Hypersensitivity Pneumonitis DR S H HASHEMI 1 INTRODUCTION






- Slides: 37
Hypersensitivity Pneumonitis DR. S. H. HASHEMI 1
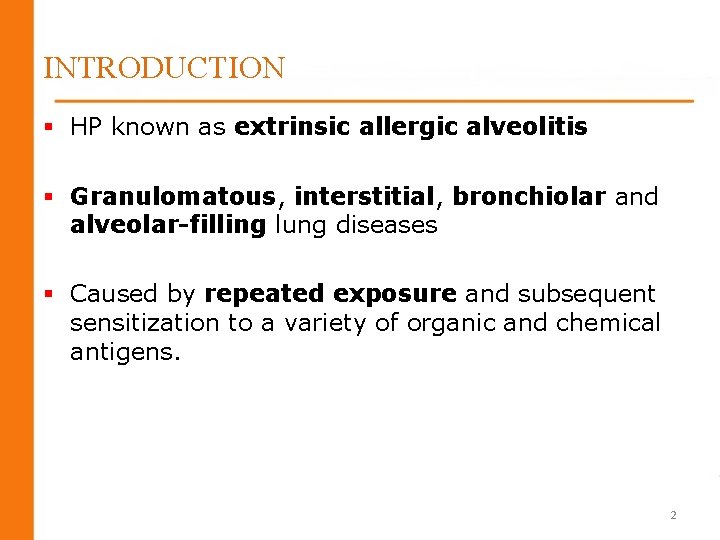
INTRODUCTION § HP known as extrinsic allergic alveolitis § Granulomatous, interstitial, bronchiolar and alveolar-filling lung diseases § Caused by repeated exposure and subsequent sensitization to a variety of organic and chemical antigens. 2
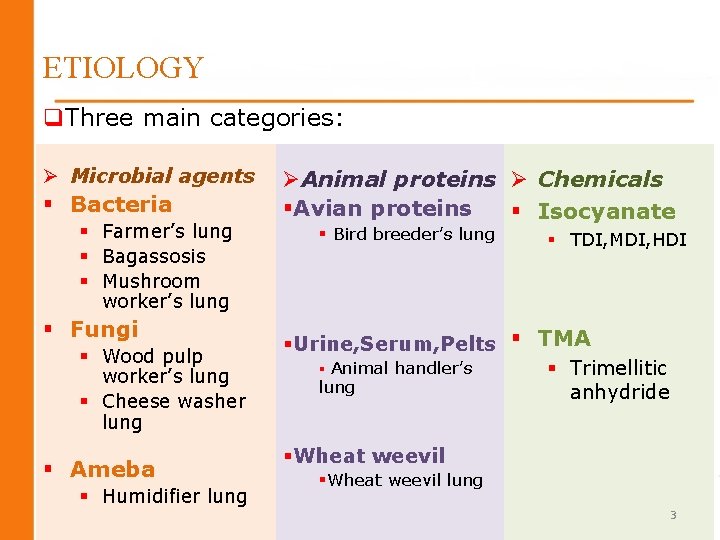
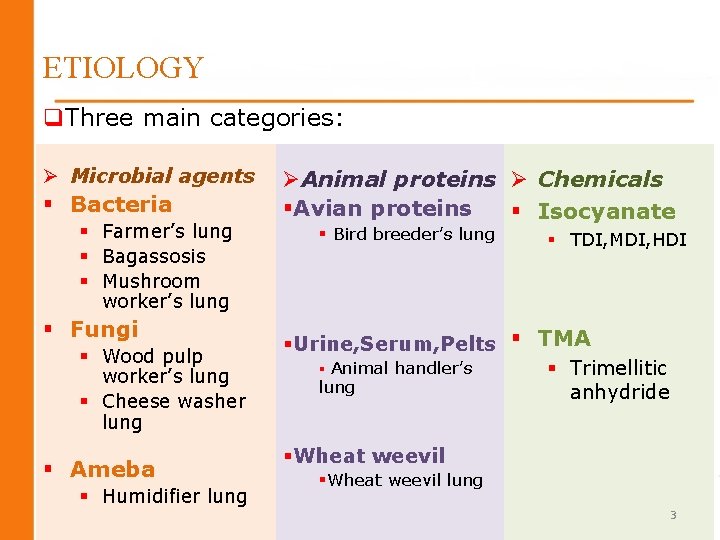
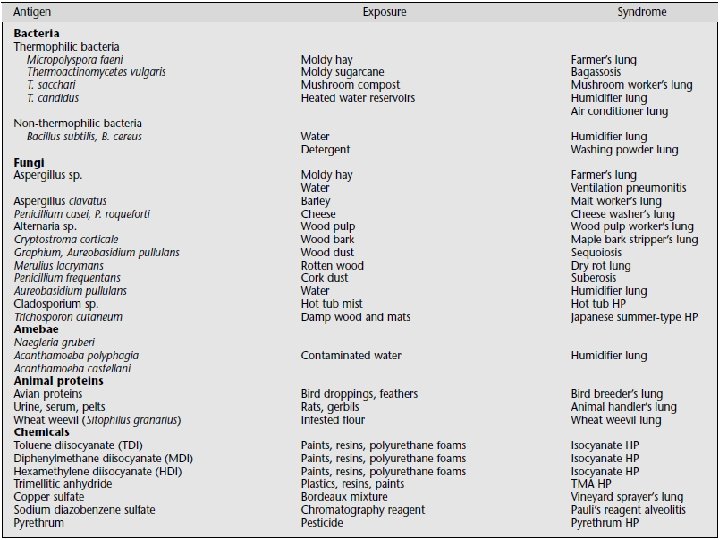
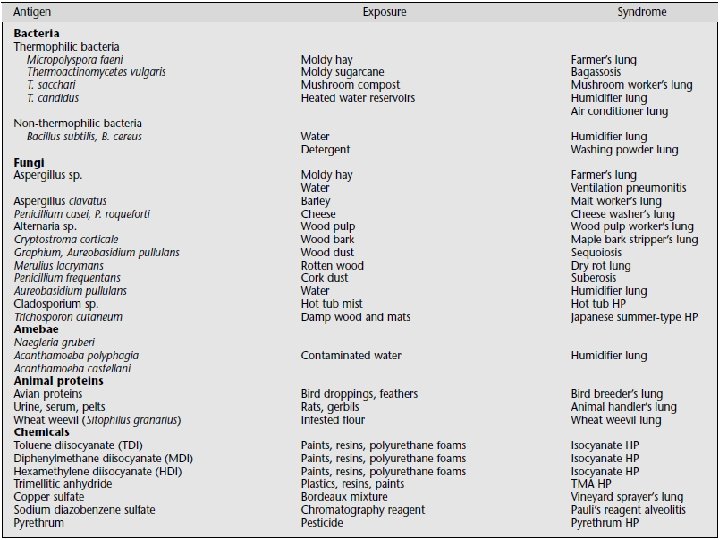
ETIOLOGY q. Three main categories: Ø Microbial agents § Bacteria § Farmer’s lung § Bagassosis § Mushroom worker’s lung § Fungi § Wood pulp worker’s lung § Cheese washer lung § Ameba § Humidifier lung ØAnimal proteins Ø Chemicals §Avian proteins § Isocyanate § Bird breeder’s lung § TDI, MDI, HDI §Urine, Serum, Pelts § TMA § Animal handler’s § Trimellitic lung anhydride §Wheat weevil lung 3
4
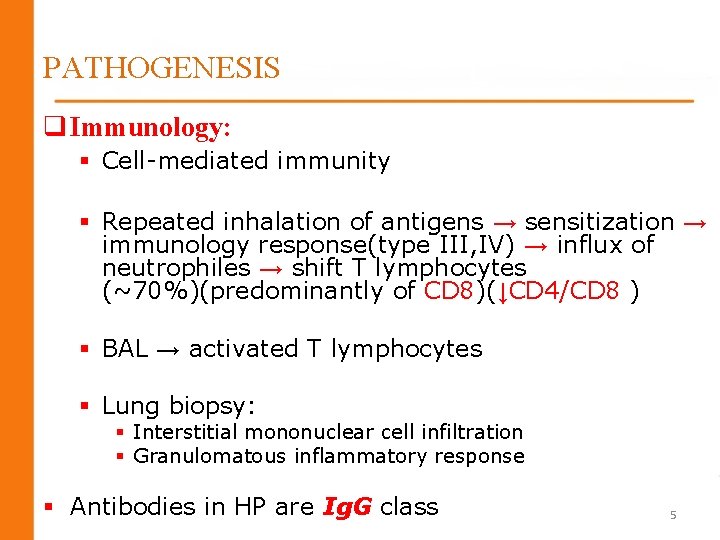
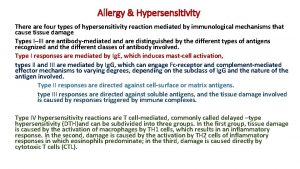
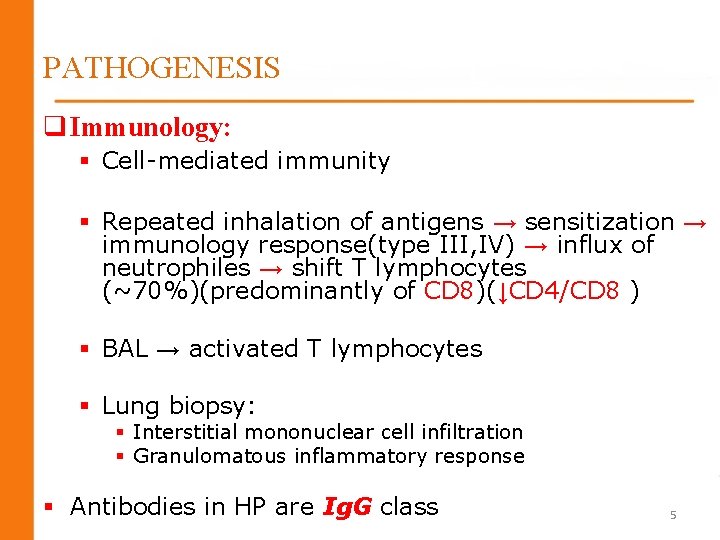
