DNACPR update postTracey Dr ChiChi Cheung Consultant in









- Slides: 23
DNACPR update: post-Tracey Dr Chi-Chi Cheung Consultant in Palliative Medicine 19 th March 2015
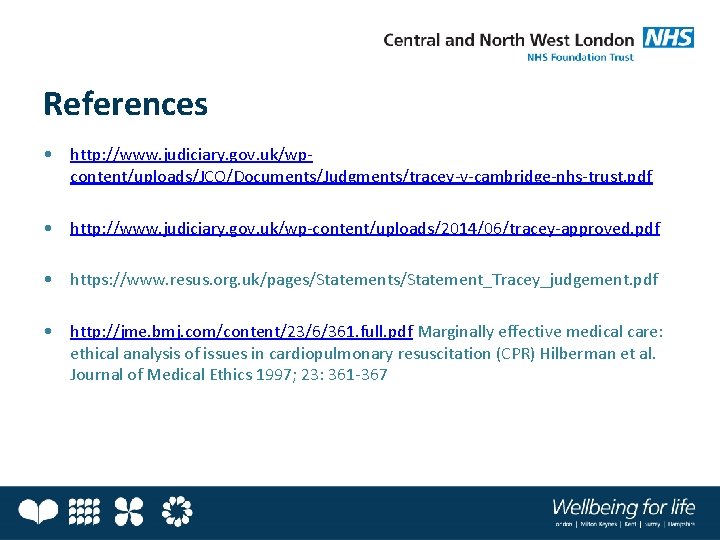
"I wish I'd bundled him up and taken him home because at least if he was going to die, he was going to die with some dignity. "

Overview • • • Background The Tracey case Key points from the Resuscitation Council guidance Best practice in the community Discussion
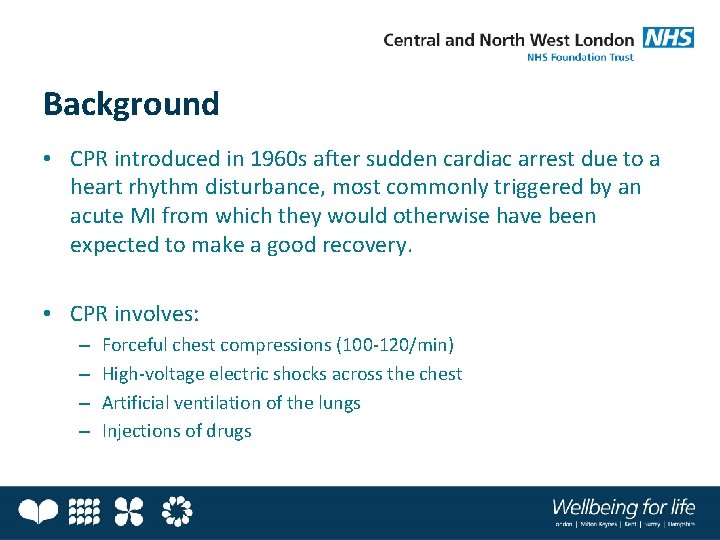
Background • CPR introduced in 1960 s after sudden cardiac arrest due to a heart rhythm disturbance, most commonly triggered by an acute MI from which they would otherwise have been expected to make a good recovery. • CPR involves: – – Forceful chest compressions (100 -120/min) High-voltage electric shocks across the chest Artificial ventilation of the lungs Injections of drugs
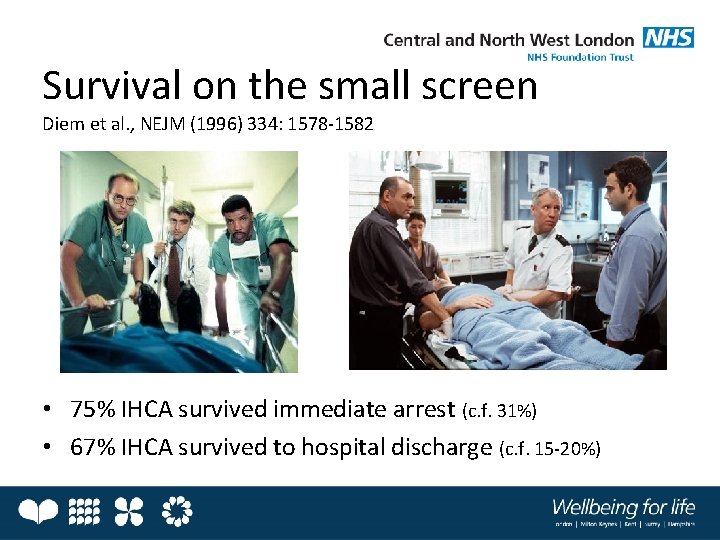
Survival on the small screen Diem et al. , NEJM (1996) 334: 1578 -1582 • 75% IHCA survived immediate arrest (c. f. 31%) • 67% IHCA survived to hospital discharge (c. f. 15 -20%)

