Oxygen as a Drug practical aspects Dr Tanmoy
- Slides: 41
Oxygen as a Drug : practical aspects Dr. Tanmoy Sar, M. D(paediatrics)
Basic chemistry… • Bivalent gas, colourless, odourless. • Has free electron pair, thus highly reactive(generates Reactive Oxygen Species/superoxide in absence of a cataion) • 21% in Air, 33% in Water, 47% in earth. Primary element behind life on earth.
Oxygen in physiology… • 62% of total body by mass is oxygen (carbon 19. 5%). • Main constituent of phosphate group( Source of energy) • Principle non halogen effector of multiple REDOX reaction (assimilation, detoxification, bacterial killing). • Main facilitator of CO 2 transport( Bohr/Haldane effect). • Oxygen sensitive K+ channels maintain synchrony of chemoreceptors. • Important regulator of pulmonary circuit pressure.
Oxygen as a Drug… • Oxygen therapy is the administration of oxygen at a concentration of pressure greater than that found in the environmental atmosphere. • It is the administration of oxygen to patients to correct hypoxemia (low oxygen blood levels) or supplemental oxygen given to a patient as a medical treatment in managing respiratory diseases that alter oxygen supply to tissue cells (hypoxia).
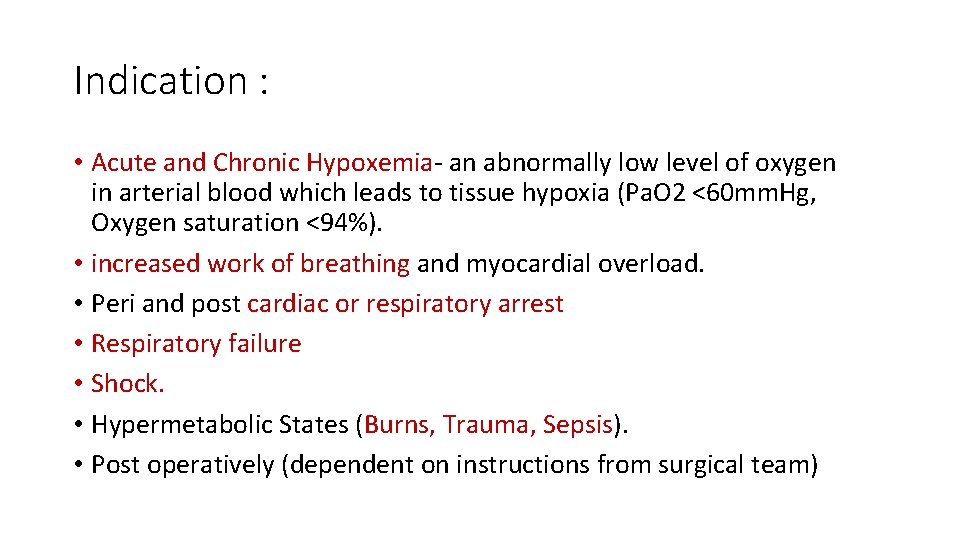
Indication : • Acute and Chronic Hypoxemia- an abnormally low level of oxygen in arterial blood which leads to tissue hypoxia (Pa. O 2 <60 mm. Hg, Oxygen saturation <94%). • increased work of breathing and myocardial overload. • Peri and post cardiac or respiratory arrest • Respiratory failure • Shock. • Hypermetabolic States (Burns, Trauma, Sepsis). • Post operatively (dependent on instructions from surgical team)
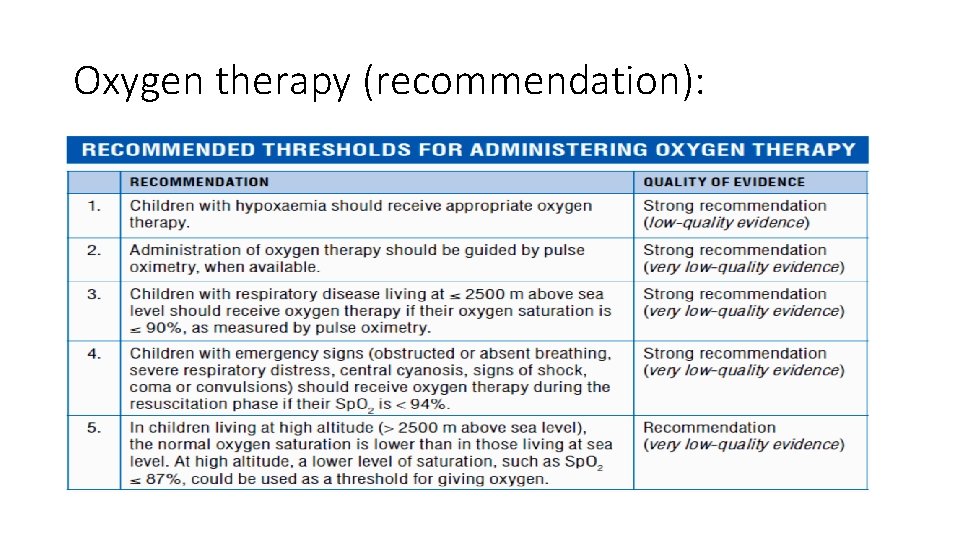
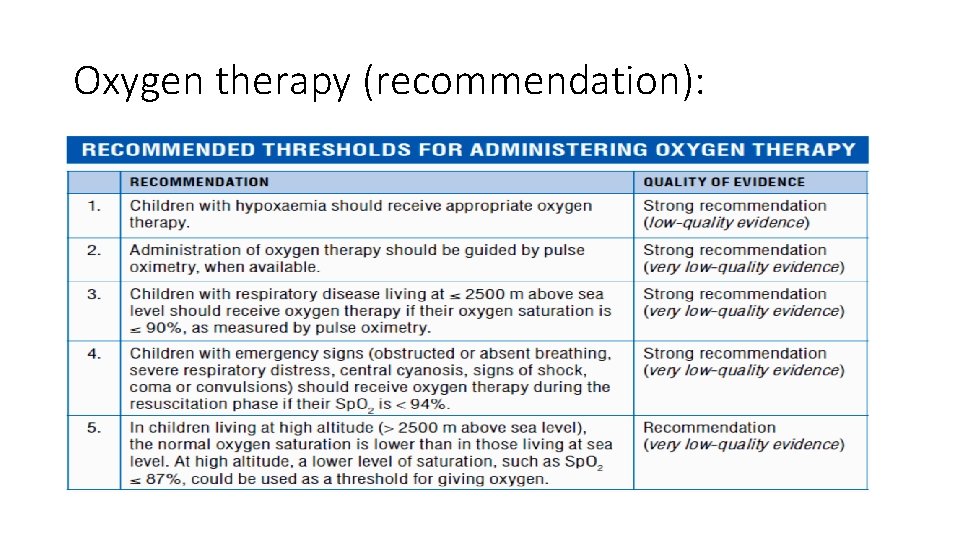
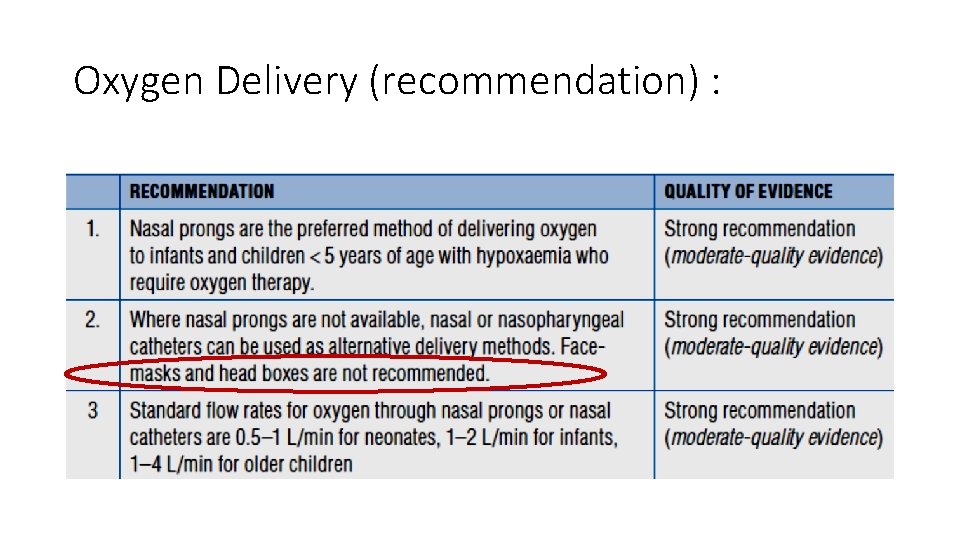
Oxygen therapy (recommendation):
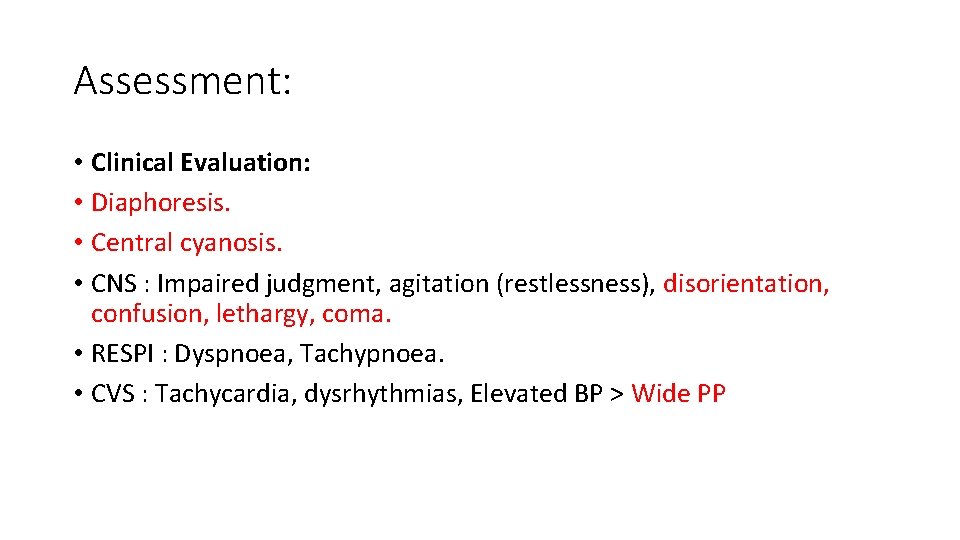
Assessment: • Clinical Evaluation: • Diaphoresis. • Central cyanosis. • CNS : Impaired judgment, agitation (restlessness), disorientation, confusion, lethargy, coma. • RESPI : Dyspnoea, Tachypnoea. • CVS : Tachycardia, dysrhythmias, Elevated BP > Wide PP
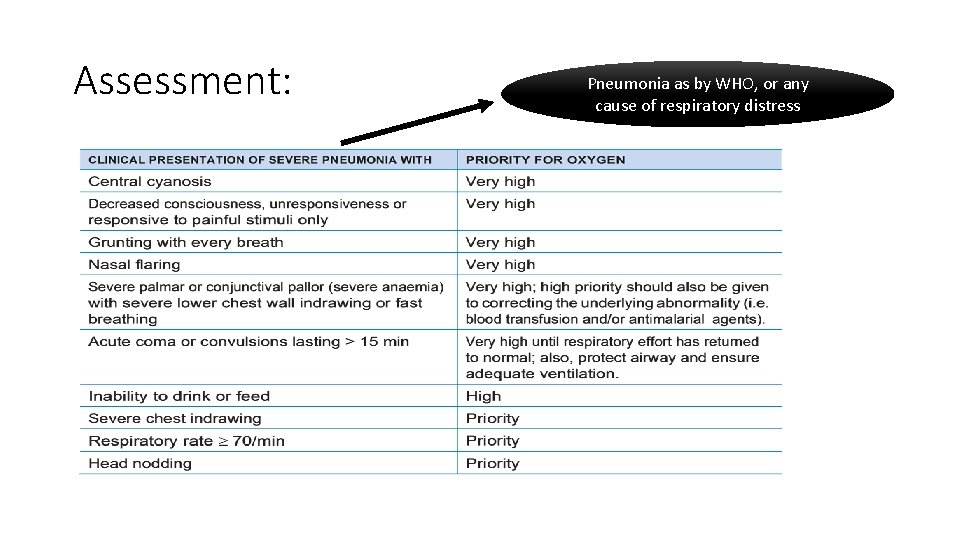
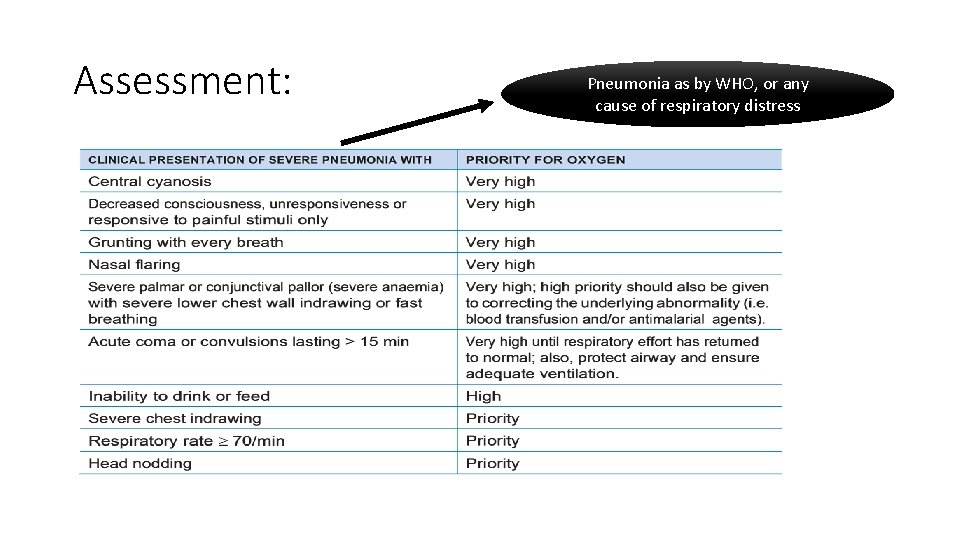
Assessment: Pneumonia as by WHO, or any cause of respiratory distress
ABG: • Gold standard to diagnose hypoxemia (Pa. O 2<60 mm Hg), some may show total oxygen content (>13 ml at STM; requires calibration), Aa. DO 2 (to dx the cause respi/ CVS). • Lack of availability , mainly in HRS.
