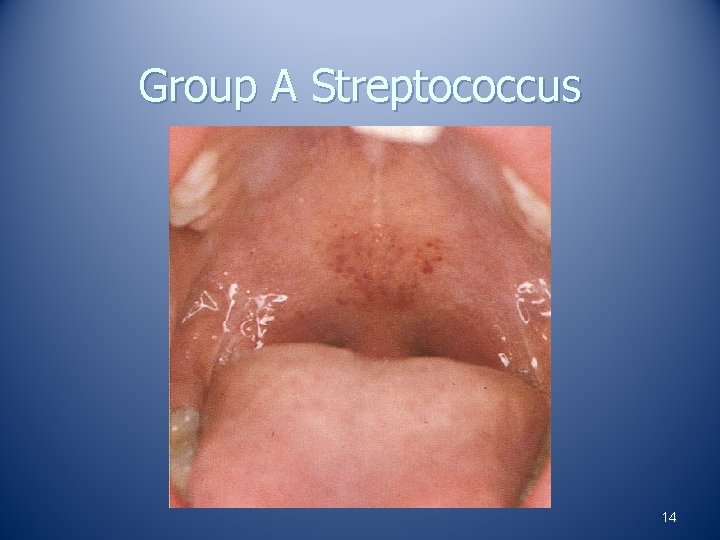
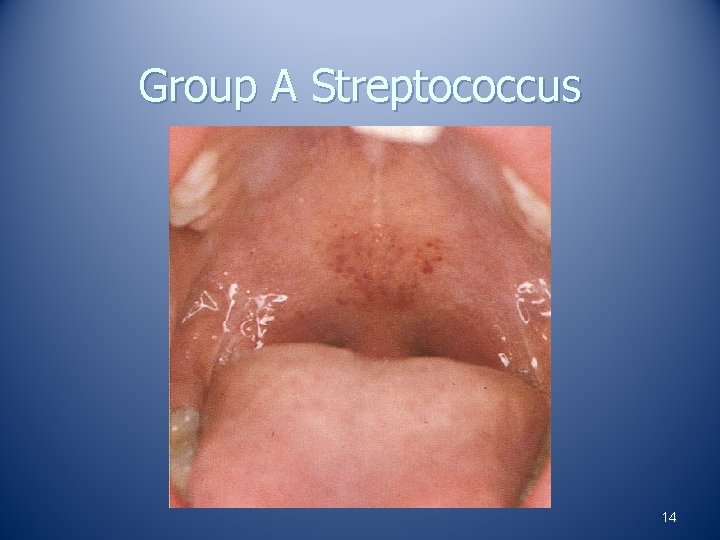
Group A Streptococcus 14
Clinical course n n Untreated; self-limited and consist of localized inflammation that resolves after 3 to 7 days. Patients are contagious during the acute illness and for approximately 1 week afterward. Prompt antibiotic treatment reduces the duration of symptoms (if treatment begins within 24 to 48 hours of symptom onset), reduces the period of contagiousness to 24 hours after beginning treatment, and likely decreases the incidence of suppurative complications. Prevention of rheumatic fever is possible if antibiotic therapy is started up to 10 days after the onset of symptoms. 15
Clinical diagnosis n n n high probability : empiric antibiotic therapy, intermediate probability: further testing ( rapid antigen test) or (throat culture) low probability: symptomatic therapy and appropriate follow-up 16
Diagnosis n n Scoring of clinical findings Rapid antigen detecting test Culture Aso 17
Scoring of clinical findings centor scoring n Exsudative tonsilltis n Absence of cough n Anterior cervical adenopathy n Fever(>38. 8) 18
Scoring of clinical findings centor scoring n n Present of 3 or 4 indicate positive value in 40 -60% Absence of 3 or 4 negative predictive value in 80% Antibiotics prescribed in 4 and 2 or 3 should be take rapid test Culture? 19
These scoring systems should not be used in n n patients who are immunocompromised, have complicated comorbidities, or have a history of rheumatic fever. during an epidemic of acute rheumatic fever, in parents with school-aged children, or for adults with occupations that bring them into frequent contact with children 20
Throat culture n n Strp carrier 18 -24 hour wast of time 21
