Streptococcal pharyngitis Strep throat Streptococcus pyogenes Resistant to

- Slides: 80
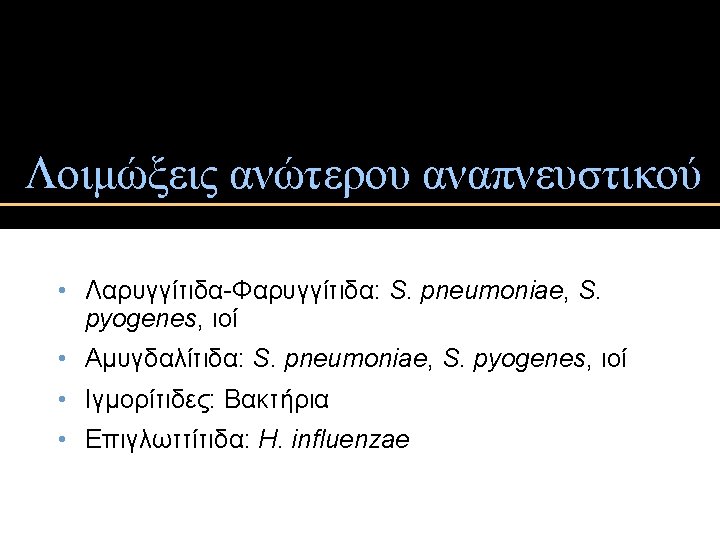
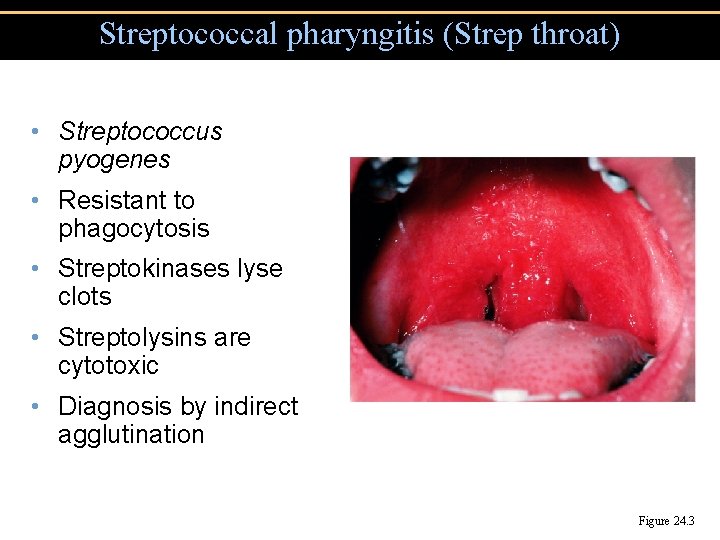
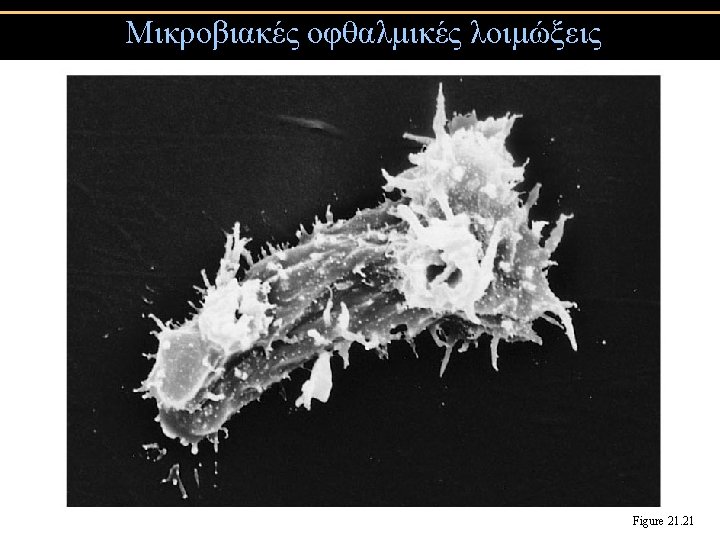
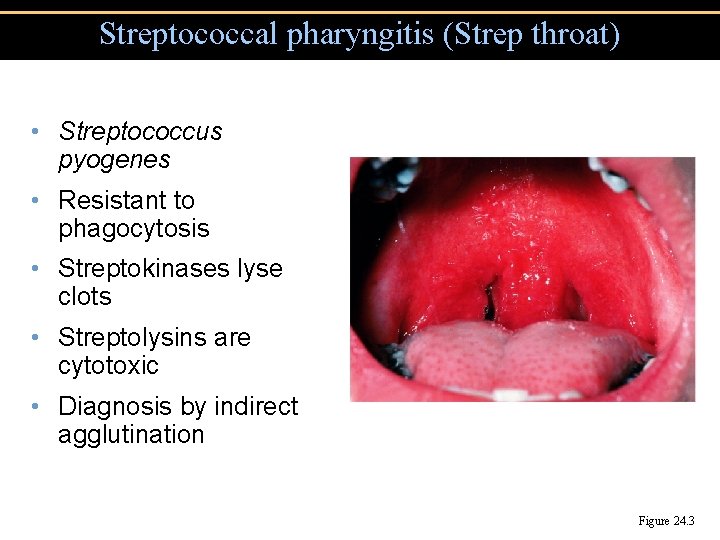
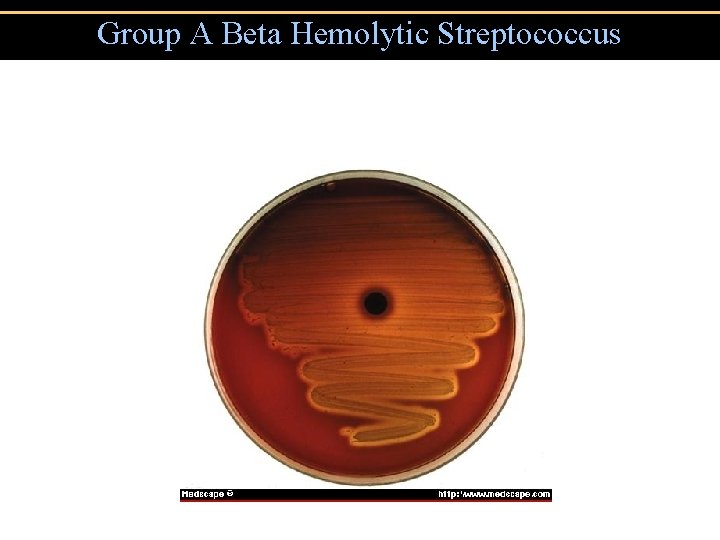
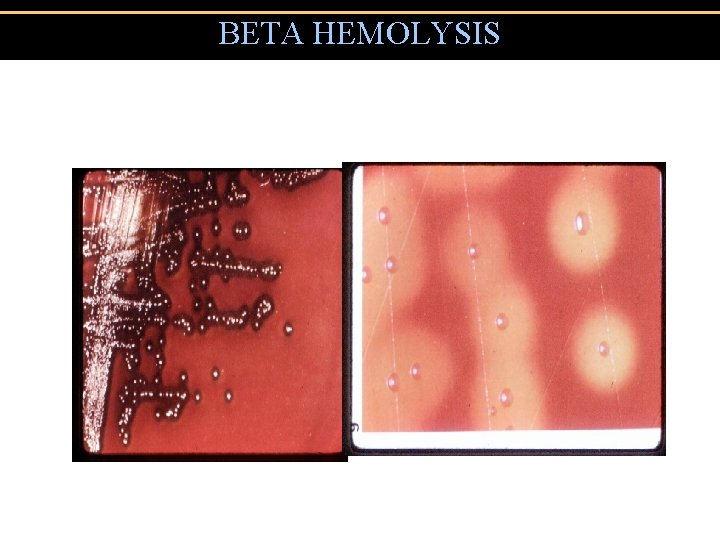
Streptococcal pharyngitis (Strep throat) • Streptococcus pyogenes • Resistant to phagocytosis • Streptokinases lyse clots • Streptolysins are cytotoxic • Diagnosis by indirect agglutination Figure 24. 3

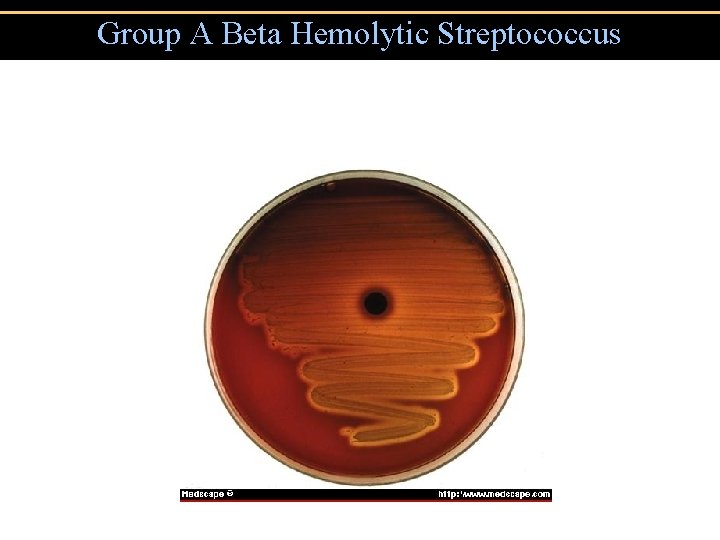
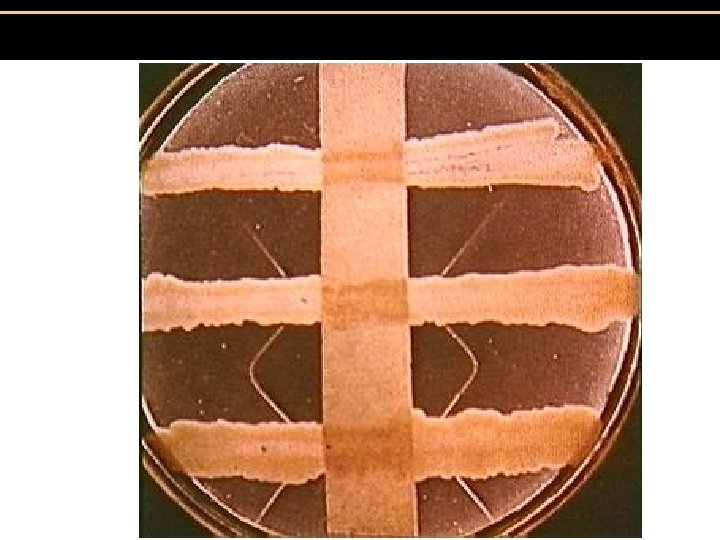
Group A Beta Hemolytic Streptococcus
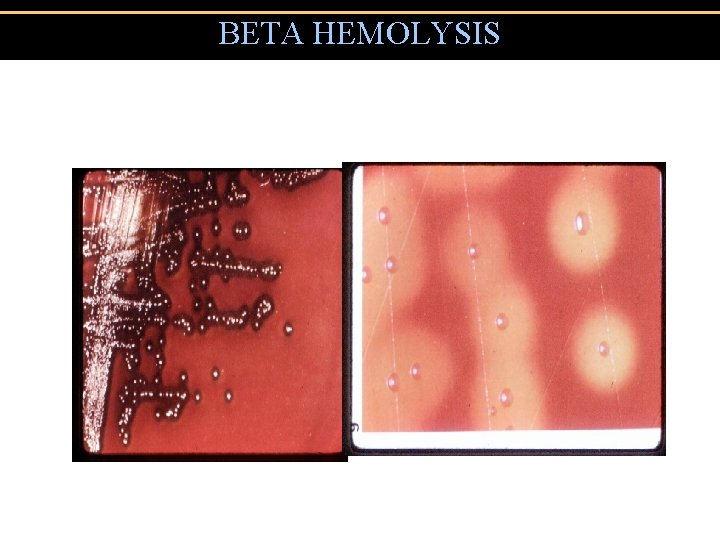
BETA HEMOLYSIS
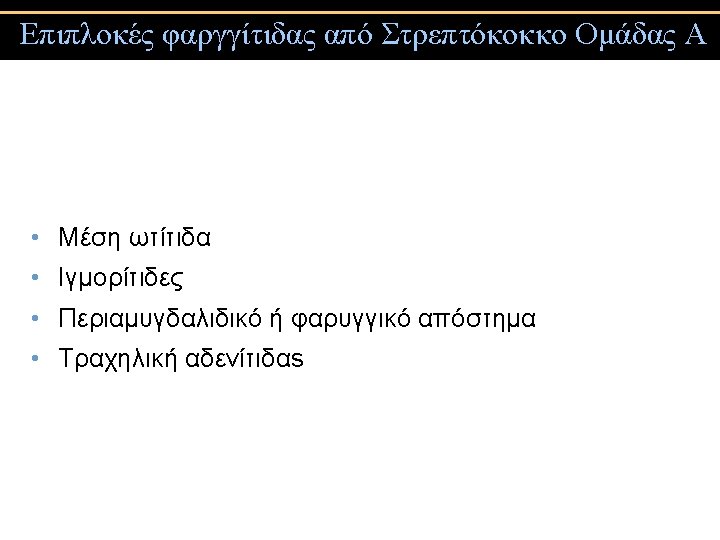
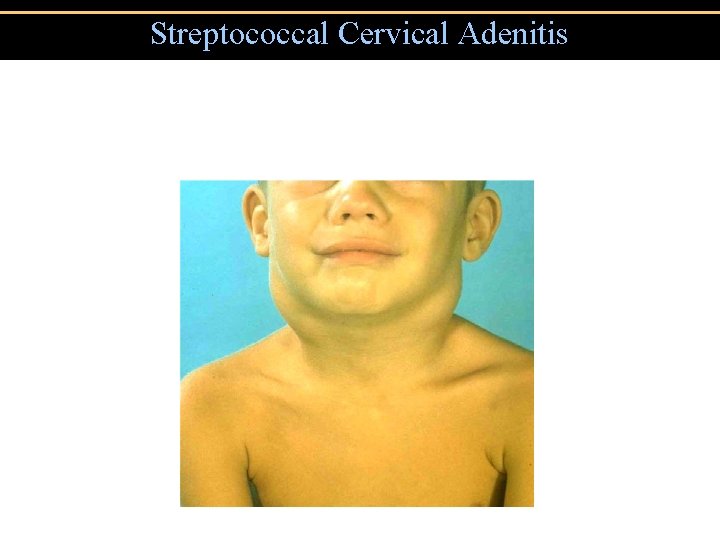
Streptococcal Cervical Adenitis
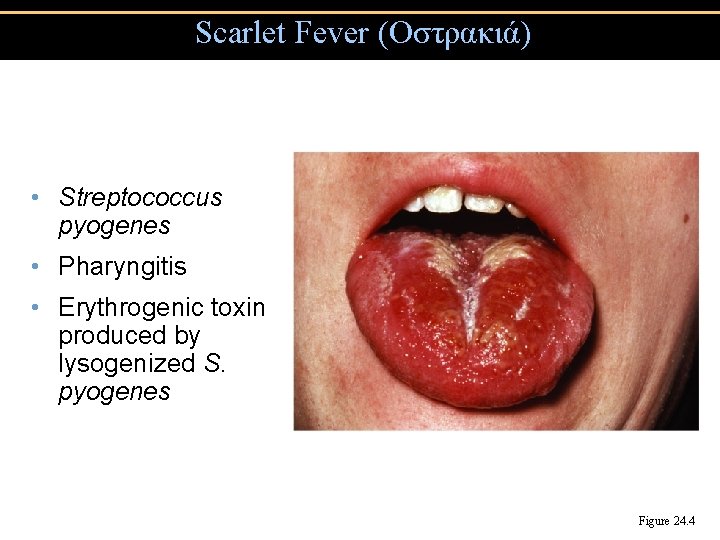
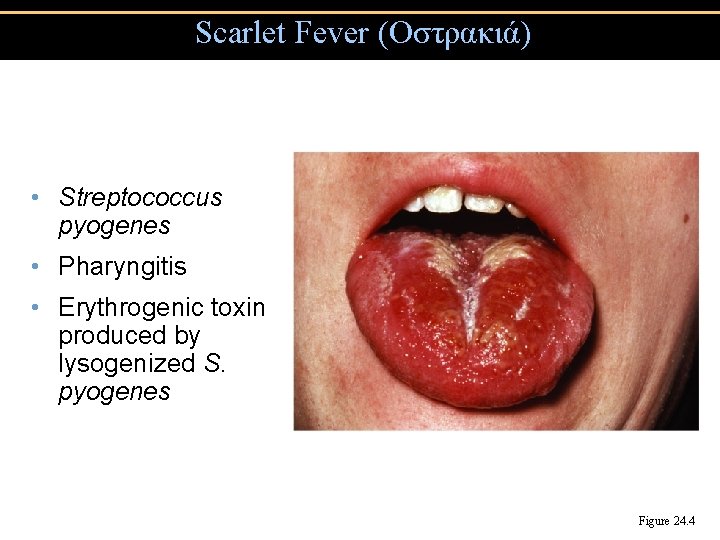
Scarlet Fever (Οστρακιά) • Streptococcus pyogenes • Pharyngitis • Erythrogenic toxin produced by lysogenized S. pyogenes Figure 24. 4
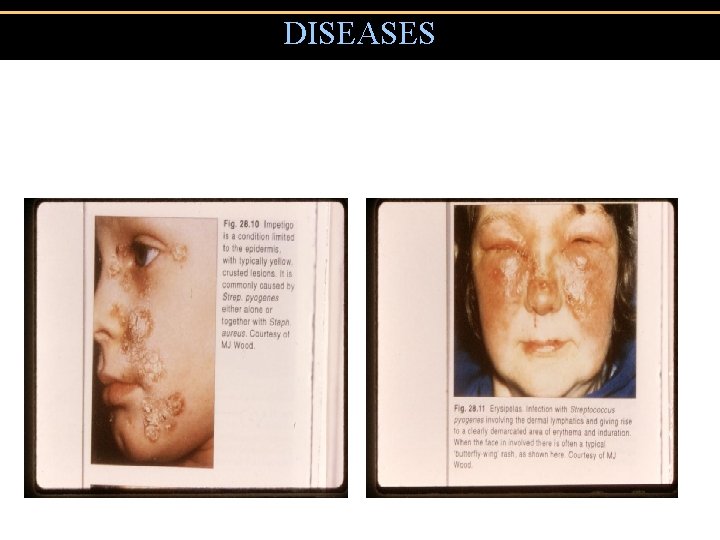
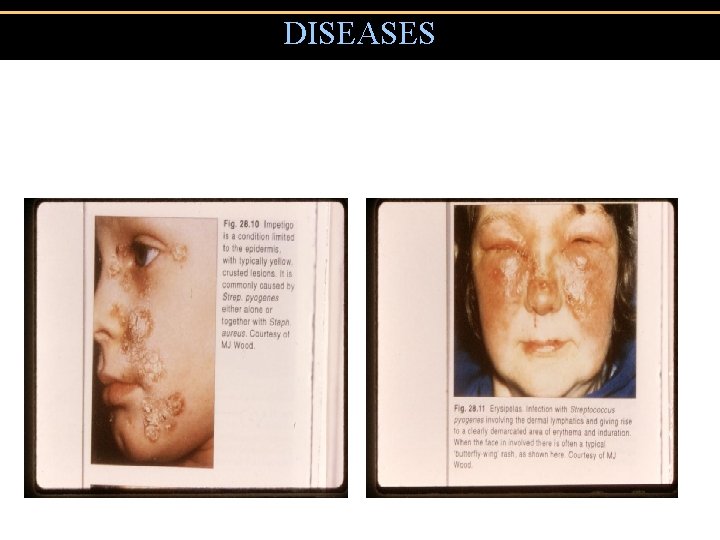
DISEASES • Impetigo • Erysipelas
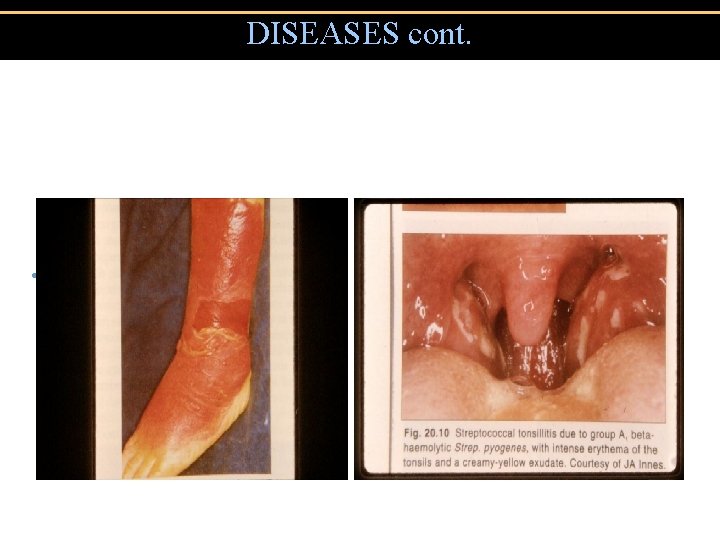
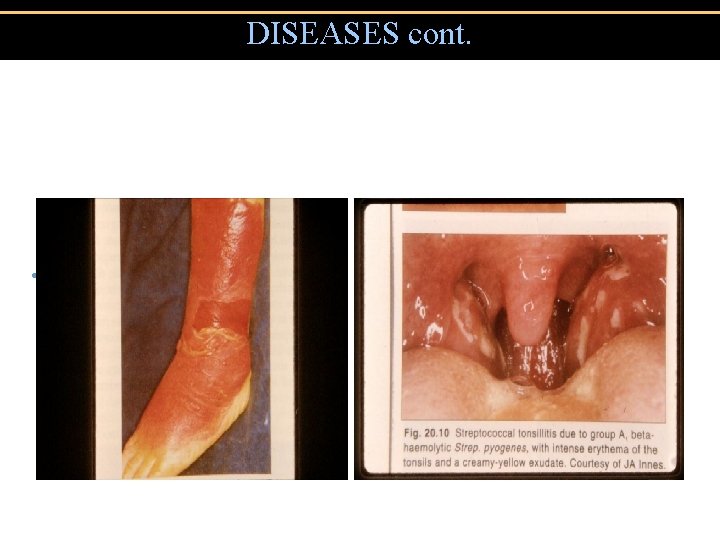
DISEASES cont. • Erysipelas • Tonsillitis
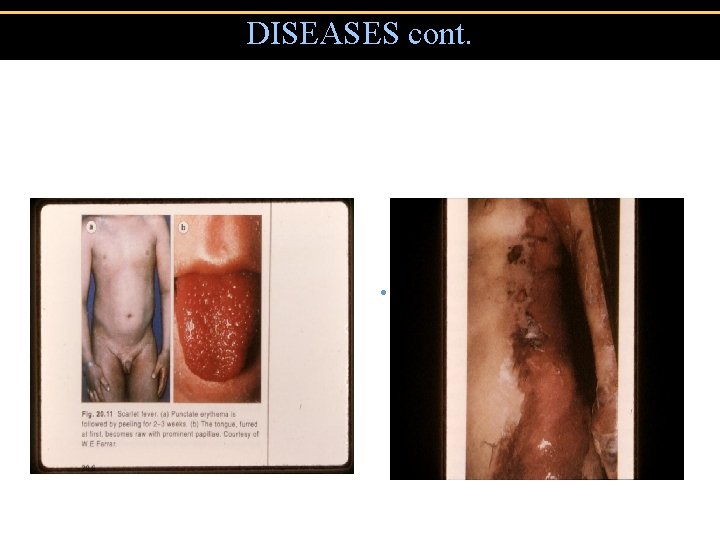
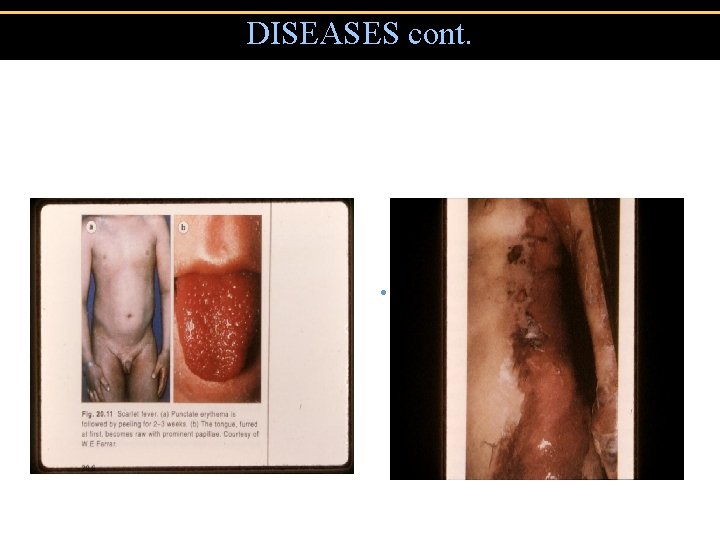
DISEASES cont. • Scarlet Fever • Toxic Shock