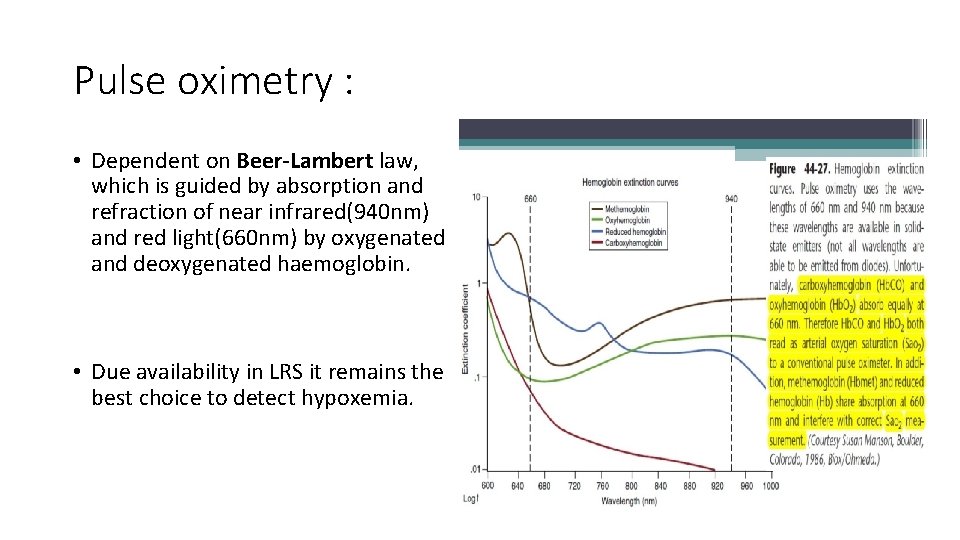
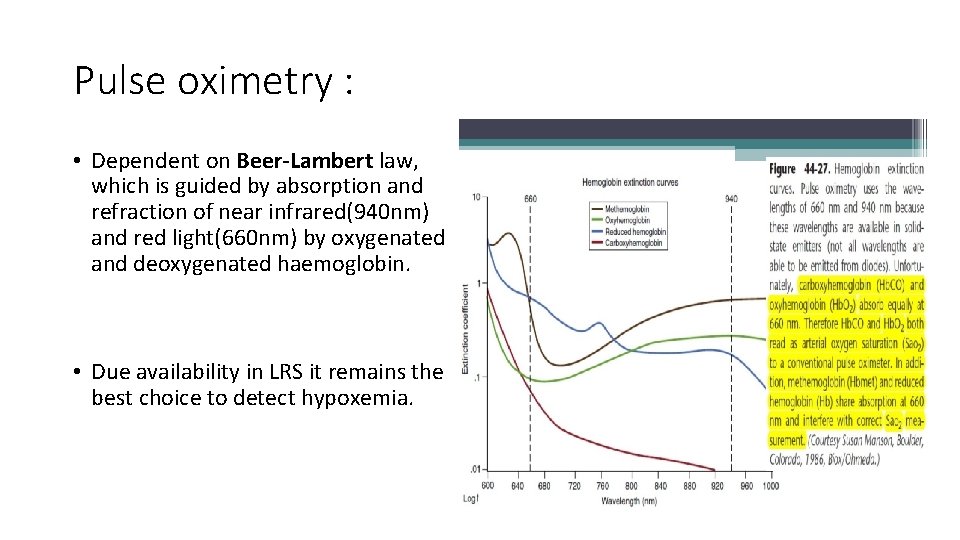
Pulse oximetry : • Dependent on Beer-Lambert law, which is guided by absorption and refraction of near infrared(940 nm) and red light(660 nm) by oxygenated and deoxygenated haemoglobin. • Due availability in LRS it remains the best choice to detect hypoxemia.
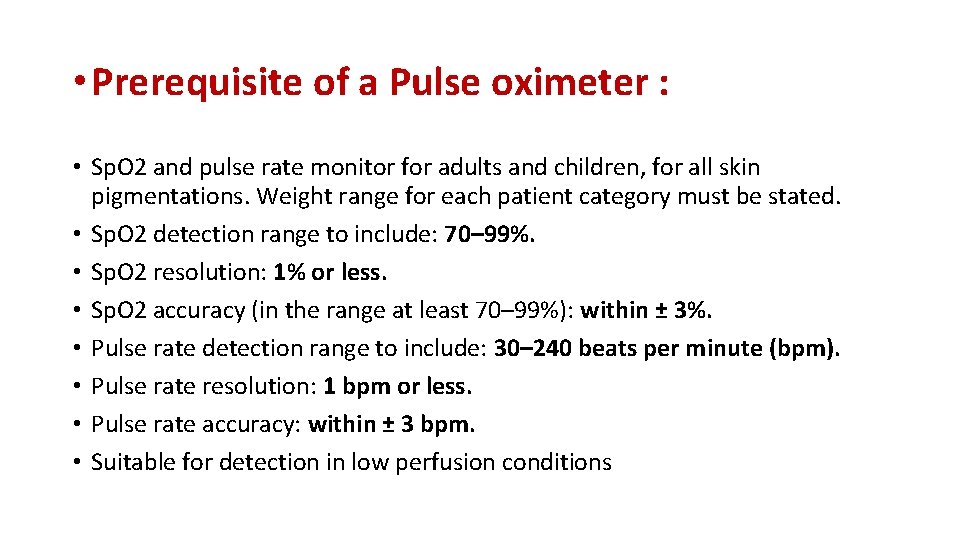
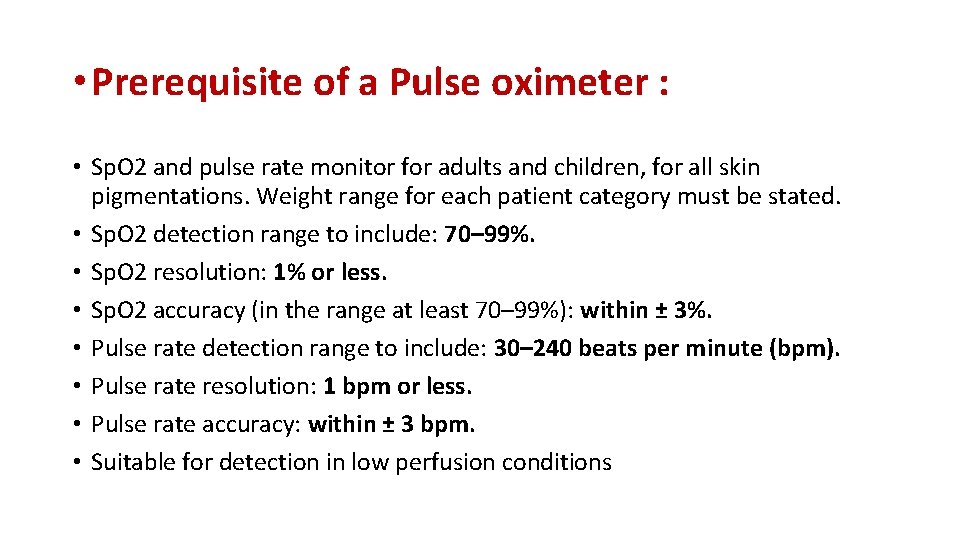
• Prerequisite of a Pulse oximeter : • Sp. O 2 and pulse rate monitor for adults and children, for all skin pigmentations. Weight range for each patient category must be stated. • Sp. O 2 detection range to include: 70– 99%. • Sp. O 2 resolution: 1% or less. • Sp. O 2 accuracy (in the range at least 70– 99%): within ± 3%. • Pulse rate detection range to include: 30– 240 beats per minute (bpm). • Pulse