Palliative Care In Heart Failure Dr ChiChi Cheung


- Slides: 17
Palliative Care In Heart Failure Dr Chi-Chi Cheung Consultant in Palliative Medicine 19 th March 2015
Overview • • • When does heart failure become palliative? Heart failure therapies Cardiac devices Pharmacological management Prescribing at the end of life
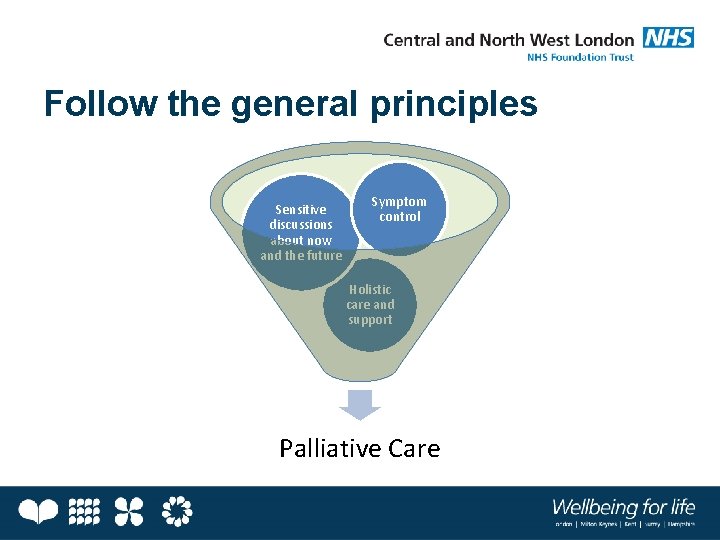
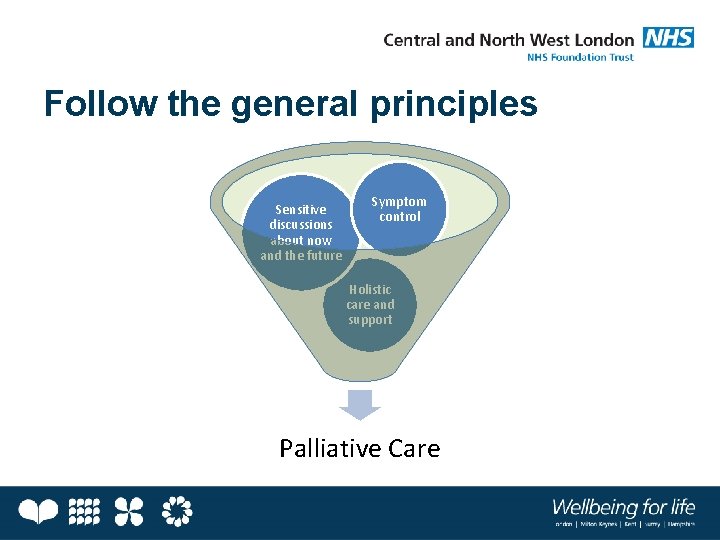
Follow the general principles Sensitive discussions about now and the future Symptom control Holistic care and support Palliative Care
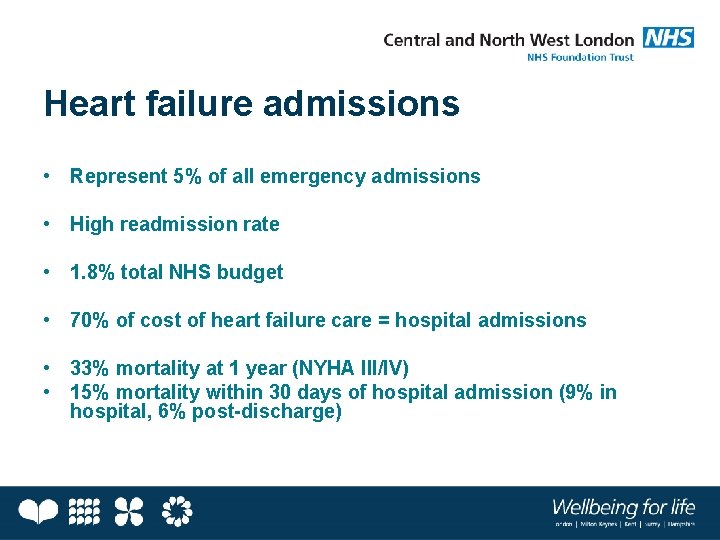
Heart failure admissions • Represent 5% of all emergency admissions • High readmission rate • 1. 