PERINATAL MENTAL HEALTH CARE Where is Scotland now








- Slides: 29

PERINATAL MENTAL HEALTH CARE Where is Scotland now? MATERNAL MENTAL HEALTH SCOTLAND CONFERENCE 8 th May 2017 Dr Juliet Brock Medical Officer, Mental Welfare Commission
Overview • About the Commission • Perinatal care in Scotland – Background – Where are we now? MWC perinatal themed visit » Key findings & themes » Key recommendations » Ongoing work • Ms OP report – Alison Thomson, Executive Director (Nursing)

Mental Welfare Commission “ We protect and promote the human rights of people with mental health problems, learning disabilities, dementia and related conditions” We do this by: • Visiting people • Monitoring use of the Acts • Investigations • Providing information, advice and guidance • Influencing and challenging

Perinatal mental health care in Scotland The past
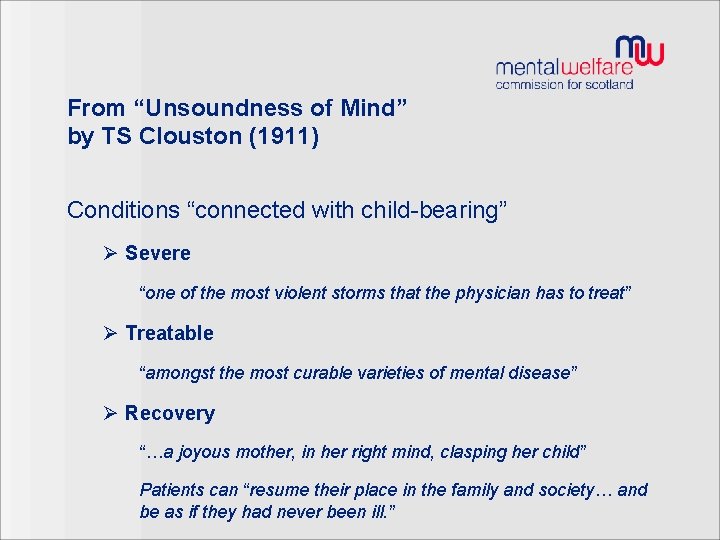
From “Unsoundness of Mind” by TS Clouston (1911) Conditions “connected with child-bearing” Ø Severe “one of the most violent storms that the physician has to treat” Ø Treatable “amongst the most curable varieties of mental disease” Ø Recovery “…a joyous mother, in her right mind, clasping her child” Patients can “resume their place in the family and society… and be as if they had never been ill. ”