Medical Management n n Acute tonsillitis usually subside in 6 day PCN is first line(no clinical isolate of GABHS has ever been documented to be resistat to penicillin) 22
treatment n n The oral course should be for 10 days. Benzathine penicillin can be alternatively used as a single intramuscular injection that provides bactericidal levels for 21 to 28 days. Erythromycin is an acceptable alternative for patients allergic to penicillin, but isolated reports of macrolide resistance (<5% of clinical isolates) have been reported in the United States. Clindamycin is an acceptable alternative for patients with both a penicillin allergy and a strain resistant to macrolides 23
Medical Management n Recurrent or unresponsive infections require treatment with beta-lactamase resistant antibiotics such as Clindamycin n Augmentin n Penicillin plus rifampin Adenotonsillar hyperplasia may respond to one month of therapy with beta-lactamase resistant antibiotics n 24
Medical Management n n n Whether treatment is prescribed in all cases or just in select cases has been debated. It has been suggested that clinicians should consider treating patients who do not respond to symptomatic therapy or patients who are at increased risk for sequelae. 23 Penicillin and clindamycin both provide effective treatment when necessary 25
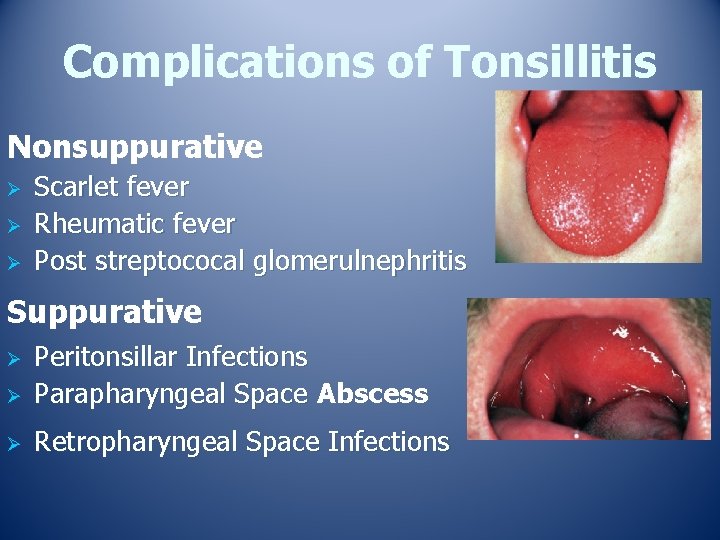
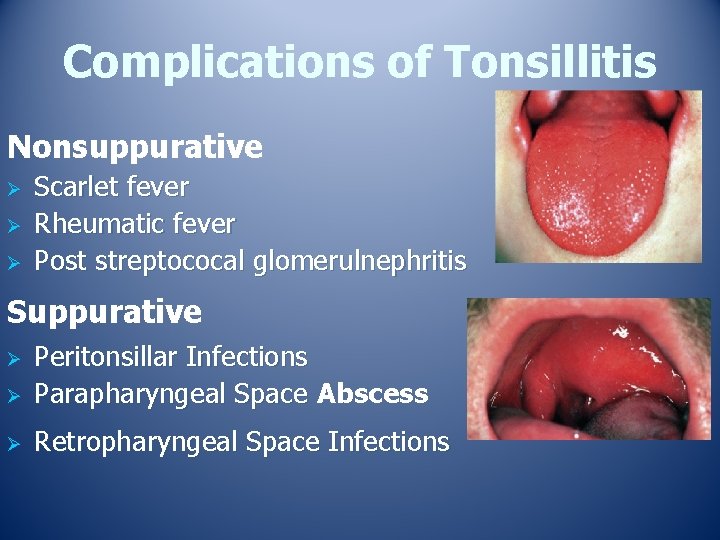
Complications of Tonsillitis Nonsuppurative Ø Ø Ø Scarlet fever Rheumatic fever Post streptococal glomerulnephritis Suppurative Ø Peritonsillar Infections Parapharyngeal Space Abscess Ø Retropharyngeal Space Infections Ø