Diphtheria • Corynebacterium diphtheriae: Gram-positive rod • Diphtheria membrane of fibrin, dead tissue, and bacteria • Diphtheria toxin produced by lysogenized C. diphtheriae • Prevented by DTa. P and Td vaccine (Diphtheria toxoid) • Cutaneous diphtheria: Infected skin wound leads to slow healing ulcer
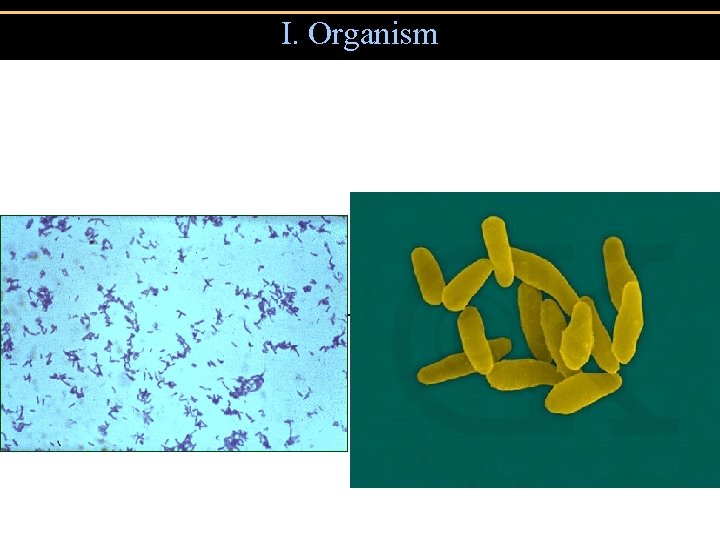
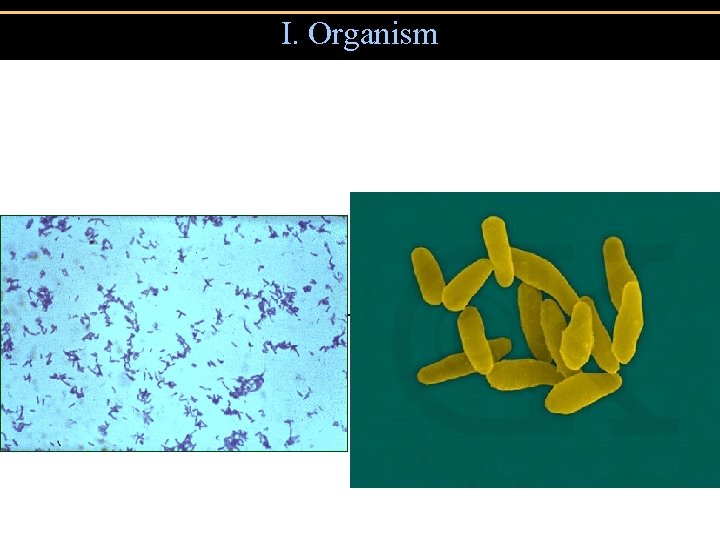
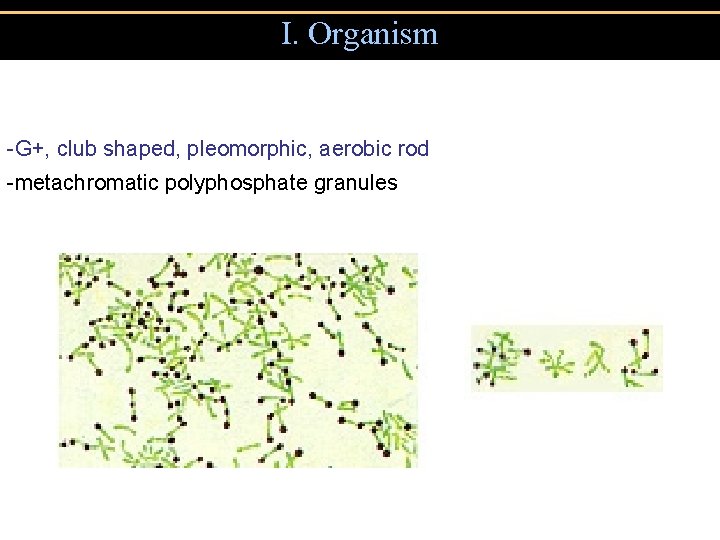
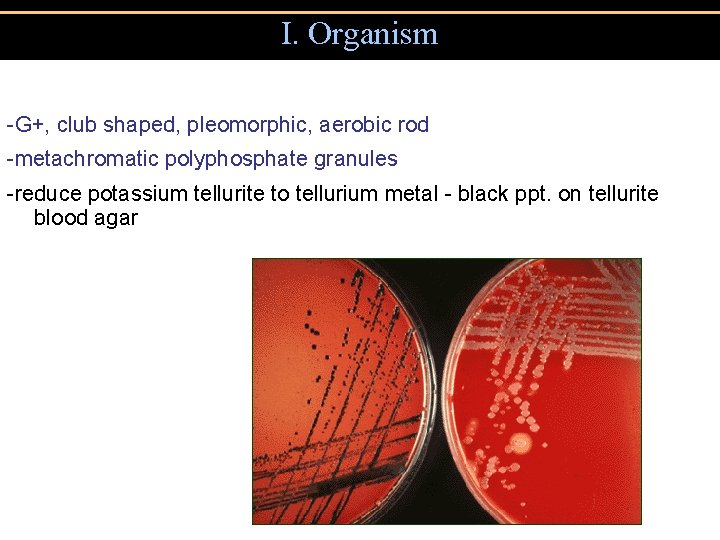
I. Organism -G+, club shaped, pleomorphic, aerobic rod
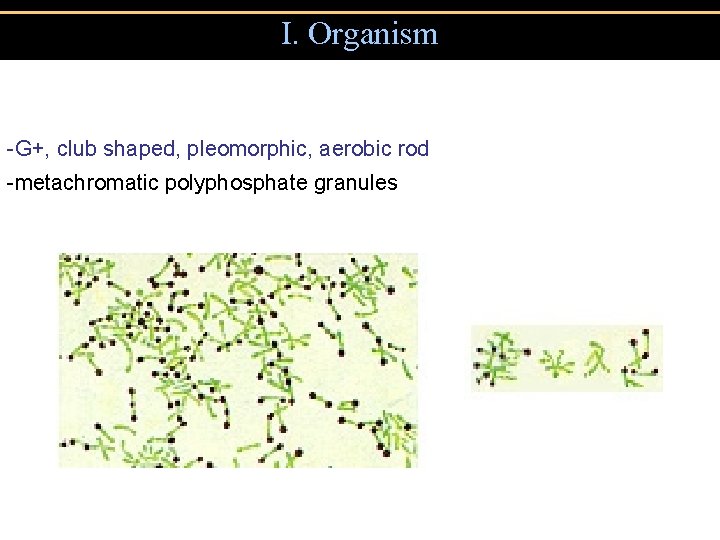
I. Organism -G+, club shaped, pleomorphic, aerobic rod -metachromatic polyphosphate granules
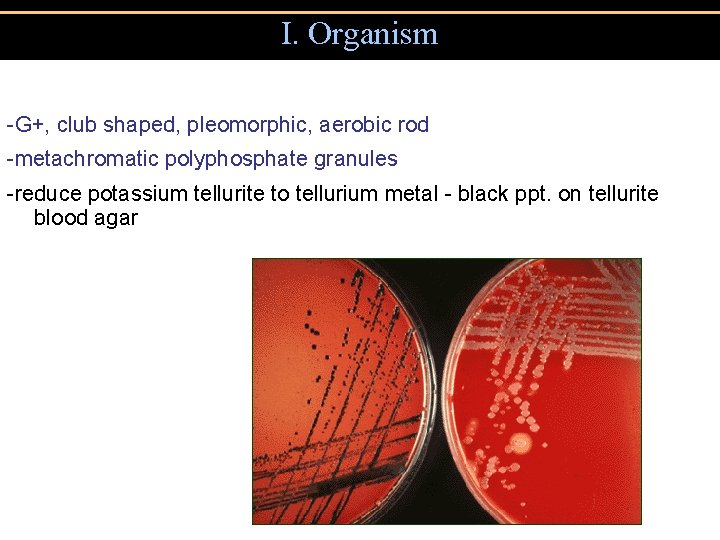
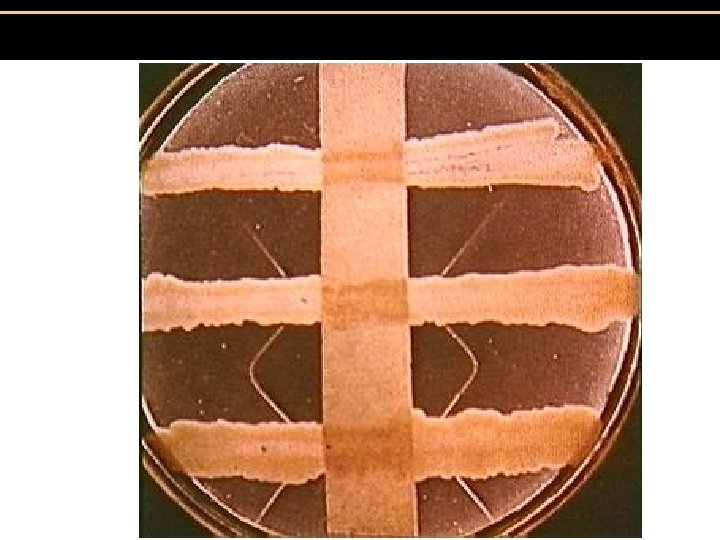
I. Organism -G+, club shaped, pleomorphic, aerobic rod -metachromatic polyphosphate granules -reduce potassium tellurite to tellurium metal - black ppt. on tellurite blood agar
I. Organism -G+, club shaped, pleomorphic, aerobic rod -metachromatic polyphosphate granules -reduce potassium tellurite to tellurium metal - black ppt. on tellurite blood agar -subtypes gravis, intermedius, mitis: severity of infection differs depending on growth rate of subtype
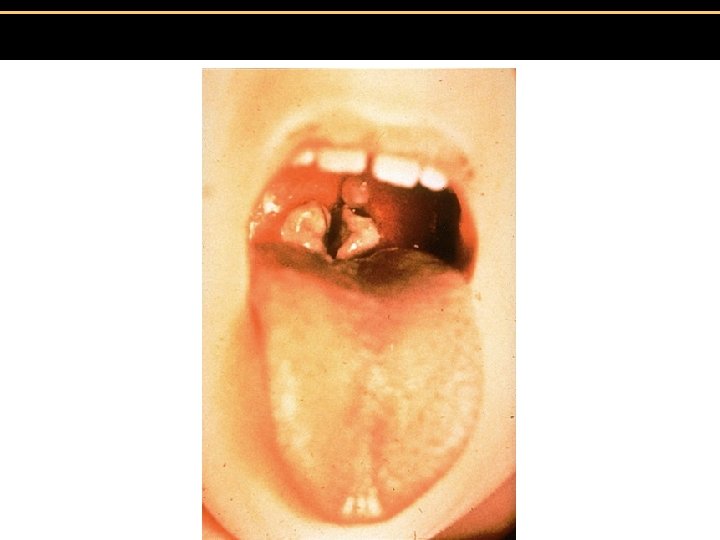
II. Clinical -usually presents as throat infection w/ sore throat, fever, sometimes swollen lymph glands -”pseudomembrane” forms at back of throat - may obstruct airway (“la garottilla”)
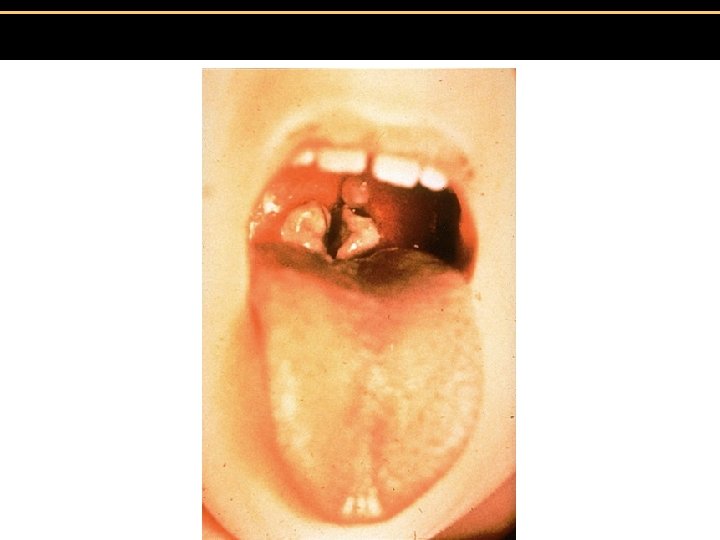
Pseudomembrane in Diptheria
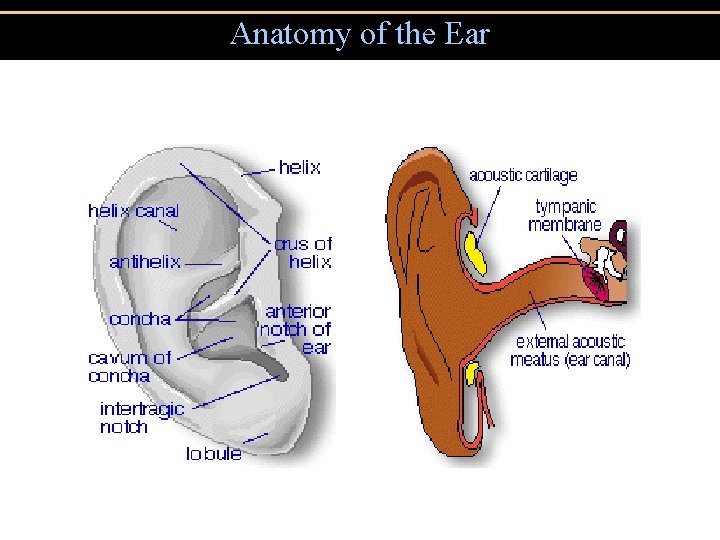
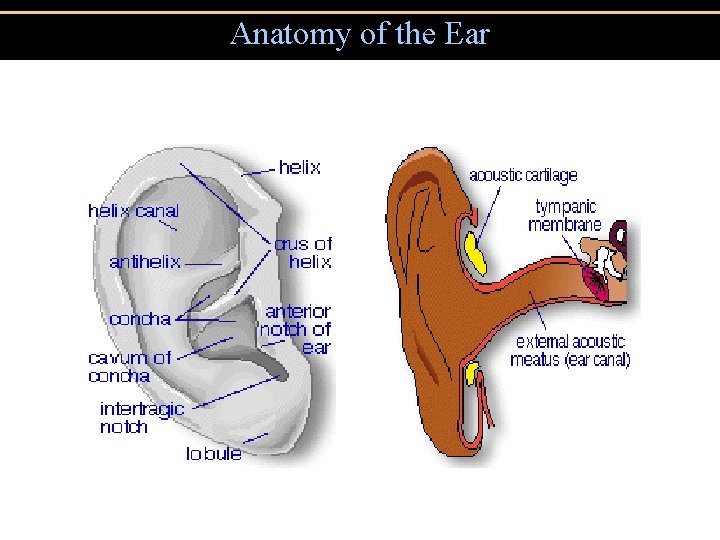
Anatomy of the Ear
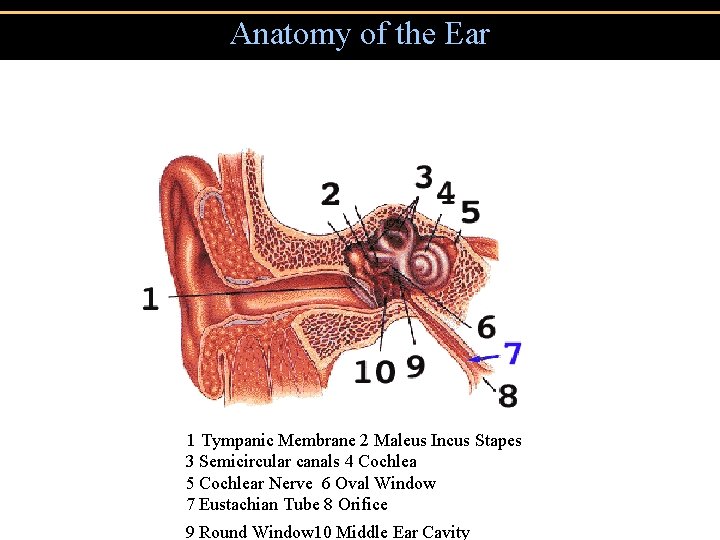
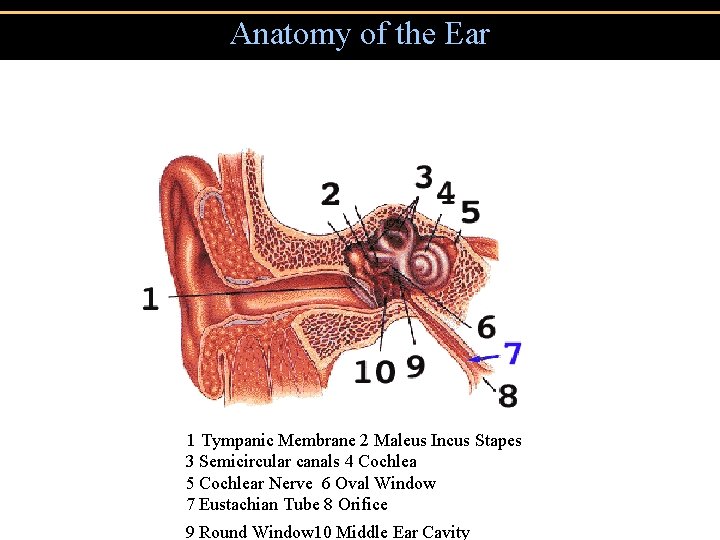
