Overview of Connective Tissue Disease Dr Ng Swee
- Slides: 28
Overview of Connective Tissue Disease Dr Ng Swee Cheng Senior Consultant SGH Department of Rheumatology & Immunology Adjunct Associate Professor Duke-NUS Medical School
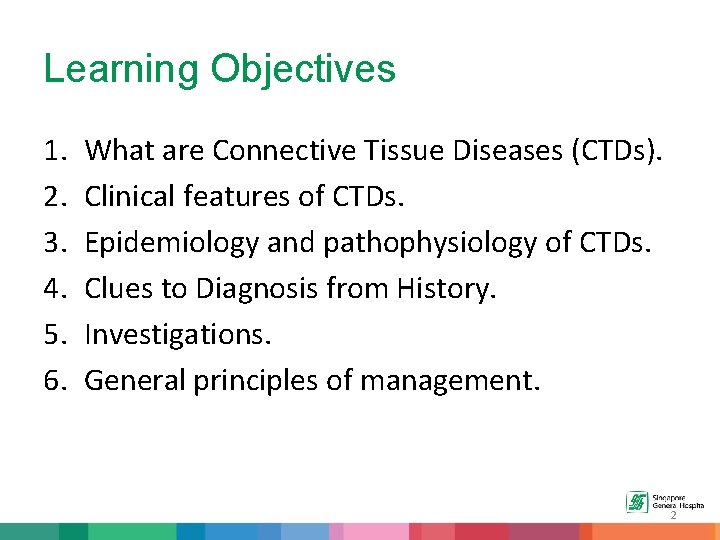
Learning Objectives 1. 2. 3. 4. 5. 6. What are Connective Tissue Diseases (CTDs). Clinical features of CTDs. Epidemiology and pathophysiology of CTDs. Clues to Diagnosis from History. Investigations. General principles of management. 2
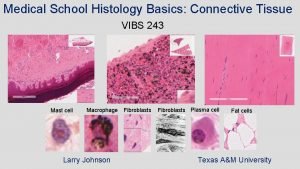
What are Connective Tissue Diseases? Connective tissue diseases are diseases of the connective tissue caused by systemic inflammation due to autoimmunity. not just any disease that affects connective tissue 3
What are Connective Tissue Diseases? • Connective Tissue Diseases 1. Systemic Lupus Erythematosus (includes Anti -Phospholipid Syndrome ) 2. Systemic Sclerosis 3. Inflammatory Muscle Disease 4. Sjogren’s Syndrome 4
Systemic Lupus Erythematosus - SLE • “Systemic” – disease can affect many systems in the body – blood cells, kidney, brain, etc. • “Lupus” – Latin word for “wolf”. Patients may have typical “wolf-like” facial rash. • “Erythematosus” – red, or inflammed.
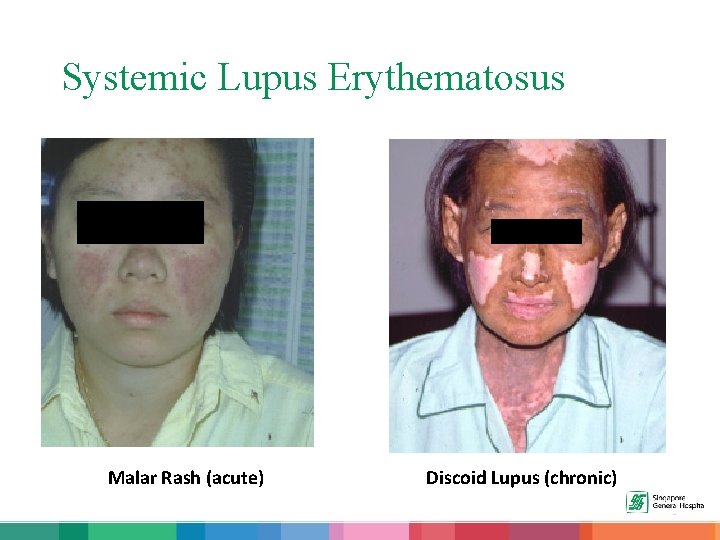
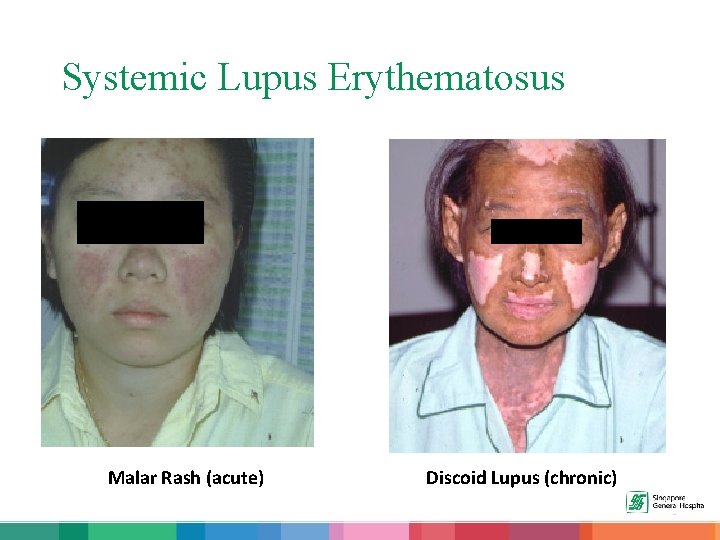
Systemic Lupus Erythematosus Malar Rash (acute) Discoid Lupus (chronic)
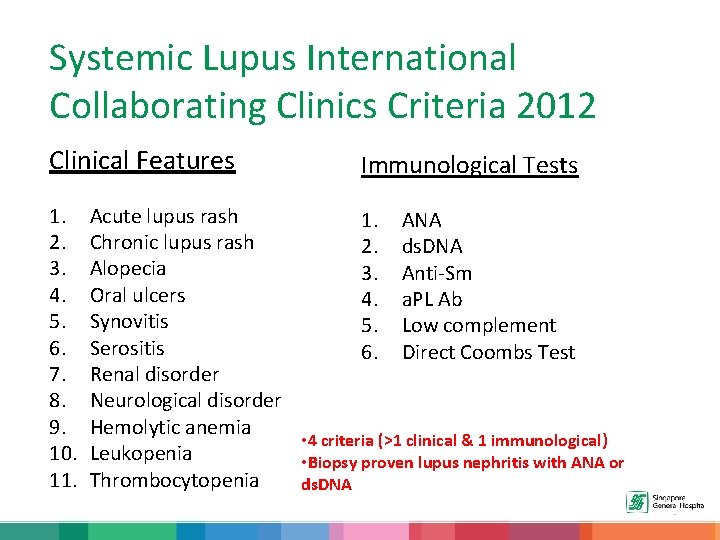
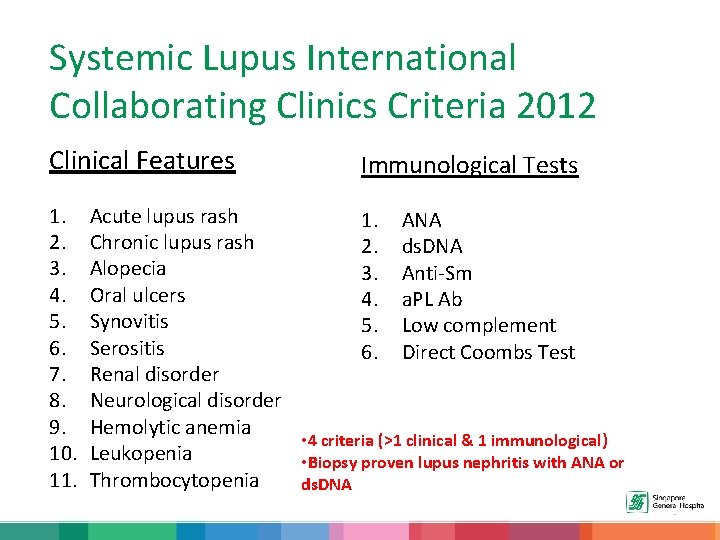
Systemic Lupus International Collaborating Clinics Criteria 2012 Clinical Features 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Immunological Tests Acute lupus rash 1. ANA Chronic lupus rash 2. ds. DNA Alopecia 3. Anti-Sm Oral ulcers 4. a. PL Ab Synovitis 5. Low complement Serositis 6. Direct Coombs Test Renal disorder Neurological disorder Hemolytic anemia • 4 criteria (>1 clinical & 1 immunological) Leukopenia • Biopsy proven lupus nephritis with ANA or Thrombocytopenia ds. DNA
Anti-Phospholipid Syndrome • Antiphospholipid syndrome (APS) is a systemic autoimmune disorder characterized by thrombosis (in veins, arteries and placenta) with evidence of antiphospholipid antibodies (Lupus Anti-Coagulant, Anti-cardiolipin, Anti Beta 2 Glycoprotein 1). • APS occurs as a primary condition, or it can occur in CTDs especially SLE.