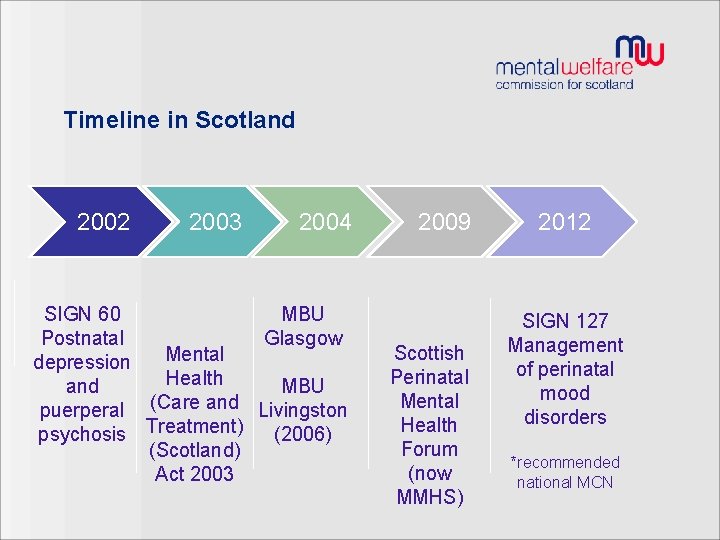
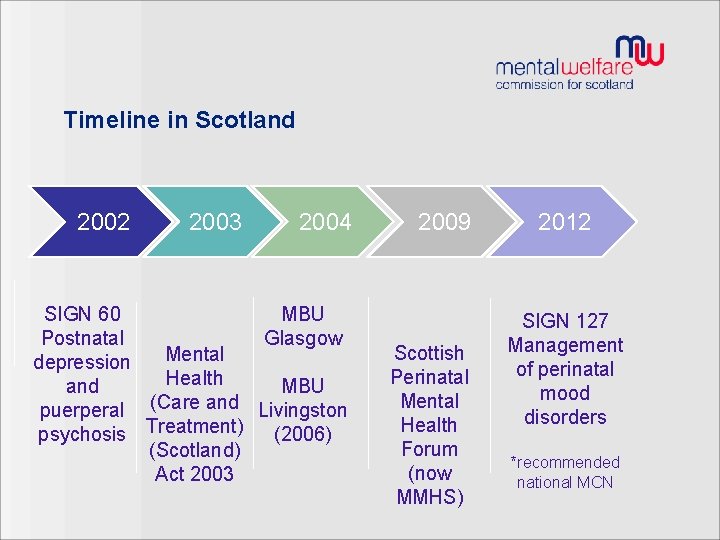
Timeline in Scotland 2002 2003 2004 SIGN 60 MBU Postnatal Glasgow Mental depression Health and MBU puerperal (Care and Livingston psychosis Treatment) (2006) (Scotland) Act 2003 2009 Scottish Perinatal Mental Health Forum (now MMHS) 2012 SIGN 127 Management of perinatal mood disorders *recommended national MCN
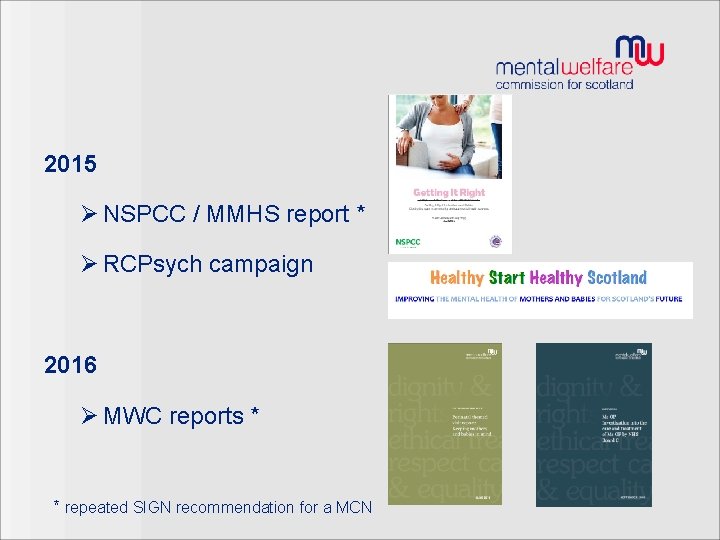
2015 Ø NSPCC / MMHS report * Ø RCPsych campaign 2016 Ø MWC reports * * repeated SIGN recommendation for a MCN
Perinatal mental health care in Scotland The present
Perinatal themed visit
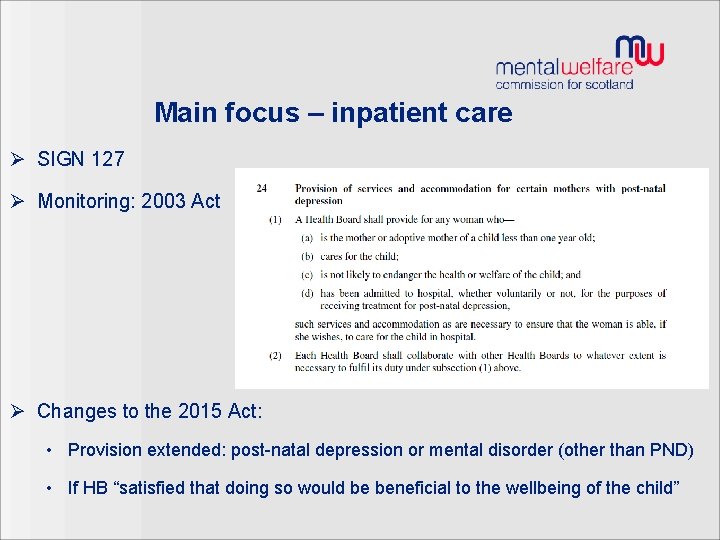
Main focus – inpatient care Ø SIGN 127 Ø Monitoring: 2003 Act Ø Changes to the 2015 Act: • Provision extended: post-natal depression or mental disorder (other than PND) • If HB “satisfied that doing so would be beneficial to the wellbeing of the child”

What we did 1. Inpatient survey 2. Visits and interviews 3. Health Board questionnaire 4. Online consultant survey
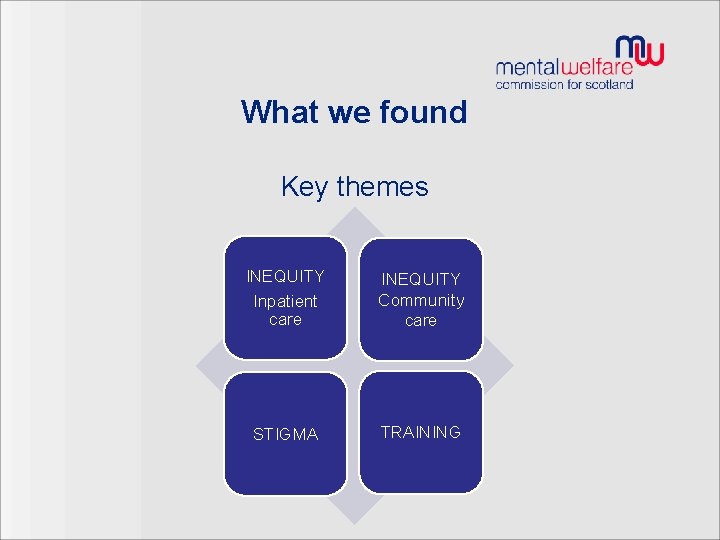
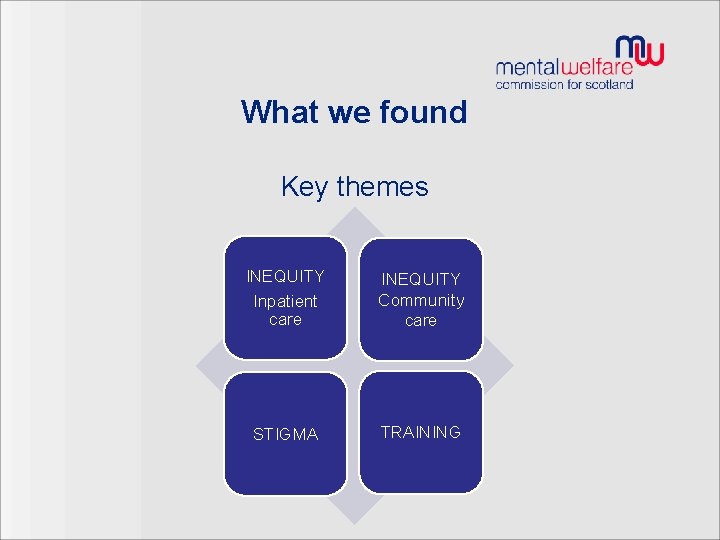
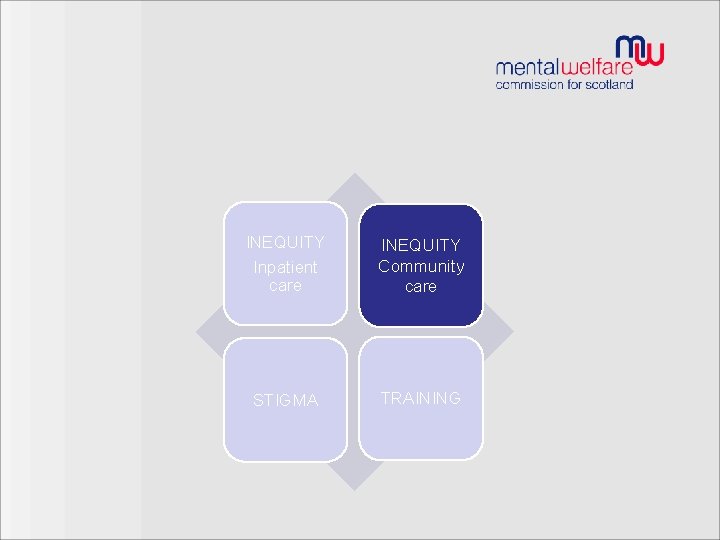
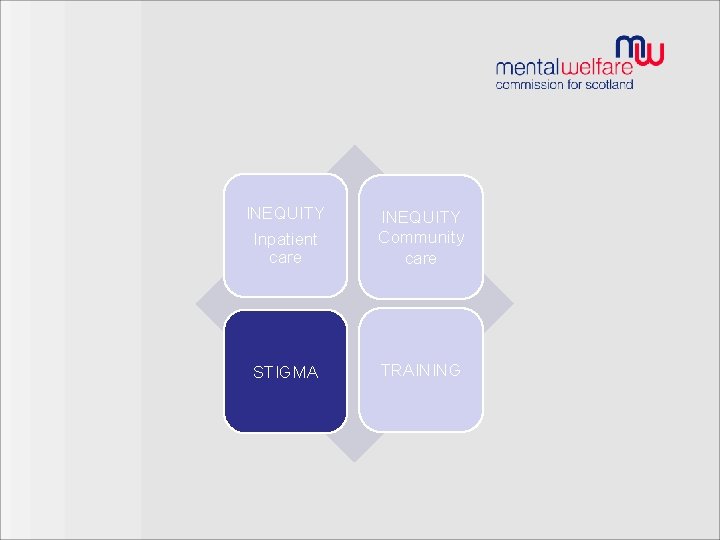
What we found Key themes INEQUITY Inpatient care INEQUITY Community care STIGMA TRAINING