Anatomy of the Ear 1 Tympanic Membrane 2 Maleus Incus Stapes 3 Semicircular canals 4 Cochlea 5 Cochlear Nerve 6 Oval Window 7 Eustachian Tube 8 Orifice 9 Round Window 10 Middle Ear Cavity
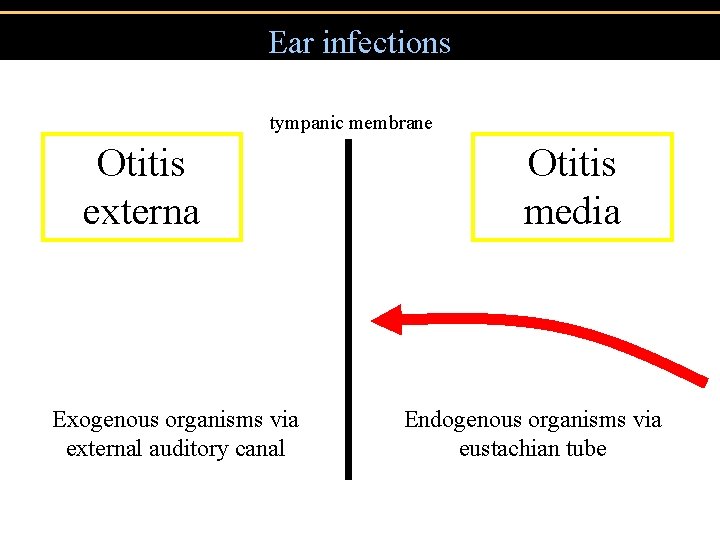
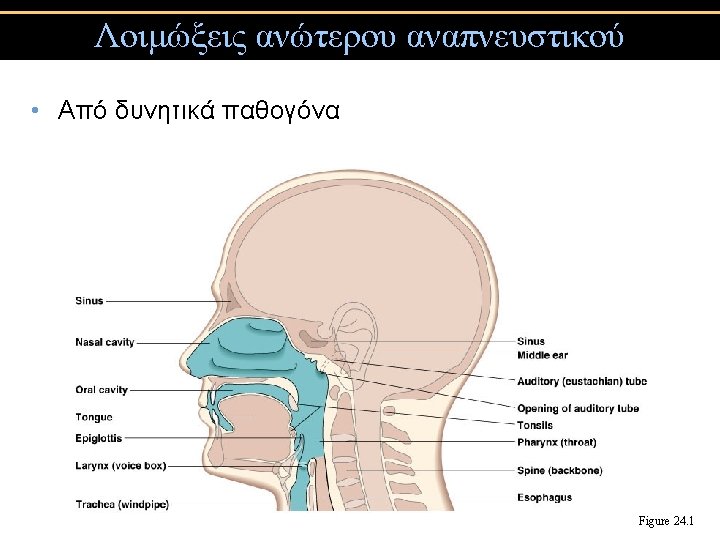
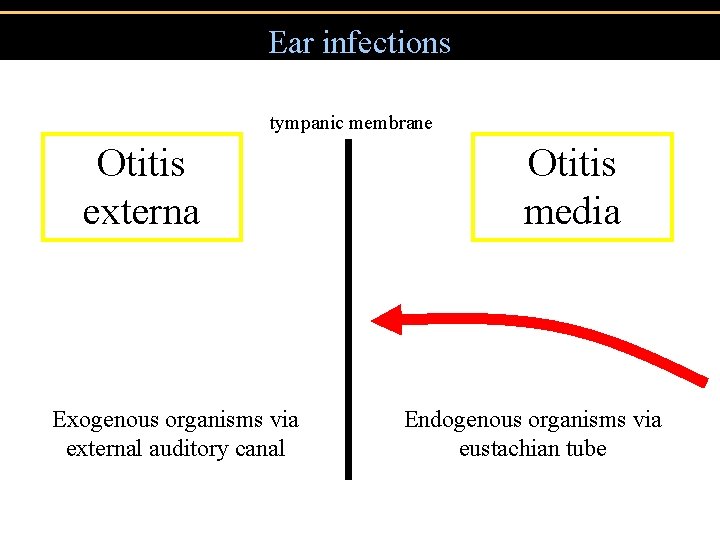
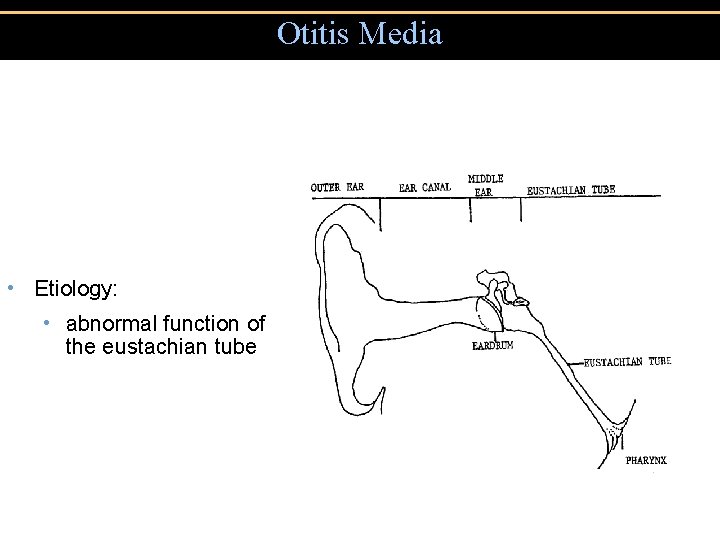
Ear infections tympanic membrane Otitis externa Exogenous organisms via external auditory canal Otitis media Endogenous organisms via eustachian tube
Otitis Media • Epidemiology and Pathophysiology: • age - almost all children have one or more episodes before age 6 • about 10% of children develop OM by age 3 months • peak incidence between ages 6 and 15 months
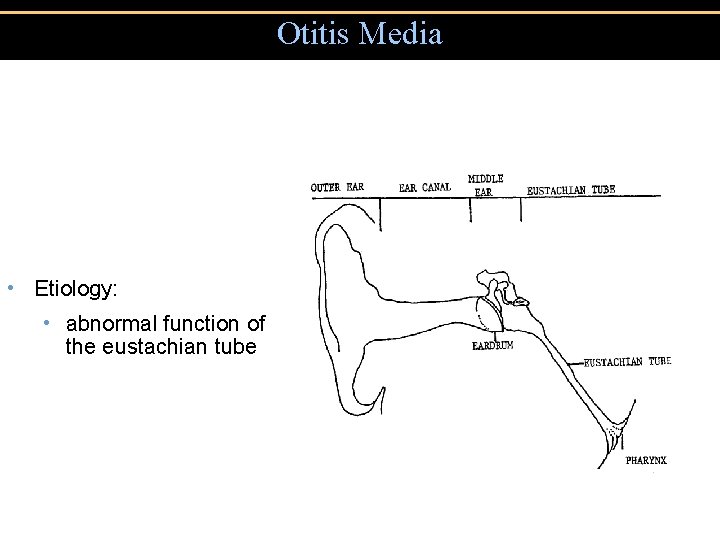
Otitis Media • Etiology: • abnormal function of the eustachian tube
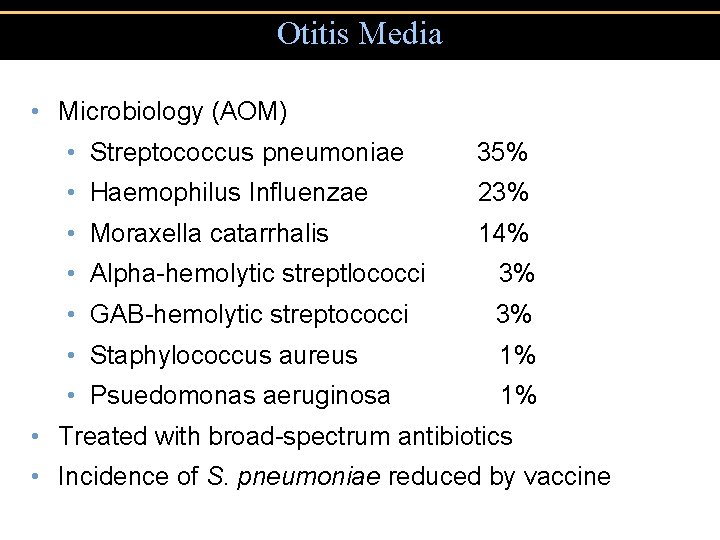
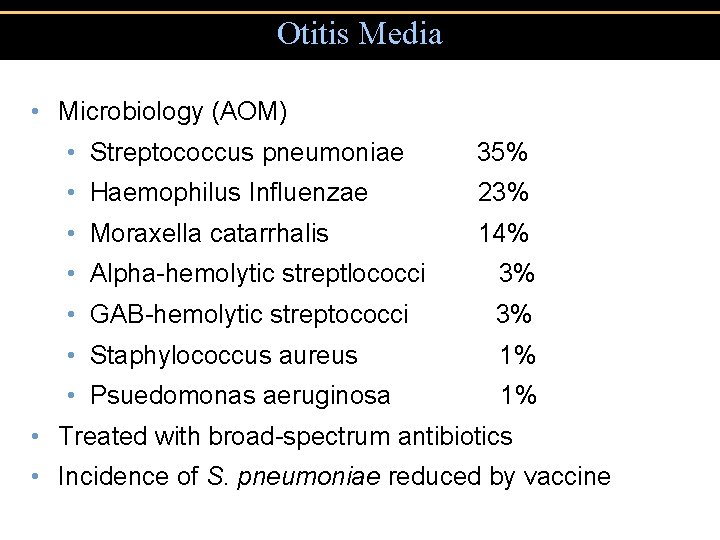
Otitis Media • Microbiology (AOM) • Streptococcus pneumoniae 35% • Haemophilus Influenzae 23% • Moraxella catarrhalis 14% • Alpha-hemolytic streptlococci 3% • GAB-hemolytic streptococci 3% • Staphylococcus aureus 1% • Psuedomonas aeruginosa 1% • Treated with broad-spectrum antibiotics • Incidence of S. pneumoniae reduced by vaccine
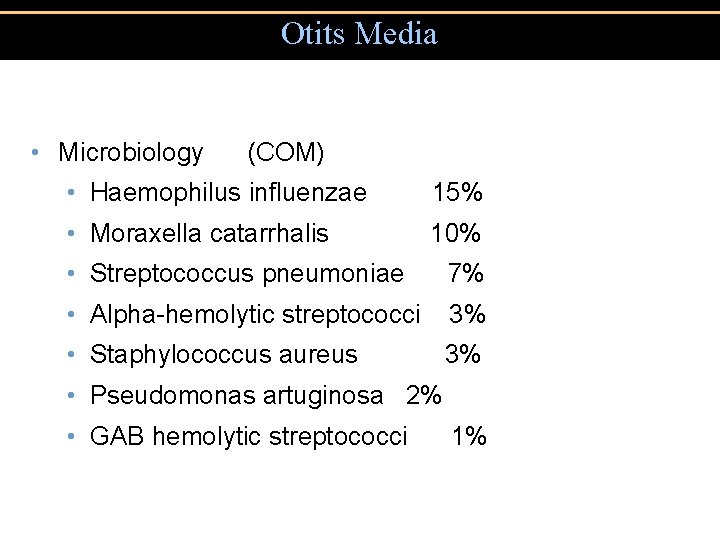
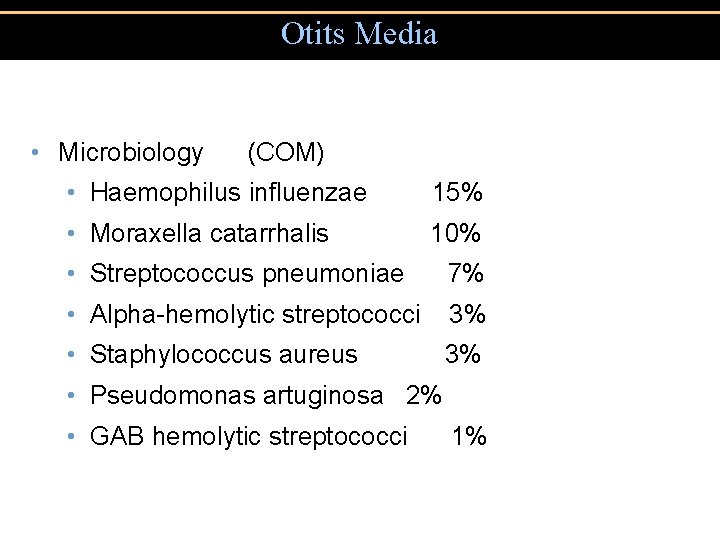
Otits Media • Microbiology (COM) • Haemophilus influenzae 15% • Moraxella catarrhalis 10% • Streptococcus pneumoniae 7% • Alpha-hemolytic streptococci 3% • Staphylococcus aureus 3% • Pseudomonas artuginosa 2% • GAB hemolytic streptococci 1%