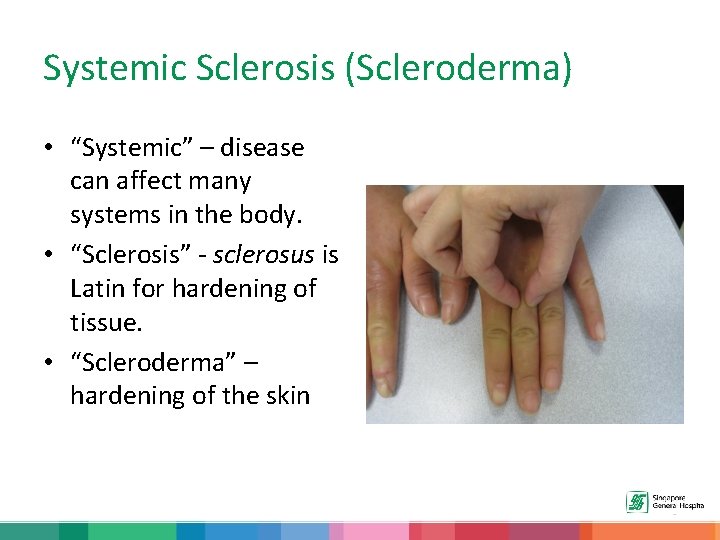
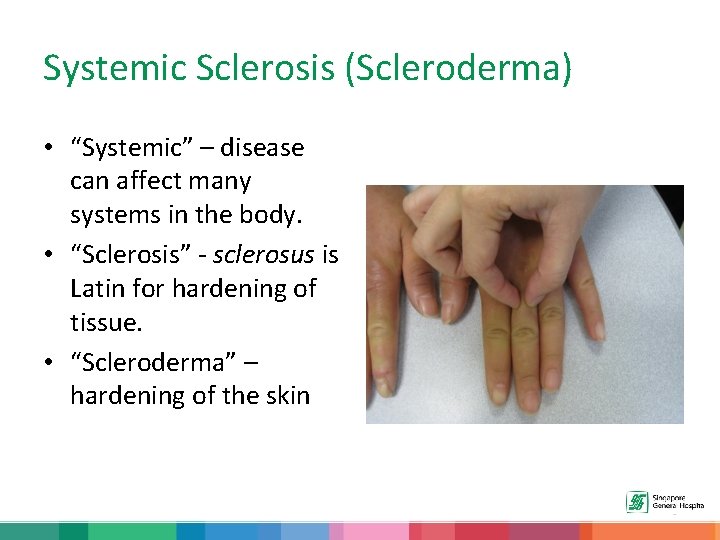
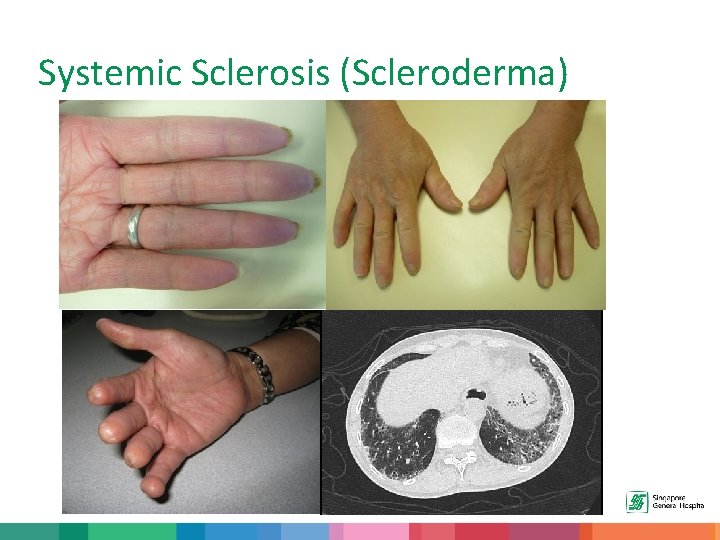
Systemic Sclerosis (Scleroderma) • “Systemic” – disease can affect many systems in the body. • “Sclerosis” - sclerosus is Latin for hardening of tissue. • “Scleroderma” – hardening of the skin
Systemic Sclerosis (Scleroderma) • Systemic Sclerosis is a connective tissue disease characterized by production and deposition of excessive quantities of collagen leading to hardening/fibrosis of the skin. • In addition to fibrosis, these patients have the problem of vasculopathy (Raynaud’s) and of course, inflammation (for example, interstitial lung disease).
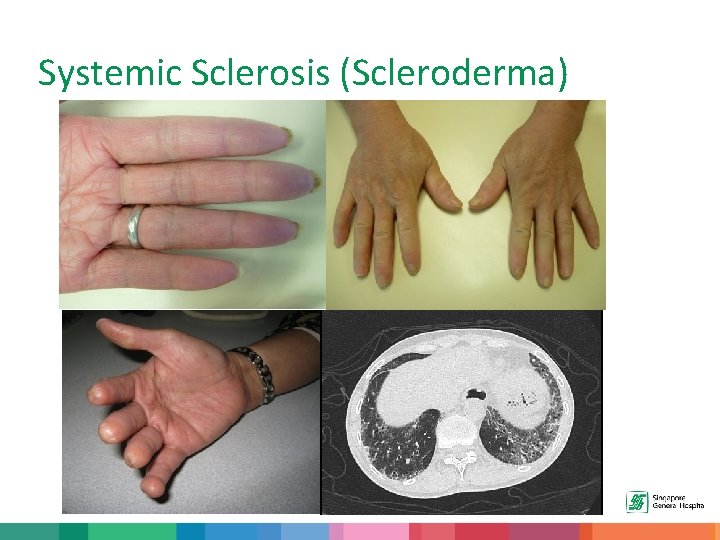
Systemic Sclerosis (Scleroderma)
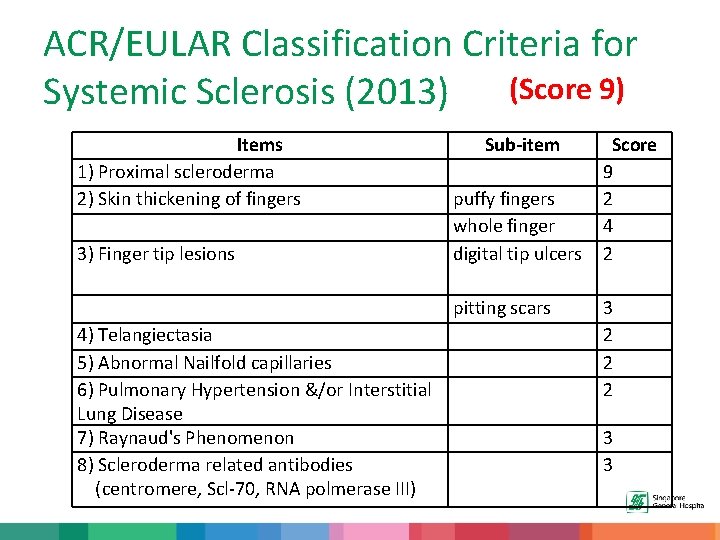
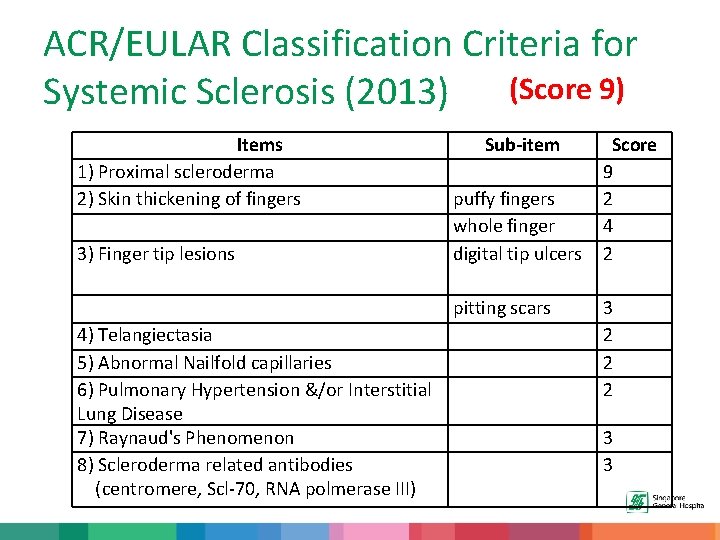
ACR/EULAR Classification Criteria for Systemic Sclerosis (2013) (Score 9) Items 1) Proximal scleroderma 2) Skin thickening of fingers 3) Finger tip lesions Sub-item puffy fingers whole finger digital tip ulcers pitting scars 4) Telangiectasia 5) Abnormal Nailfold capillaries 6) Pulmonary Hypertension &/or Interstitial Lung Disease 7) Raynaud's Phenomenon 8) Scleroderma related antibodies (centromere, Scl-70, RNA polmerase III) Score 9 2 4 2 3 2 2 2 3 3