Recurrent Acute Tonsillitis n n Same signs and symptoms as acute Occurring in 7 separate episodes per year 5 episodes per year for 2 years 3 episodes per year for 3 years M HASEMI MD 27
NON–GROUP A β-HEMOLYTIC STREPTOCOCCAL INFECTIONS n Pharyngeal infection with groups C and G streptococci can cause acute glomerulonephritis but has never been shown to cause acute rheumatic fever 28
Viruses n Major cause of acute respiratory disease Influenza virus n Parainfluenza viruses n Rhinovirus n Adenoviruses n Respiratory syncicial virus n Coronaviruses n 29
symptoms of the common cold The average adult gets 2 to 4 colds each year, Presenting symptoms of the common cold may overlap with those of GABHS pharyngitis, but the sore throat is usually not severe, and odynophagia is unusual. Patients usually complain of nasal symptoms (rhinorrhea, nasal stuffiness) that lead the throat symptoms. A nonproductive cough, hoarseness, and low-grade fever may also be present. The nasal mucosa is typically edematous, and the oropharynx has mild erythema. Specific virologic diagnosis is unnecessary for most patients, because it usually does not affect the management 30
EBV n EBV is the causative agent of infectious mononucleosis (IM). The initial route of infection occurs through the lymphoid tissues and pharyngeal epithelial cells. 31
CLINICAL COURSE n n n The initial incubation period is from 3 to 7 weeks. A prodrome of malaise, fever, and chills is followed 1 to 2 weeks later by sore throat, fever, anorexia, and lymphadenopathy (especially cervical). Sore throat is found in 82% of patients with IM and is the most common omplaint. Other symptoms may include abdominal discomfort, headache, stiff neck, and skin rash 32
EBV n Diagnosis By Clinical presentation n CBC with differential (atypical lymphocytes –T lymphocytes) n Detection of heterophil antibodies (Monospot test) n Ig. M titers n 33