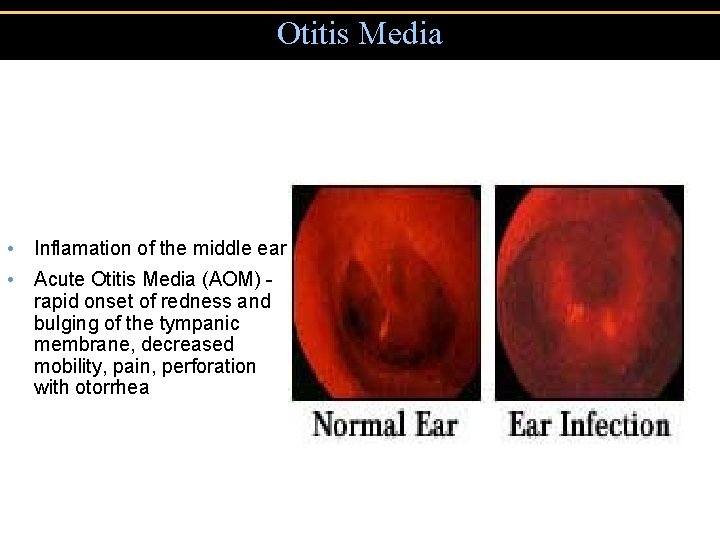
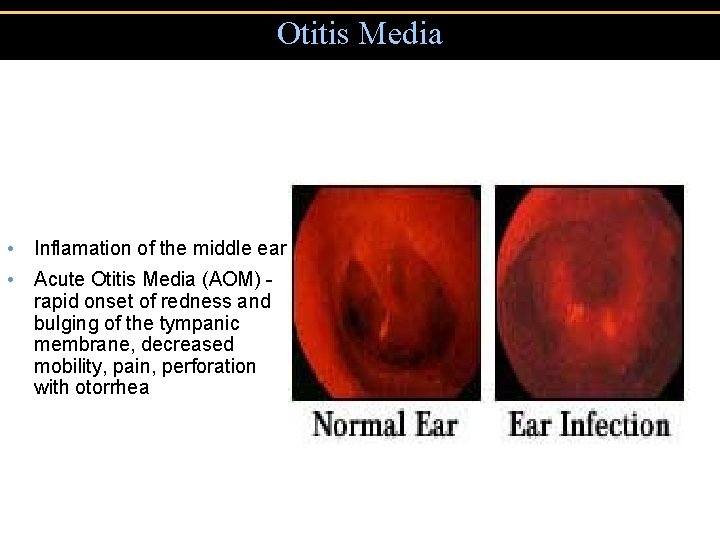
Otitis Media • Inflamation of the middle ear • Acute Otitis Media (AOM) rapid onset of redness and bulging of the tympanic membrane, decreased mobility, pain, perforation with otorrhea
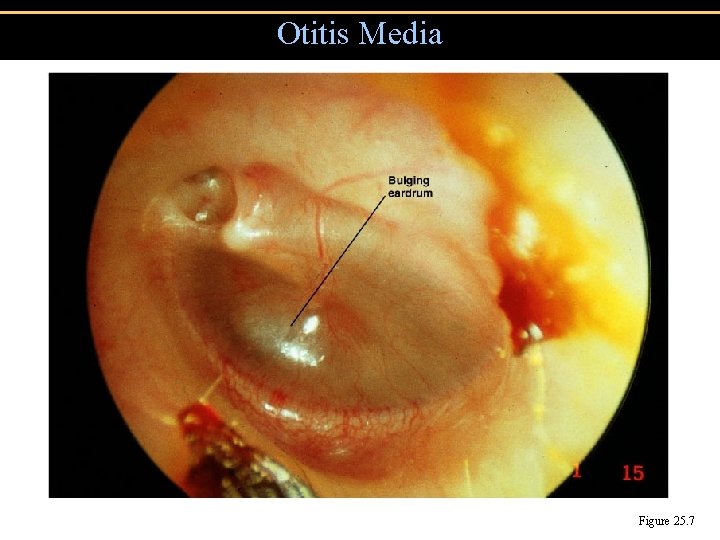
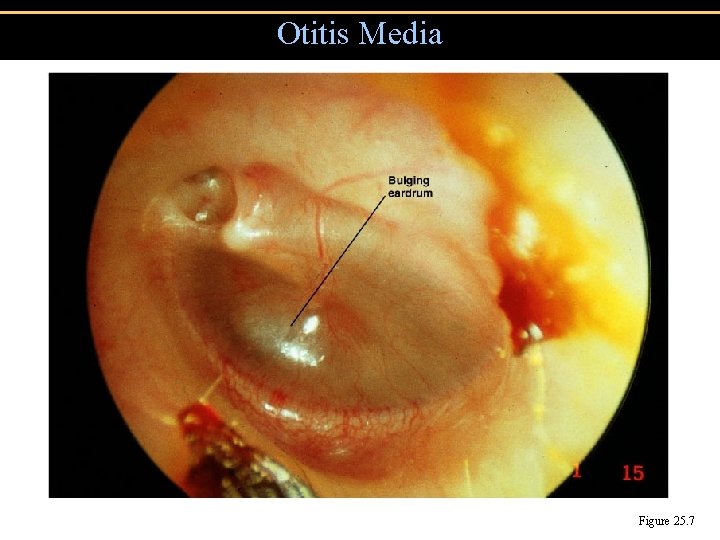
Otitis Media Figure 25. 7
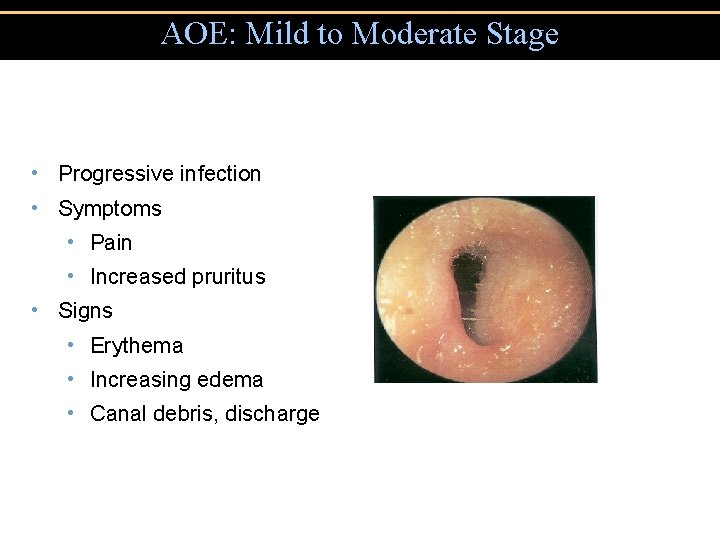
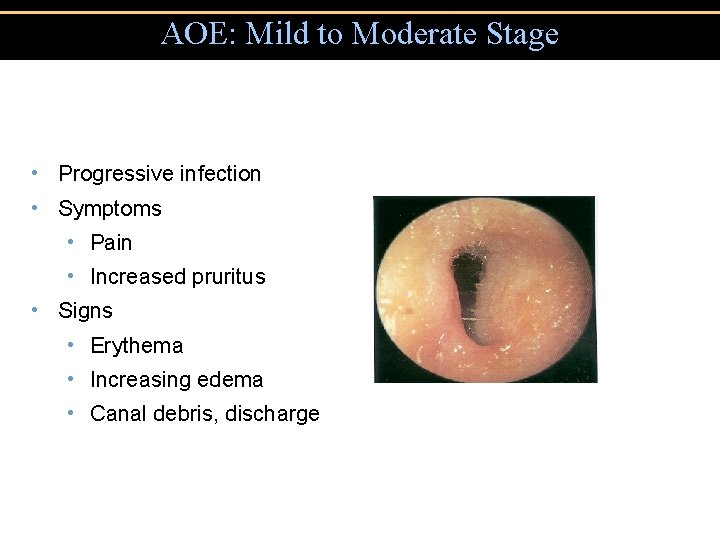
AOE: Mild to Moderate Stage • Progressive infection • Symptoms • Pain • Increased pruritus • Signs • Erythema • Increasing edema • Canal debris, discharge
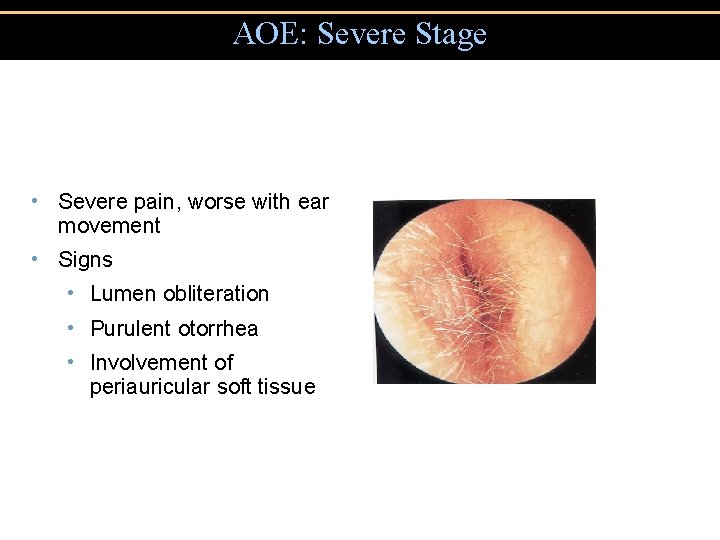
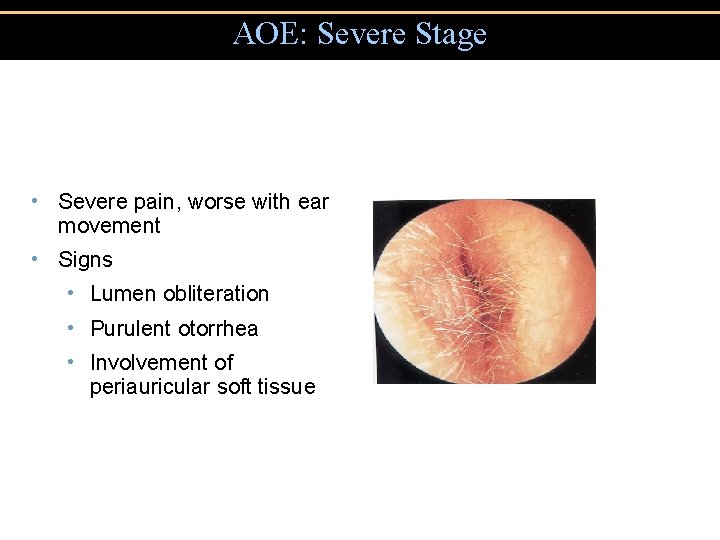
AOE: Severe Stage • Severe pain, worse with ear movement • Signs • Lumen obliteration • Purulent otorrhea • Involvement of periauricular soft tissue
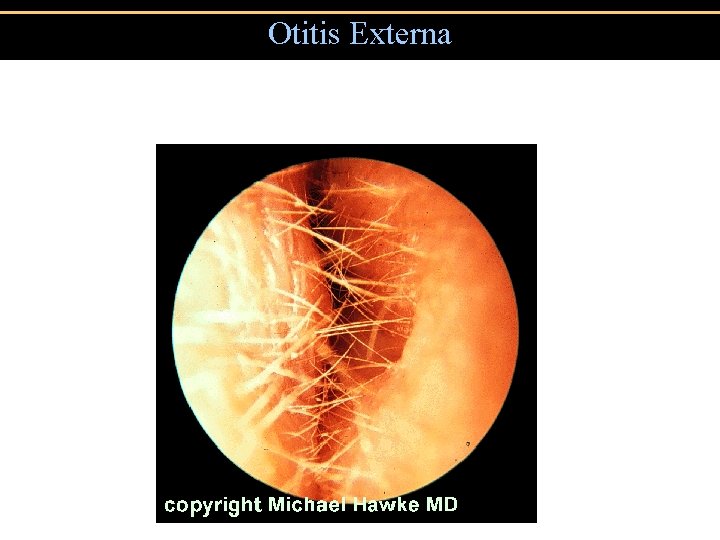
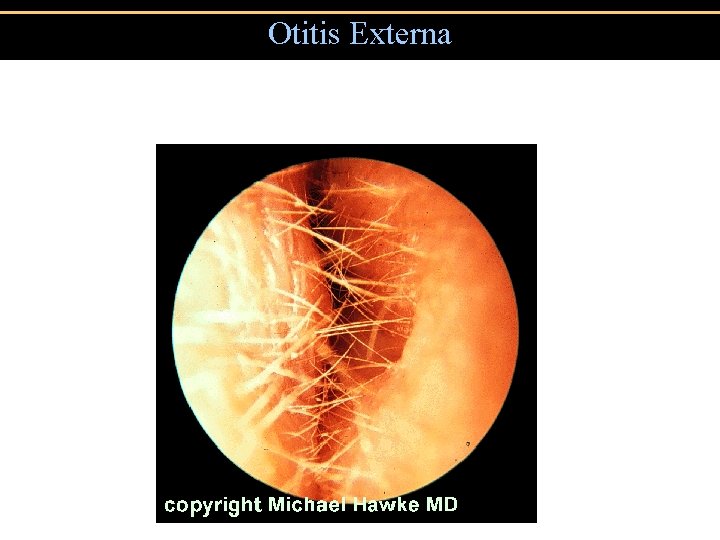
Otitis Externa
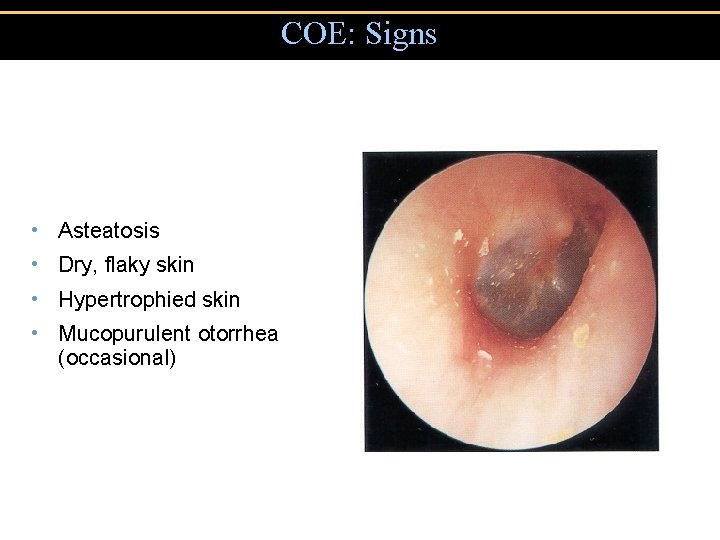
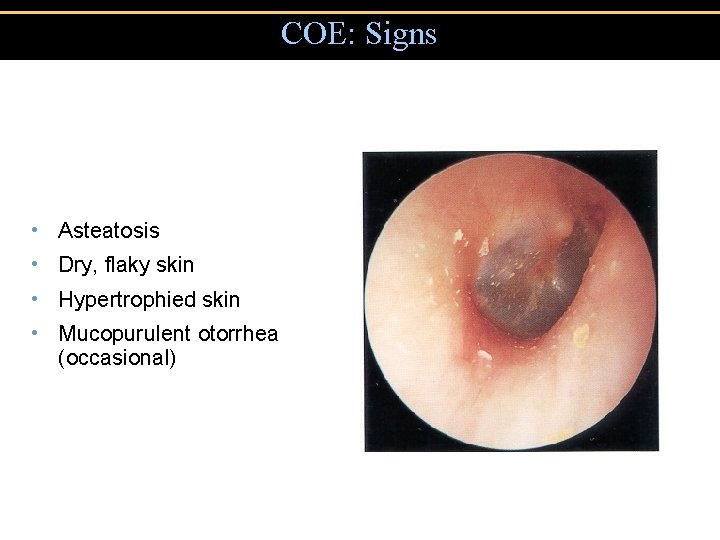
COE: Signs • Asteatosis • Dry, flaky skin • Hypertrophied skin • Mucopurulent otorrhea (occasional)
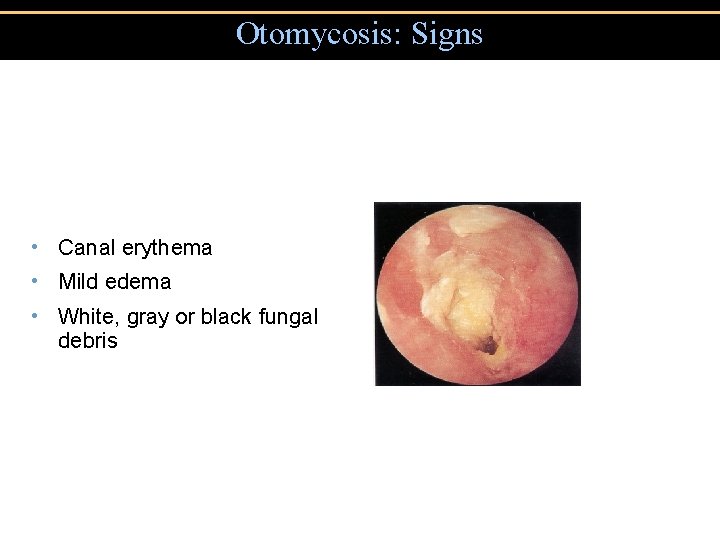
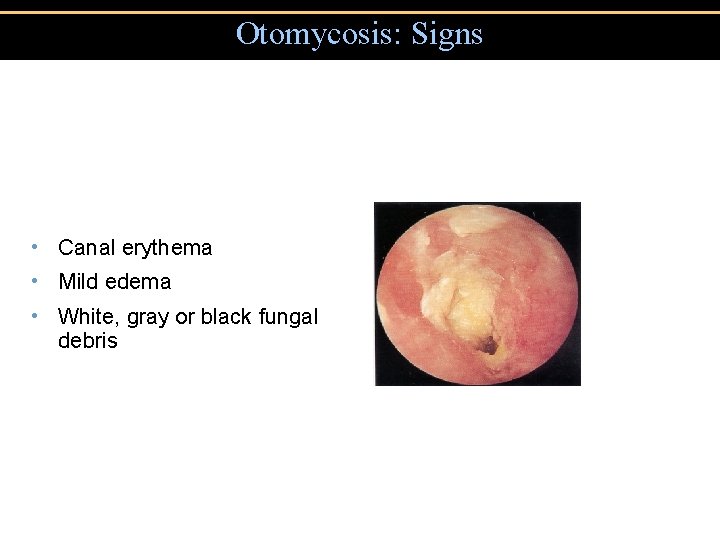
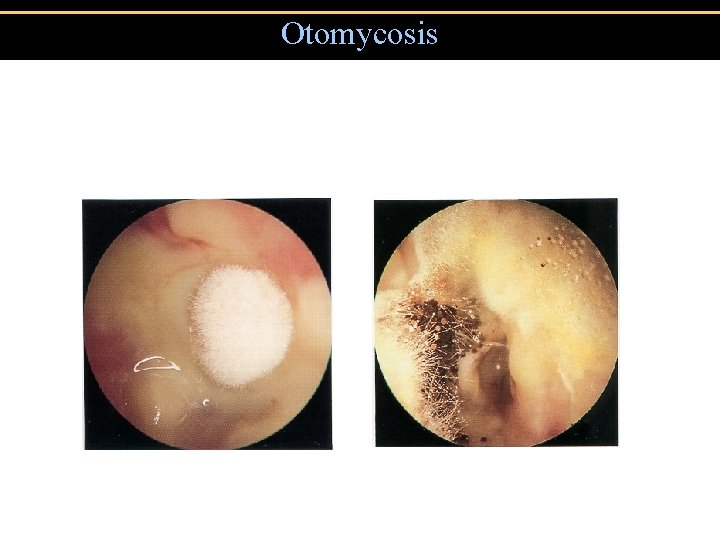
Otomycosis: Signs • Canal erythema • Mild edema • White, gray or black fungal debris
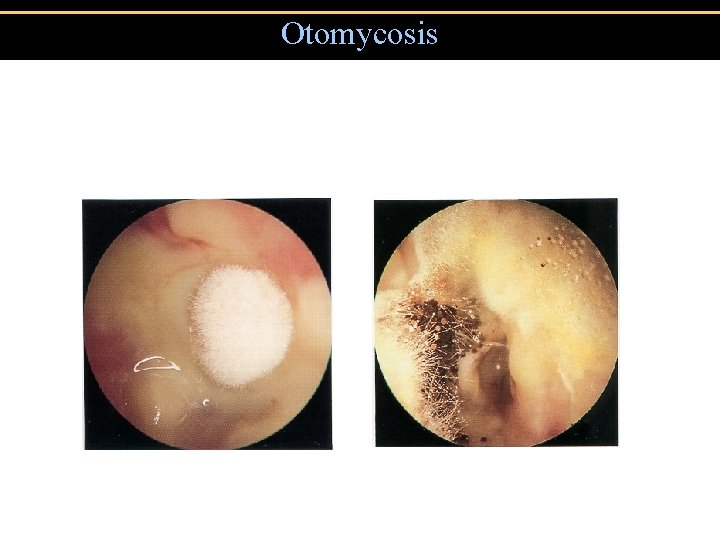
Otomycosis
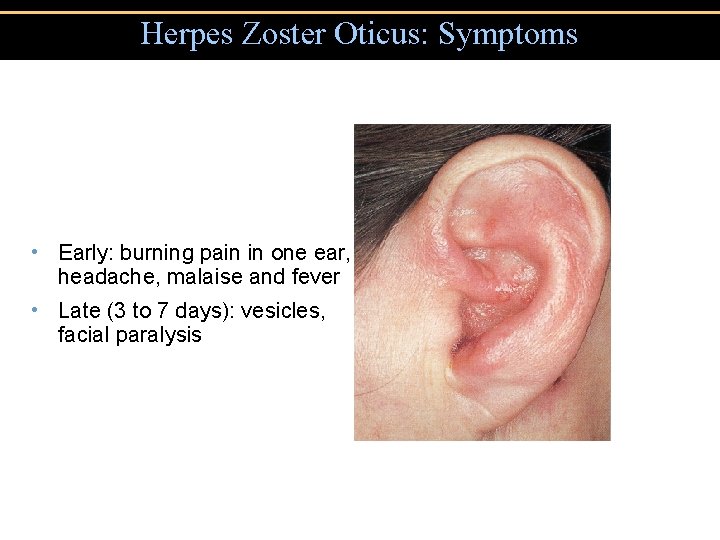
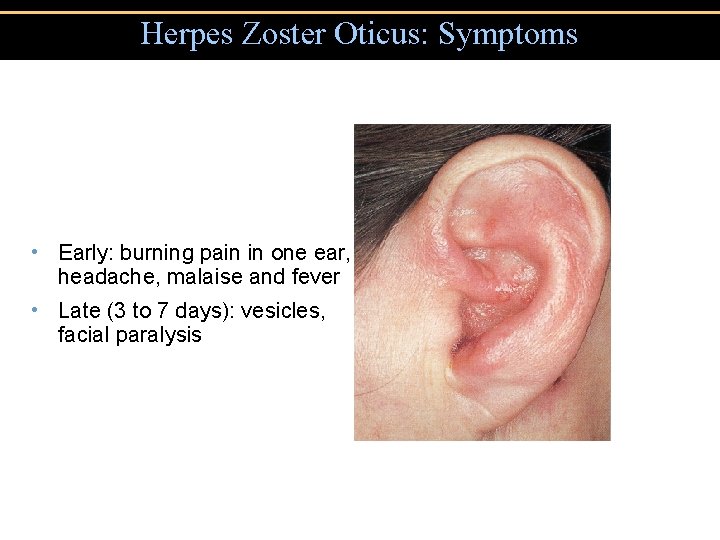
Herpes Zoster Oticus: Symptoms • Early: burning pain in one ear, headache, malaise and fever • Late (3 to 7 days): vesicles, facial paralysis