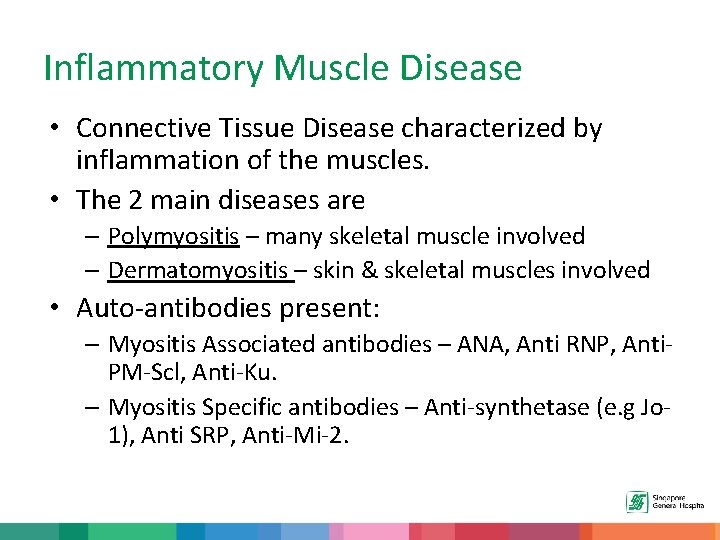
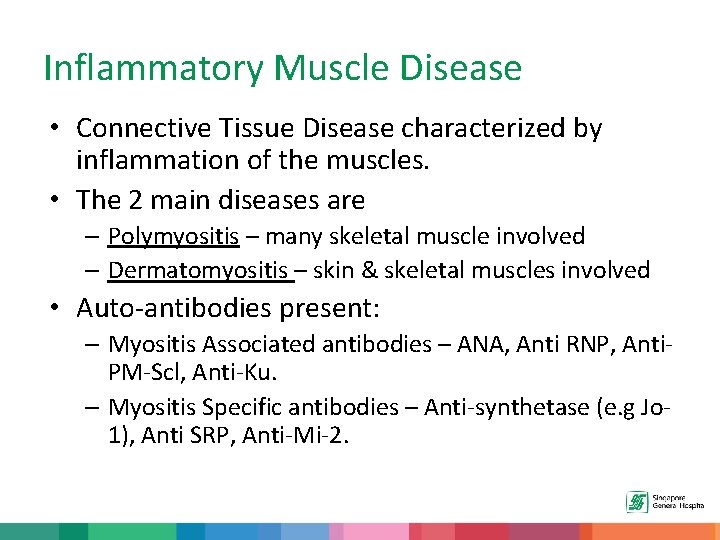
Inflammatory Muscle Disease • Connective Tissue Disease characterized by inflammation of the muscles. • The 2 main diseases are – Polymyositis – many skeletal muscle involved – Dermatomyositis – skin & skeletal muscles involved • Auto-antibodies present: – Myositis Associated antibodies – ANA, Anti RNP, Anti. PM-Scl, Anti-Ku. – Myositis Specific antibodies – Anti-synthetase (e. g Jo 1), Anti SRP, Anti-Mi-2.
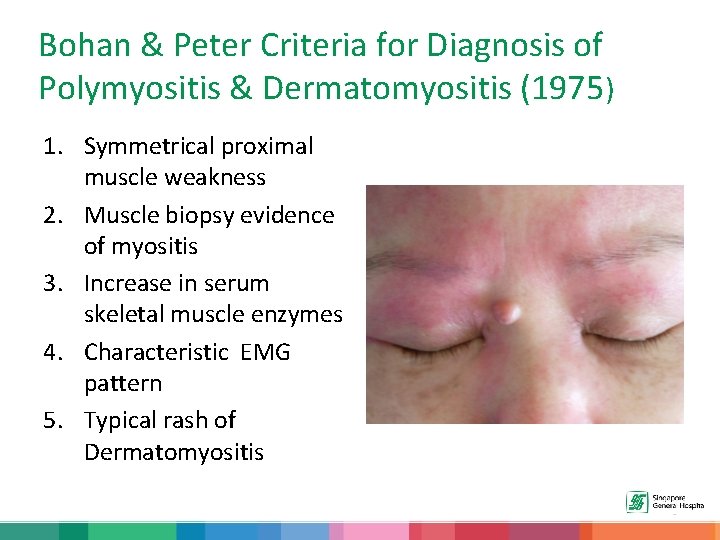
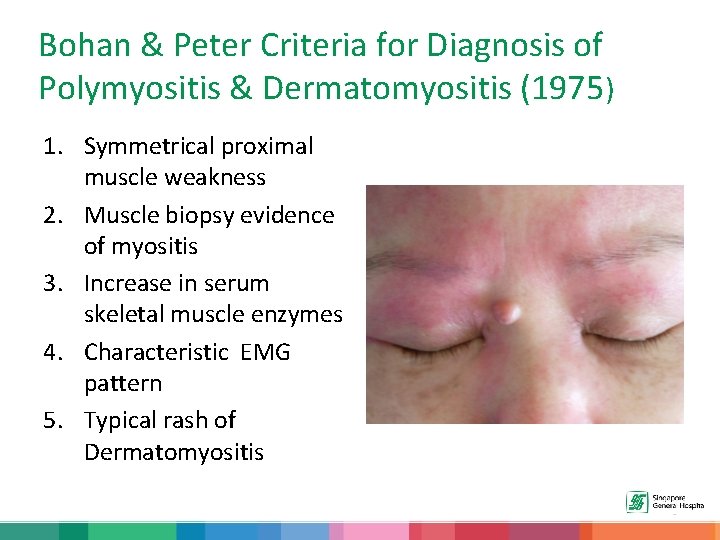
Bohan & Peter Criteria for Diagnosis of Polymyositis & Dermatomyositis (1975) 1. Symmetrical proximal muscle weakness 2. Muscle biopsy evidence of myositis 3. Increase in serum skeletal muscle enzymes 4. Characteristic EMG pattern 5. Typical rash of Dermatomyositis
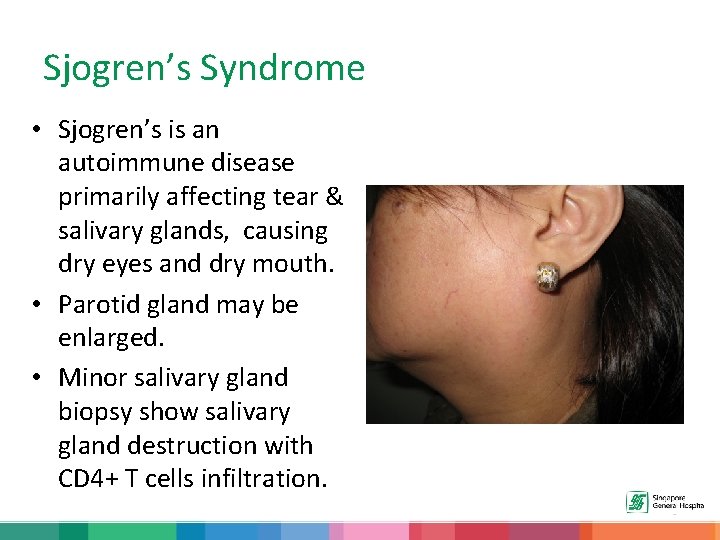
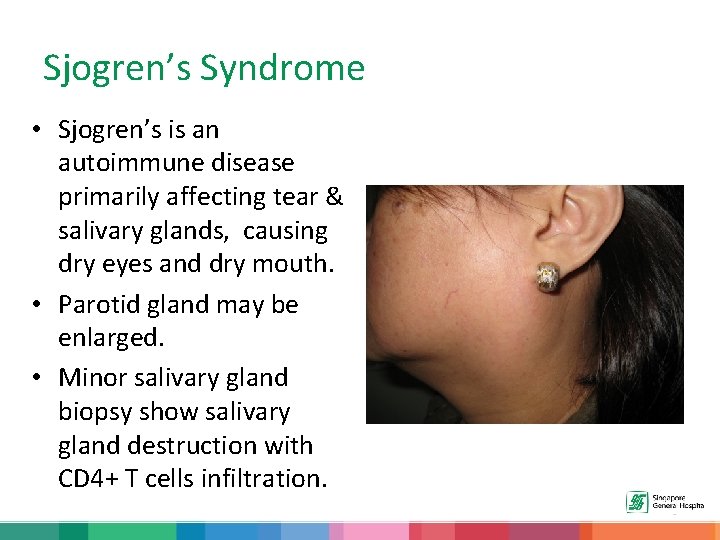
Sjogren’s Syndrome • Sjogren’s is an autoimmune disease primarily affecting tear & salivary glands, causing dry eyes and dry mouth. • Parotid gland may be enlarged. • Minor salivary gland biopsy show salivary gland destruction with CD 4+ T cells infiltration.