INEQUITY Inpatient care INEQUITY Community care STIGMA TRAINING
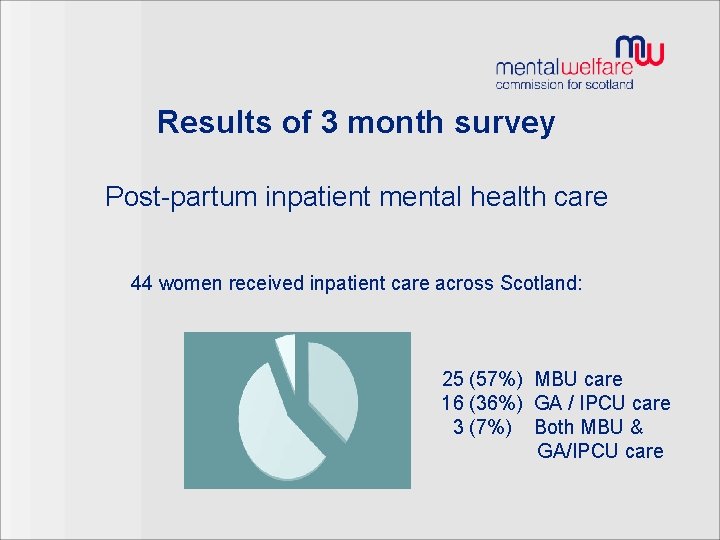
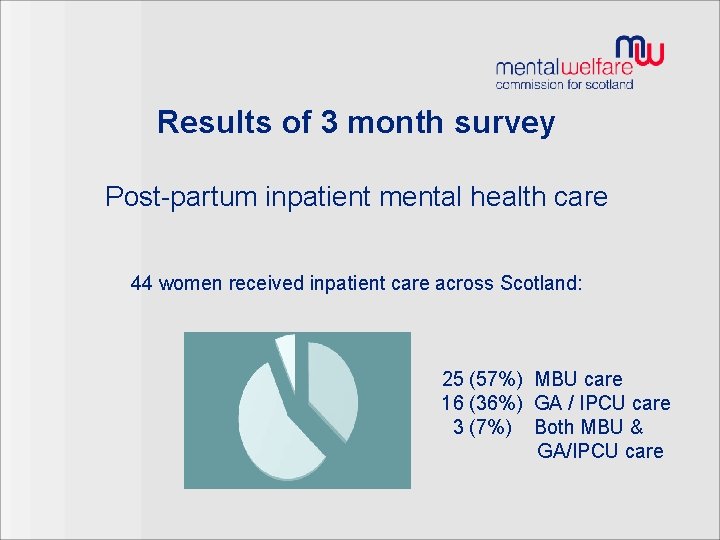
Results of 3 month survey Post-partum inpatient mental health care 44 women received inpatient care across Scotland: 25 (57%) MBU care 16 (36%) GA / IPCU care 3 (7%) Both MBU & GA/IPCU care
Why were women not being admitted to MBUs? – Distance & family commitments – Patient preference – Staff awareness and knowledge of MBUs – Woman not main carer for baby
Inequity in inpatient care: What women told us: • Contrasting experiences: MBU vs GA care* Ø Contact with baby Ø Staff: specialist knowledge & installation of hope Ø Role of peer support Ø Family participation / inclusion *exception GA wards with ‘perinatal’ focus
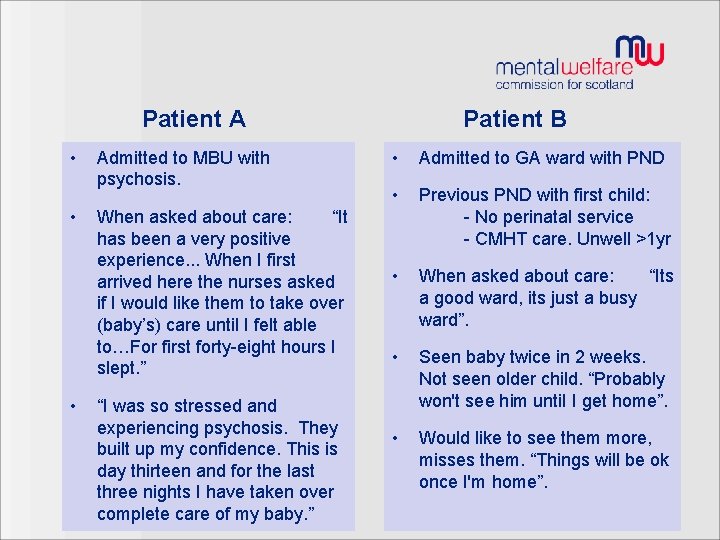
Patient A • • • Admitted to MBU with psychosis. When asked about care: “It has been a very positive experience. . . When I first arrived here the nurses asked if I would like them to take over (baby’s) care until I felt able to…For first forty-eight hours I slept. ” “I was so stressed and experiencing psychosis. They built up my confidence. This is day thirteen and for the last three nights I have taken over complete care of my baby. ” Patient B • Admitted to GA ward with PND • Previous