rate resolution: 1 bpm or less. • Pulse rate accuracy: within ± 3 bpm. • Suitable for detection in low perfusion conditions
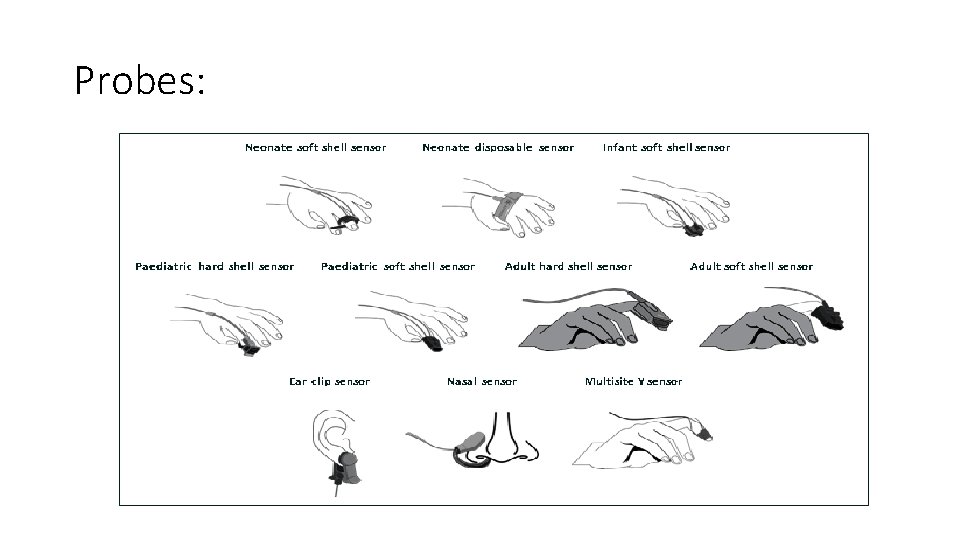
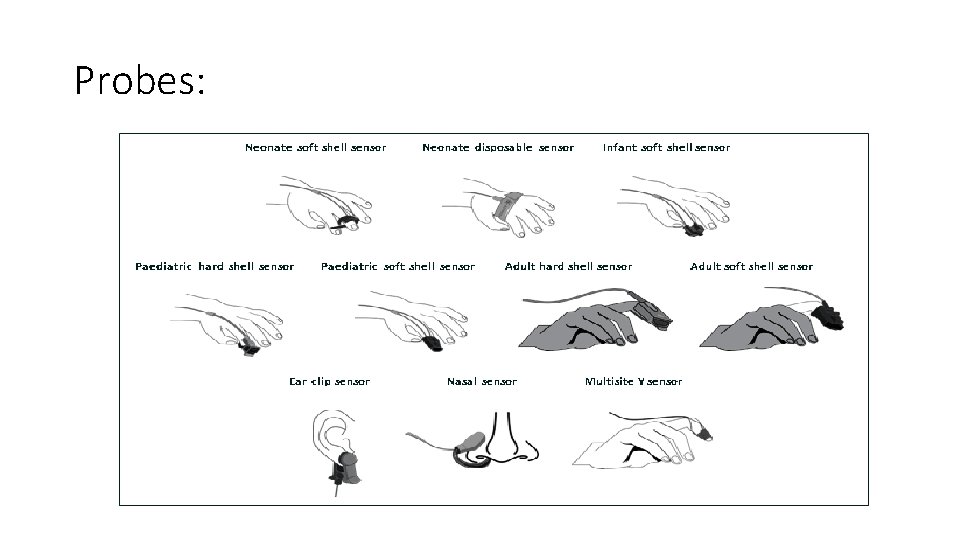
Probes:
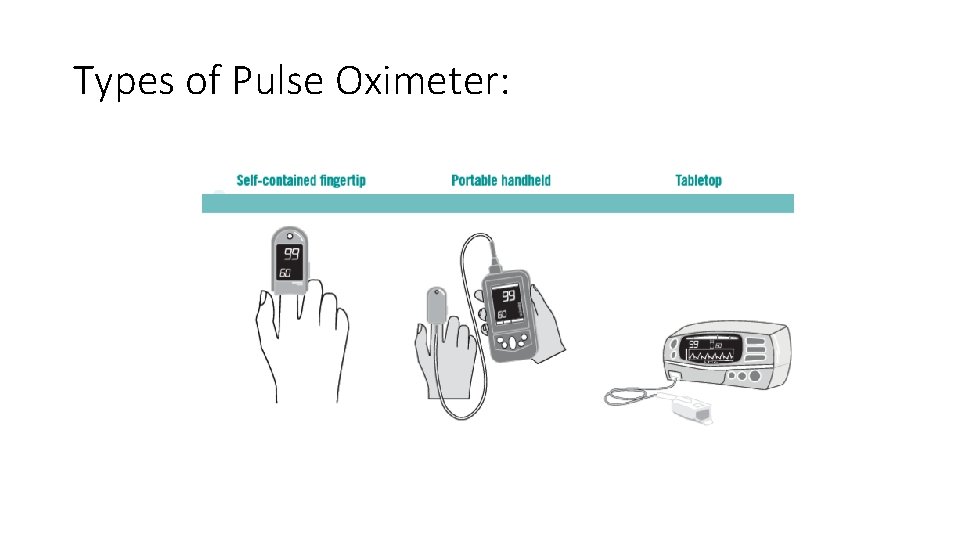
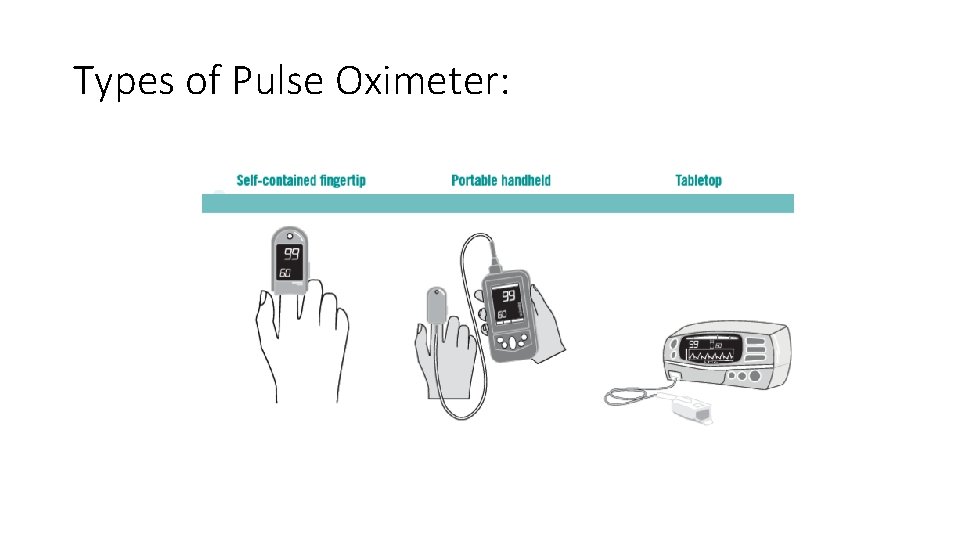
Types of Pulse Oximeter:
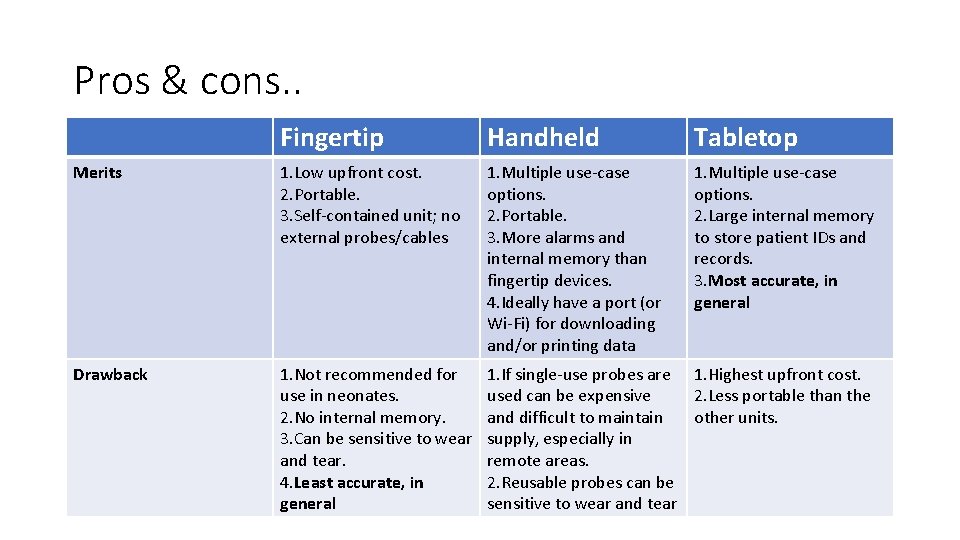
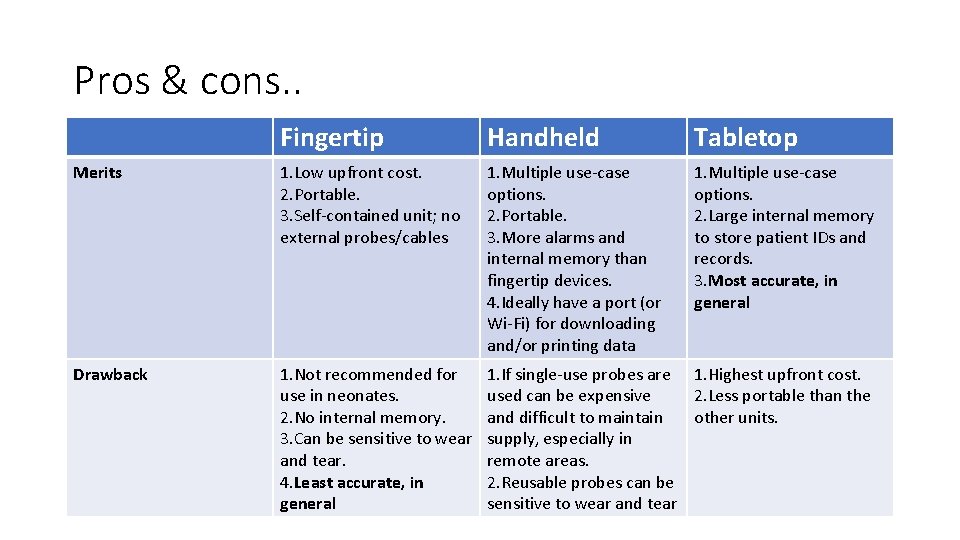
Pros & cons. . Fingertip Handheld Tabletop Merits 1. Low upfront cost. 2. Portable. 3. Self-contained unit; no external probes/cables 1. Multiple use-case options. 2. Portable. 3. More alarms and internal memory than fingertip devices. 4. Ideally have a port (or Wi-Fi) for downloading and/or printing data 1. Multiple use-case options. 2. Large internal memory to store patient IDs and records. 