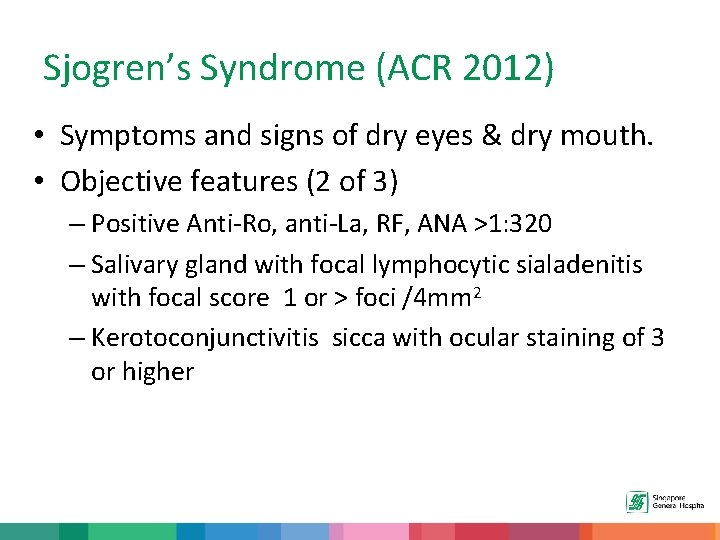
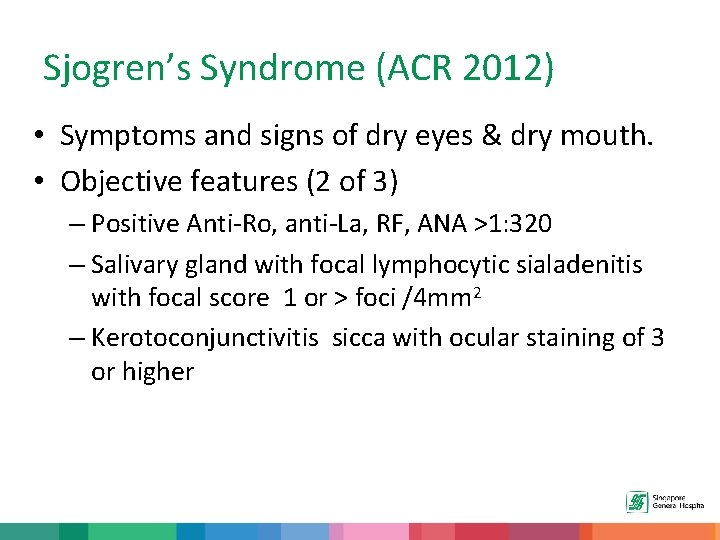
Sjogren’s Syndrome (ACR 2012) • Symptoms and signs of dry eyes & dry mouth. • Objective features (2 of 3) – Positive Anti-Ro, anti-La, RF, ANA >1: 320 – Salivary gland with focal lymphocytic sialadenitis with focal score 1 or > foci /4 mm 2 – Kerotoconjunctivitis sicca with ocular staining of 3 or higher
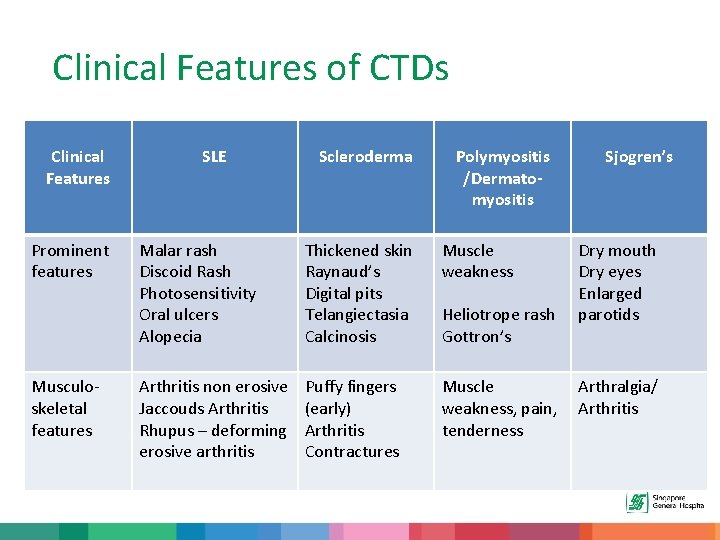
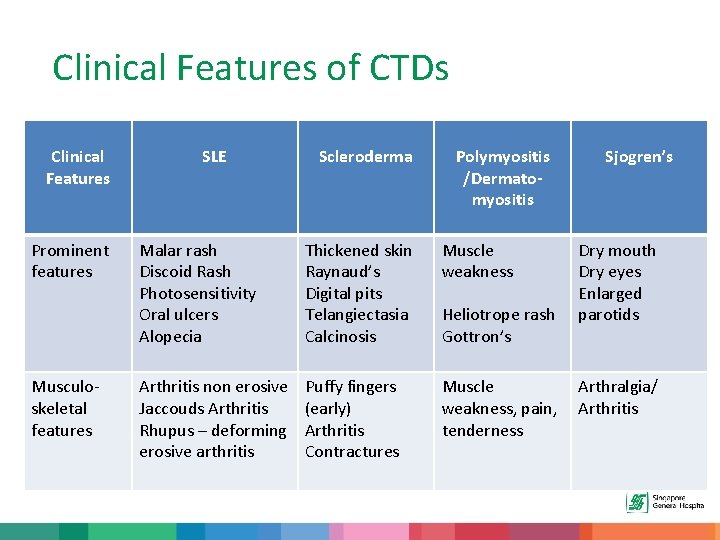
Clinical Features of CTDs Clinical Features Prominent features Musculoskeletal features SLE Scleroderma Polymyositis /Dermatomyositis Malar rash Discoid Rash Photosensitivity Oral ulcers Alopecia Thickened skin Raynaud’s Digital pits Telangiectasia Calcinosis Muscle weakness Arthritis non erosive Jaccouds Arthritis Rhupus – deforming erosive arthritis Puffy fingers (early) Arthritis Contractures Muscle weakness, pain, tenderness Heliotrope rash Gottron’s Sjogren’s Dry mouth Dry eyes Enlarged parotids Arthralgia/ Arthritis
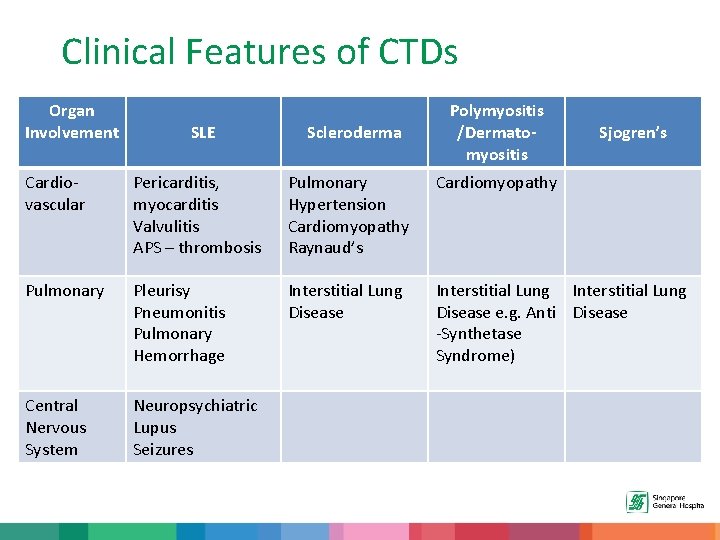
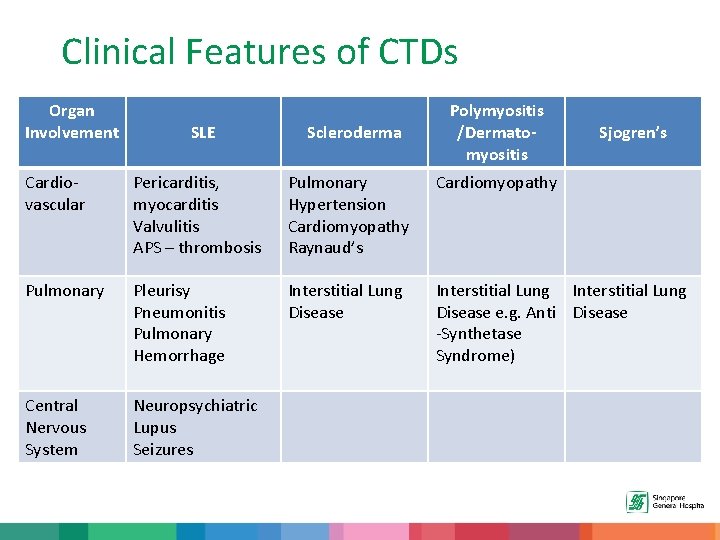