PND with first child: - No perinatal service - CMHT care. Unwell >1 yr • When asked about care: “Its a good ward, its just a busy ward”. • Seen baby twice in 2 weeks. Not seen older child. “Probably won't see him until I get home”. • Would like to see them more, misses them. “Things will be ok once I'm home”.

What we found: Differences MBU vs GA care Ø Focus on mother-infant relationship Ø Specialist MDT care (n. nurses, psychology, SW) Ø Risk management Ø Carer participation & family-friendly visiting Large regional variations in MBU use (data 2012 -15)
Carer views • Importance of: – Information – Carer support – Involvement – Experienced and knowledgeable staff – Community support + perinatal expertise
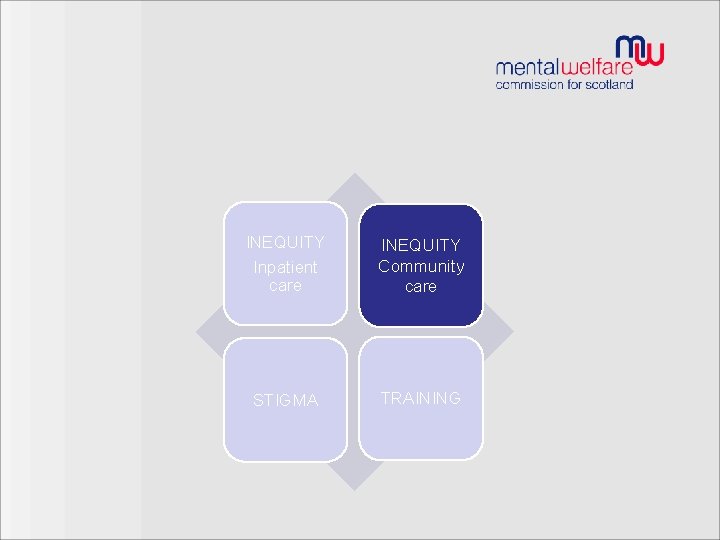
INEQUITY Inpatient care INEQUITY Community care STIGMA TRAINING
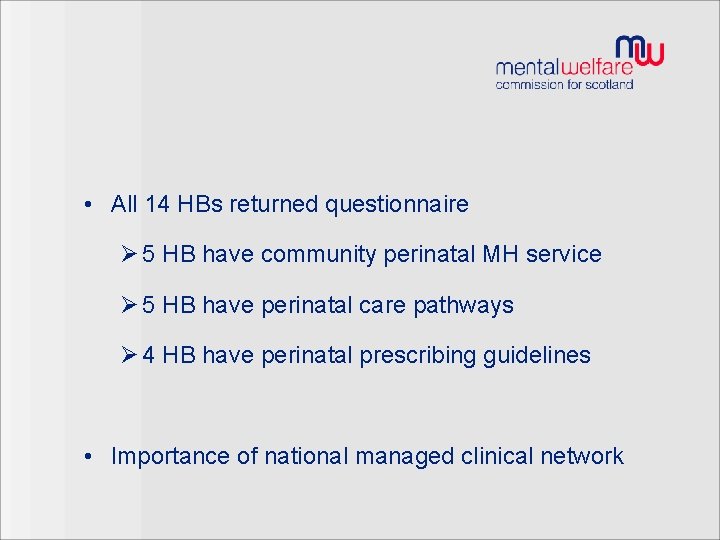
• All 14 HBs returned questionnaire Ø 5 HB have community perinatal MH service Ø 5 HB have perinatal care pathways Ø 4 HB have perinatal prescribing guidelines • Importance of national managed clinical network
INEQUITY Inpatient care INEQUITY Community care STIGMA TRAINING
Experiences of community care - seeking help Stigma and fears about seeking help: “I didn’t tell anyone. I felt too ashamed” “I was very worried (my baby) would be taken off me” Feeling supported in seeking help: “As soon as I realised I was unwell, I went to my GP because I wanted to continue to look after my baby”