PATHOGENESIS q Immunology: § Cell-mediated immunity § Repeated inhalation of antigens → sensitization → immunology response(type III, IV) → influx of neutrophiles → shift T lymphocytes (~70%)(predominantly of CD 8)(↓CD 4/CD 8 ) § BAL → activated T lymphocytes § Lung biopsy: § Interstitial mononuclear cell infiltration § Granulomatous inflammatory response § Antibodies in HP are Ig. G class 5
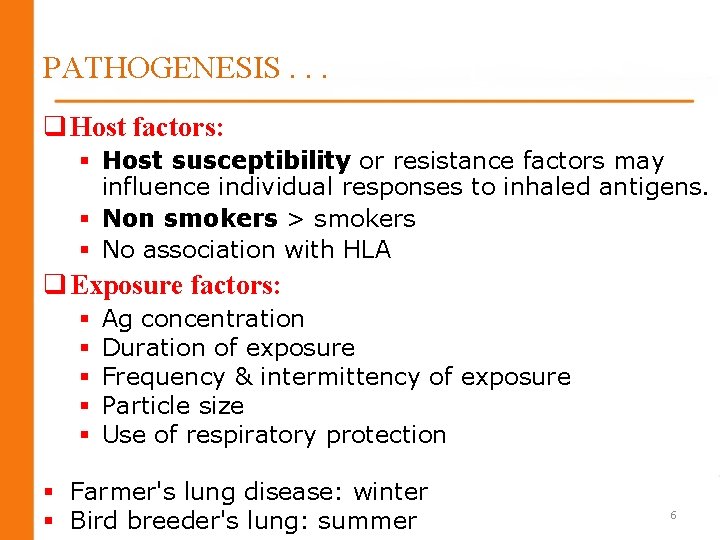
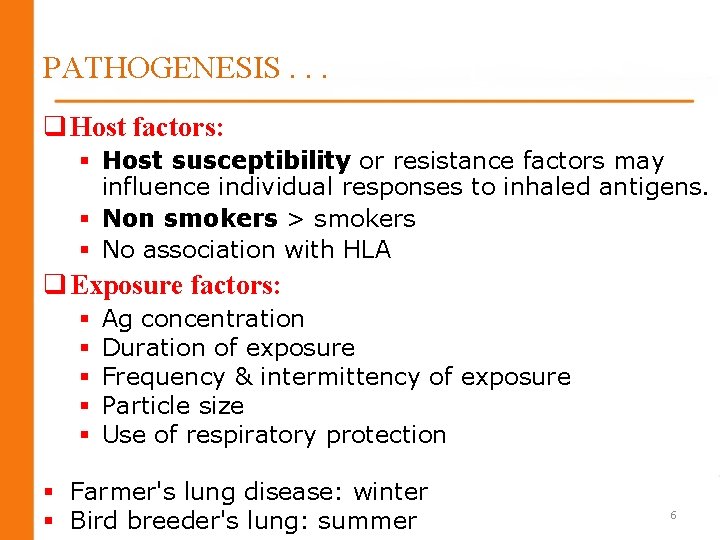
PATHOGENESIS. . . q Host factors: § Host susceptibility or resistance factors may influence individual responses to inhaled antigens. § Non smokers > smokers § No association with HLA q Exposure factors: § § § Ag concentration Duration of exposure Frequency & intermittency of exposure Particle size Use of respiratory protection § Farmer's lung disease: winter § Bird breeder's lung: summer 6

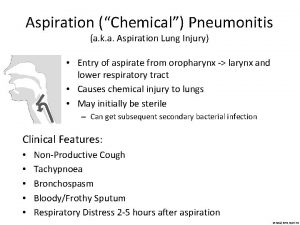
CLINICAL FEATURES q. Acute HP: § Fever , chills , myalgia , cough , dyspnea (4 -12 h after heavy exp. ) § Ph/E : basilar rales , peripheral leukocytosis § Recurrent febrile episodes (most frequent presentation) 7
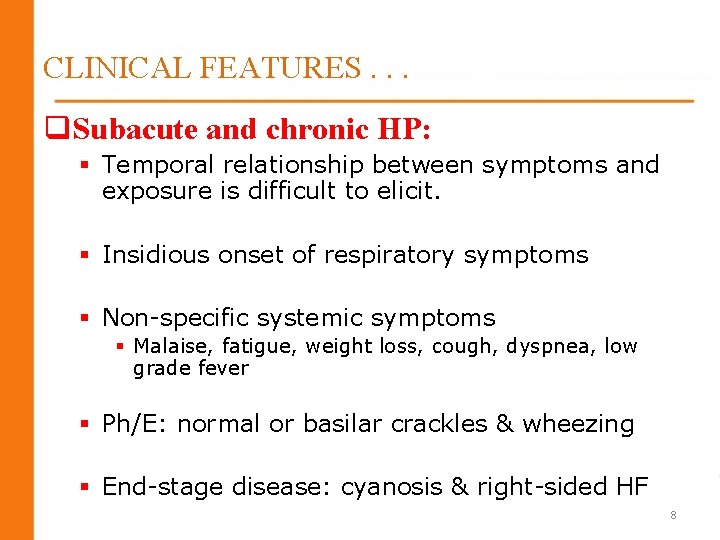
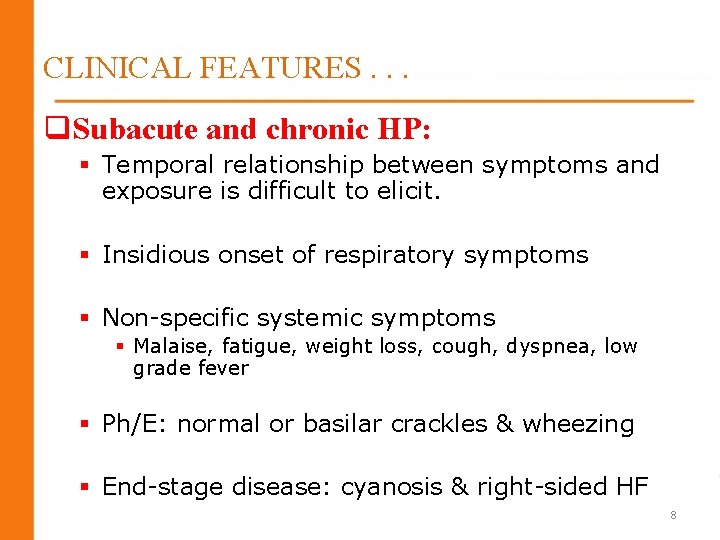
CLINICAL FEATURES. . . q. Subacute and chronic HP: § Temporal relationship between symptoms and exposure is difficult to elicit. § Insidious onset of respiratory symptoms § Non-specific systemic symptoms § Malaise, fatigue, weight loss, cough, dyspnea, low grade fever § Ph/E: normal or basilar crackles & wheezing § End-stage disease: cyanosis & right-sided HF 8