3. Most accurate, in general Drawback 1. Not recommended for use in neonates. 2. No internal memory. 3. Can be sensitive to wear and tear. 4. Least accurate, in general 1. If single-use probes are 1. Highest upfront cost. used can be expensive 2. Less portable than the and difficult to maintain other units. supply, especially in remote areas. 2. Reusable probes can be sensitive to wear and tear
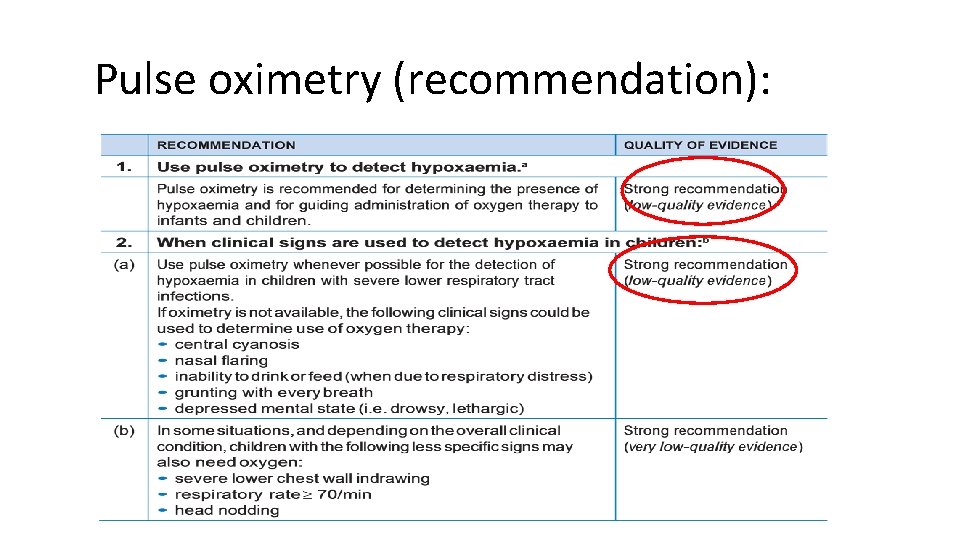
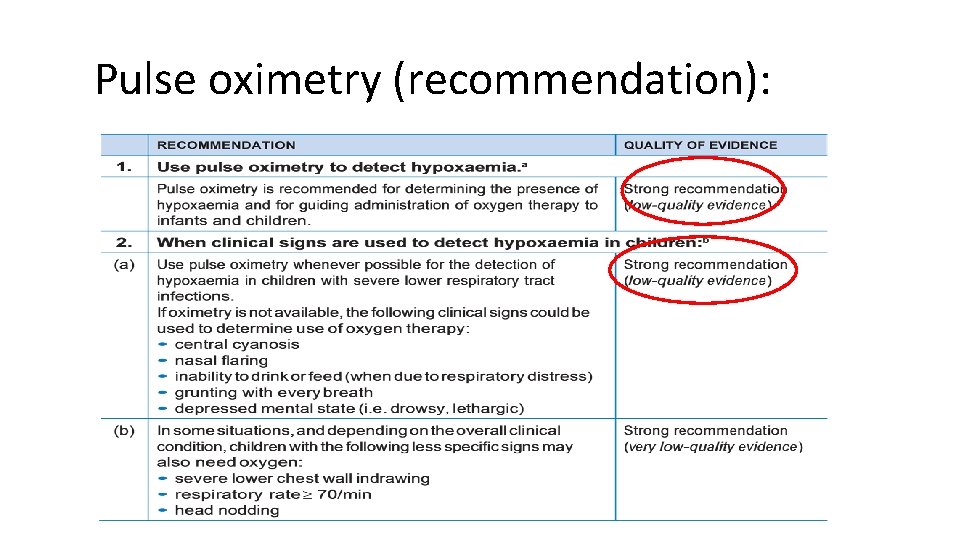
Pulse oximetry (recommendation):
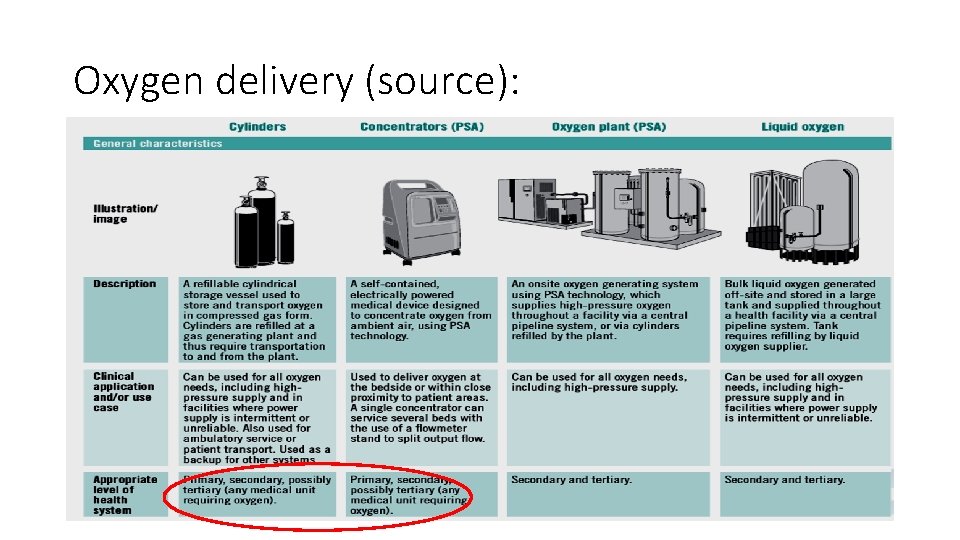
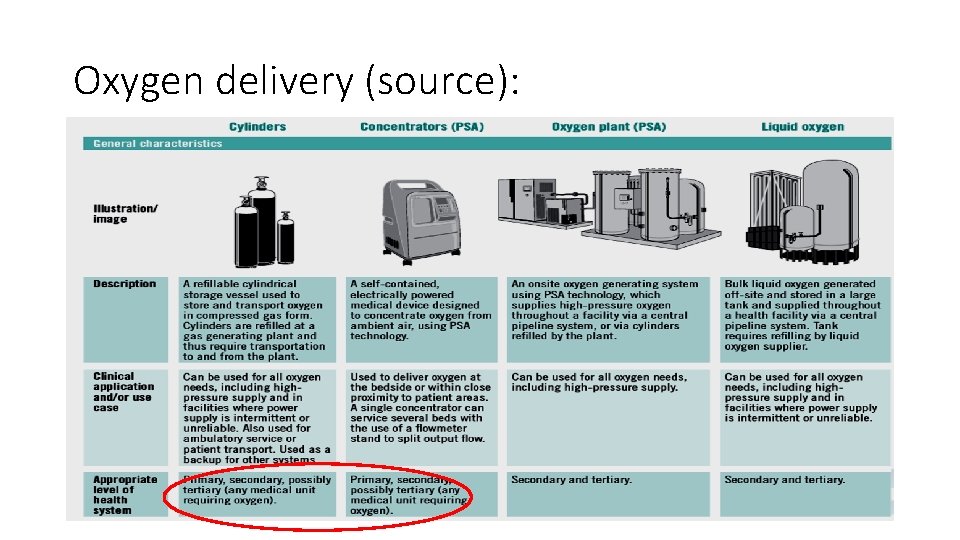
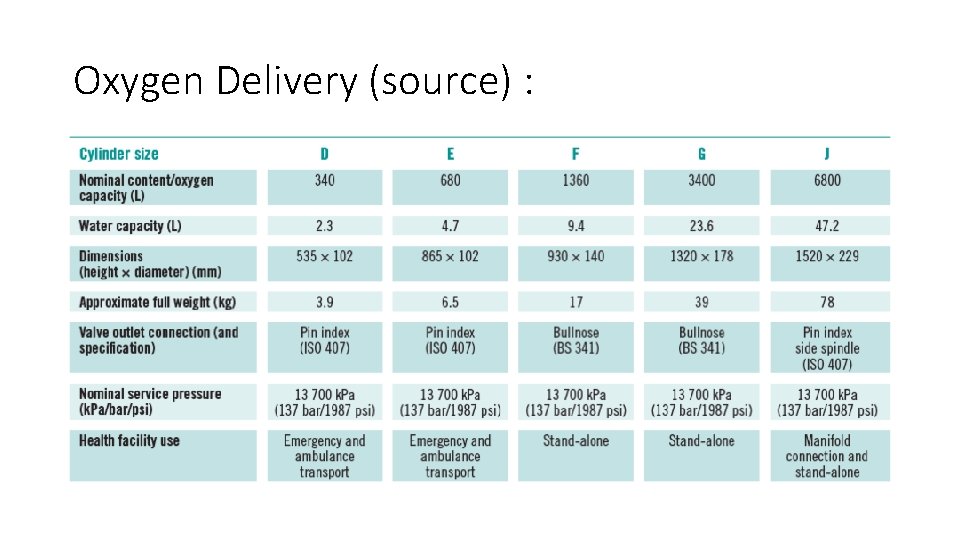
Oxygen delivery (source):
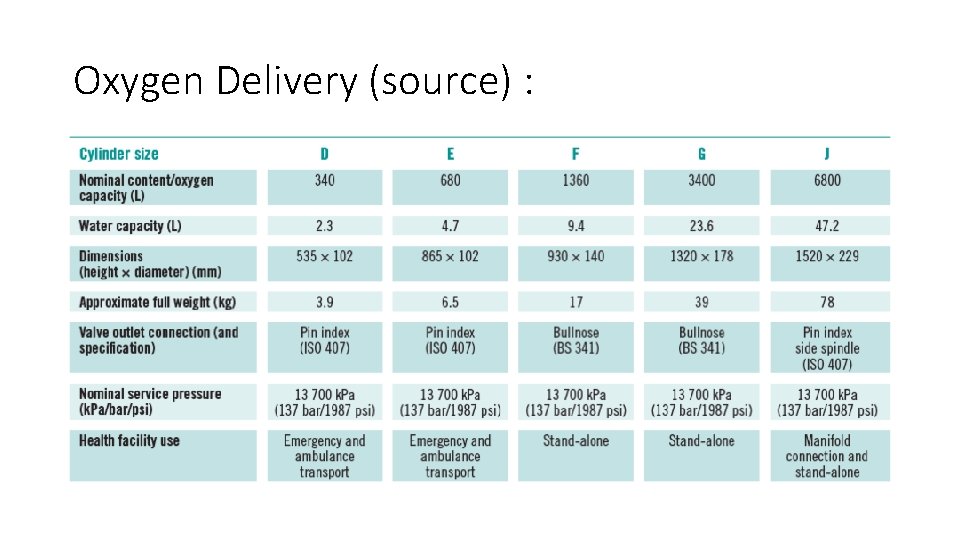
Oxygen Delivery (source) :
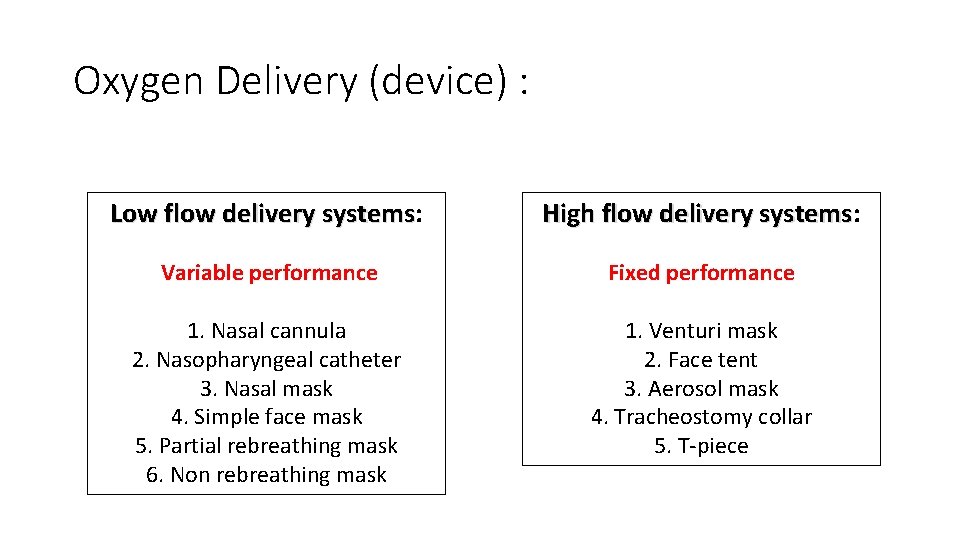