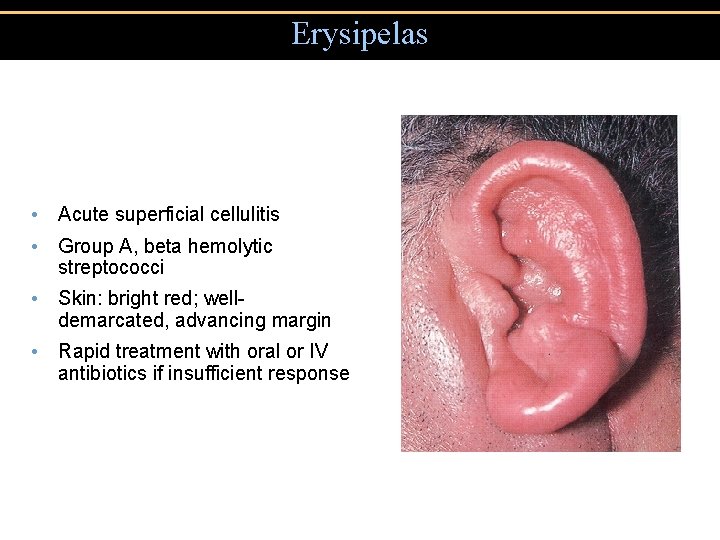
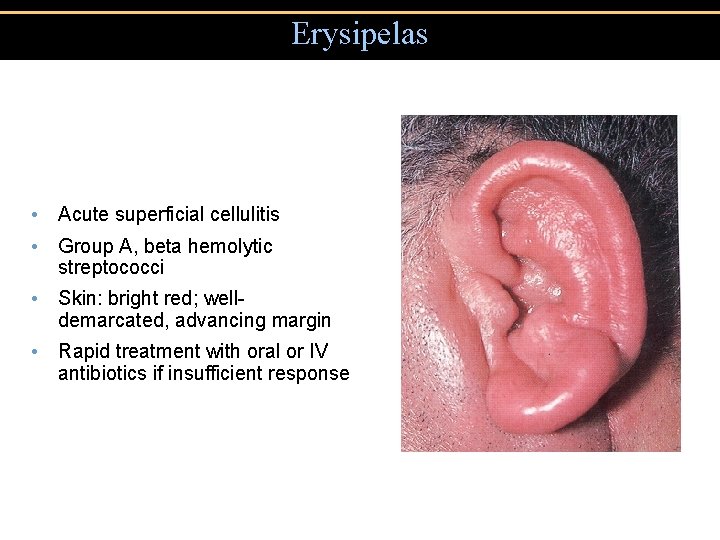
Erysipelas • Acute superficial cellulitis • Group A, beta hemolytic streptococci • Skin: bright red; welldemarcated, advancing margin • Rapid treatment with oral or IV antibiotics if insufficient response
Otitis externa • Organisms - Pseudomonas aeruginosa - Staphylococcus aureus - Aspergillus spp. • Treatment - oral antibiotics – NO! - topical broad spectrum (thick drops or wicks) - cotricosteroids • Prevention - avoid predisposing events. ( post swim drops, blue tack, ear “ NO GO” zone)
Sinusitis • 32 million cases annually in U. S. • 0. 5 -0. 2% of colds are complicated by sinusitis • Most acute sinusitis occurs from viral and bacterial co-infection
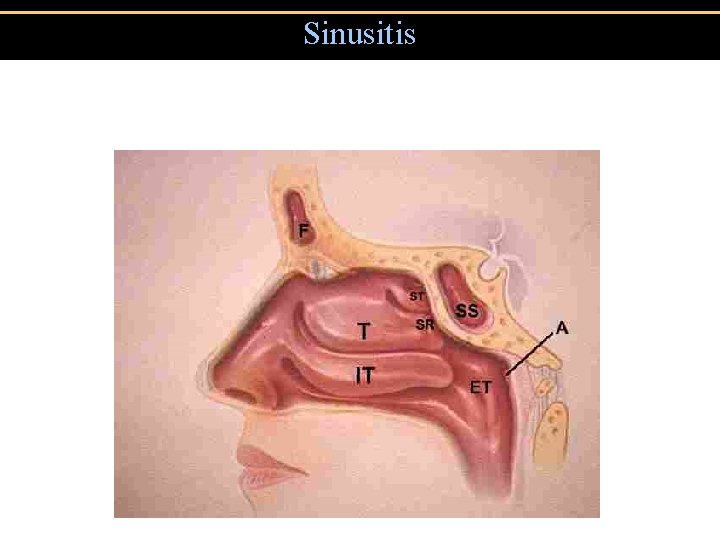
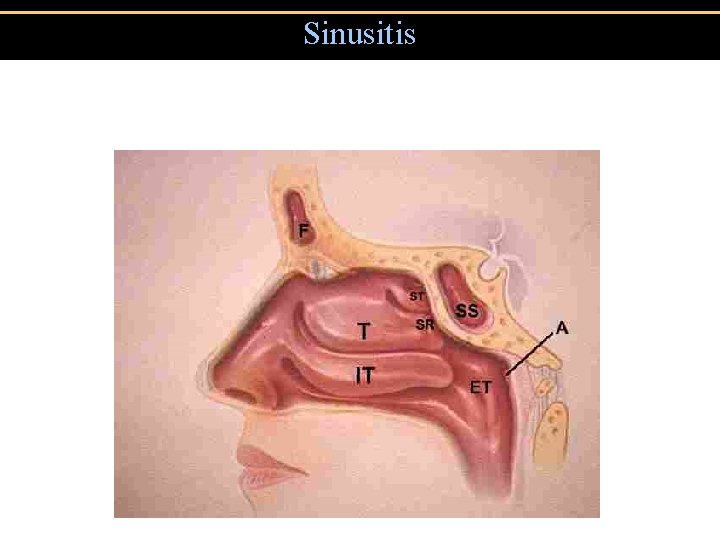
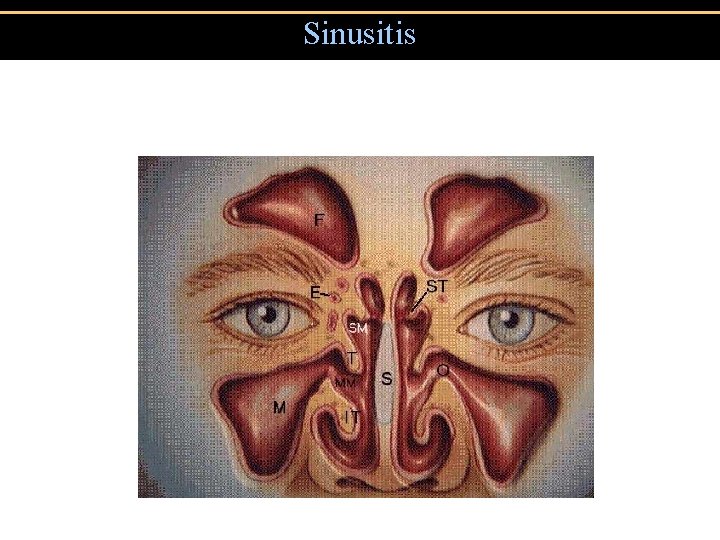
Sinusitis
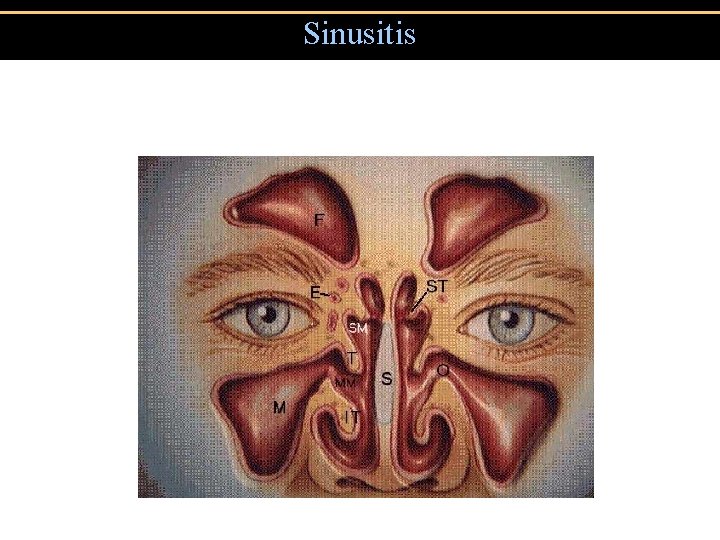
Sinusitis
Sinusitis • Major symptoms • Facial Pain* • Nasal Obstruction • Nasal Discharge • Postnasal Drainage • Hyposmia • Fever *Location = diagnosis • Minor Symptoms • Headache • Halitosis • Fatigue • Oral Pain • Cough • Ear pain, pressure, fullness
Sinusitis • Microbiology • S. pneumoniae and H. influenzae cause 70% of sinusitis • Anaerobes, S. aureus and M. catarrhalis cause most of remaining 30%
Common cold • Rhinoviruses (50%) • Coronaviruses (15 -20%) • Rhinoviruses attached to ICAN-1 on nasal mucosa
Microbial Diseases of the Lower Respiratory System • Bacteria, viruses, & fungi cause: • Bronchitis • Bronchiolitis • Pneumonia