Clinical Features of CTDs Organ Involvement SLE Scleroderma Polymyositis /Dermatomyositis Sjogren’s Cardiovascular Pericarditis, myocarditis Valvulitis APS – thrombosis Pulmonary Hypertension Cardiomyopathy Raynaud’s Cardiomyopathy Pulmonary Pleurisy Pneumonitis Pulmonary Hemorrhage Interstitial Lung Disease e. g. Anti Disease -Synthetase Syndrome) Central Nervous System Neuropsychiatric Lupus Seizures
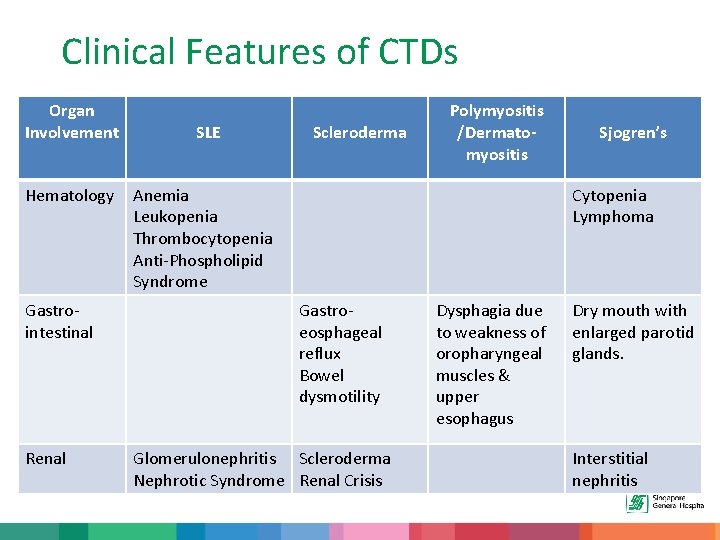
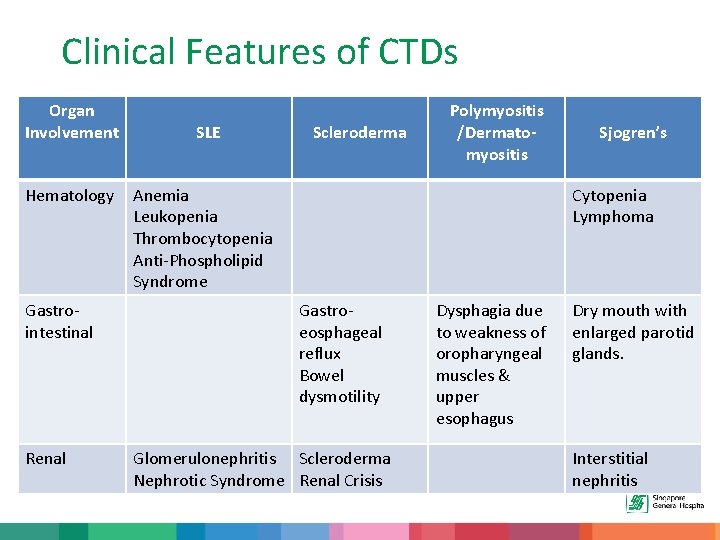
Clinical Features of CTDs Organ Involvement Hematology Gastrointestinal Renal SLE Scleroderma Polymyositis /Dermatomyositis Anemia Leukopenia Thrombocytopenia Anti-Phospholipid Syndrome Sjogren’s Cytopenia Lymphoma Gastroeosphageal reflux Bowel dysmotility Glomerulonephritis Scleroderma Nephrotic Syndrome Renal Crisis Dysphagia due to weakness of oropharyngeal muscles & upper esophagus Dry mouth with enlarged parotid glands. Interstitial nephritis
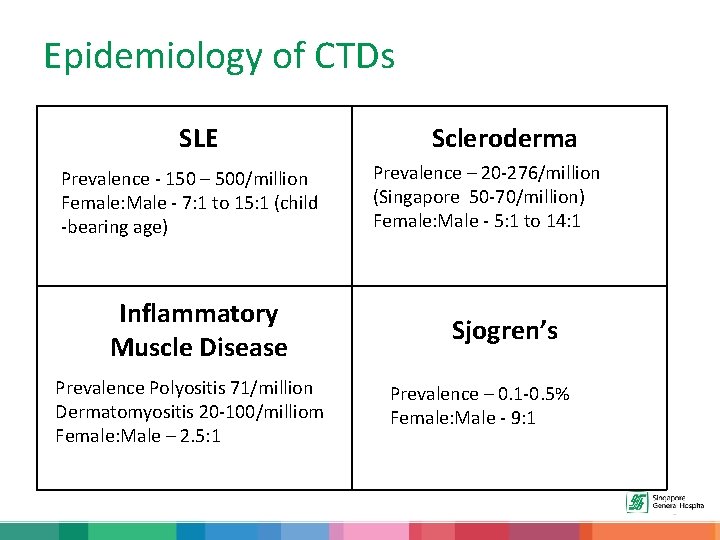
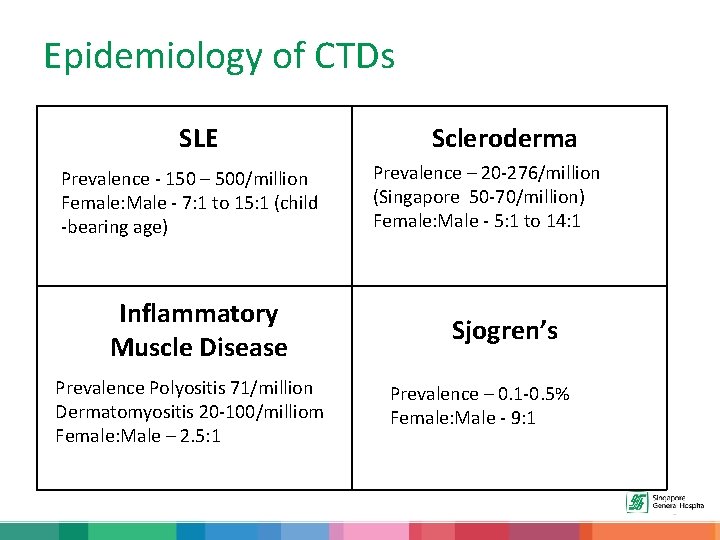
Epidemiology of CTDs SLE Prevalence - 150 – 500/million Female: Male - 7: 1 to 15: 1 (child -bearing age) Inflammatory Muscle Disease Prevalence Polyositis 71/million Dermatomyositis 20 -100/milliom Female: Male – 2. 5: 1 Scleroderma Prevalence – 20 -276/million (Singapore 50 -70/million) Female: Male - 5: 1 to 14: 1 Sjogren’s Prevalence – 0. 1 -0. 5% Female: Male - 9: 1