Diagnosis n n n Infectious mononucleosis causes an absolute lymphocytosis with more than 10% atypical lymphocytes. Finding atypical lymphocytes on a peripheral blood smear may be consistent with a clinical impression of IM but is not specific for this illness. Toxoplasmosis, cytomegalovirus, acute HIVinfection, hepatitis A, tularemia, and rubella can also be associated with this finding 34
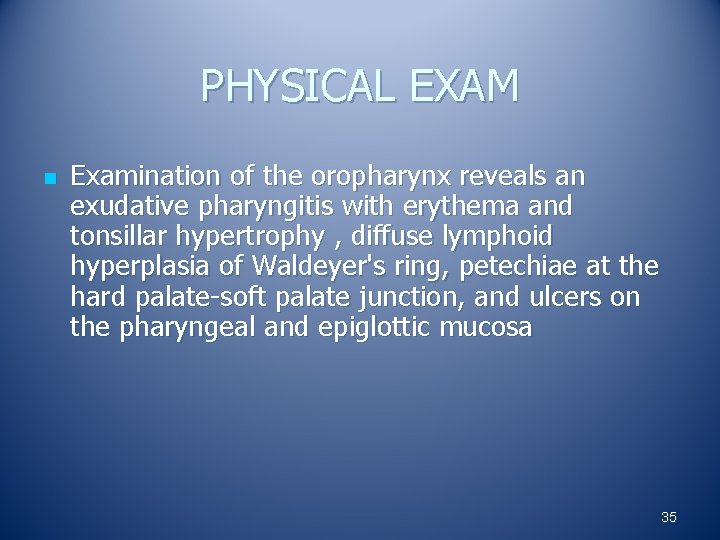
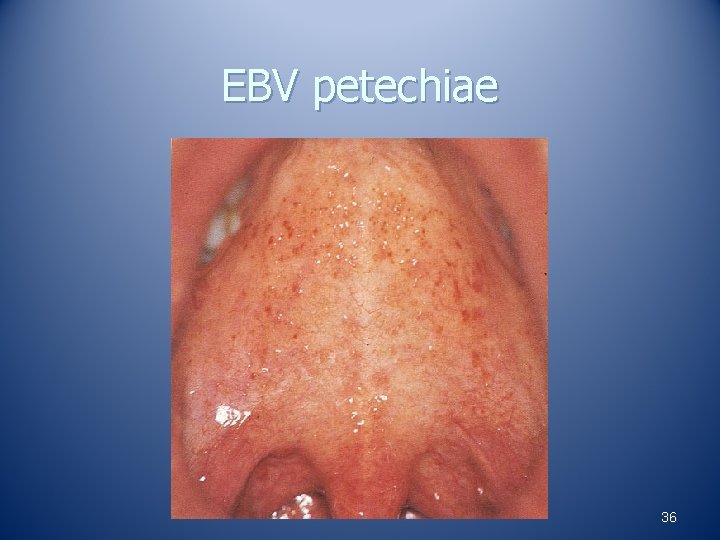
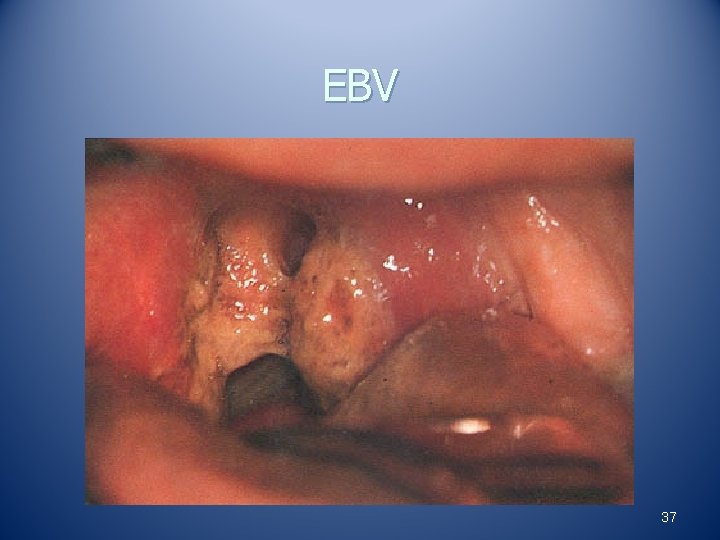
PHYSICAL EXAM n Examination of the oropharynx reveals an exudative pharyngitis with erythema and tonsillar hypertrophy , diffuse lymphoid hyperplasia of Waldeyer's ring, petechiae at the hard palate-soft palate junction, and ulcers on the pharyngeal and epiglottic mucosa 35
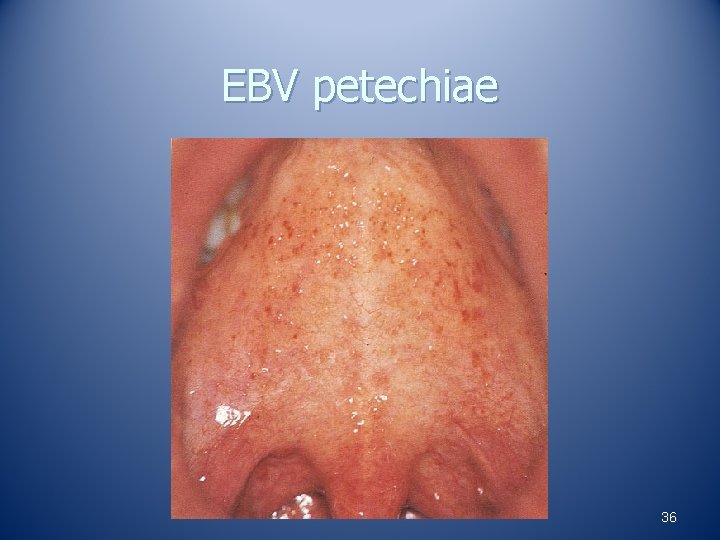
EBV petechiae 36
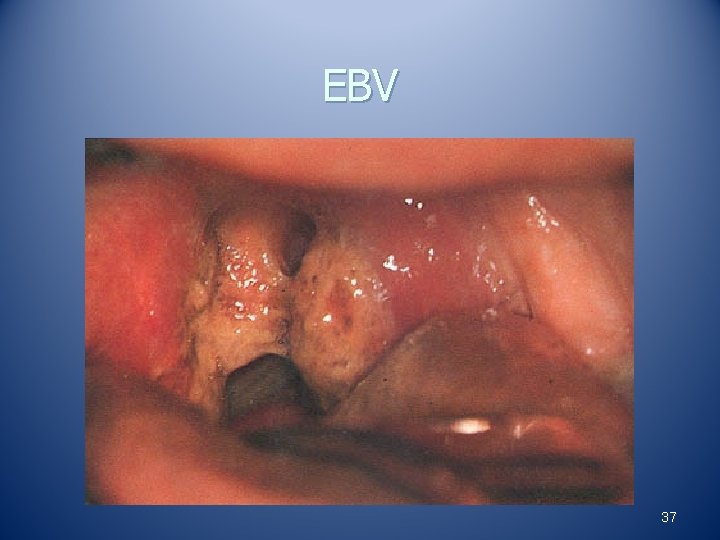
EBV 37
38
Treatment n n Supportive management Rest Avoidance of contact sports (? ->splenic rupture? ) Steroids are indicated for complications related to impending upper airway obstruction, severe hemolytic anemia, severe thrombocytopenia, or persistent severe disease 39
Human Immunodeficiency Virus n n n Acute human immunodeficiency virus (HIV) type 1 infection causes a mononucleosis-like syndrome in 40% to 90% of patients, which starts days to weeks after exposure. This febrile illness is called acute retroviral syndrome (ARS). Due to the nonspecific signs and symptoms, even patients at risk for HIV are frequently not promptly diagnosed. Thus ARS should be included in the differential diagnosis in any patient with a fever of unknown origin and risk factors for HIV exposure.