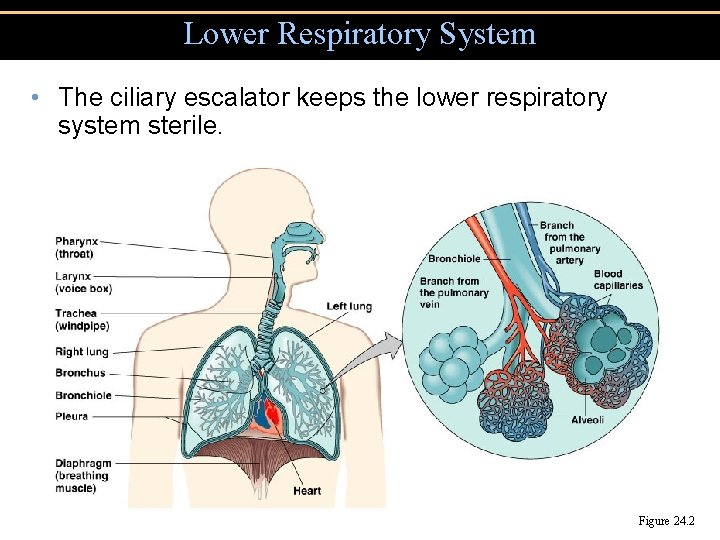
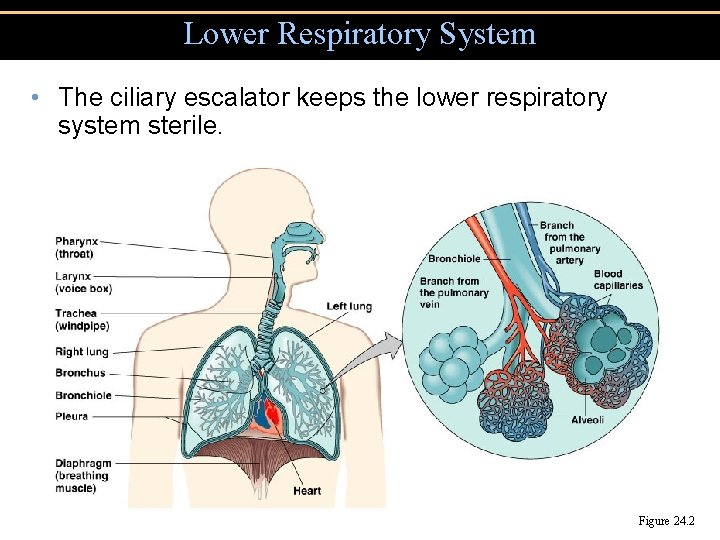
Lower Respiratory System • The ciliary escalator keeps the lower respiratory system sterile. Figure 24. 2
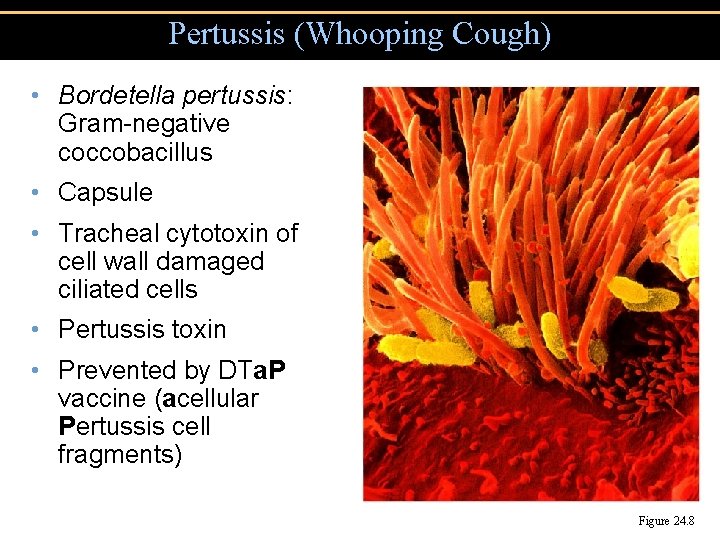
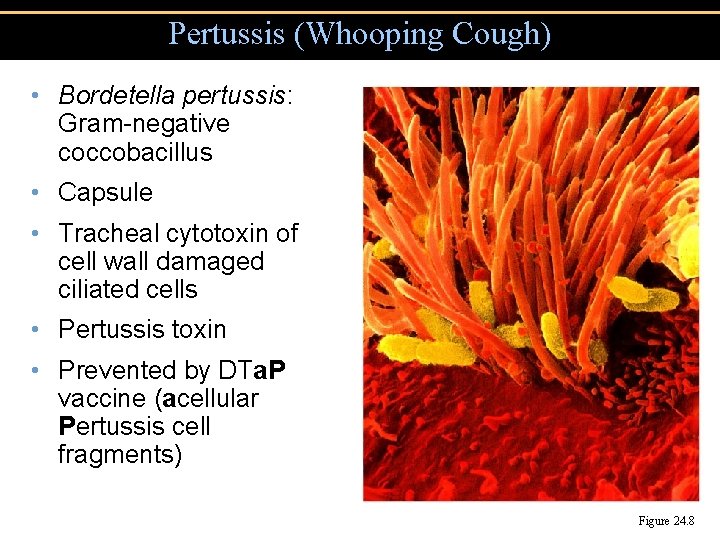
Pertussis (Whooping Cough) • Bordetella pertussis: Gram-negative coccobacillus • Capsule • Tracheal cytotoxin of cell wall damaged ciliated cells • Pertussis toxin • Prevented by DTa. P vaccine (acellular Pertussis cell fragments) Figure 24. 8
Pertussis (Whooping Cough) • Stage 1: Catarrhal stage, like common cold • Stage 2: Paroxysmal stage: Violent coughing sieges • Stage 3: Convalescence stage
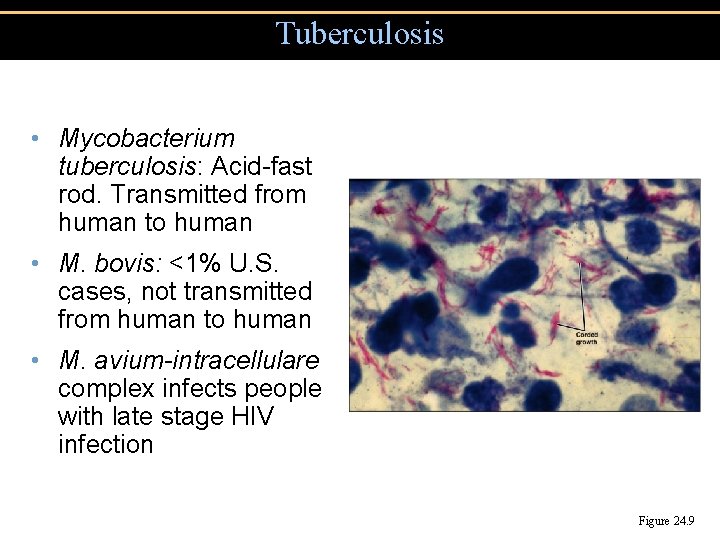
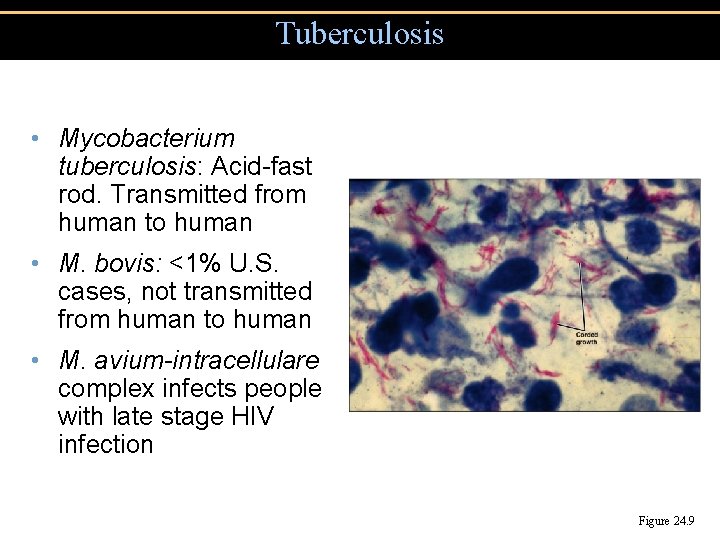
Tuberculosis • Mycobacterium tuberculosis: Acid-fast rod. Transmitted from human to human • M. bovis: <1% U. S. cases, not transmitted from human to human • M. avium-intracellulare complex infects people with late stage HIV infection Figure 24. 9
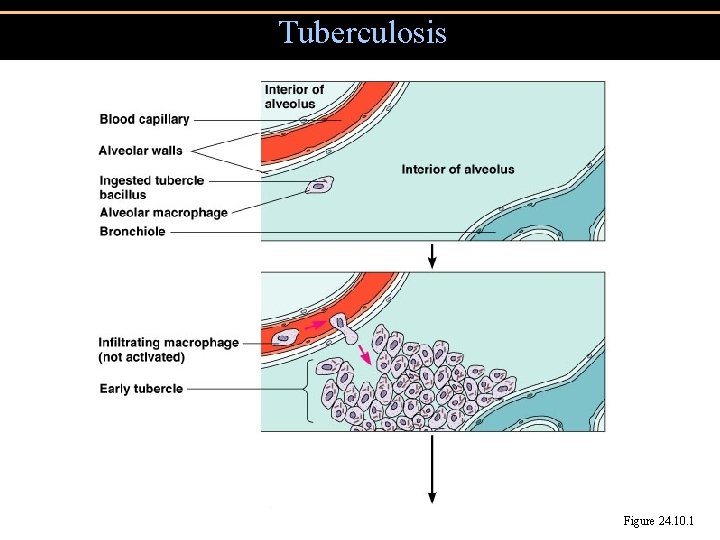
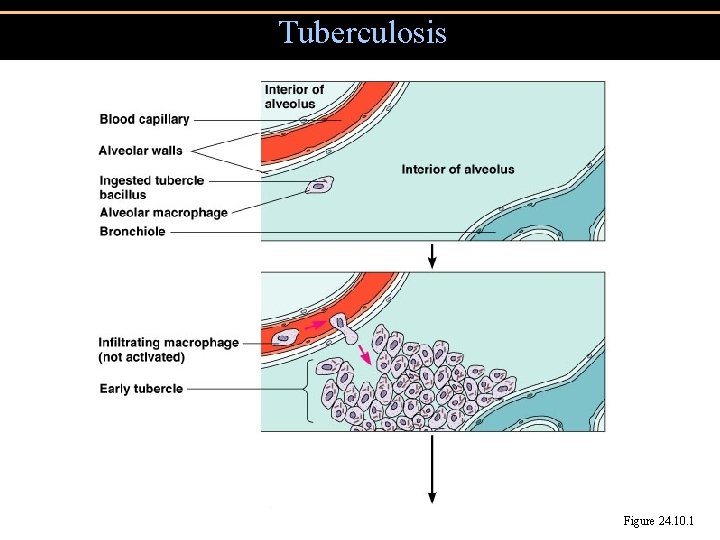
Tuberculosis Figure 24. 10. 1
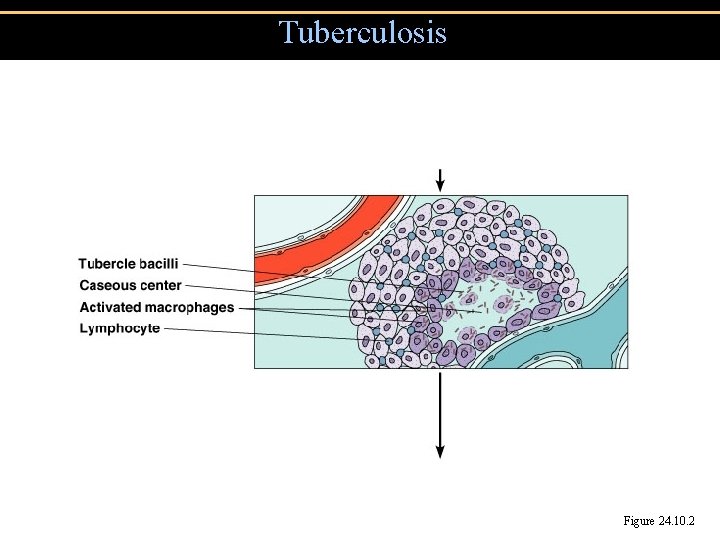
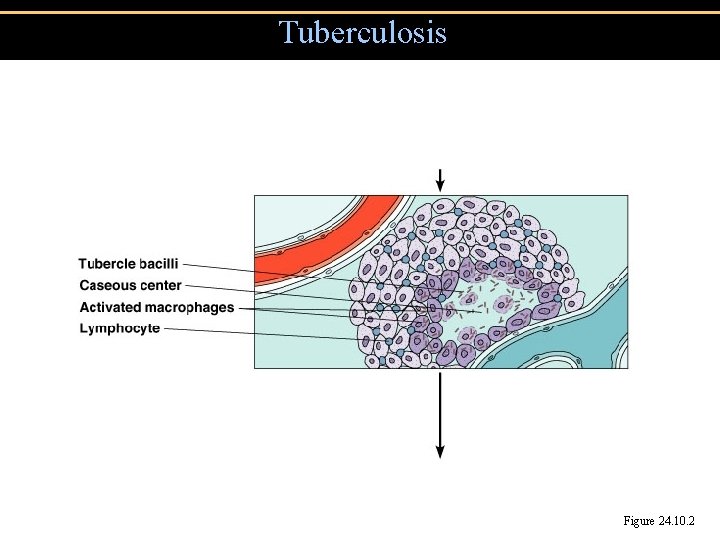
Tuberculosis Figure 24. 10. 2
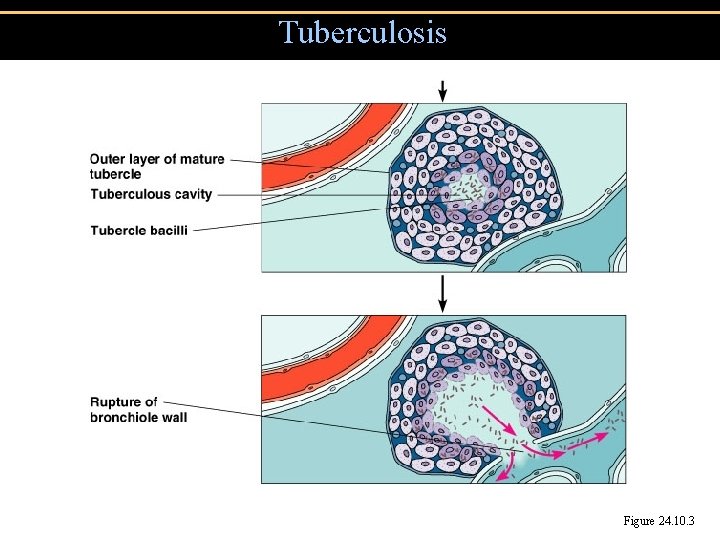
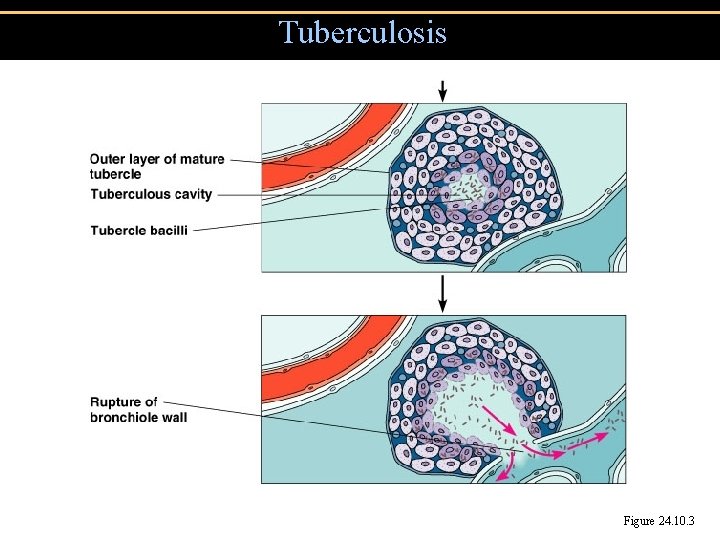
Tuberculosis Figure 24. 10. 3
Tuberculosis • Treatment of Tuberculosis: Prolonged treatment with multiple antibiotics • Vaccines: BCG, live, avirulent M. bovis. Not widely used in U. S.