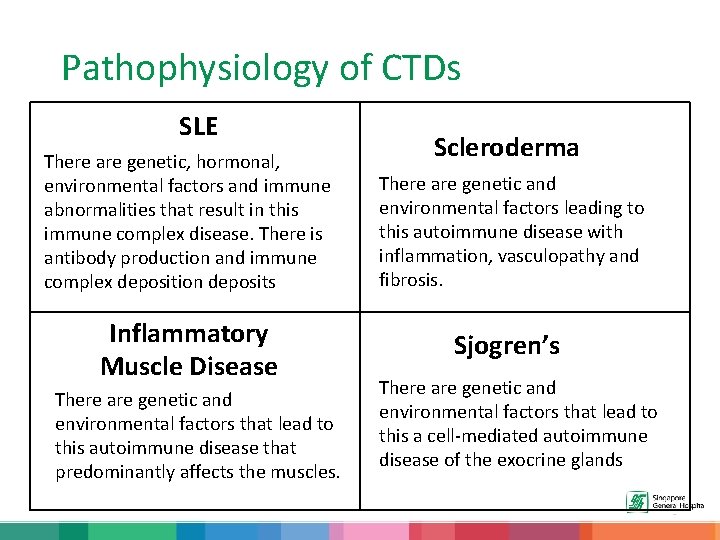
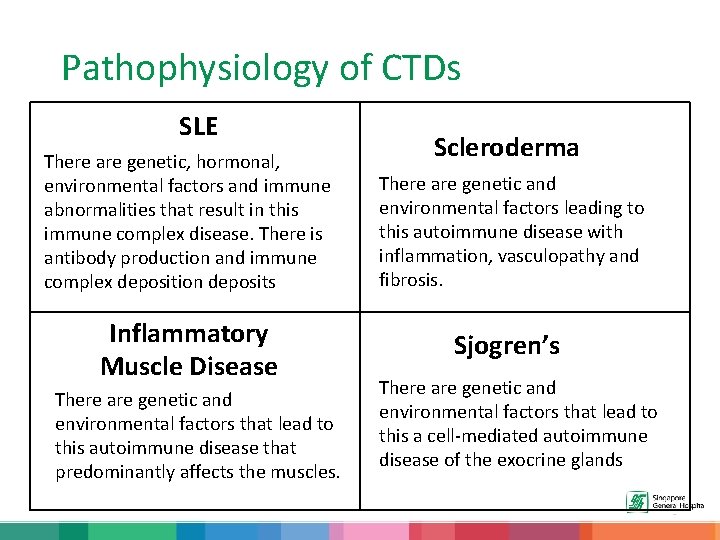
Pathophysiology of CTDs SLE There are genetic, hormonal, environmental factors and immune abnormalities that result in this immune complex disease. There is antibody production and immune complex deposition deposits Inflammatory Muscle Disease There are genetic and environmental factors that lead to this autoimmune disease that predominantly affects the muscles. Scleroderma There are genetic and environmental factors leading to this autoimmune disease with inflammation, vasculopathy and fibrosis. Sjogren’s There are genetic and environmental factors that lead to this a cell-mediated autoimmune disease of the exocrine glands
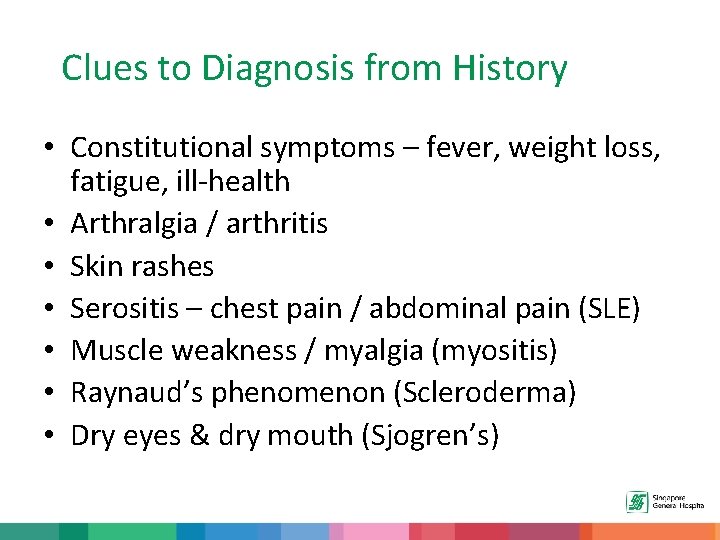
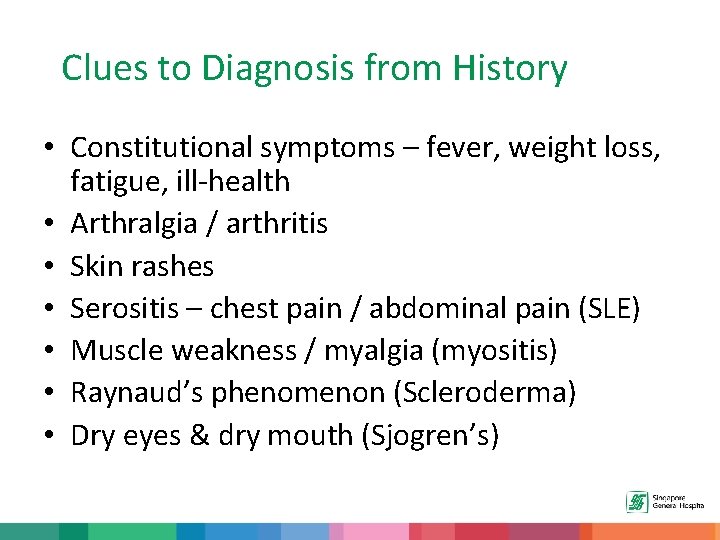
Clues to Diagnosis from History • Constitutional symptoms – fever, weight loss, fatigue, ill-health • Arthralgia / arthritis • Skin rashes • Serositis – chest pain / abdominal pain (SLE) • Muscle weakness / myalgia (myositis) • Raynaud’s phenomenon (Scleroderma) • Dry eyes & dry mouth (Sjogren’s)
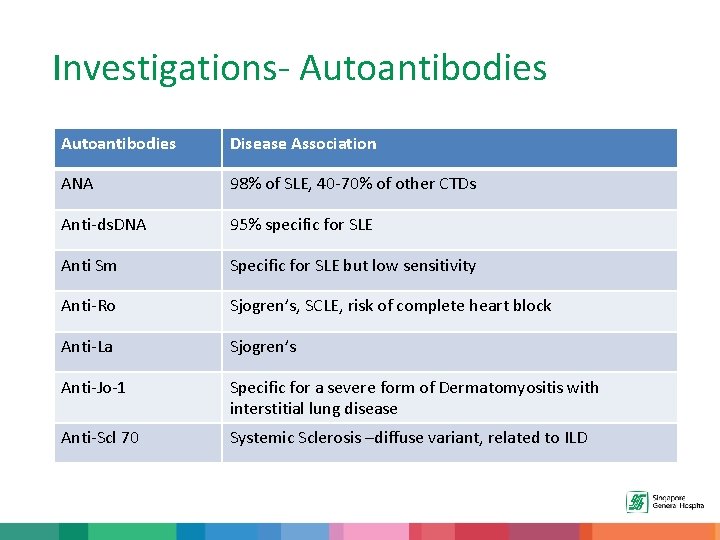
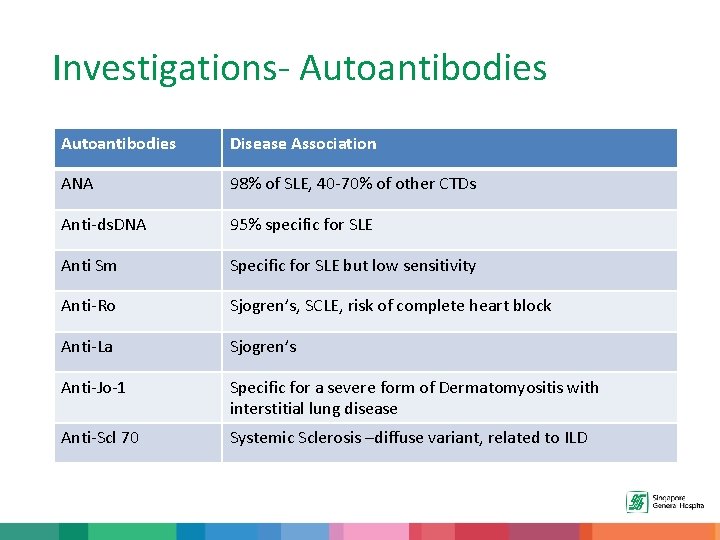