symptoms and signs n n n The most common symptoms and signs include fever (median maximum temperature 38. 9°C), lethargy, skin rash, myalgia, headache, pharyngitis, cervical adenopathy, and arthralgia. Pharyngitis occurs in 50% to 70% of patients and usually appears as hypertrophy of the tissues of Waldeyer's ring without exudates. Other oral manifestations that are less commonly observed include ulcers (29%) and candidiasis (17%). [88] 41
Diagnosis n n n Diagnosis is dependent upon laboratory tests. Complete blood count (CBC) may reveal lymphopenia or trhrombocytopenia. 6’ Atypical lymphocytes and a decreased CD 4 cell count are usually not observed at this time. Because antibodies to HIV appear approximately 4 weeks later. A quantitative plasma HIV-1 RNA level, tested by PCR, is necessary to make a timely diagnosis
Arcanobacterium haemolyticum n n Arcanobacterium haemolyticum is a nonmotile, β-hemolytic, gram positive bacillus that causes 0. 5% to 2. 5% of bacterial pharyngitis cases. 24 This organism also causes deep-seated infections such as pneumonia, meningitis, osteomyelitis, brain abscess, and peritonsillar abscess 43
A. haemolyticum n Pharyngitis caused by A. haemolyticum is easily mistaken for GABHS or viral pharyngitis with an exanthem because of the overlap in symptoms. When suspected, throat culture needs to be performed using 5% human blood agar. 26 Using this culture media, prominent hemolytic zones are formed within 24 hours by A. haemolyticum.
n n Oral penicillin was recommended for treatment in the past, but bactericidal tests demonstrated increasing tolerance of this organism; thus first-line antibiotic therapy for A. haemolyticumpharyngitis is erythromycin.