Oxygen Delivery (device) : Low flow delivery systems: systems High flow delivery systems: systems Variable performance Fixed performance 1. Nasal cannula 2. Nasopharyngeal catheter 3. Nasal mask 4. Simple face mask 5. Partial rebreathing mask 6. Non rebreathing mask 1. Venturi mask 2. Face tent 3. Aerosol mask 4. Tracheostomy collar 5. T-piece
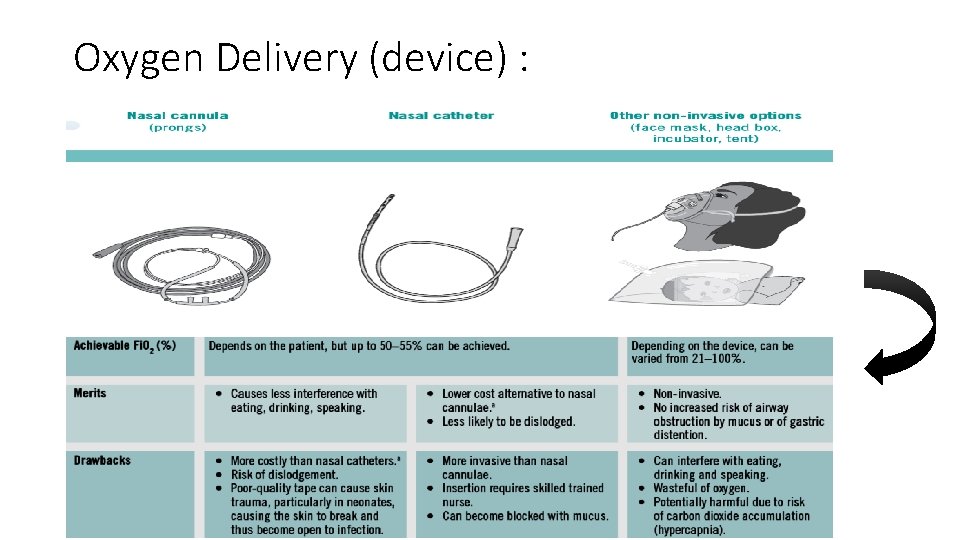
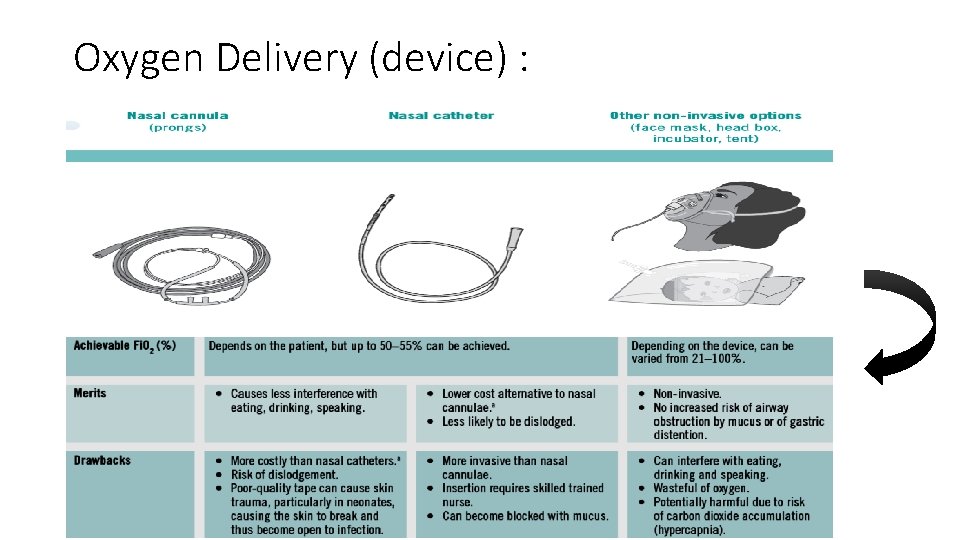
Oxygen Delivery (device) :
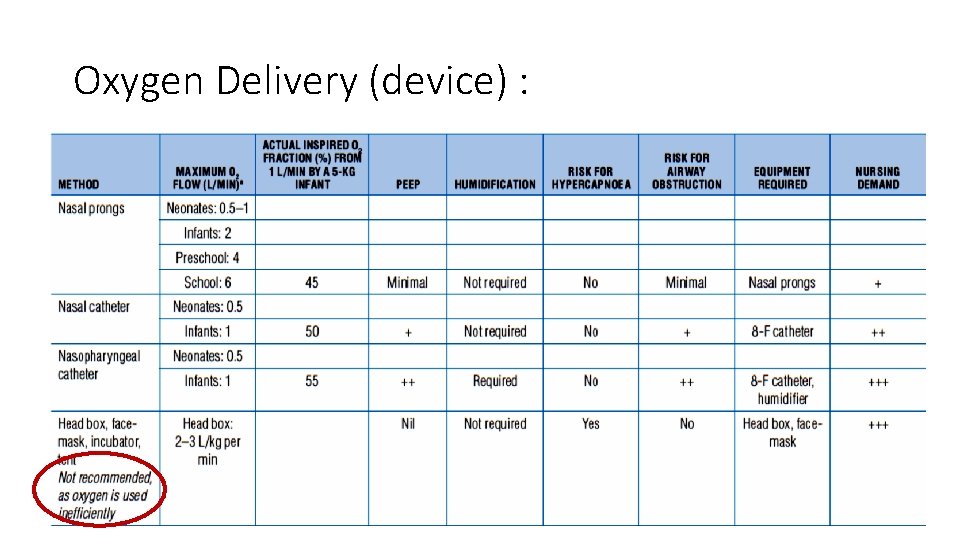
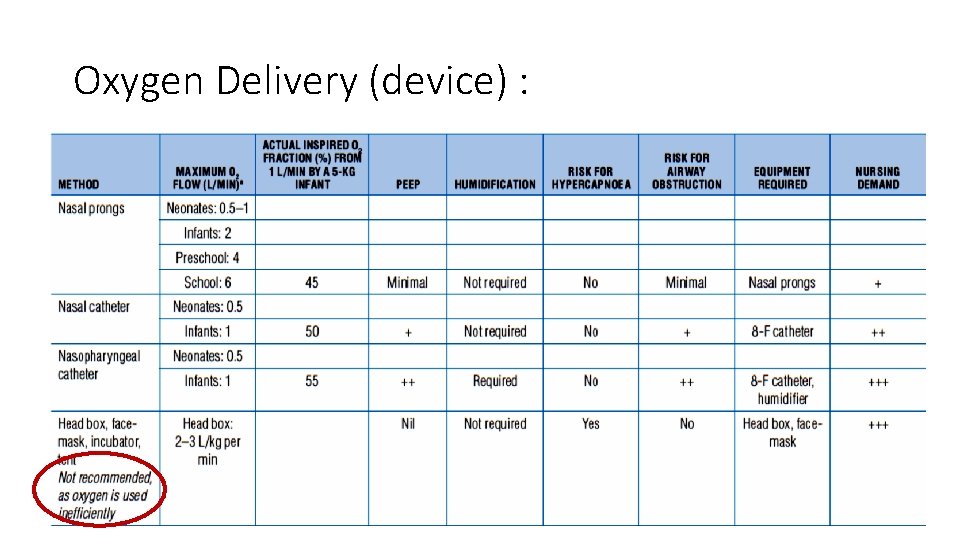
Oxygen Delivery (device) :
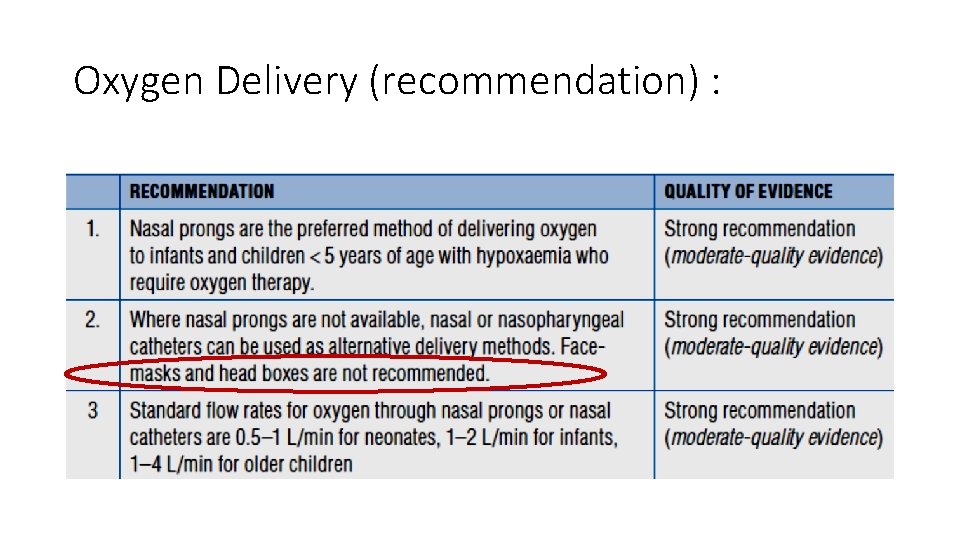
Oxygen Delivery (recommendation) :
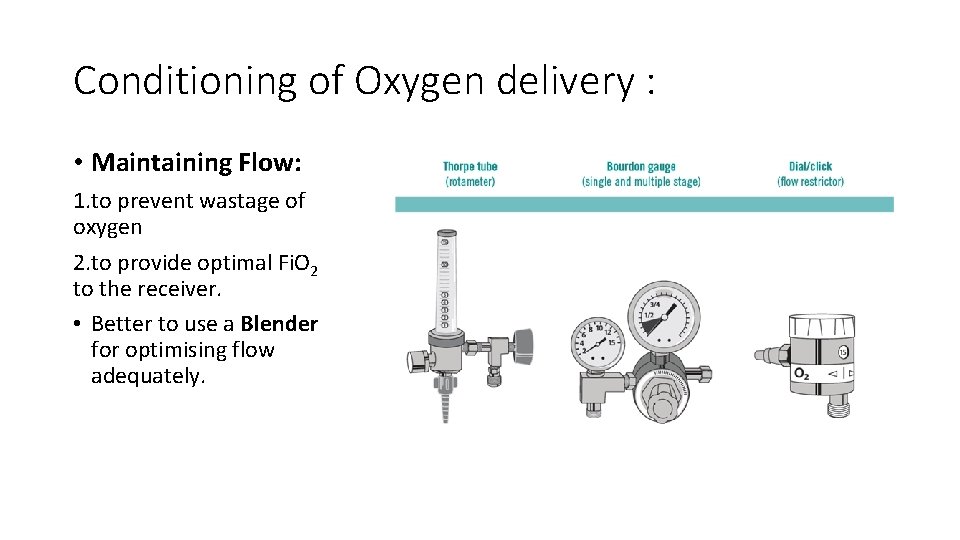
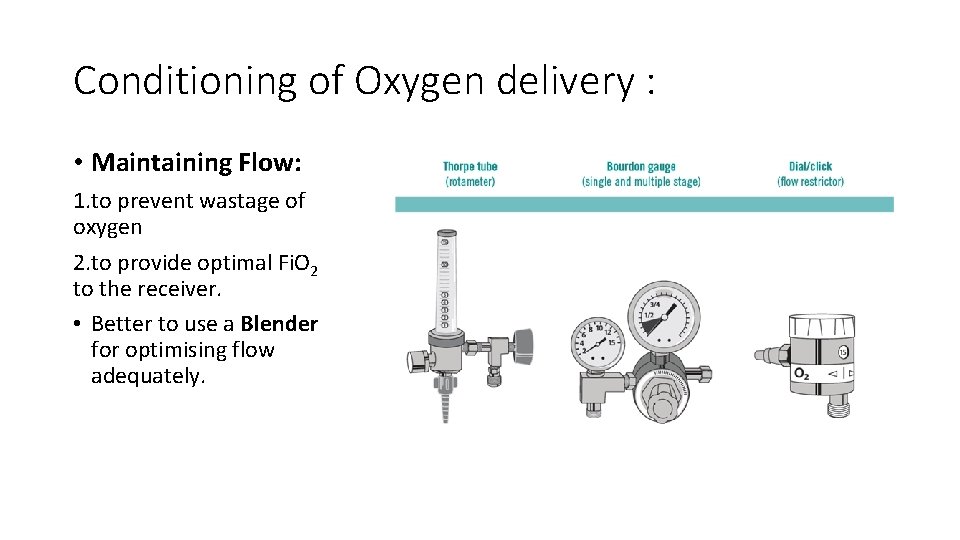
Conditioning of Oxygen delivery : • Maintaining Flow: 1. to prevent wastage of oxygen 2. to provide optimal Fi. O 2 to the receiver. • Better to use a Blender for optimising flow adequately.