Investigations- Autoantibodies Disease Association ANA 98% of SLE, 40 -70% of other CTDs Anti-ds. DNA 95% specific for SLE Anti Sm Specific for SLE but low sensitivity Anti-Ro Sjogren’s, SCLE, risk of complete heart block Anti-La Sjogren’s Anti-Jo-1 Specific for a severe form of Dermatomyositis with interstitial lung disease Anti-Scl 70 Systemic Sclerosis –diffuse variant, related to ILD
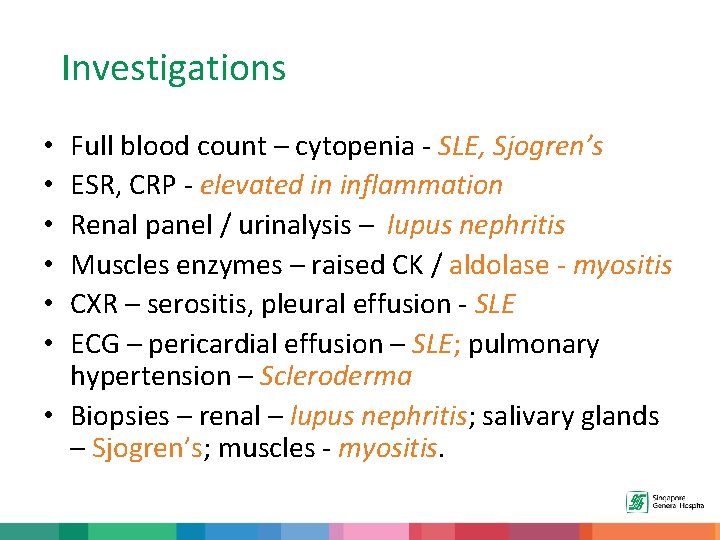
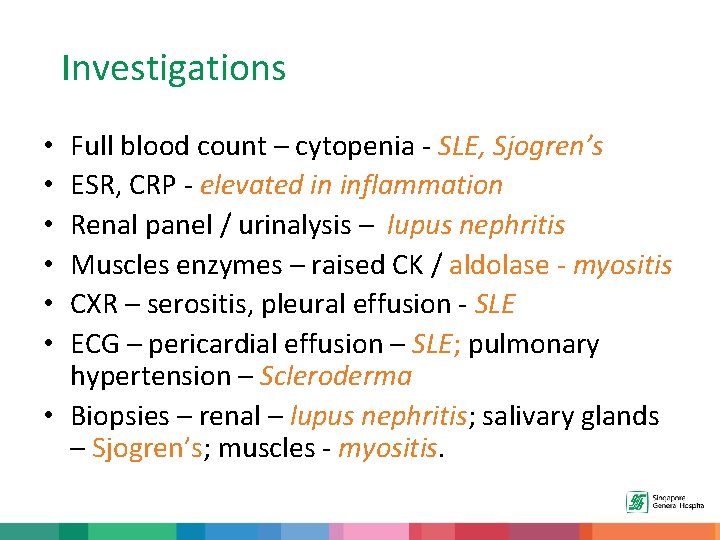
Investigations Full blood count – cytopenia - SLE, Sjogren’s ESR, CRP - elevated in inflammation Renal panel / urinalysis – lupus nephritis Muscles enzymes – raised CK / aldolase - myositis CXR – serositis, pleural effusion - SLE ECG – pericardial effusion – SLE; pulmonary hypertension – Scleroderma • Biopsies – renal – lupus nephritis; salivary glands – Sjogren’s; muscles - myositis. • • •
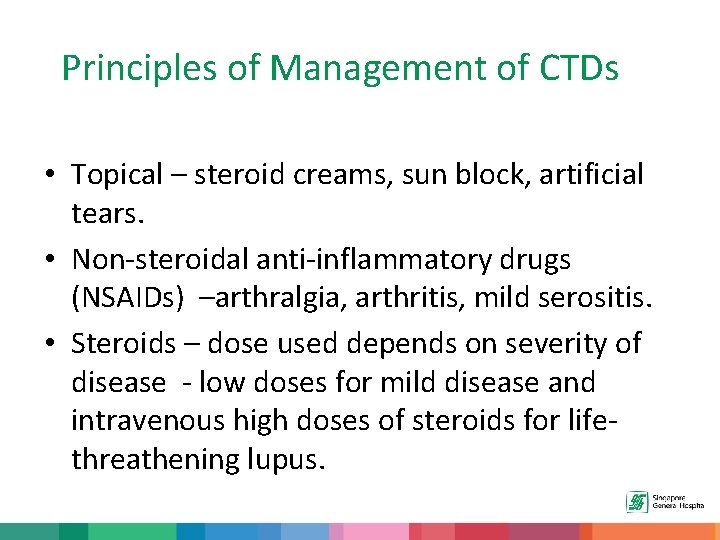
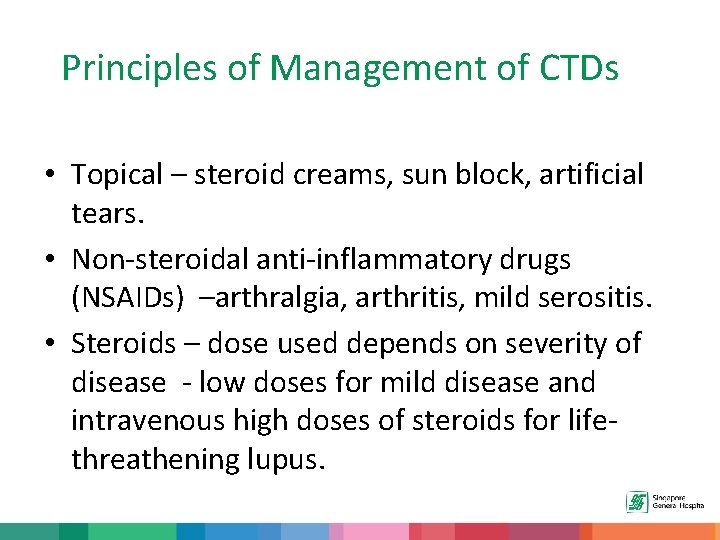
Principles of Management of CTDs • Topical – steroid creams, sun block, artificial tears. • Non-steroidal anti-inflammatory drugs (NSAIDs) –arthralgia, arthritis, mild serositis. • Steroids – dose used depends on severity of disease - low doses for mild disease and intravenous high doses of steroids for lifethreathening lupus.