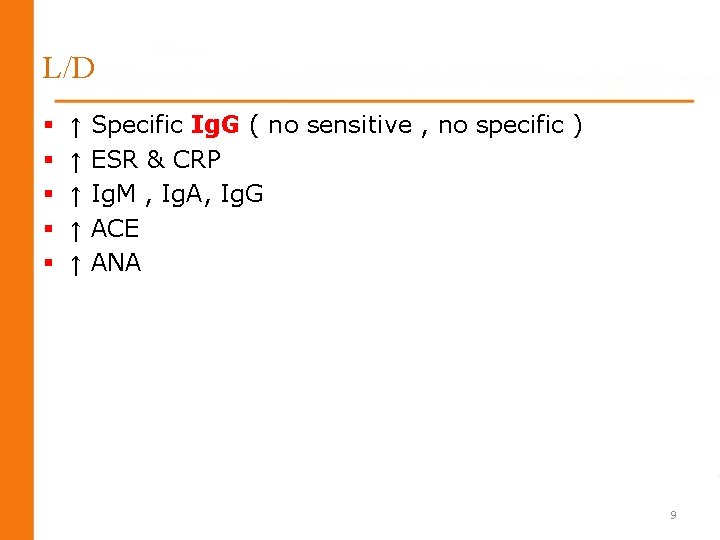
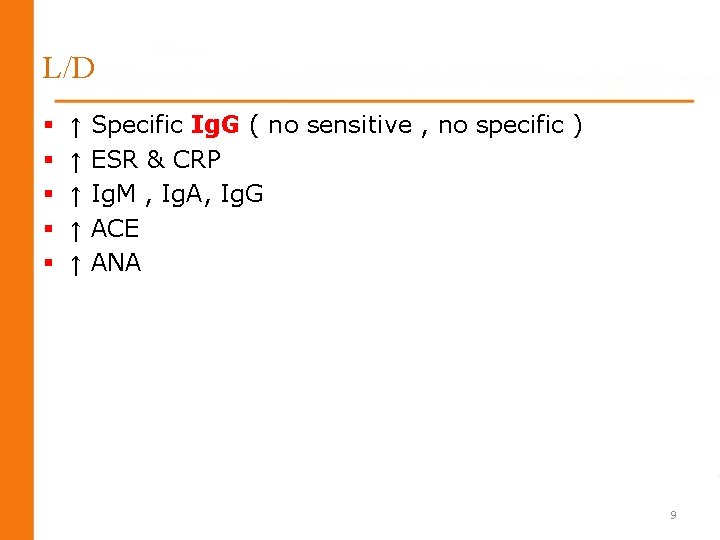
L/D § § § ↑ ↑ ↑ Specific Ig. G ( no sensitive , no specific ) ESR & CRP Ig. M , Ig. A, Ig. G ACE ANA 9
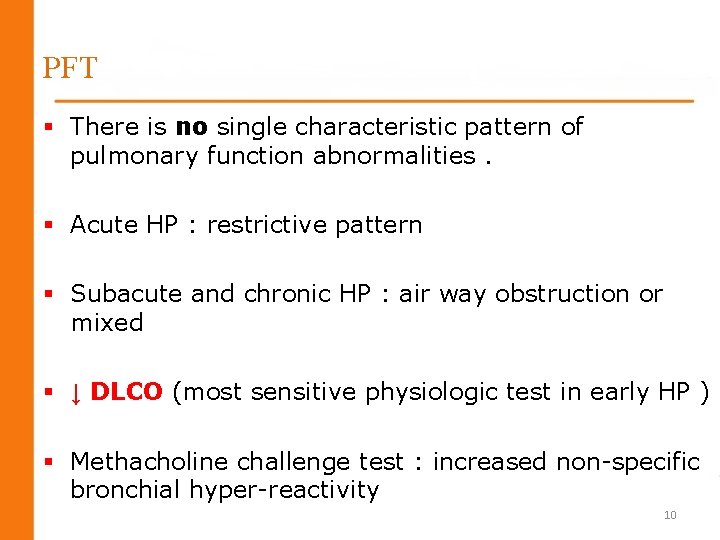
PFT § There is no single characteristic pattern of pulmonary function abnormalities. § Acute HP : restrictive pattern § Subacute and chronic HP : air way obstruction or mixed § ↓ DLCO (most sensitive physiologic test in early HP ) § Methacholine challenge test : increased non-specific bronchial hyper-reactivity 10
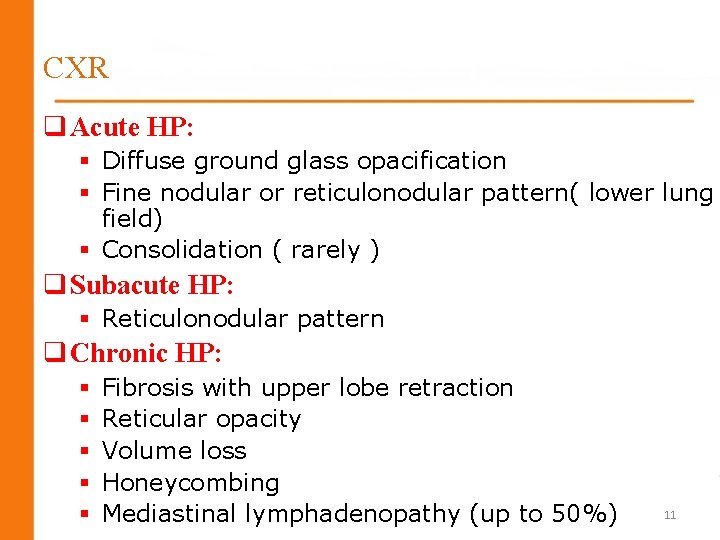
CXR q Acute HP: § Diffuse ground glass opacification § Fine nodular or reticulonodular pattern( lower lung field) § Consolidation ( rarely ) q Subacute HP: § Reticulonodular pattern q Chronic HP: § § § Fibrosis with upper lobe retraction Reticular opacity Volume loss Honeycombing Mediastinal lymphadenopathy (up to 50%) 11
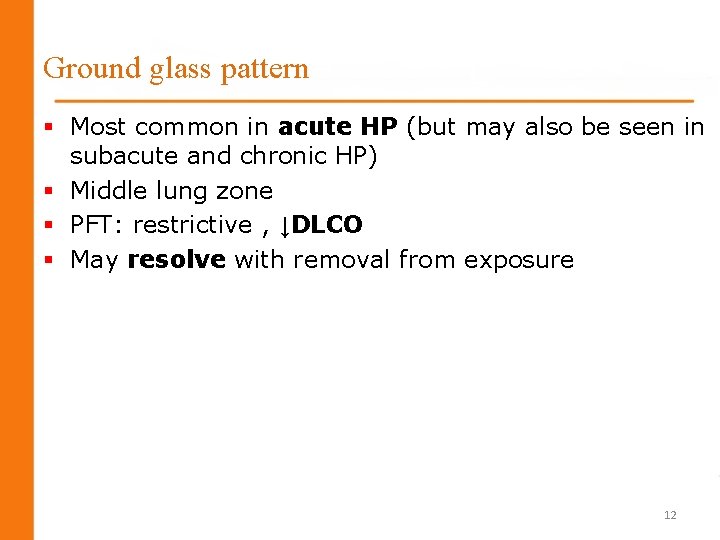
Ground glass pattern § Most common in acute HP (but may also be seen in subacute and chronic HP) § Middle lung zone § PFT: restrictive , ↓DLCO § May resolve with removal from exposure 12