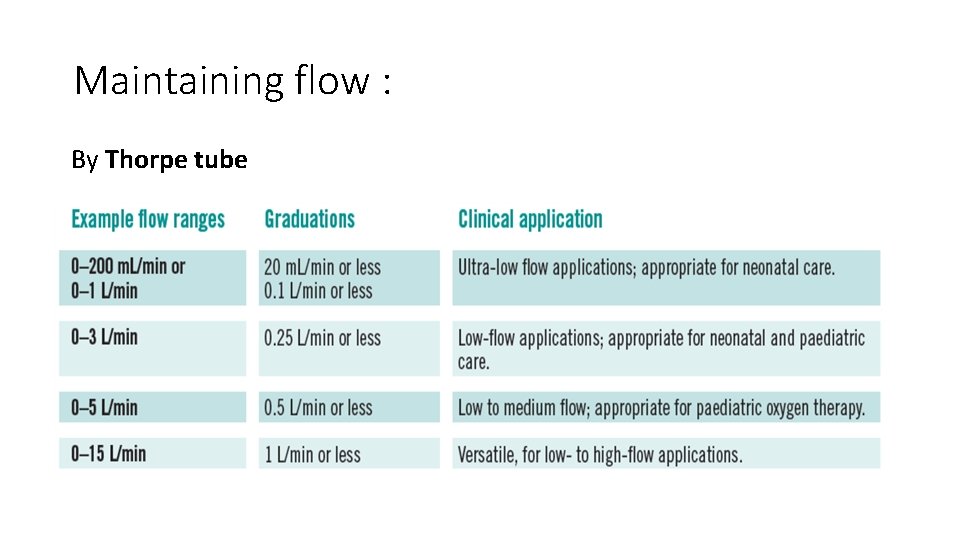
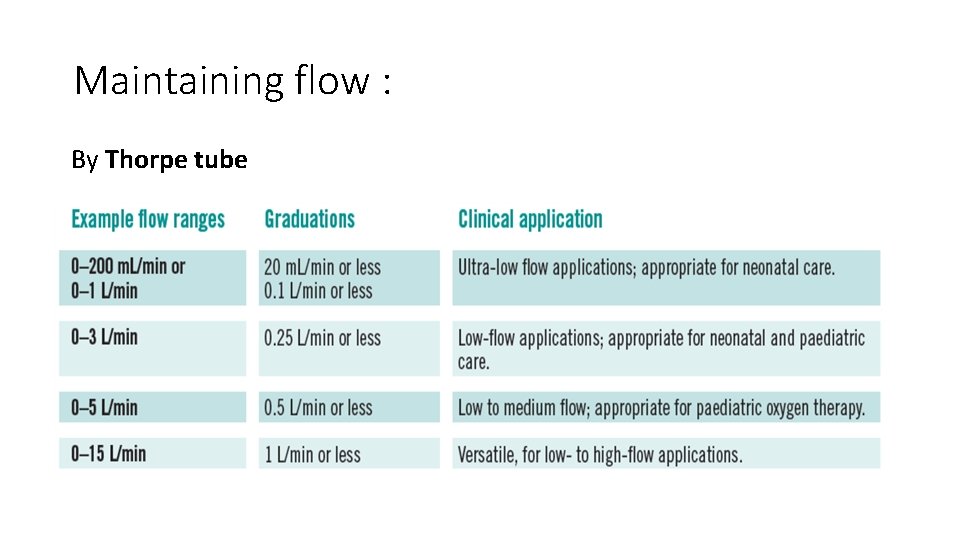
Maintaining flow : By Thorpe tube
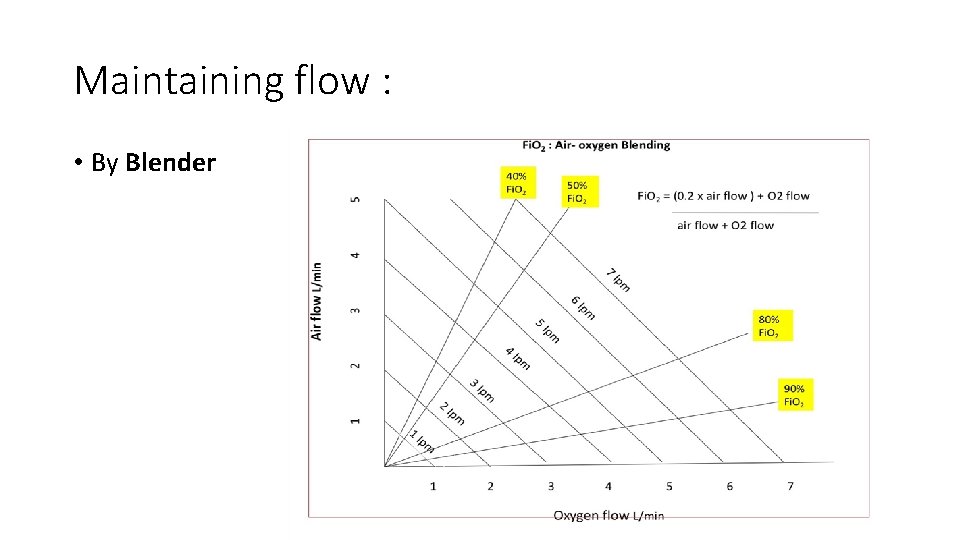
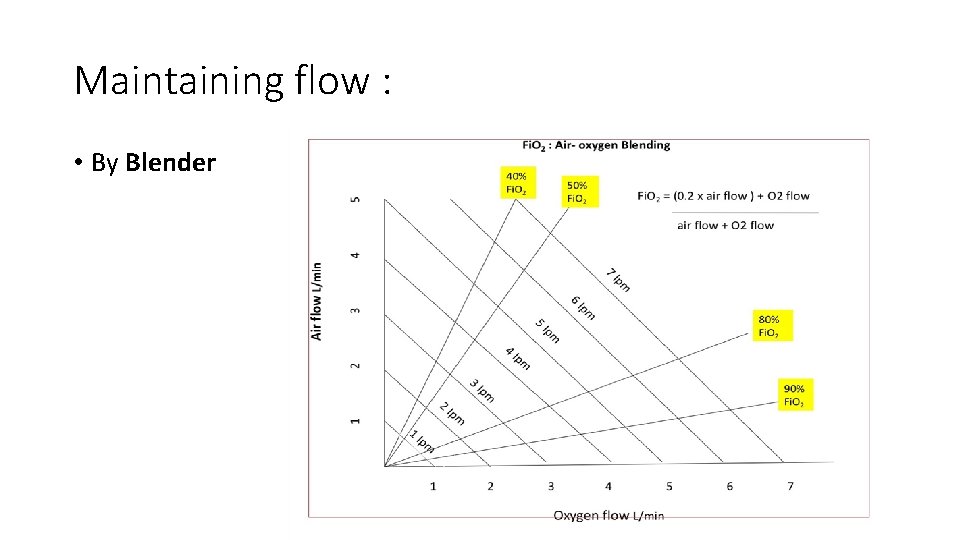
Maintaining flow : • By Blender
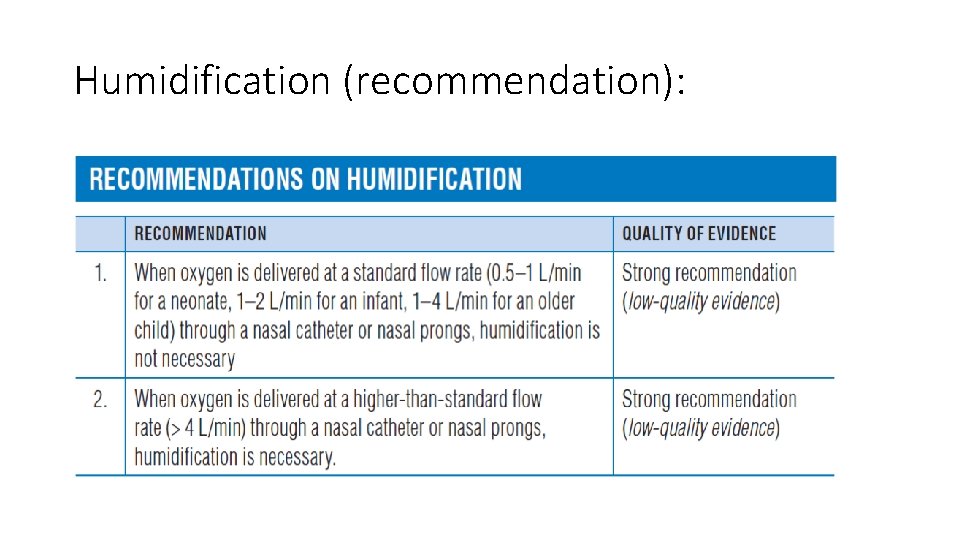
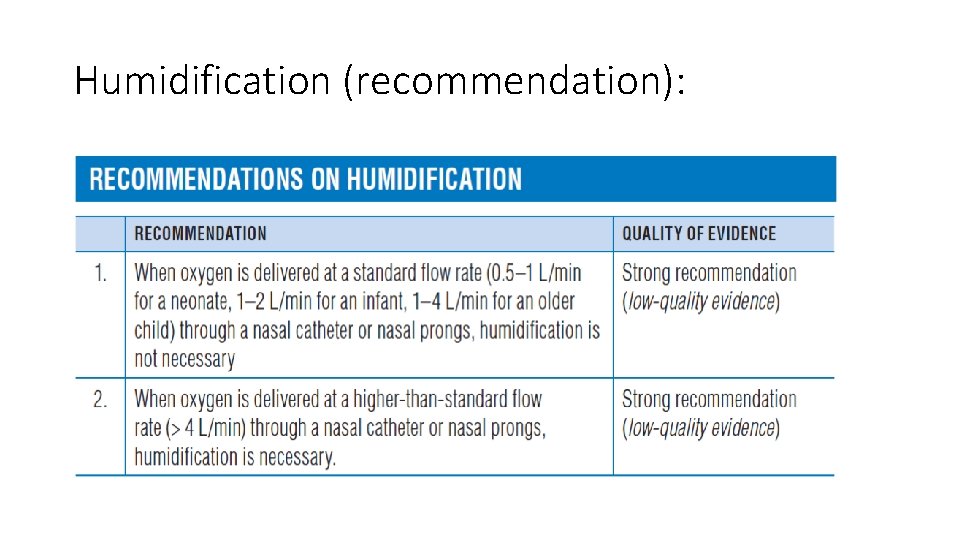
Humidification (recommendation):
O 2 therapy in acute cases…… • Paediatric practice remains one of the most chaotic area in regard to oxygen therapy because of the patients age, parents anxiety and above all very less intervention time to prevent drastic consequences. • 3 most prevalent cause of respiratory distress needing immediate oxygen support are 1. severe pneumonia 2. Bronchiolitis 3. Acute exacerbation of Childhood asthma.