Resuscitation Council Guidance • Revised guidance 2007 (Joint Statement) – Compliance with MCA 2005 – MDT working – Practical implementation of the guidance • Revised guidance 2014 (Decisions Relating to CPR) – Post-Tracey case – Emphasis on high quality communication and recording of CPR decisions
The case of Tracey v. Cambridge Hospitals NHS Trust

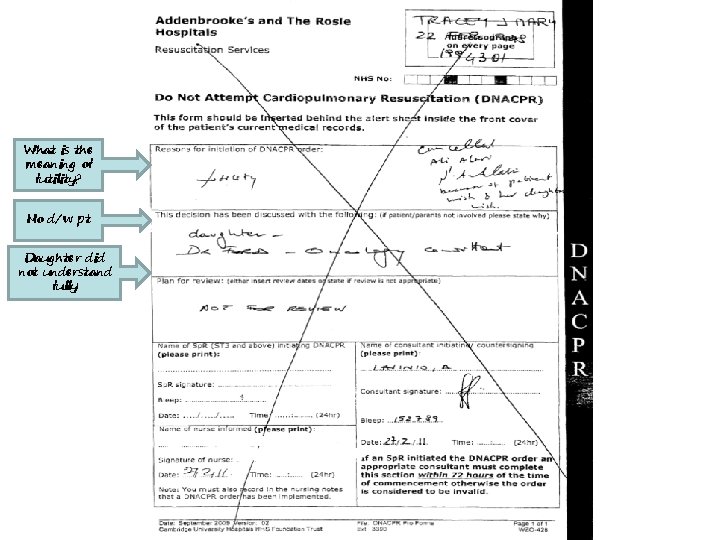
JT case summary • JT admitted to Addenbrooke’s 19 Feb 2011 following an RTA in which she sustained a cervical fracture • Approximately 1 -2 weeks prior to this admission, JT had been diagnosed with terminal lung cancer (prognosis 9/12) • During the admission, JT’s clinical condition in ICU deteriorated • A DNACPR order was made on 27 Feb 2011. Her condition improved and it was cancelled on 2 Mar 2011 at family’s request • A second DNACPR order was made on 5 Mar 2011, in agreement with family, following further deterioration • JT died on 7 Mar 2011
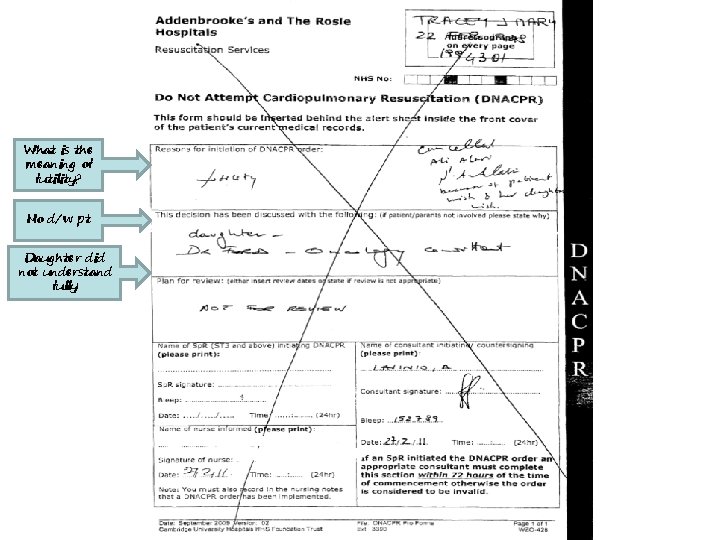
What is the meaning of futility? No d/w pt Daughter did not understand fully