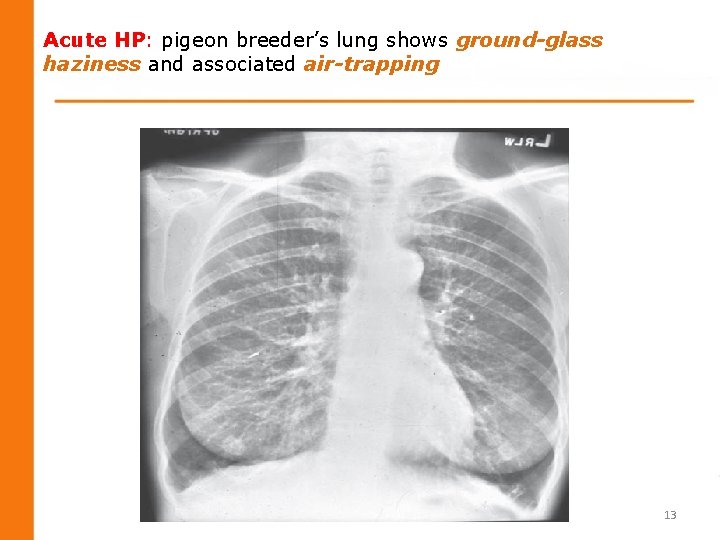
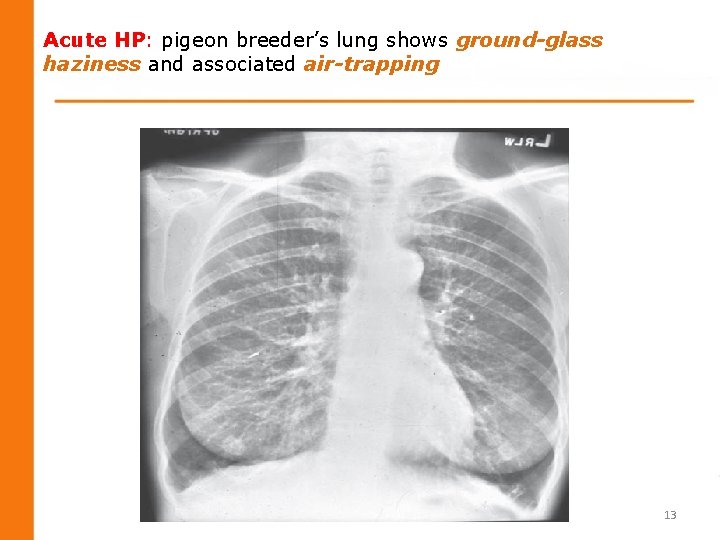
Acute HP: pigeon breeder’s lung shows ground-glass haziness and associated air-trapping 13
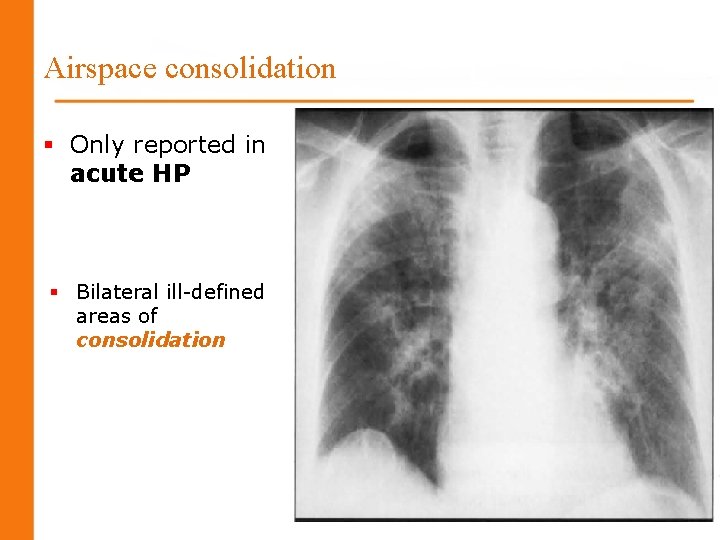
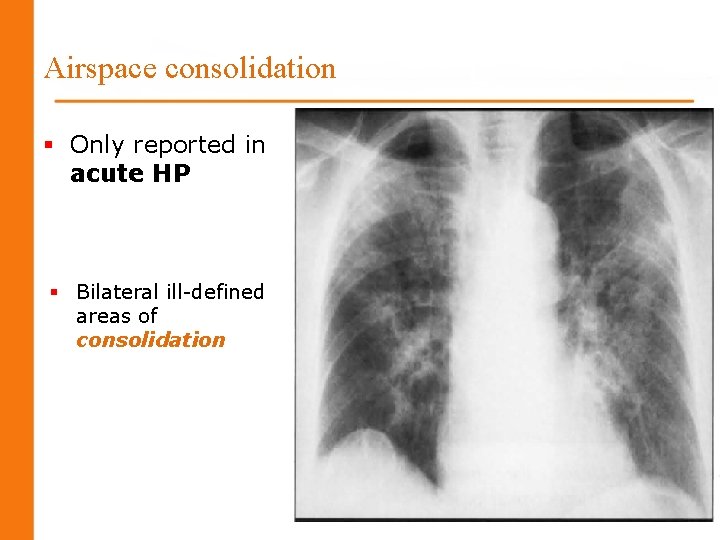
Airspace consolidation § Only reported in acute HP § Bilateral ill-defined areas of consolidation 14
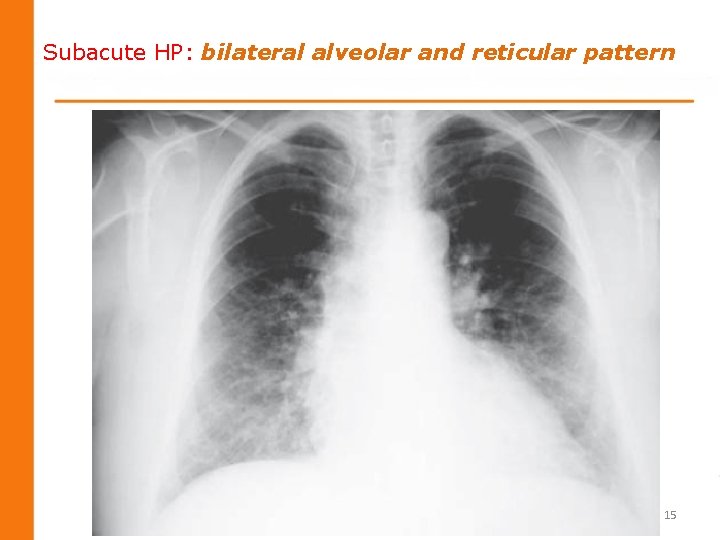
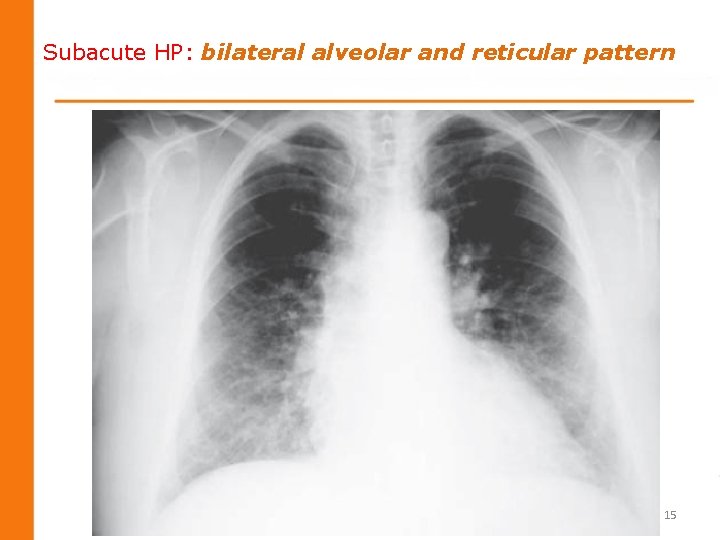
Subacute HP: bilateral alveolar and reticular pattern 15

Centrilobular nodules § Round, poorly defined, less than 5 mm in diameter § Typically centrilobular § Profuse throughout the lung, but a middle to lower lung zone predominance. § Most frequent HRCT finding in HP § Centrilobular nodules + ground glass opacification are highly suggestive for HP. § PFT : normal 16

Fibrosis § § Chronic HP (subacute HP) Irregular linear opacities Traction bronchiectasis Honeycombing 17
Emphysema § Chronic HP § Emphysema occurred more commonly than fibrosis in chronic farmer’s lung. 18
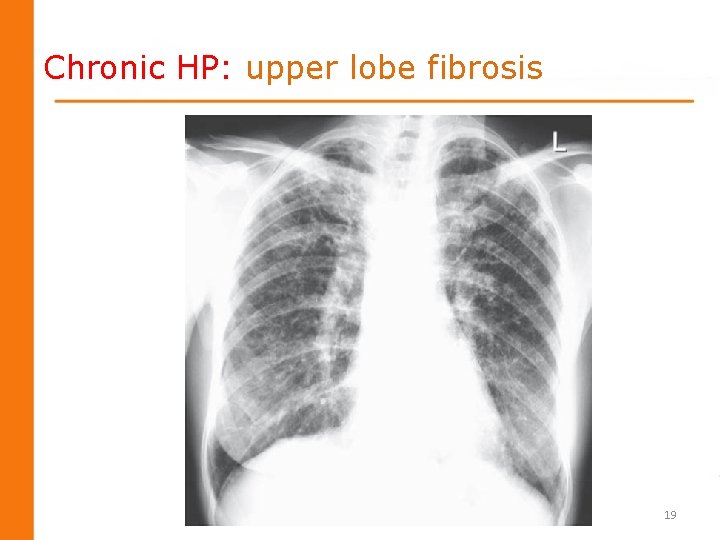
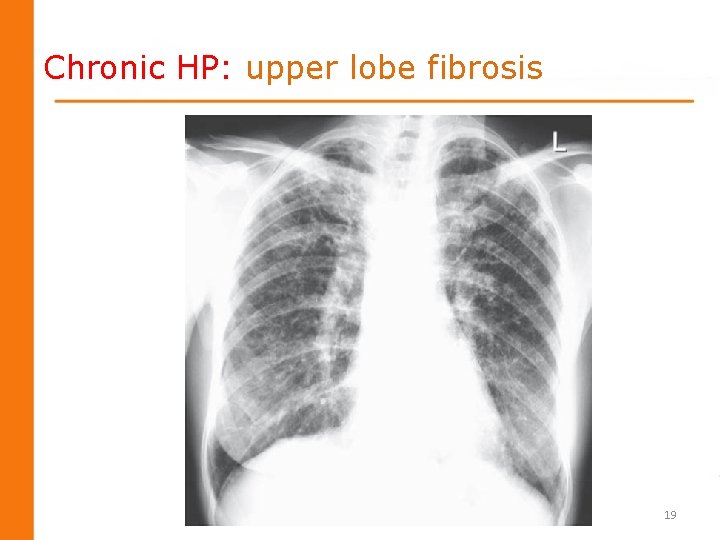
Chronic HP: upper lobe fibrosis 19
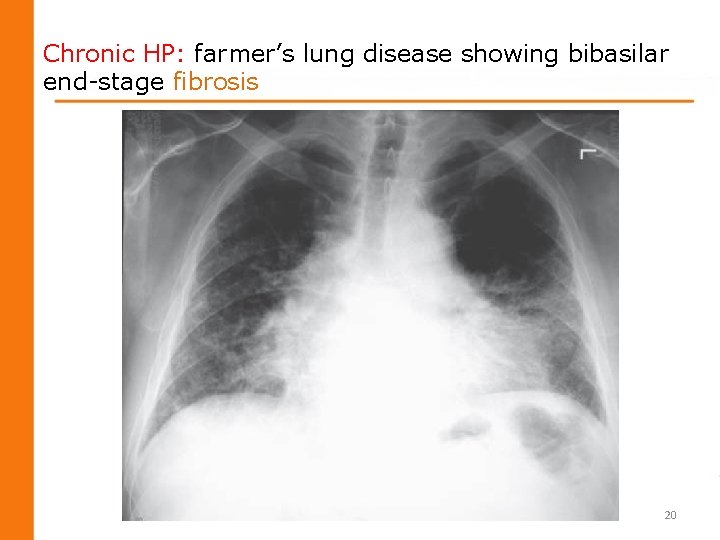
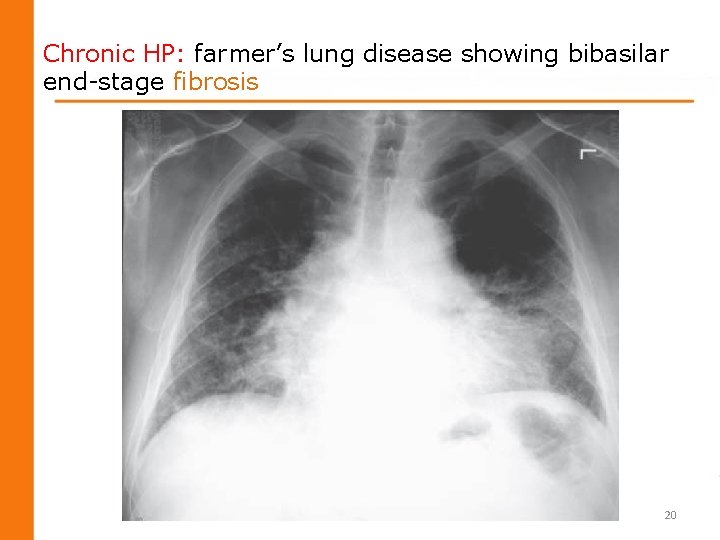
Chronic HP: farmer’s lung disease showing bibasilar end-stage fibrosis 20