Guideline : • According to WHO, for severe pneumonia the cut off to start oxygen therapy remains at Sp. O 2 <94% with emergency signs @sea level, Sp. O 2 < 90% @2500 mtr with distress, Sp. O 2 < 87% above 2500 mtr with distress. • For AE Asthma, guideline given by GINA (2020 update) defines Severe acute exacerbation when Sp. O 2 < 90% (previously 92%), which is the indication to start oxygen therapy in a controlled way to achieve a target of 93 -95% Sp. O 2 (94 -98% for age 6 -11 yrs) but not at 100%.
Guideline : • For Bronchiolitis the AAP 2014 CPG says that the threshold to start oxygen is Sp. O 2<90% which may be discontinued if Sp. O 2 > 90% for infants and children.
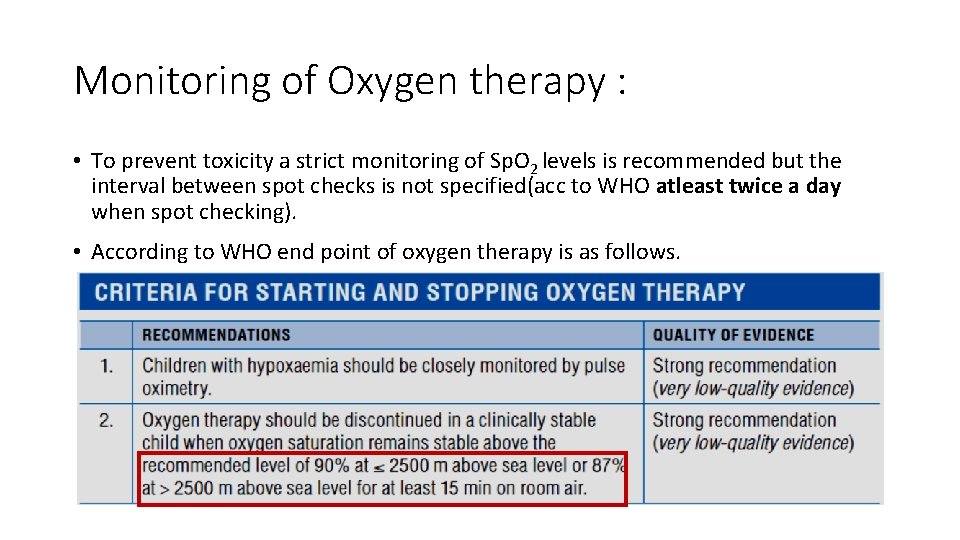
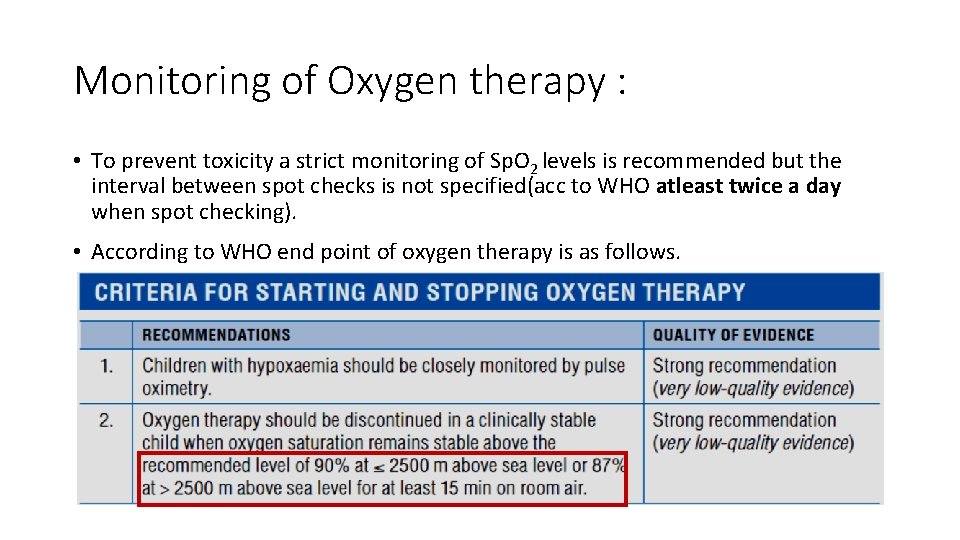
Monitoring of Oxygen therapy : • To prevent toxicity a strict monitoring of Sp. O 2 levels is recommended but the interval between spot checks is not specified(acc to WHO atleast twice a day when spot checking). • According to WHO end point of oxygen therapy is as follows.
Home O 2 therapy: • Approved by ATS on December 2018 to provide evidenced based care to those patients who are in need for chronic long term oxygen therapy(chronic respiratory and vascular conditions) which is not possible in hospital settings. • Approved technique : 1. Weight and age appropriate nasal cannula, nasal mask. 2. Oxygen concentrators(flow 1 -5 lt/min max Fi. O 2 ~ 95%), cylinders if only for few months. 3. Age appropriate flow meters (low flow upto 1 lt/min and low to high flow 1 -5 lt/min) 4. Humidification if flow >1 lt/min.
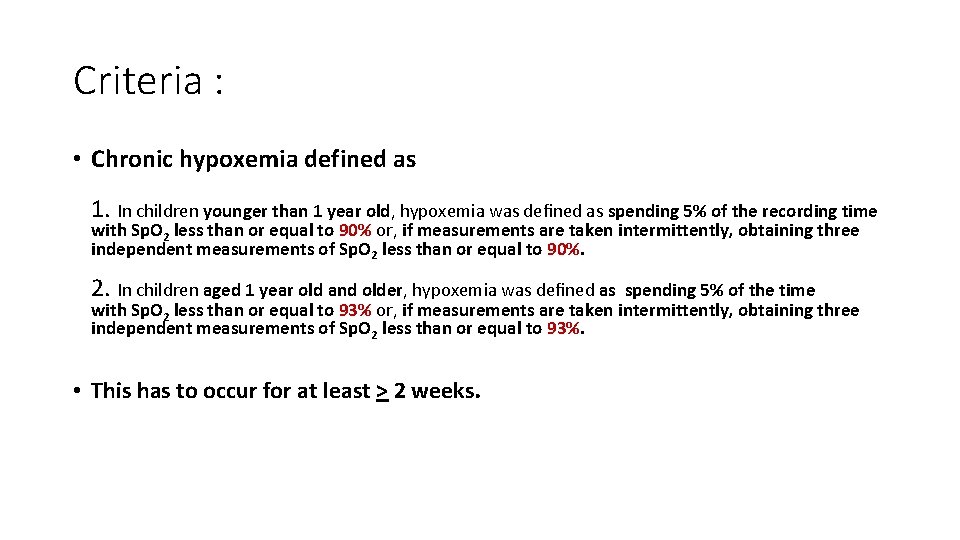
Criteria : • Chronic hypoxemia defined as 1. In children younger than 1 year old, hypoxemia was defined as spending 5% of the recording time with Sp. O 2 less than or equal to 90% or, if measurements are taken intermittently, obtaining three independent measurements of Sp. O 2 less than or equal to 90%. 2. In children aged 1 year old and older, hypoxemia was defined as spending 5% of the time with Sp. O 2 less than or equal to 93% or, if measurements are taken intermittently, obtaining three independent measurements of Sp. O 2 less than or equal to 93%. • This has to occur for at least > 2 weeks.