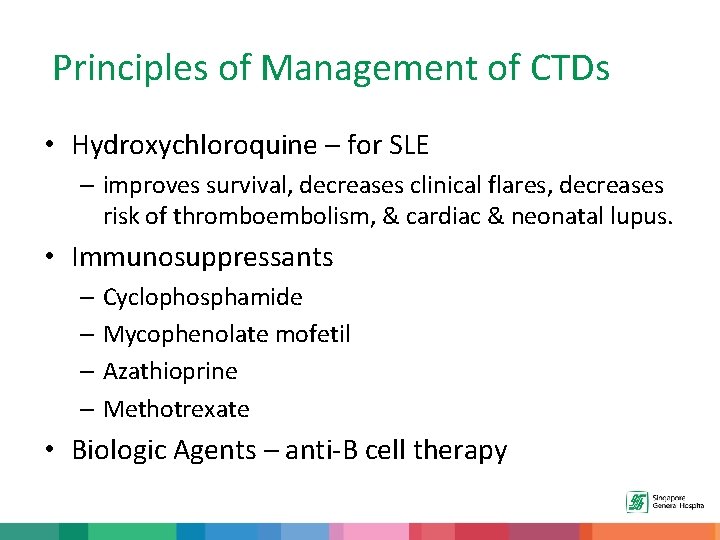
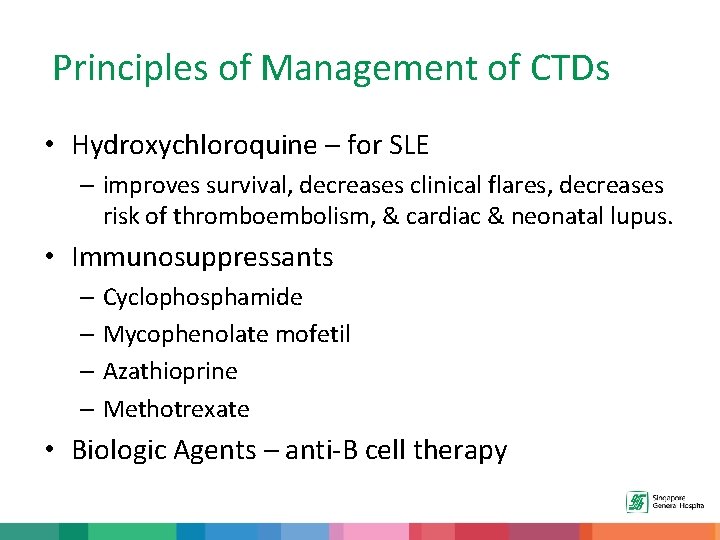
Principles of Management of CTDs • Hydroxychloroquine – for SLE – improves survival, decreases clinical flares, decreases risk of thromboembolism, & cardiac & neonatal lupus. • Immunosuppressants – Cyclophosphamide – Mycophenolate mofetil – Azathioprine – Methotrexate • Biologic Agents – anti-B cell therapy
Summary Checklist 1. 2. 3. 4. 5. 6. What are Connective Tissue Diseases (CTDs). Clinical features of CTDs. Epidemiology and pathophysiology of CTDs. Clues to Diagnosis from History. Investigations. General principles of management. 27
Thank you 28
 Basement membrane
Basement membrane Connective tissue disease adalah
Connective tissue disease adalah Lacunae,
Lacunae, Hyaline cartilage cells
Hyaline cartilage cells Brain soap md
Brain soap md Connective tissue disease adalah
Connective tissue disease adalah Dr ng swee soon
Dr ng swee soon Phang swee kim v beh i hock
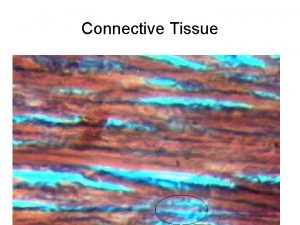
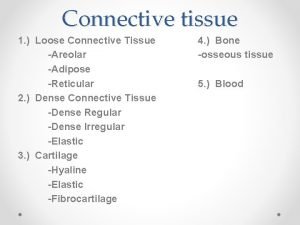
Phang swee kim v beh i hock Dense regular connective tissue tendon
Dense regular connective tissue tendon Dense irregular connective tissue description
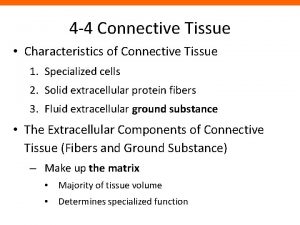
Dense irregular connective tissue description Connective tissue lab practical
Connective tissue lab practical Specialized connective tissue blood
Specialized connective tissue blood Dense irregular connective tissue
Dense irregular connective tissue Reticular connective tissue
Reticular connective tissue Tissue types in the body
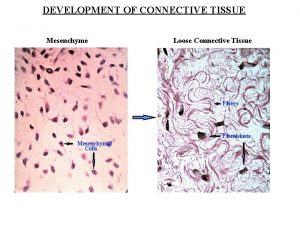
Tissue types in the body Embryonic connective tissue
Embryonic connective tissue Identify the cells
Identify the cells Dense regular connective
Dense regular connective Cells and fibres of connective tissue
Cells and fibres of connective tissue Yellow fibrous connective tissue
Yellow fibrous connective tissue Connective
Connective Bone marrow connective tissue
Bone marrow connective tissue Connective tissue oncology society
Connective tissue oncology society Histology smooth muscle
Histology smooth muscle Goblet cell
Goblet cell Reticular fibers definition
Reticular fibers definition Spinal cord
Spinal cord What type of connective tissue are tendons and ligaments
What type of connective tissue are tendons and ligaments Specialised connective tissue
Specialised connective tissue