HRCT § § § Sensitivity of HRCT is significantly better than CXR Ground glass Centrilobular nodules Fibrosis Emphysema Mediastinal lymphadenopathy (> 20 mm ) 21
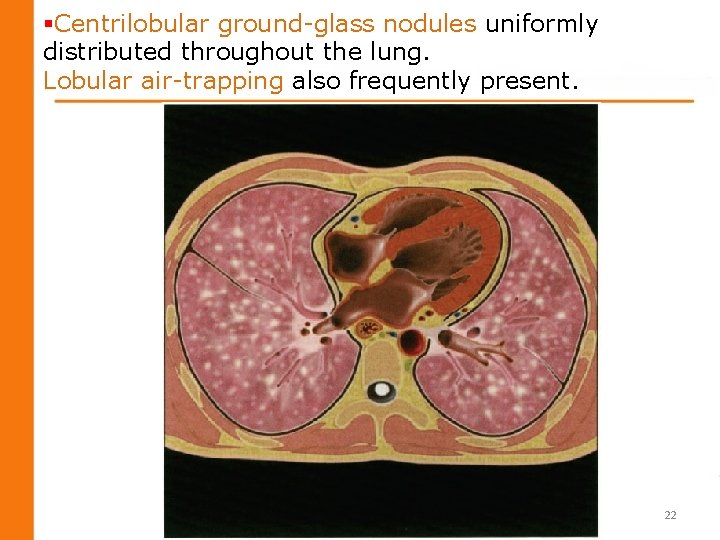
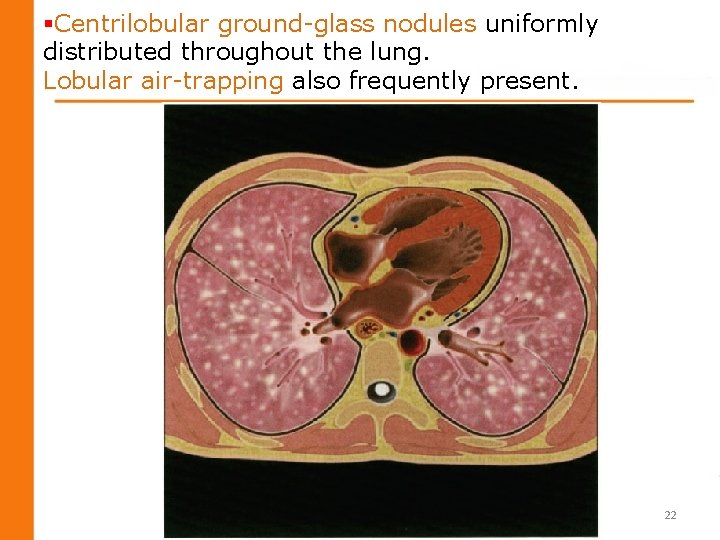
§Centrilobular ground-glass nodules uniformly distributed throughout the lung. Lobular air-trapping also frequently present. 22

Multiple low density ill-defined centrilobularnodules 23
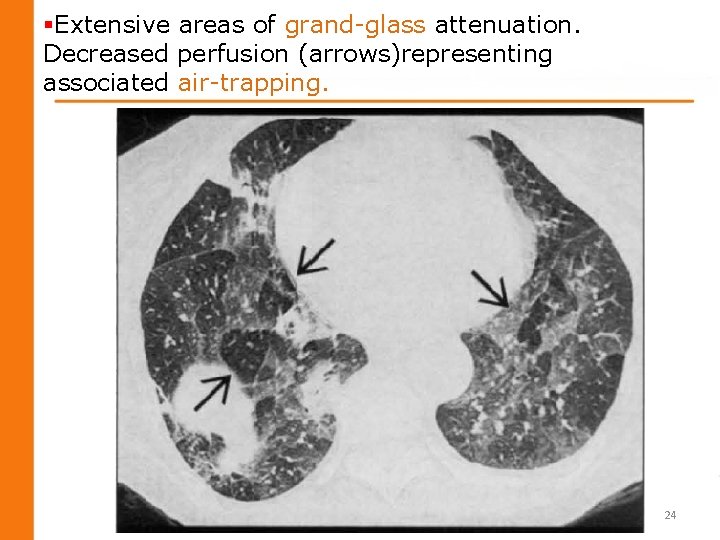
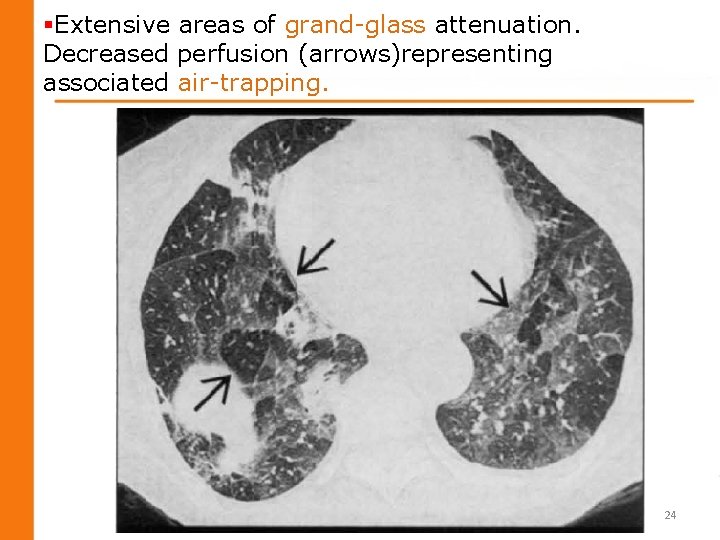
§Extensive areas of grand-glass attenuation. Decreased perfusion (arrows)representing associated air-trapping. 24
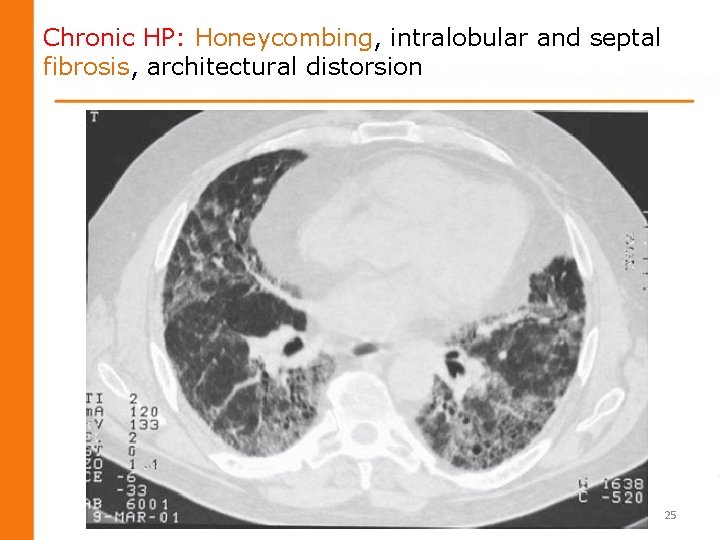
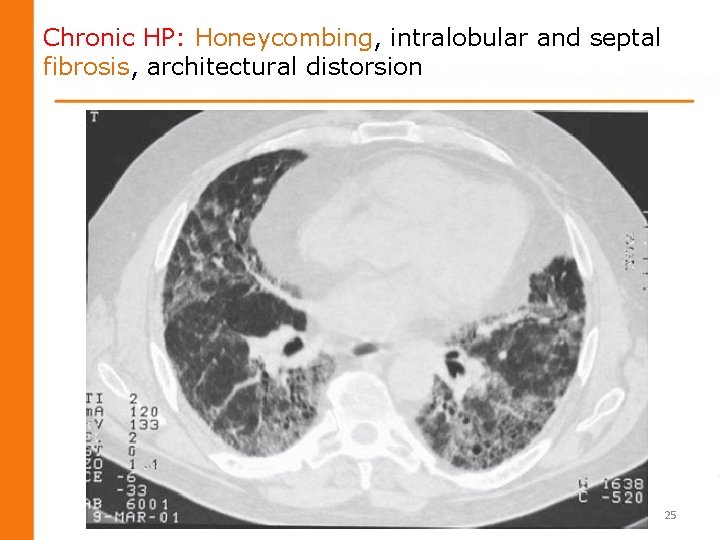
Chronic HP: Honeycombing, intralobular and septal fibrosis, architectural distorsion 25
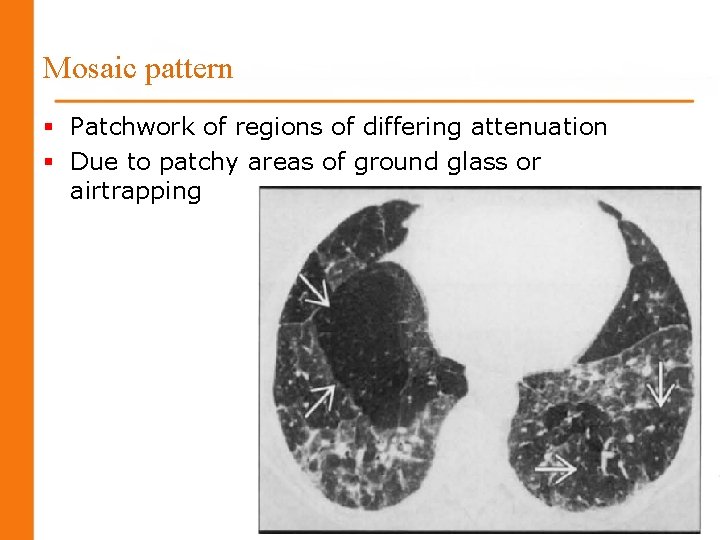
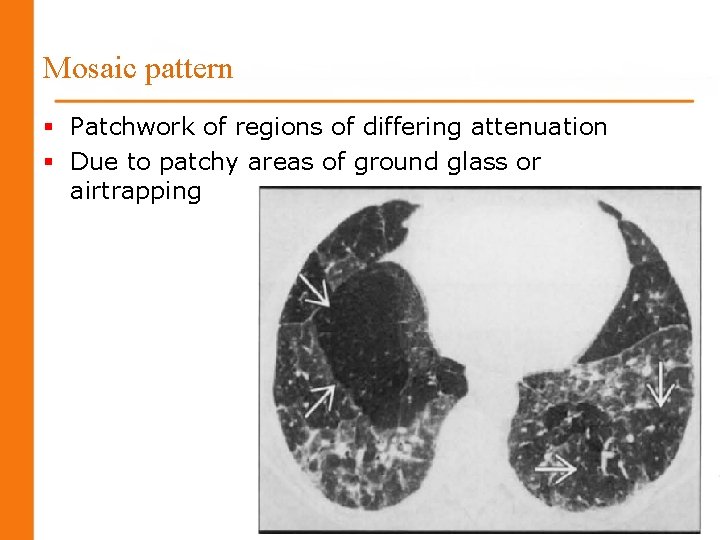
Mosaic pattern § Patchwork of regions of differing attenuation § Due to patchy areas of ground glass or airtrapping 26
Histopathology § Classic triad: § Cellular bronchiolitis § Lympho-plasmocytic interstitial infiltration § Non-necrotizing granulomas 27

Diagnosis Ø Temporal relationship between symptoms and certain activities is often the first clue to the diagnosis of HP 28