8% total NHS budget • 70% of cost of heart failure care = hospital admissions • 33% mortality at 1 year (NYHA III/IV) • 15% mortality within 30 days of hospital admission (9% in hospital, 6% post-discharge)
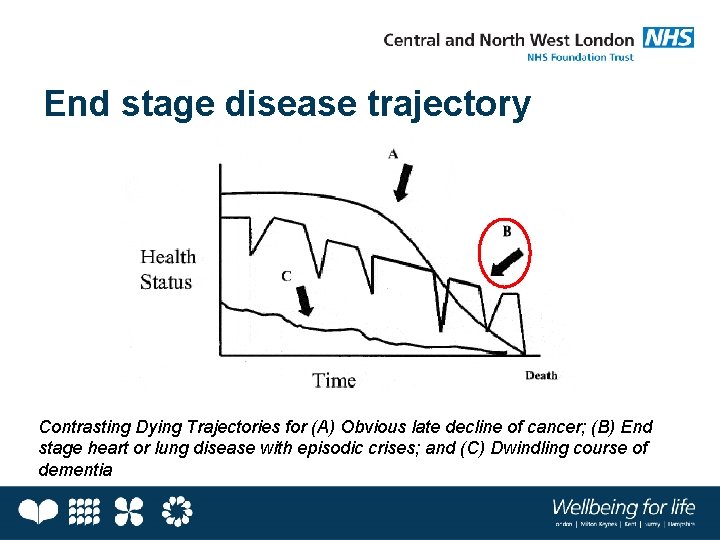
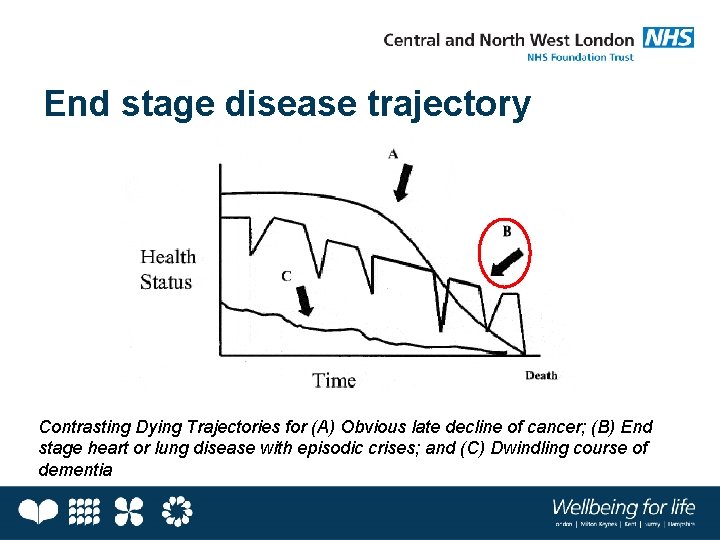
End stage disease trajectory Contrasting Dying Trajectories for (A) Obvious late decline of cancer; (B) End stage heart or lung disease with episodic crises; and (C) Dwindling course of dementia
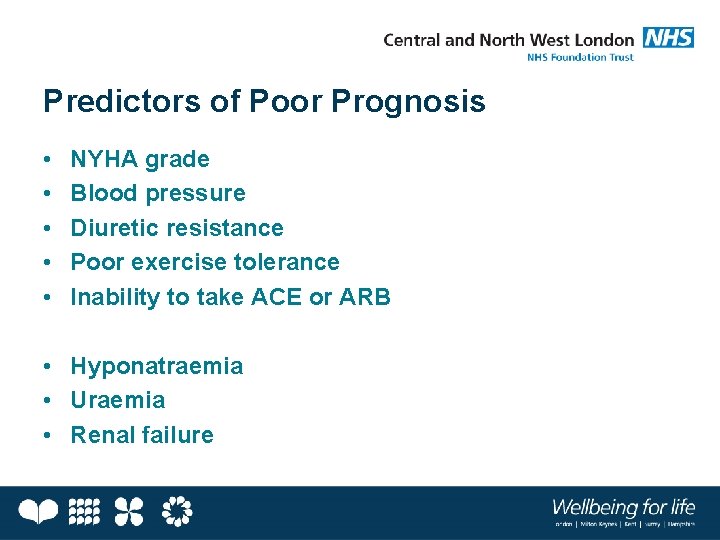
Predictors of Poor Prognosis • • • NYHA grade Blood pressure Diuretic resistance Poor exercise tolerance Inability to take ACE or ARB • Hyponatraemia • Uraemia • Renal failure
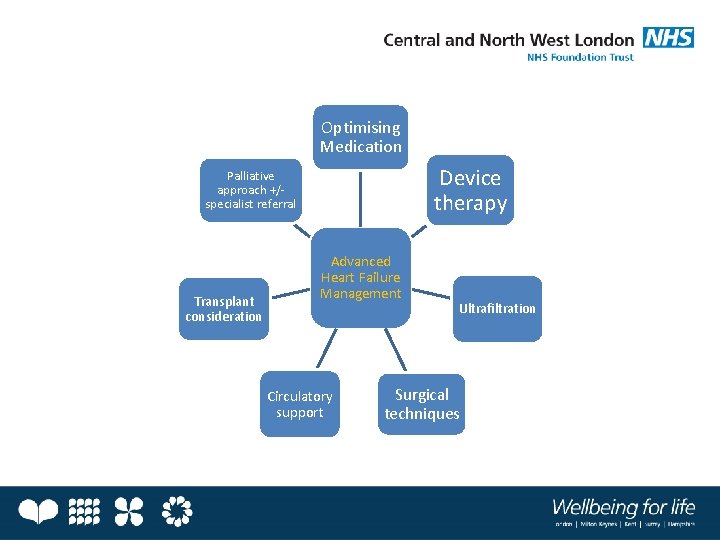