What is this case about? • Lawyers for the Tracey family argued that the imposition of a DNACPR order on a patient with capacity, without first informing them or giving them any opportunity to express their views was a breach under Article 8 of the Human Rights Act, which provides that: “Everyone has the right to respect for their private and family life". • This is about discussing DNACPR decisions with patients who have capacity, with those close to them, and documenting details of the conversation, and sharing with others involved in their care.
Decisions Relating to Cardiopulmonary Resuscitation (2014) Making a decision not to attempt CPR that has no realistic prospect of success does not require the consent of the patient or of those close to the patient. However there is a presumption in favour of informing a patient of such a decision.
Decisions Relating to Cardiopulmonary Resuscitation (2014) Some healthcare professionals do not find it easy to discuss CPR with their patients, but this must not prevent discussion, to involve patients in shared decision-making whenever appropriate, or in some circumstances to inform patients of a decision and explain the reasons for it. There must be a presumption in favour of such patient involvement. Discussion about dying and about CPR must not be avoided to try to spare the patient distress unless there is good reason to believe that such distress will cause them harm.
Decisions Relating to Cardiopulmonary Resuscitation (2014) For many people anticipatory decisions about CPR are best made in the wider context of advance care planning, before a crisis necessitates a hurried decision in an emergency setting.

Decisions Relating to Cardiopulmonary Resuscitation (2014) Triggers for review should include any request from the patient or those close to them, any substantial change in the patient’s clinical condition or prognosis, and transfer of the patient to a different location.

Decisions Relating to Cardiopulmonary Resuscitation (2014) Failure to make timely and appropriate decisions about CPR will leave people at risk of receiving inappropriate or unwanted attempts at CPR as they die. The resulting indignity, with no prospect of benefit, is unacceptable, especially when many would not have wanted CPR had their needs and wishes been explored.
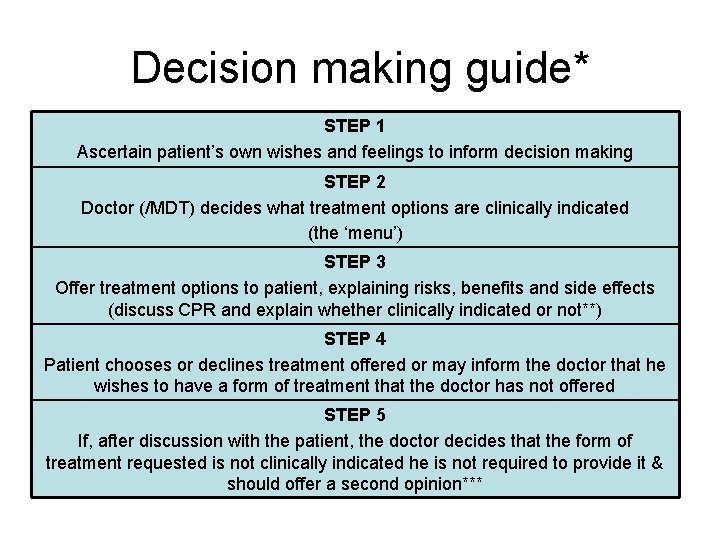
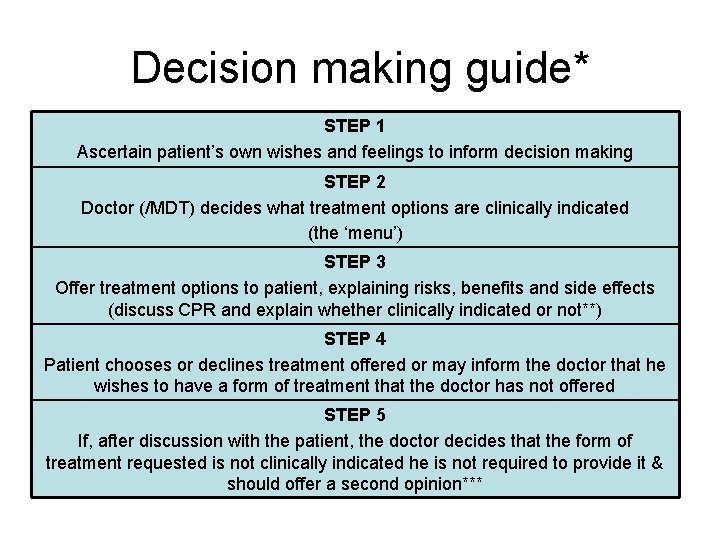
Decision making guide* STEP 1 Ascertain patient’s own wishes and feelings to inform decision making STEP 2 Doctor (/MDT) decides what treatment options are clinically indicated (the ‘menu’) STEP 3 Offer treatment options to patient, explaining risks, benefits and side effects (discuss CPR and explain whether clinically indicated or not**) STEP 4 Patient chooses or declines treatment offered or may inform the doctor that he wishes to have a form of treatment that the doctor has not offered STEP 5 If, after discussion with the patient, the doctor decides that the form of treatment requested is not clinically indicated he is not required to provide it & should offer a second opinion***