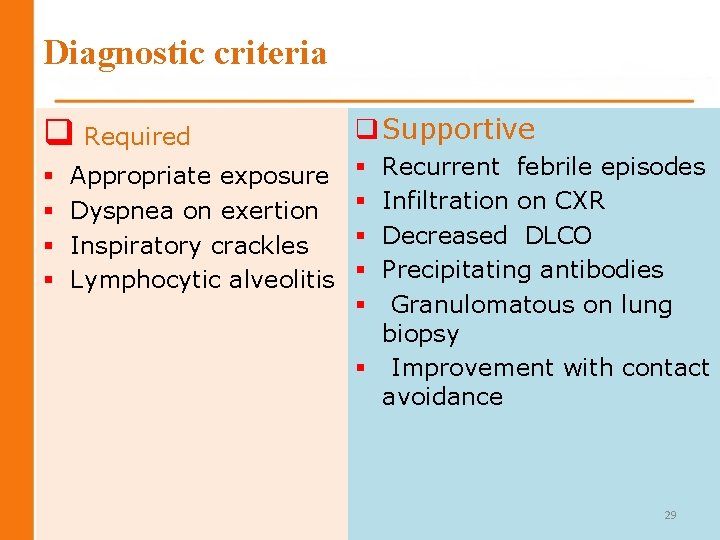
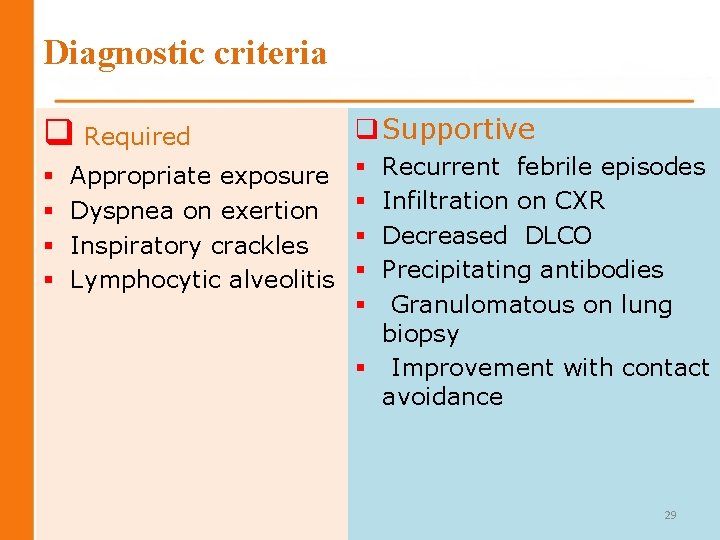
Diagnostic criteria q Required § § Appropriate exposure Dyspnea on exertion Inspiratory crackles Lymphocytic alveolitis q Supportive Recurrent febrile episodes Infiltration on CXR Decreased DLCO Precipitating antibodies Granulomatous on lung biopsy § Improvement with contact avoidance § § § 29
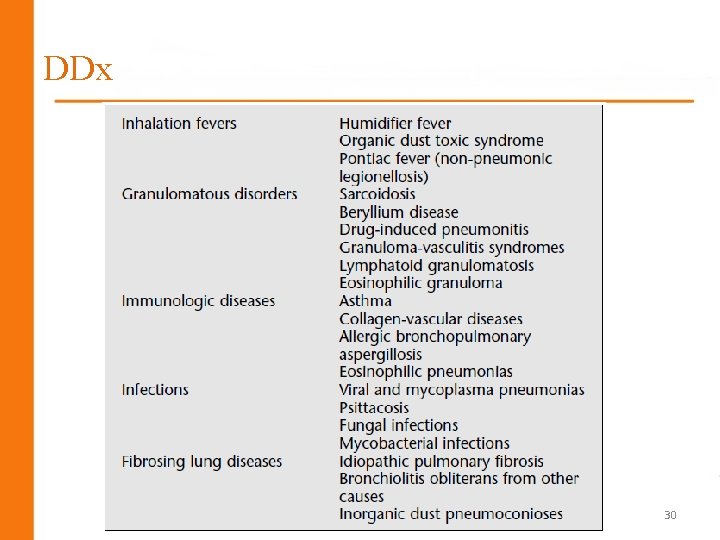
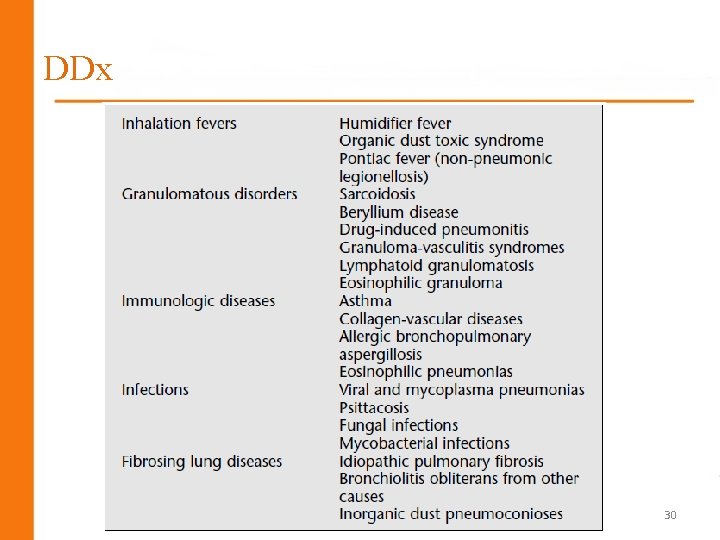
DDx 30
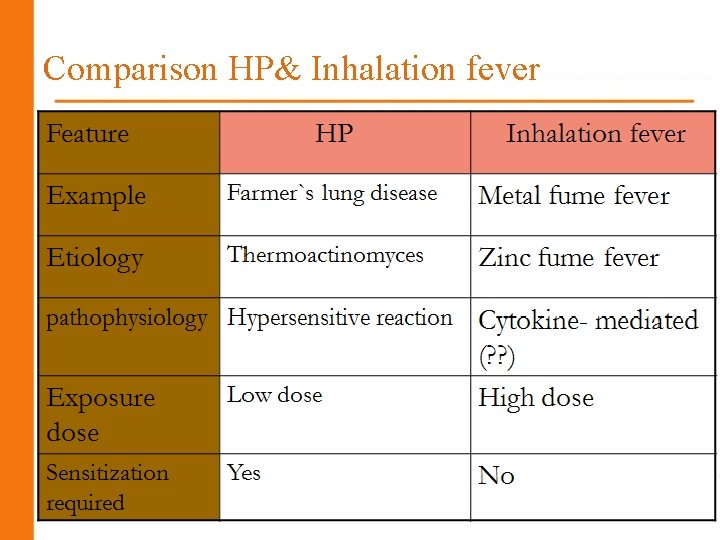
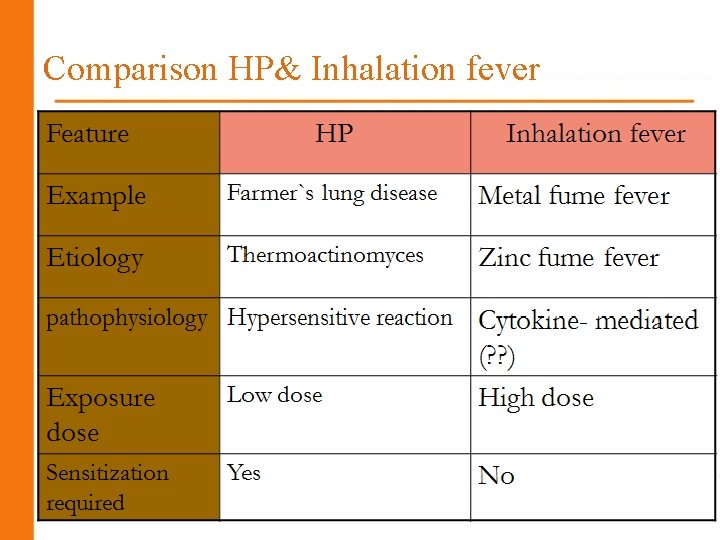
Comparison HP& Inhalation fever 31
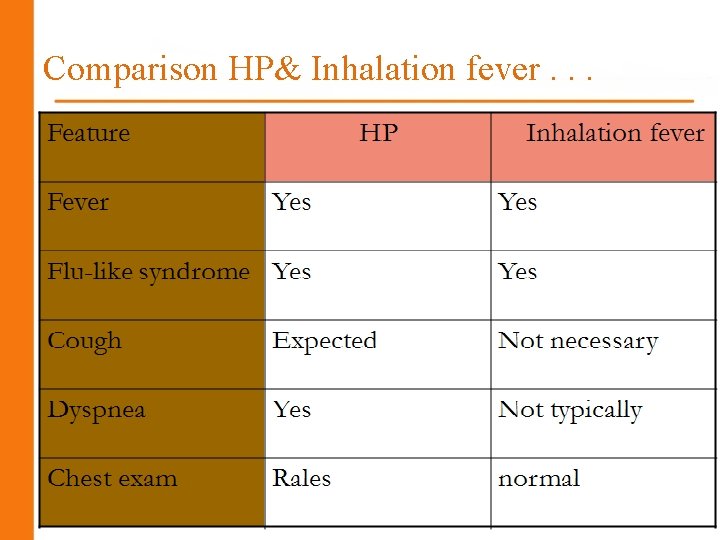
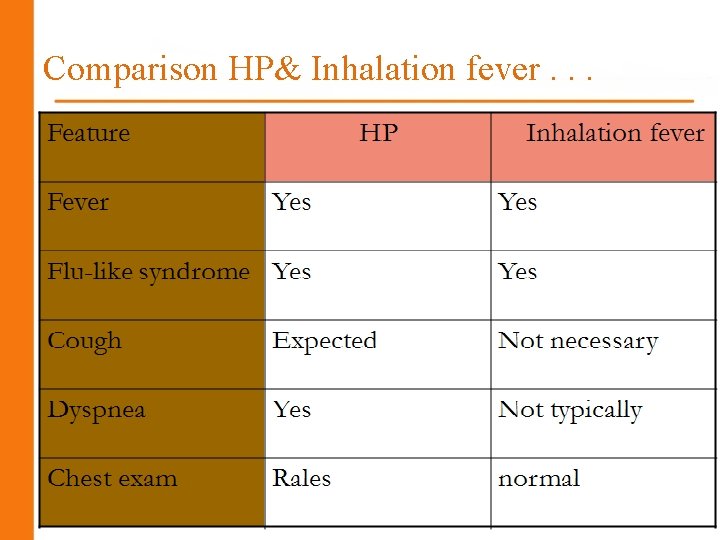
Comparison HP& Inhalation fever. . . 32

Comparison HP& Inhalation fever. . . 33
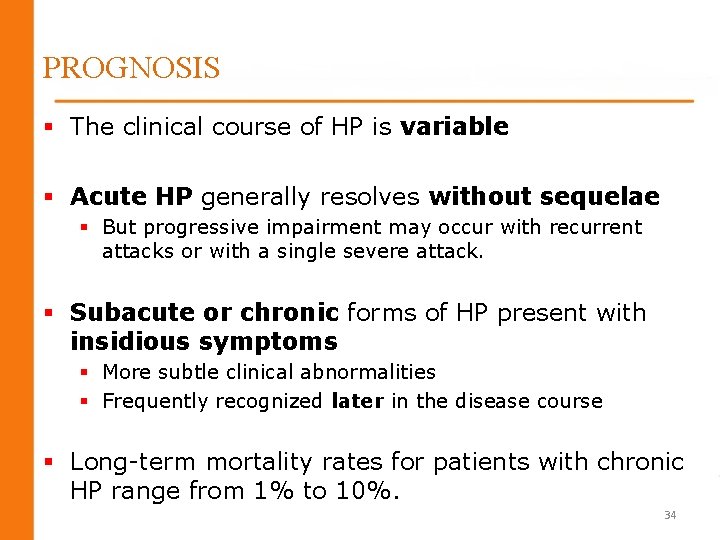
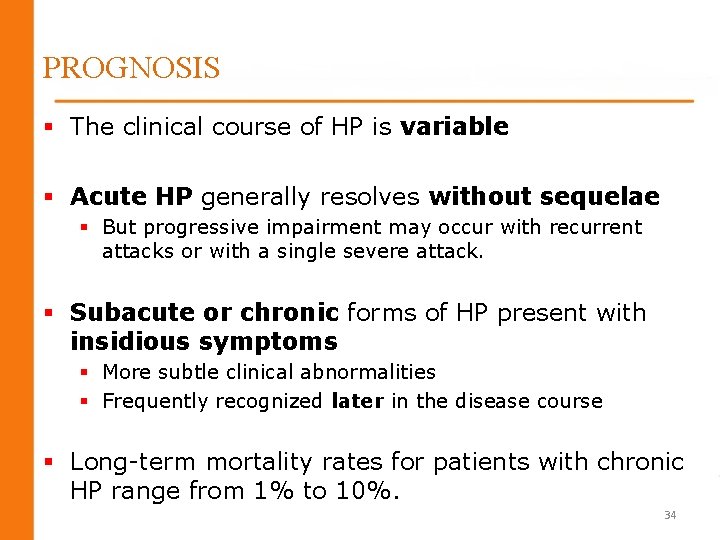
PROGNOSIS § The clinical course of HP is variable § Acute HP generally resolves without sequelae § But progressive impairment may occur with recurrent attacks or with a single severe attack. § Subacute or chronic forms of HP present with insidious symptoms § More subtle clinical abnormalities § Frequently recognized later in the disease course § Long-term mortality rates for patients with chronic HP range from 1% to 10%. 34