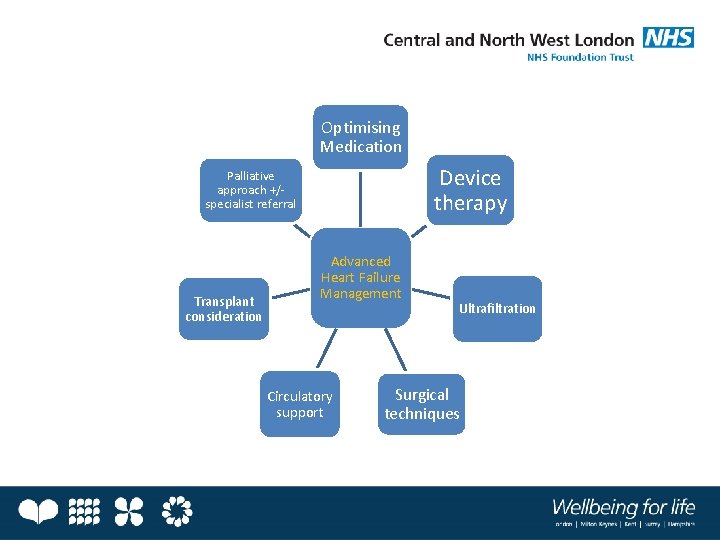
Optimising Medication Device therapy Palliative approach +/specialist referral Transplant consideration Advanced Heart Failure Management Circulatory support Ultrafiltration Surgical techniques
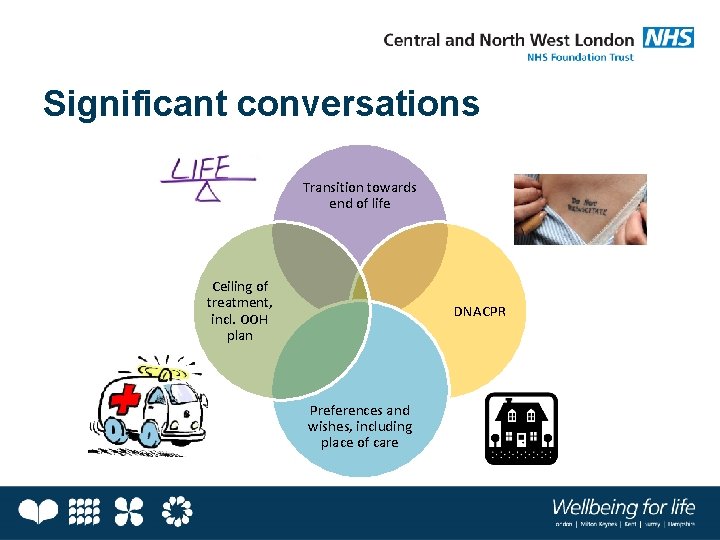
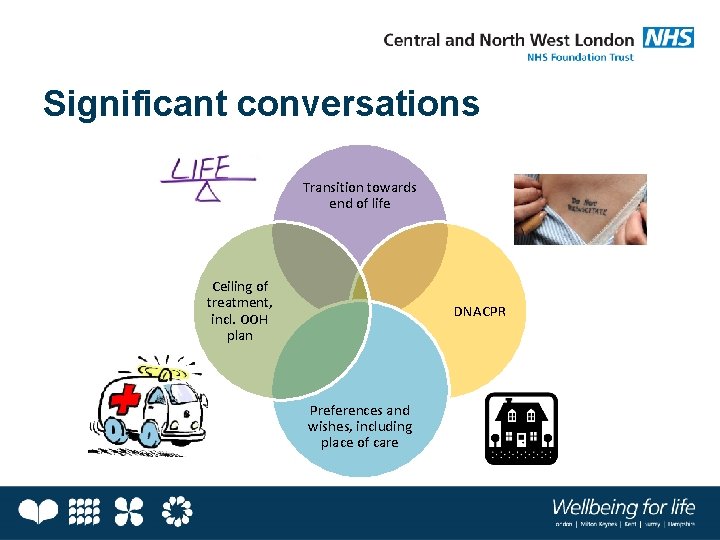
Significant conversations Transition towards end of life Ceiling of treatment, incl. OOH plan DNACPR Preferences and wishes, including place of care

Cardiac Device Therapy ICD CRT-P (implantable cardiac defibrillator) (P=pacemaker) CRT-D (D=defibrillator) CRT = cardiac resynchronisation therapy
Deactivating ICD/CRT-D devices
But…
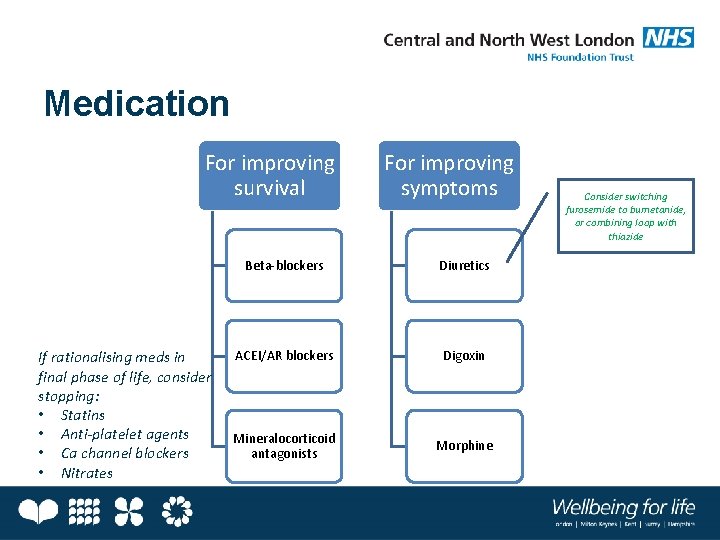
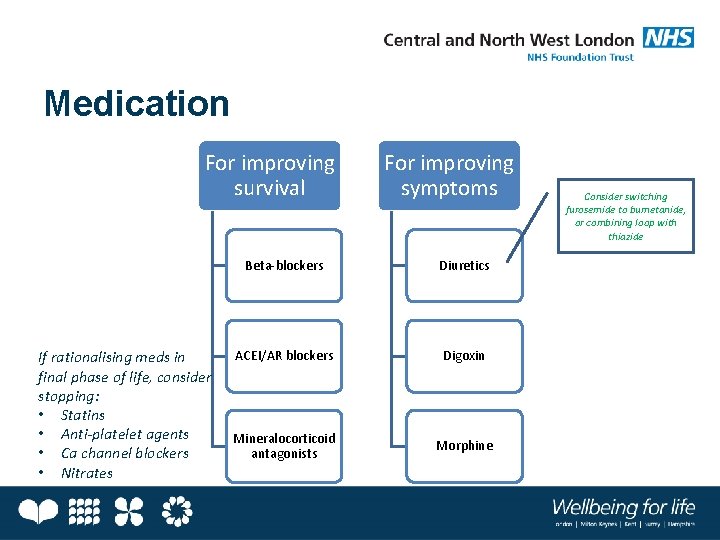