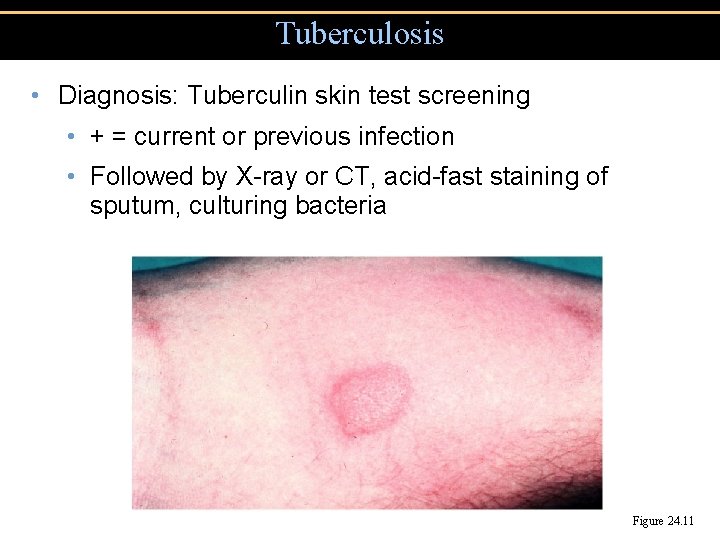
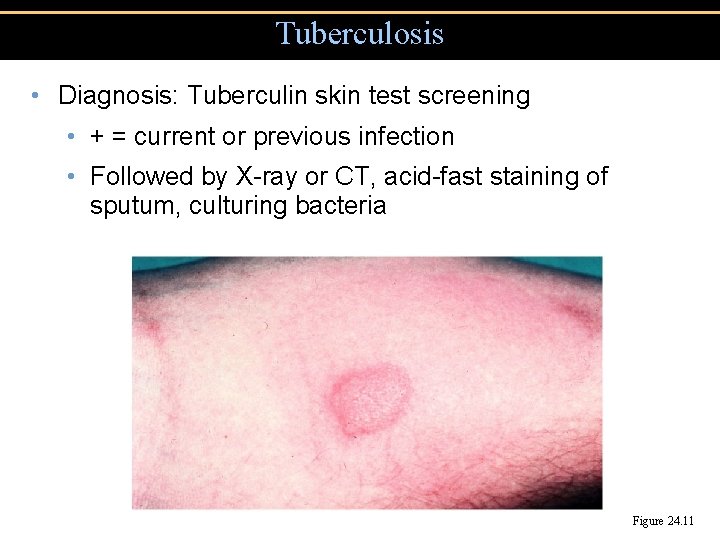
Tuberculosis • Diagnosis: Tuberculin skin test screening • + = current or previous infection • Followed by X-ray or CT, acid-fast staining of sputum, culturing bacteria Figure 24. 11
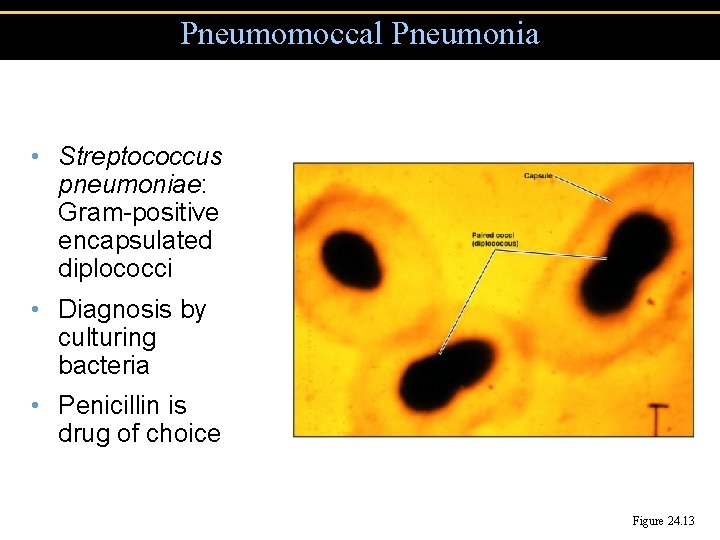
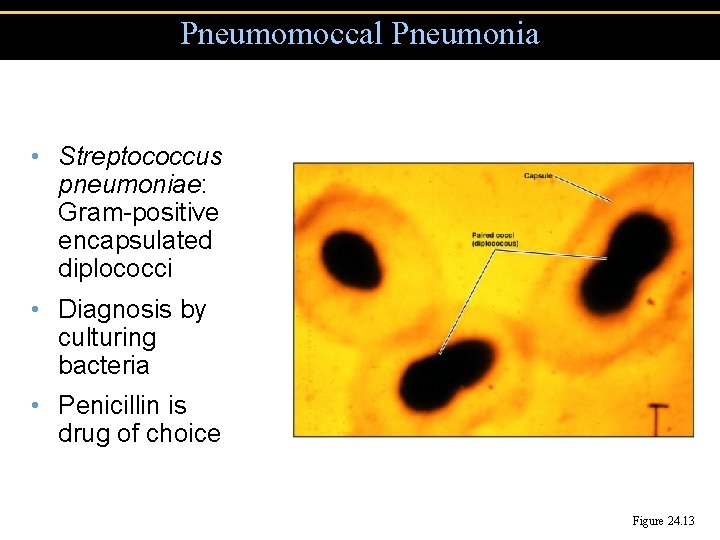
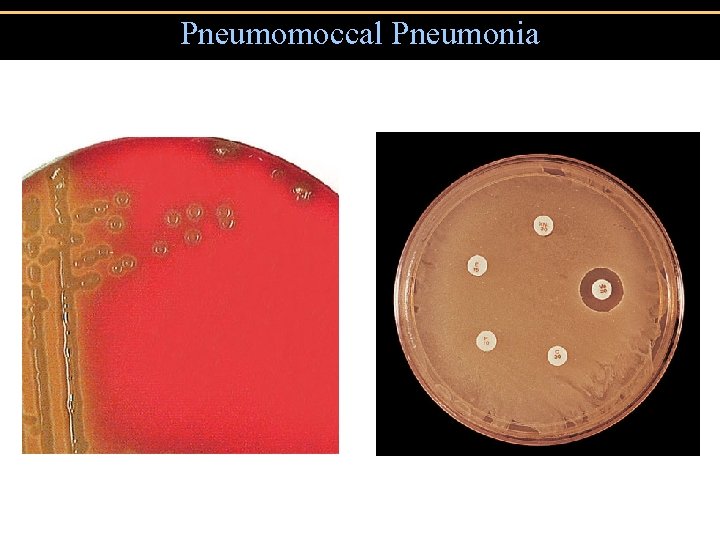
Pneumomoccal Pneumonia • Streptococcus pneumoniae: Gram-positive encapsulated diplococci • Diagnosis by culturing bacteria • Penicillin is drug of choice Figure 24. 13
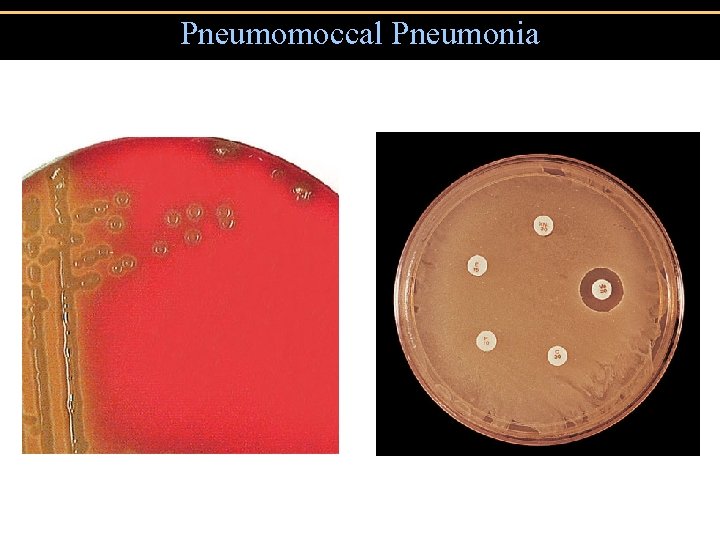
Pneumomoccal Pneumonia
Haemophilus influenzae Pneumonia • Gram-negative coccobacillus • Alcoholism, poor nutrition, cancer, or diabetes are predisposing factors • Second-generation cephalosporins
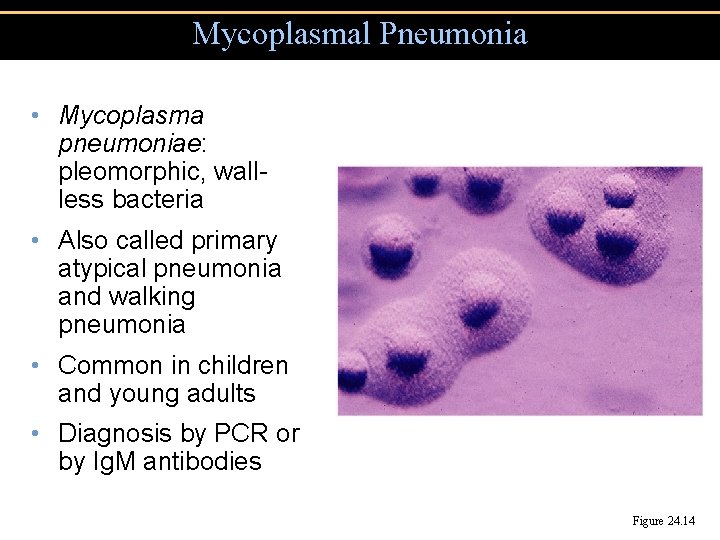
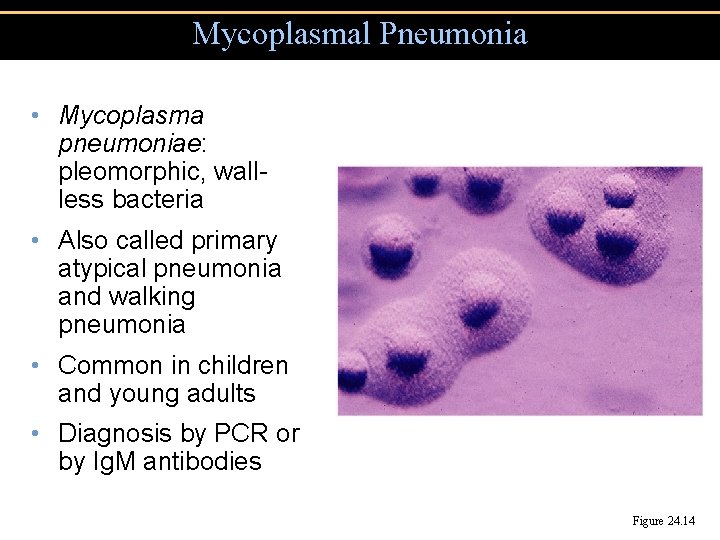
Mycoplasmal Pneumonia • Mycoplasma pneumoniae: pleomorphic, wallless bacteria • Also called primary atypical pneumonia and walking pneumonia • Common in children and young adults • Diagnosis by PCR or by Ig. M antibodies Figure 24. 14
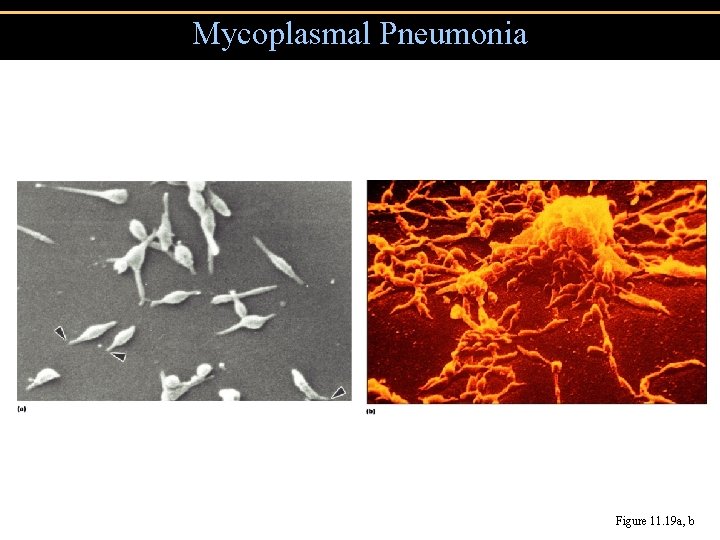
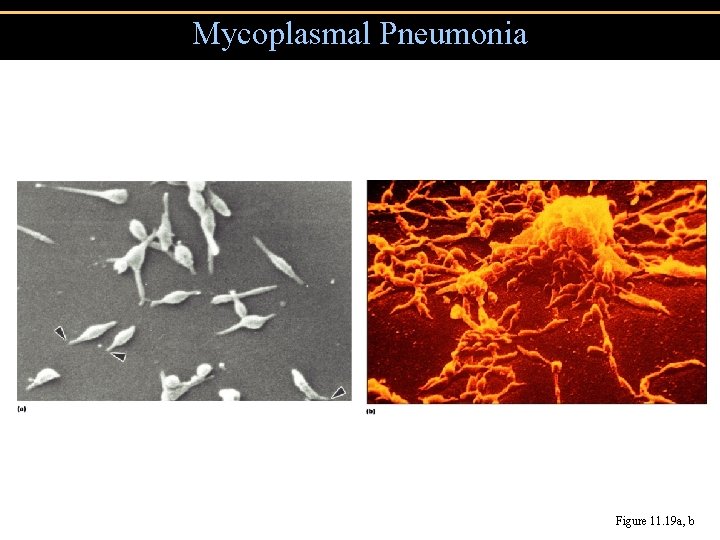
Mycoplasmal Pneumonia Figure 11. 19 a, b
Legionellosis • Legionella pneumophila: Gram-negative rod • L. pneumophila is found in water • Transmitted by inhaling aerosols, not transmitted from human to human • Diagnosis: culturing bacteria • Treatment: Erythromycin
Psittacosis (Ornithosis) • Chlamydia psittaci: gram-negative intracellular bacterium • Transmitted by elementary bodies from bird dropping to humans • Reorganizes into reticulate body after being phagocytized • Diagnosis: culturing bacteria in eggs or cell culture • Treatment: Tetracycline
Chlamydial Pneumonia • Chlamydia pneumoniae • Transmitted from human to human • Diagnosis by FA test • Treatment: Tetracycline
Mycoplasmal pneumonia • Mycoplasma pneumoniae: pleomorphic, wall-less bacteria • Also called primary atypical pneumonia and walking pneumonia • Common in children and young adults • Diagnosis by PCR or by Ig. M antibodies