Neisseria gonorrhoeae is a sexually transmitted organism that affects the anogenital region but can also cause gingivitis, stomatitis, glossitis, and pharyngitis. 28. Fellatio is the high risk behavior, and thus the incidence of disease is highest in homosexual males and females 46
signs Symptomatic patients usually come to medical attention with findings suggestive of tonsillitis. The tonsils are enlarged, and a white-yellow exudate arises from the crypts. 2 8 Oropharyngeal trauma may be evident, particularly on the soft palate or uvula. Fever (8%) and lymphadenopathy (9%) are uncommon findings 47
Treatment n n Recommended treatment is with a single dose of intramuscular ceftriaxone. The higher dose of a 250 -mg single injection of ceftriaxone has improved efficacy for pharyngeal infection.
Corynebacterium diphtheriae n n Diphtheria is an example of an infectious disease that has almost been eradicated by the application of microbiologic and public health principles and simultaneous administration of diphtheria toxoid shortly after World War II
diphtheria n n Toxigenic strains are pathogenic, Toxin production is mediated by a bacteriophage. The diphtheria exotoxin inhibits protein synthesis in mammalian cells. Antitoxin neutralizes circulating toxin but is ineffective once cell penetration has occurred.
diphtheria n n n Transmission occurs through infected secretions from the nose, throat, eyes, or skin lesions. Entry occurs through the mouth or nose, and the organism initially remains localized to the mucosal surfaces of the upper respiratory tract. Local inflammation and toxin-mediated tissue necrosis causes formation of a fibrinous, patchy, adherent, gray-black pseudomembrane. The location of pseudomembranes can be nasal, tonsillar, pharyngeal, laryngotracheal, conjunctival, genital, or cutaneous. More than one area can be affected, but the oropharynx is the most commonly involved site
diphtheria n n Toxin effects at distant sites cause myocarditis, neuritis, and acute tubular necrosis. Myocarditis is associated with delayed administration of antitoxin and typically occurs just as the local disease is improving at 2 weeks after onset. Peripheral neuritis occurs 3 to 7 weeks later, usually affects motor rather than sensory nerves, and commonly affects the soft palate and pharyngeal muscles.
n n Definitive diagnosis is based on isolation of the organism. The pseudomembrane should be cultured,
Treatment n n Treatment consists of both the antitoxin and antibiotics. Outcome depends on the location and extent of the pseudomembrane, the patient’s immunization status, and how quickly the antitoxin is administered. The antitoxin should be given as soon as possible, because it can only inactivate toxin that has not already entered the cells.
booster injection n n . Diphtheria toxoid booster injection is recommended every 10 years in adults. This is especially important for people who travel to epidemic or endemic areas. Immunized patients can still be carriers for the organism, because the vaccination is directed solely against the toxin. When carriers are detected, treatment should consist of a course of antibiotics and a toxoid booster injection, if none was administered during the previous year.

56
oropharyngeal candidiasis (OPC) is considered an opportunistic infection and is now the most frequent opportunistic infection found in symptomatic HIV-positive patients. 93 In those who receive radiation for head and neck cancer, Candida can be isolated in 73% of patients and can cause infection in 27%. 94 Other populations at risk for disease include those with xerostomia, either because of prior radiation to the head and neck, from Sjögren syndrome, or as a side effect from medications; people who use steroid inhalers or broad-spectrum antibiotics; immunosuppressed individuals; people with diabetes mellitus, Cushing syndrome, and terminally ill conditions; and those on a high-carbohydrate diet. 91 57
Initial therapy for uncomplicated OPC includes improving oral hygiene and use of topical antifungals. 91 Patients with a refractory or recurrent infection and those at high risk for systemic disease should be treated with systemic antifungals. Fluconazole is the predominant medication used to treat OPC, because the predominant organism, C. albicans, has consistently shown sensitivity to the drug, 58
Prophylaxis for patients at high risk for relapse of OPC has been considered. Such populations include HIV-infected patients, bone marrow transplant patients, patients with chemotherapy-induced neutropenia, and those receiving radiation for head and neck cancer. Fluconazole appears to be better than nystatin in this regard. 91 OPC that responded to a 7 -day course of fluconazole (200 mg/day). 9 59

Thanks for your attention!