Medication For improving survival If rationalising meds in final phase of life, consider stopping: • Statins • Anti-platelet agents • Ca channel blockers • Nitrates For improving symptoms Beta-blockers Diuretics ACEI/AR blockers Digoxin Mineralocorticoid antagonists Morphine Consider switching furosemide to bumetanide, or combining loop with thiazide
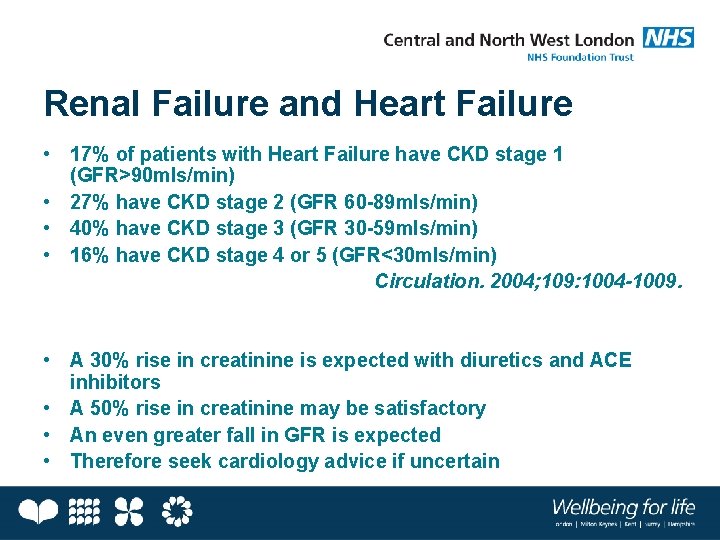
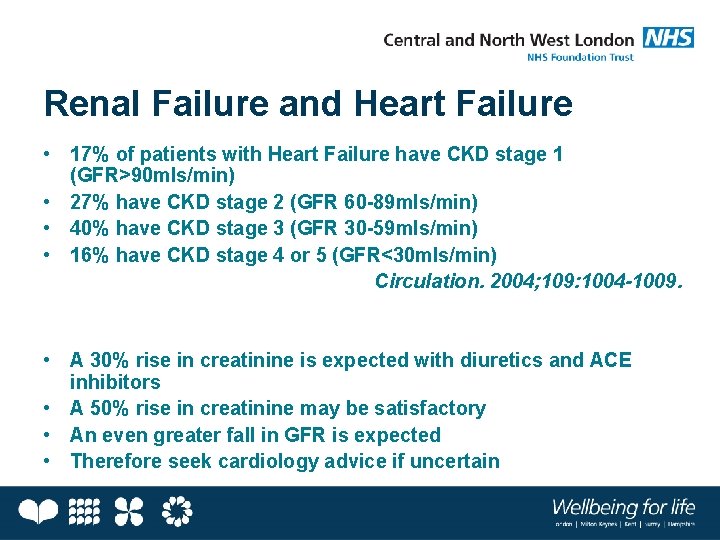
Renal Failure and Heart Failure • 17% of patients with Heart Failure have CKD stage 1 (GFR>90 mls/min) • 27% have CKD stage 2 (GFR 60 -89 mls/min) • 40% have CKD stage 3 (GFR 30 -59 mls/min) • 16% have CKD stage 4 or 5 (GFR<30 mls/min) Circulation. 2004; 109: 1004 -1009. • A 30% rise in creatinine is expected with diuretics and ACE inhibitors • A 50% rise in creatinine may be satisfactory • An even greater fall in GFR is expected • Therefore seek cardiology advice if uncertain
Common Symptoms • • • Breathlessness Fatigue Oedema Postural hypotension Pain Poor appetite Depression Poor energy levels Nausea Cough Fear Syncope NB Treat cause where possible
Specific symptoms • Breathlessness: Morphine (reduce dose or frequency in renal impairment, e. g. oramorph 2. 5 mg tds instead of 4 hourly) • Pain: Avoid NSAIDs, pregabalin, TCAs • Nausea/vomiting: Avoid cyclizine • Depression: Avoid TCAs, venlafaxine • Remember non-pharmacological modes of treatment • Remember laxatives with opioids!