* For patients with capacity ** Unless the patient will be distressed by being consulted and that distress might cause the patient harm (eg suicidal ideation, CVA) *** Transfer of the patient’s care to another doctor or team can be considered if there is still a lack of agreement and it is feasible. In exceptional circumstances, where there is ongoing disagreement, it may be necessary to seek legal advice.

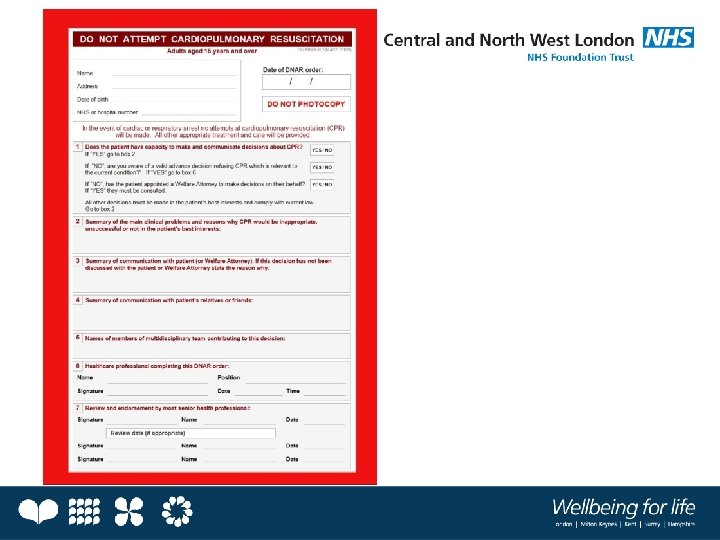
Best practice in the community (1) • Decision-making – Ideally multi-disciplinary decision – GP is usually the most senior clinician in charge of the patient’s care – If palliative care team member completes the form, the decision should be discussed with the GP and subsequently authorised/ countersigned – After hospital discharge the inpatient DNACPR decision no longer applies. Therefore the decision should be reviewed and a new form completed as soon as is practicable.
Best practice in the community (2) • Communication of DNACPR decisions – With the patient (provide information and check understanding) – With those close to the patient (unless confidentiality requested by the patient) – With all those involved in the patient’s care • Electronic: CMC including DNACPR form • Paper: Resus council model form in the patient’s home • Specific communication with acute trusts where relevant