Prognostic factors § Age § Duration of exposure after onset of symptoms § Time of exposure prior to diagnosis 35
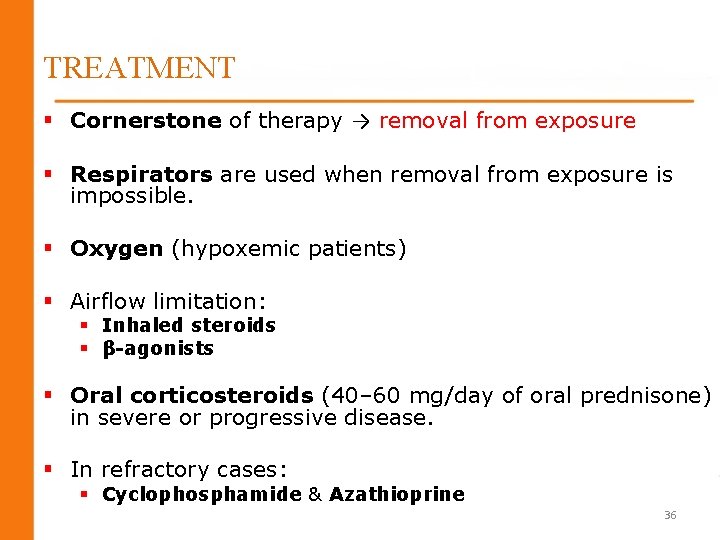
TREATMENT § Cornerstone of therapy → removal from exposure § Respirators are used when removal from exposure is impossible. § Oxygen (hypoxemic patients) § Airflow limitation: § Inhaled steroids § β-agonists § Oral corticosteroids (40– 60 mg/day of oral prednisone) in severe or progressive disease. § In refractory cases: § Cyclophosphamide & Azathioprine 36
37
 Dr aswin djoko baskoro
Dr aswin djoko baskoro Walled world map
Walled world map Hooman hashemi
Hooman hashemi Sayed hadi hashemi
Sayed hadi hashemi Saeid hashemi
Saeid hashemi Hila hashemi
Hila hashemi Carotid sinus hypersensitivity
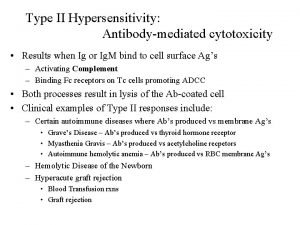
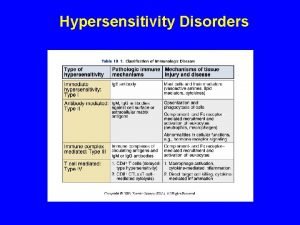
Carotid sinus hypersensitivity Type 2 hypersensitivity
Type 2 hypersensitivity Complications of local anesthesia in dentistry
Complications of local anesthesia in dentistry Pemphigus vulgaris type 2 hypersensitivity
Pemphigus vulgaris type 2 hypersensitivity Hypersensitivity personality
Hypersensitivity personality Hypersensitivity types and examples
Hypersensitivity types and examples Serum sickness hypersensitivity type