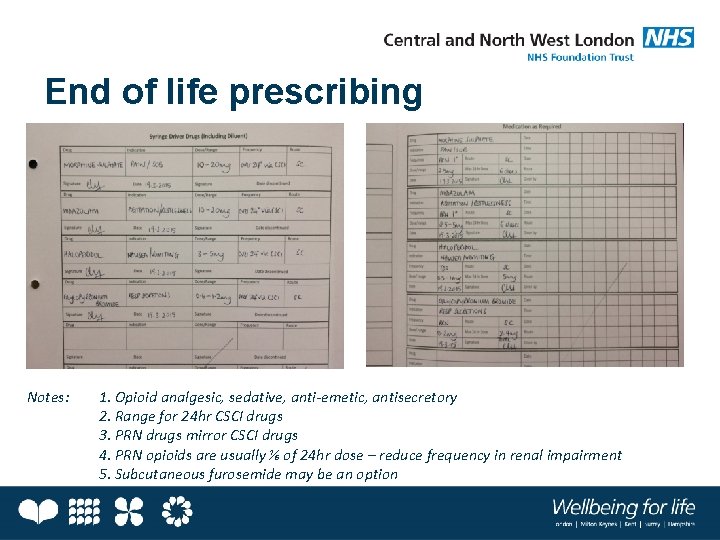
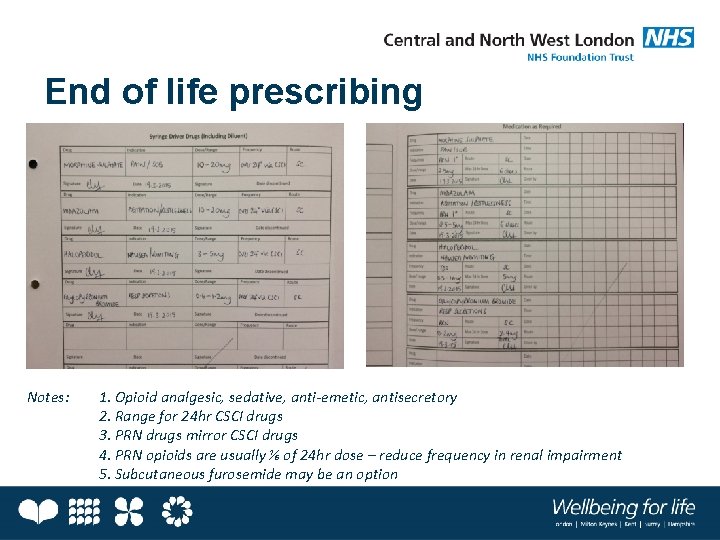
End of life prescribing Notes: 1. Opioid analgesic, sedative, anti-emetic, antisecretory 2. Range for 24 hr CSCI drugs 3. PRN drugs mirror CSCI drugs 4. PRN opioids are usually ⅙ of 24 hr dose – reduce frequency in renal impairment 5. Subcutaneous furosemide may be an option

Take home messages General principles Specific to Heart Failure Optimise medications HF meds may be useful for symptom control Assess symptoms and treat cause where possible Avoid cyclizine, TCAs, venlafaxine, pregabalin where possible Key discussions re transition, future care, preferences etc. Discussions re deactivation of ICD, CRT-D (but not pacemakers or CRT-P)
 Palliative care vs hospice care
Palliative care vs hospice care Chichi takes on nnn
Chichi takes on nnn Failure to capture vs failure to sense ecg
Failure to capture vs failure to sense ecg Vvi pacemaker
Vvi pacemaker Brittle failure vs ductile failure
Brittle failure vs ductile failure Esas-r
Esas-r Akps palliative
Akps palliative Hospice satisfaction survey
Hospice satisfaction survey Principles of palliative care
Principles of palliative care Palliative care in nepal
Palliative care in nepal Palliative care assistant
Palliative care assistant European certificate in palliative care
European certificate in palliative care Parallel planning palliative care
Parallel planning palliative care Franciscan hospice and palliative care
Franciscan hospice and palliative care Integrated palliative care outcome scale
Integrated palliative care outcome scale Problem severity scale
Problem severity scale Pcqc registry
Pcqc registry Antiemetic ladder
Antiemetic ladder