INEQUITY Inpatient care INEQUITY Community care STIGMA TRAINING
Experiences of community care - receiving help • Primary care: – Most women received timely support from GP or HV – Mixed experiences • Community mental health care: - Some concerns re: lack of perinatal expertise and management of risk • Need for better education & training

KEY RECOMMENDATIONS • For Scottish Government to establish a MCN • Health boards Ø Duties re MBU admission Ø Link-workers Ø Specialist community provision Ø Training
Ongoing work • Follow-up on recommendations – 11 of 14 HB responses – Ongoing reviewing of progress • Sharing information with MCN

Ms OP report September 2016 Alison Thomson, Executive Director (Nursing)

Thank you Contacts: juliet. brock@mwcscot. org. uk alison. thomson@mwcscot. org. uk MWC: 0131 313 8777
 Dad mental health scotland
Dad mental health scotland Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Jeopardy mental health
Jeopardy mental health Enhanced primary care mental health
Enhanced primary care mental health Beacon mental health la care
Beacon mental health la care Primary secondary tertiary care
Primary secondary tertiary care Health and social care values unit 2
Health and social care values unit 2 Now i see it now you don't
Now i see it now you don't Sexual health and relationships education scotland
Sexual health and relationships education scotland Clear perinatal quality
Clear perinatal quality Perinatal matrices grof
Perinatal matrices grof Perinatal mortality rate
Perinatal mortality rate Classification of birth asphyxia
Classification of birth asphyxia Neonatarum
Neonatarum Perinatal audit
Perinatal audit Motor gelişimi etkileyen faktörler
Motor gelişimi etkileyen faktörler Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Certain conditions originating in the perinatal period
Certain conditions originating in the perinatal period Ccqi perinatal standards
Ccqi perinatal standards South dakota perinatal association
South dakota perinatal association Standing around crying
Standing around crying Perinatal
Perinatal Ruta materno perinatal
Ruta materno perinatal Waiter's tip deformity
Waiter's tip deformity Hie staging
Hie staging Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing Mental capacity care plan
Mental capacity care plan Peninsula
Peninsula Lenawee community mental health authority
Lenawee community mental health authority Van buren cmh
Van buren cmh