Monitoring : • By intermittent Sp. O 2 measurement to maintain a Sp. O 2 above defined ranges ( 90%/93%). • In case of erroneous Sp. O 2 measurement in a spot check better to verify by sleep time continuous Sp. O 2 monitoring. • Scope of Pa. O 2 measurement is very scant thus it is generally not recommended.
Weaning : • No definite criteria, if nocturnal Sp. O 2 assessment is above expected range, then can be gradually weaned of by quartile reduction of flow over weeks. • Other medications like diuretics in BPD should be used per protocol to facilitate the weaning process. • To enlist for long term follow up.
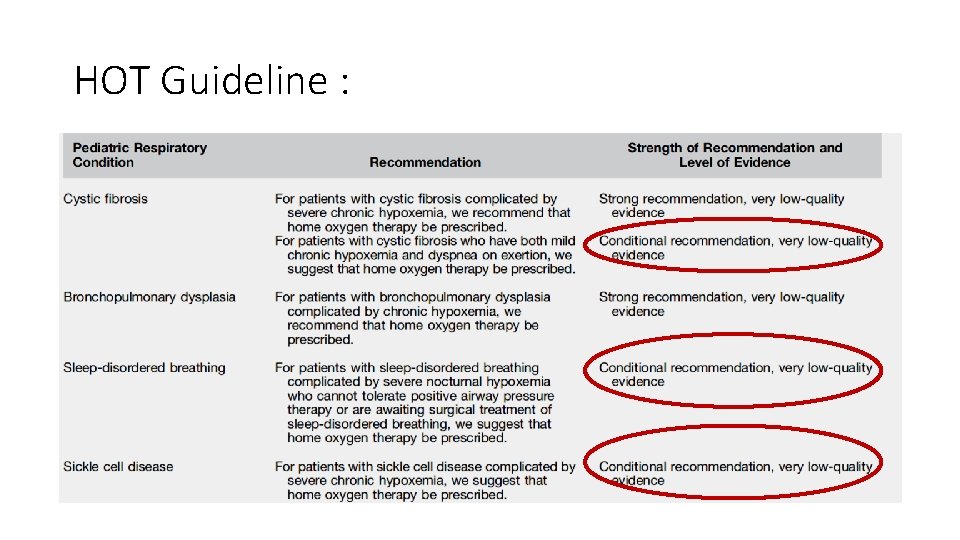
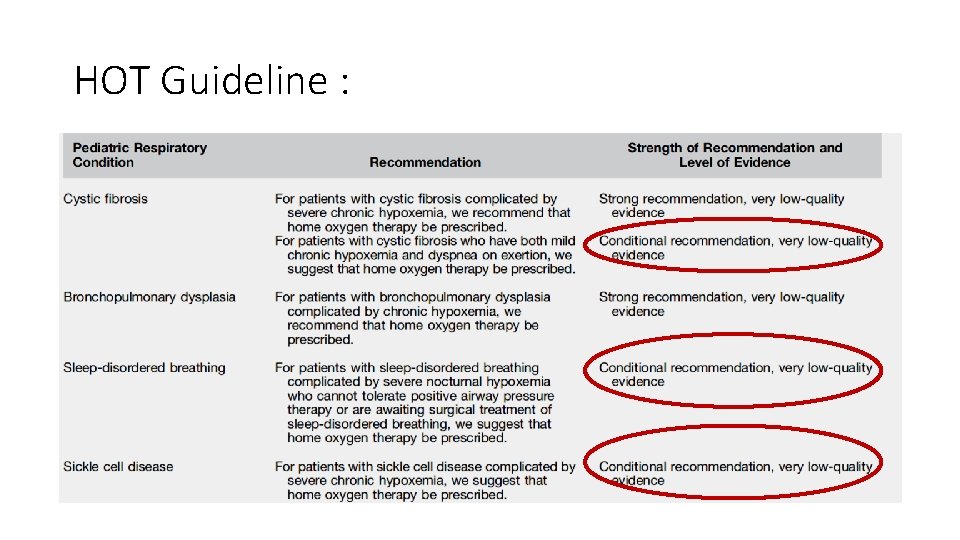
HOT Guideline :
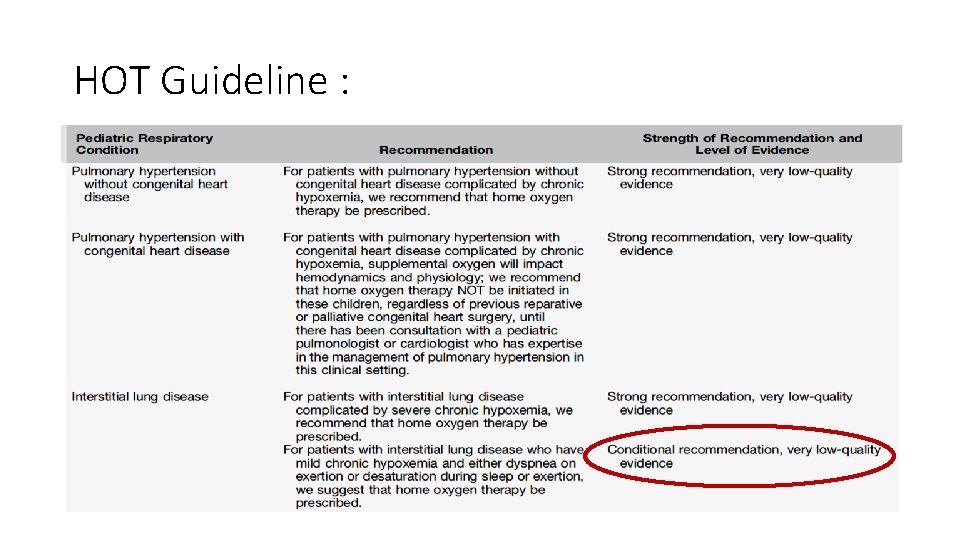
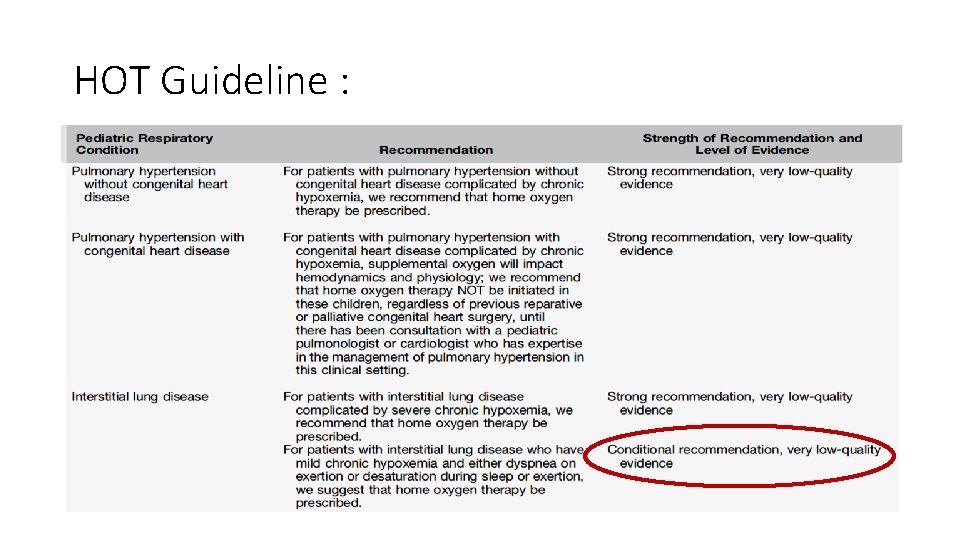
HOT Guideline :
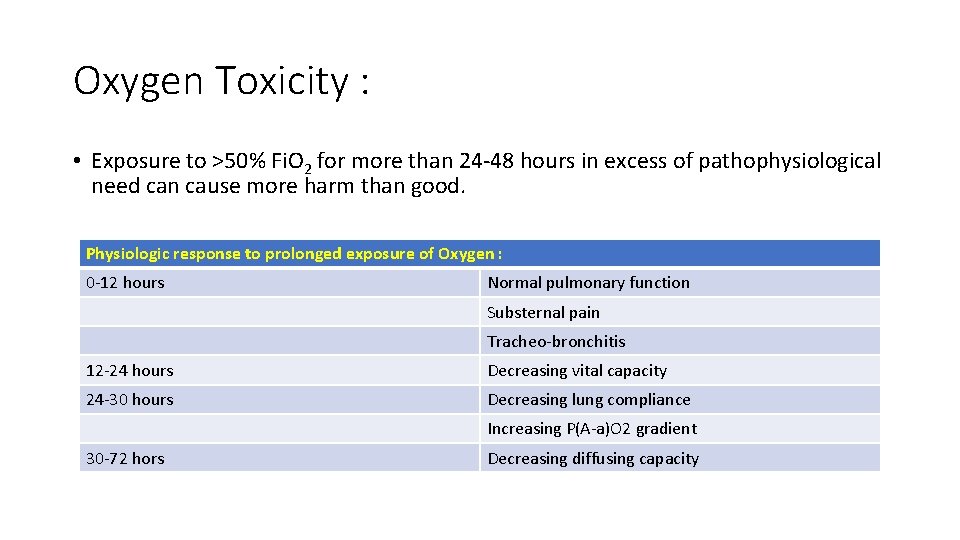
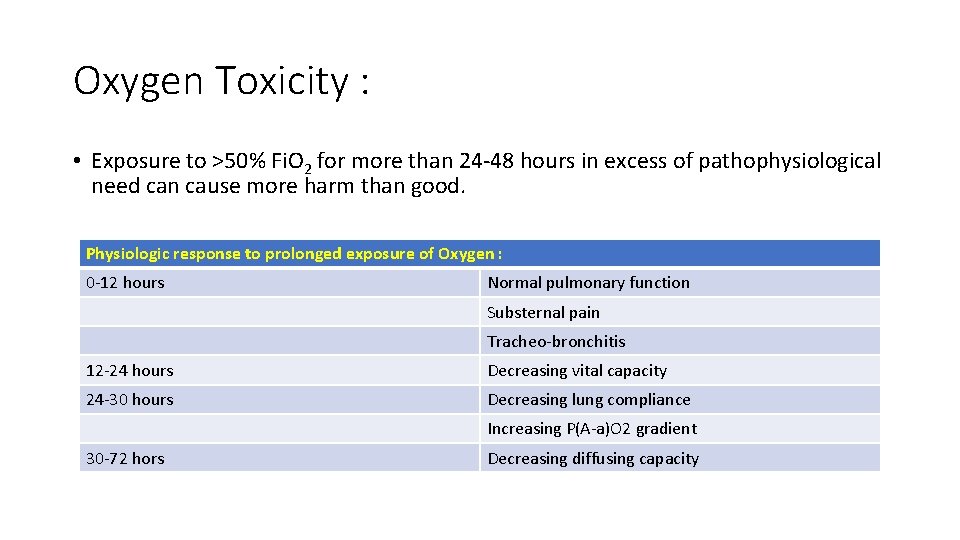
Oxygen Toxicity : • Exposure to >50% Fi. O 2 for more than 24 -48 hours in excess of pathophysiological need can cause more harm than good. Physiologic response to prolonged exposure of Oxygen : 0 -12 hours Normal pulmonary function Substernal pain Tracheo-bronchitis 12 -24 hours Decreasing vital capacity 24 -30 hours Decreasing lung compliance Increasing P(A-a)O 2 gradient 30 -72 hors Decreasing diffusing capacity
Oxygen Toxicity : • Mainly affects CNS & Lungs by Intracellular generation of free radicals e. g. : superoxide, H 2 O 2 , singlet oxygen (anti-oxidants ineffective in high O 2). • CNS symptoms are tremor, twitching, convulsion if breathed >1 atm pressure for prolonged period. • Lungs are damaged by free radicals and LORRAIN-SMITH EFFECT( interstitial oedema) simulates a broncho-pneumonia like CXR and symptoms ultimately progressing to fibrosis and PAH.
Oxygen Toxicity : • Can cause depression of ventilation in low tidal volume/ hypercapnia adapted patients. (Head injury) • Absorption atelectasis by washing out nitrogen. (one lung ventilation = upper lobe collapse) • Retinopathy of prematurity. • Retrolental Fibroplasia.
Precautions : • Fire Hazard. (not inflammable but acts as a facilitator).
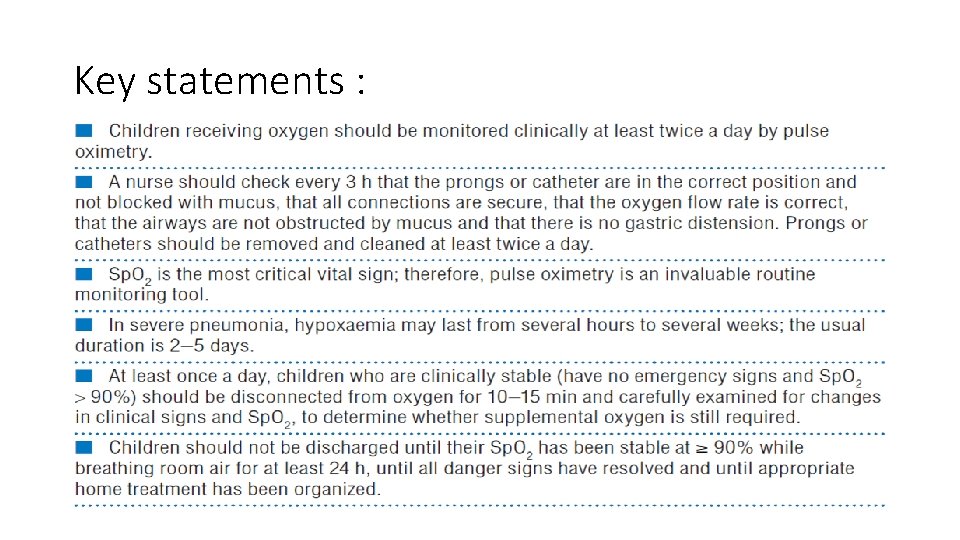
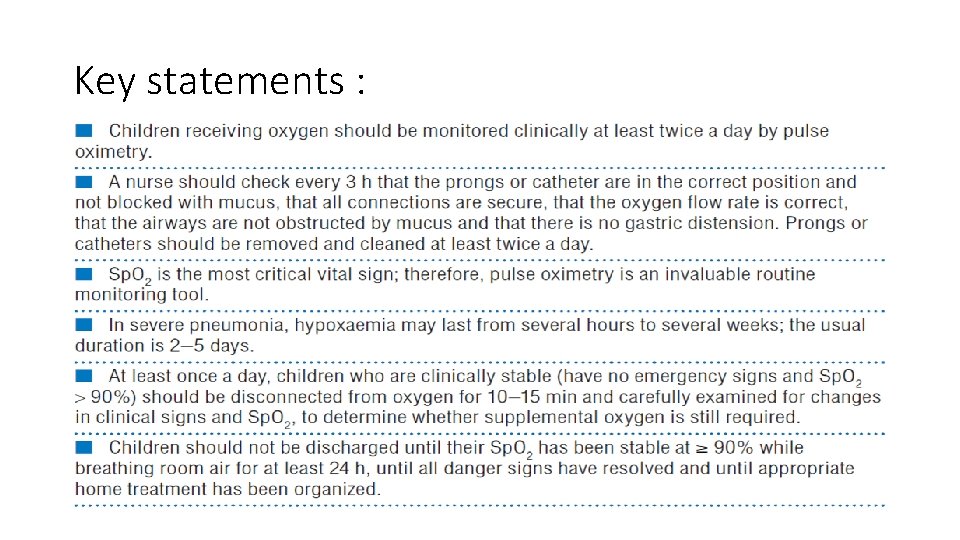
Key statements :
Thank You