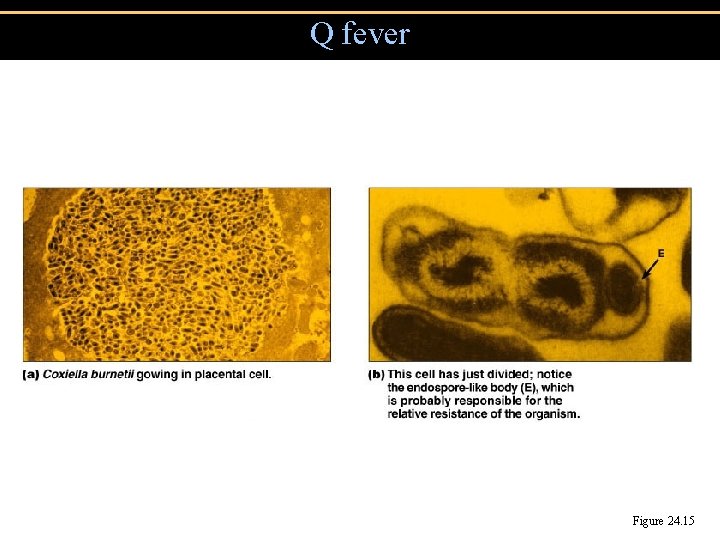
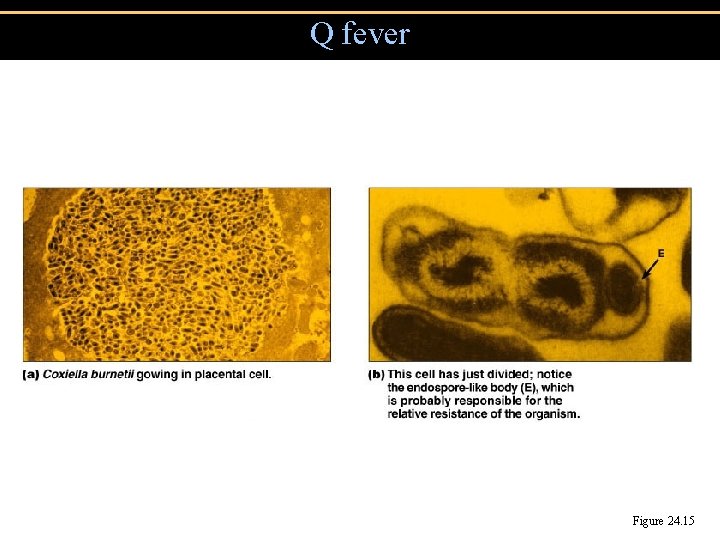
Q fever Figure 24. 15
Viral Pneumonia • Viral pneumonia as a complication of influenza, measles, chickenpox • Viral etiology suspected if no cause determined • Respiratory Syncytial Virus (RSV) • Common in infants; 4500 deaths annually • Causes cell fusion (syncytium) in cell culture • Symptoms: coughing • Diagnosis by serologic test for viruses and antibodies • Treatment: Ribavirin
Influenza • Chills, fever, headache, muscle aches (no intestinal symptoms) • 1% mortality due to secondary bacterial infections • Treatment: Amantadine • Vaccine for high-risk individuals
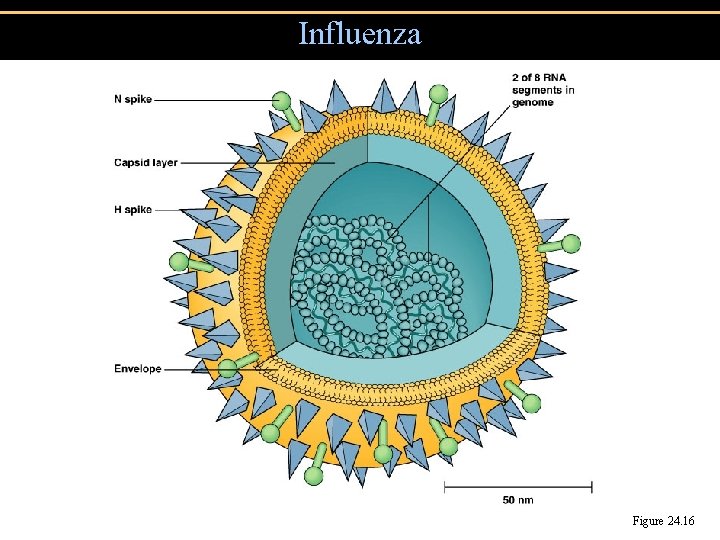
Influenza • Hemagglutinin (H) spikes used for attachment to host cells • Neuraminidase (N) spikes used to release virus from cell
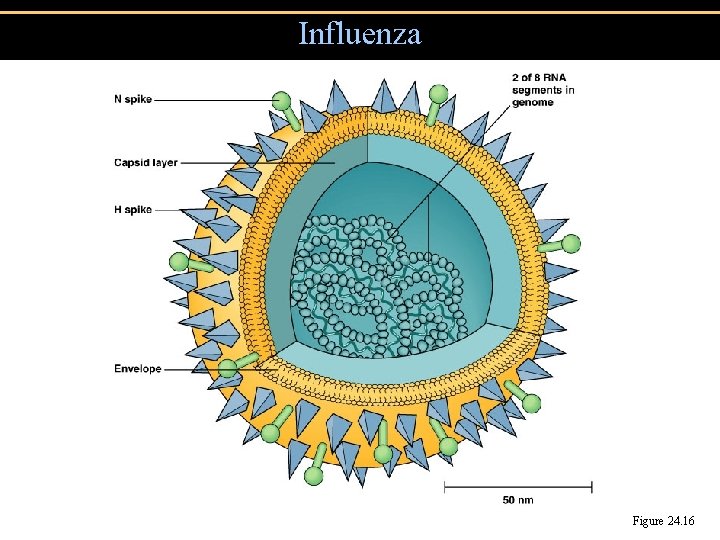
Influenza Figure 24. 16
Influenza • Antigenic shift • Changes in H and N spikes • Probably due to genetic recombination between different strains infecting the same cell • Antigenic drift • Mutations in genes encoding H or N spikes • May involve only 1 amino acid • Allows virus to avoid mucosal Ig. A antibodies
Influenza serotypes • A: causes most epidemics, H 3 N 2, H 1 N 1, H 2 N 2 • B: moderate, local outbreaks • C: mild disease
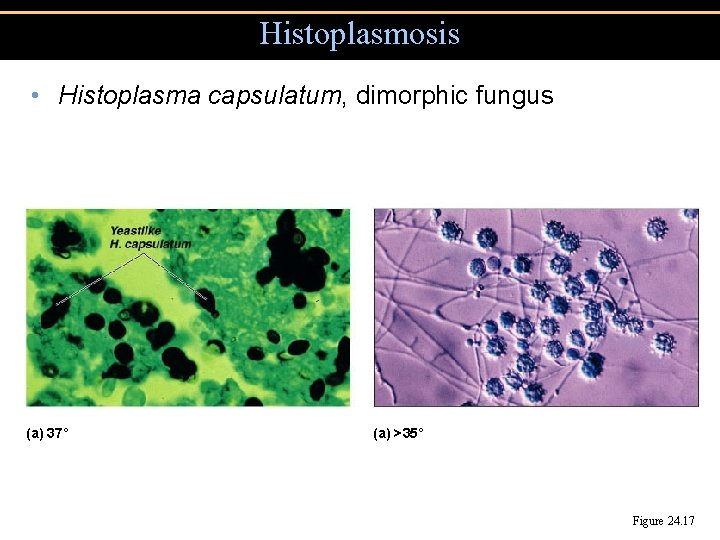
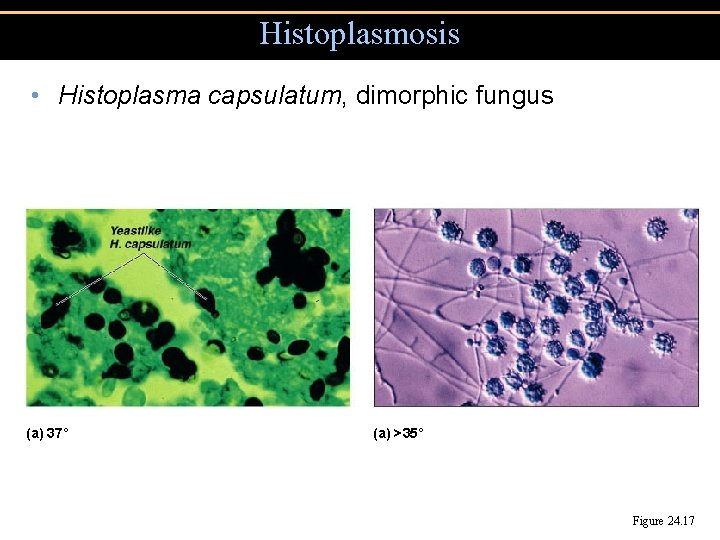
Histoplasmosis • Histoplasma capsulatum, dimorphic fungus (a) 37˚ (a) >35˚ Figure 24. 17
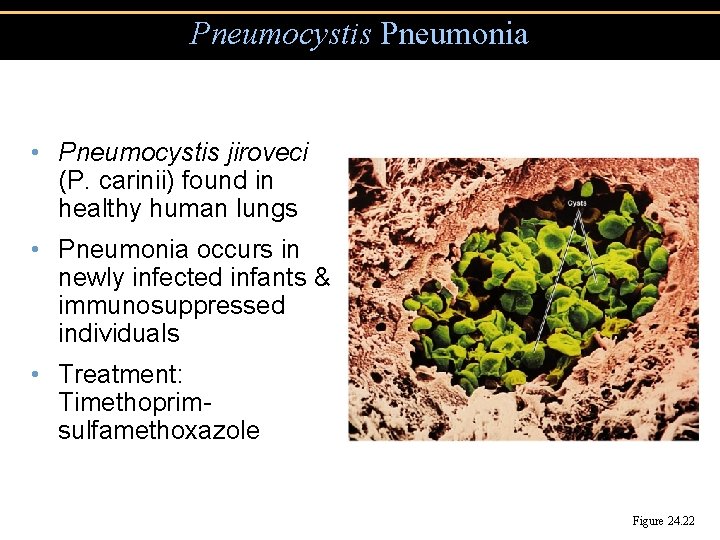
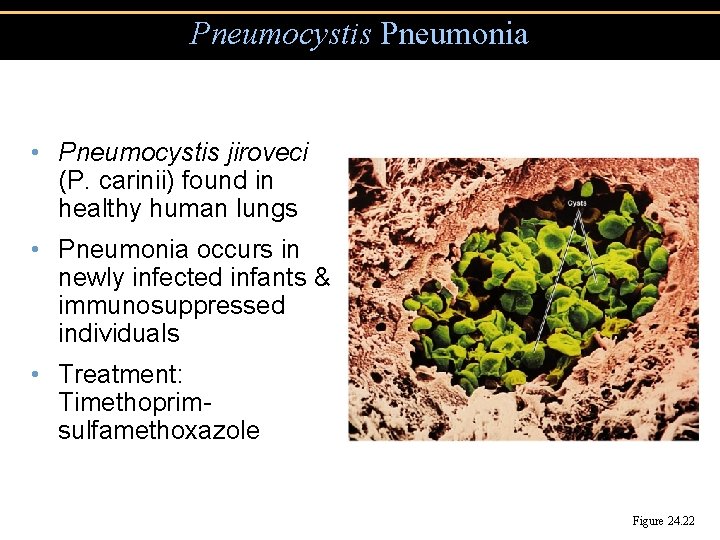
Pneumocystis Pneumonia • Pneumocystis jiroveci (P. carinii) found in healthy human lungs • Pneumonia occurs in newly infected infants & immunosuppressed individuals • Treatment: Timethoprimsulfamethoxazole Figure 24. 22
Blastomycosis • Blastomyces dermatitidis, dimorphic fungus • Found in soil • Can cause extensive tissue destruction • Treatment: amphotericin B
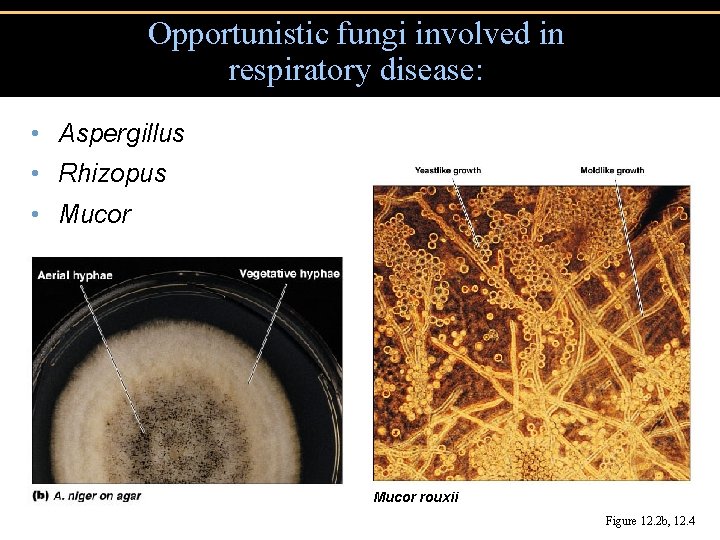
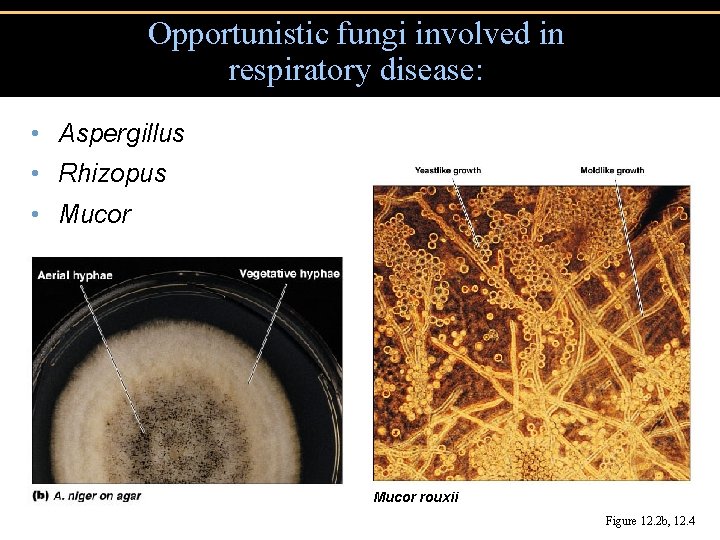
Opportunistic fungi involved in respiratory disease: • Aspergillus • Rhizopus • Mucor rouxii Figure 12. 2 b, 12. 4