Serum sickness hypersensitivity type Defination of hypersensitivity
Defination of hypersensitivity Hypersensitivity
Hypersensitivity Capers allergy
Capers allergy Dermatomyositis hypersensitivity type
Dermatomyositis hypersensitivity type Type 2 hypersensitivity
Type 2 hypersensitivity Hypersensitivity reactions
Hypersensitivity reactions Gingivectomy
Gingivectomy Dental hypersensitivity
Dental hypersensitivity Hygiene hypothesis
Hygiene hypothesis Delayed type hypersensitivity reactions
Delayed type hypersensitivity reactions Visceral hypersensitivity
Visceral hypersensitivity Latex allergy
Latex allergy Hypersensitivity definition
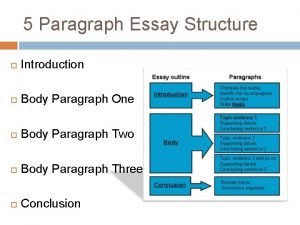
Hypersensitivity definition Essay structure introduction
Essay structure introduction Conclusion of learning without burden
Conclusion of learning without burden Introduction to yacc
Introduction to yacc Dare essay rubric
Dare essay rubric Academic essay
Academic essay Abstract vs introduction
Abstract vs introduction Long introduction
Long introduction Topics to write an email
Topics to write an email Paragraph bridge
Paragraph bridge Introduction answer the question
Introduction answer the question Whats an informative essay
Whats an informative essay Writing an editorial
Writing an editorial