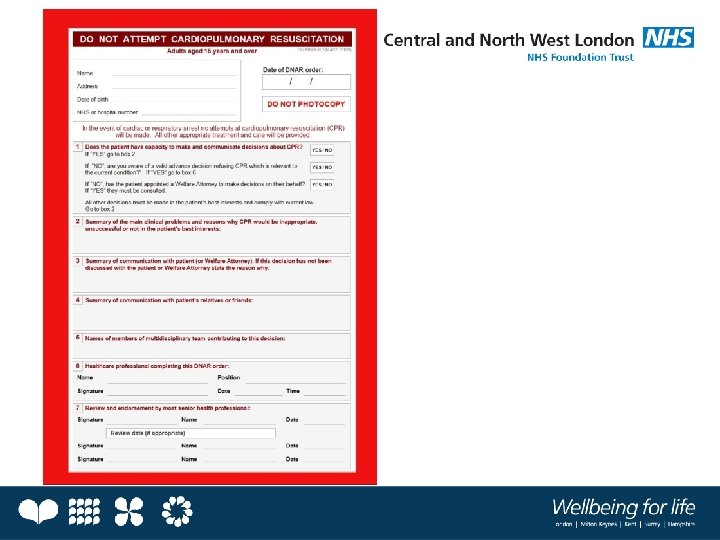
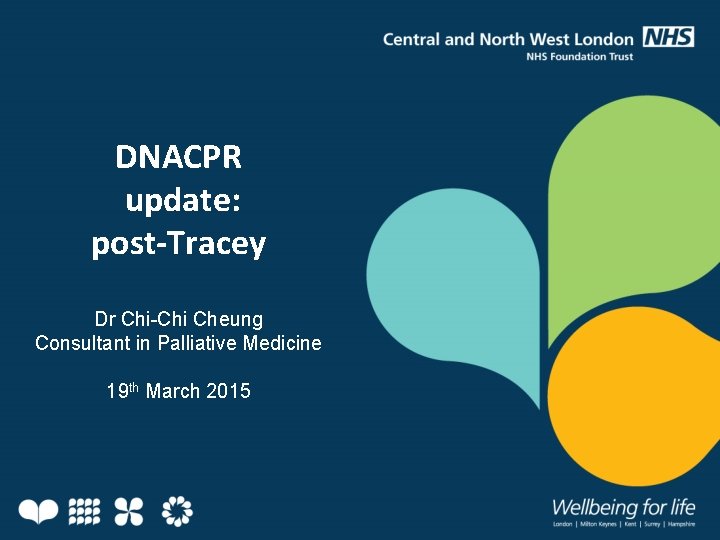
Do: ü Discuss CPR in the wider context of advance care planning and anticipatory decision-making ü Take on board patient’s view prior to making DNACPR decision ü Offer a patient information leaflet ü Make a multidisciplinary decision where possible ü Communicate DNACPR decision to patient and others involved in care ü Offer 2 nd opinion if there is disagreement & inform patient of interim plan for DNACPR ü Use the term ‘not clinically indicated due to…’ rather than ‘futile…’ perhaps as ‘cardiopulmonary arrest would represent the terminal event in their illness’ or ‘no realistic prospect of success given x condition’ ü Write conversation in notes as well as on form ü If not discussed with patient due to physical or psychological harm document this clearly (distress is not sufficient)
References • http: //www. judiciary. gov. uk/wpcontent/uploads/JCO/Documents/Judgments/tracey-v-cambridge-nhs-trust. pdf • http: //www. judiciary. gov. uk/wp-content/uploads/2014/06/tracey-approved. pdf • https: //www. resus. org. uk/pages/Statement_Tracey_judgement. pdf • http: //jme. bmj. com/content/23/6/361. full. pdf Marginally effective medical care: ethical analysis of issues in cardiopulmonary resuscitation (CPR) Hilberman et al. Journal of Medical Ethics 1997; 23: 361 -367