Online Personalised Care maternity and early years QIPP






![§ [Slide Removed] 04/06/2021 45 § [Slide Removed] 04/06/2021 45](https://slidetodoc.com/presentation_image_h2/56548a1d0ea897863d915ff22498d9ec/image-44.jpg)
- Slides: 44

Online Personalised Care - maternity and early years QIPP Digital and Technology Vision work stream - National Candidate 1 a April 2011 V 1. 0 (redacted version)
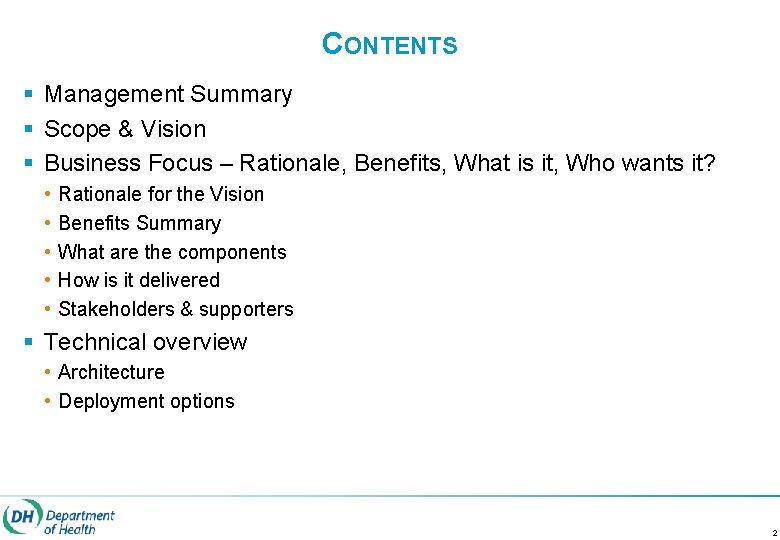
CONTENTS § Management Summary § Scope & Vision § Business Focus – Rationale, Benefits, What is it, Who wants it? • • • Rationale for the Vision Benefits Summary What are the components How is it delivered Stakeholders & supporters § Technical overview • Architecture • Deployment options 2

Management Summary
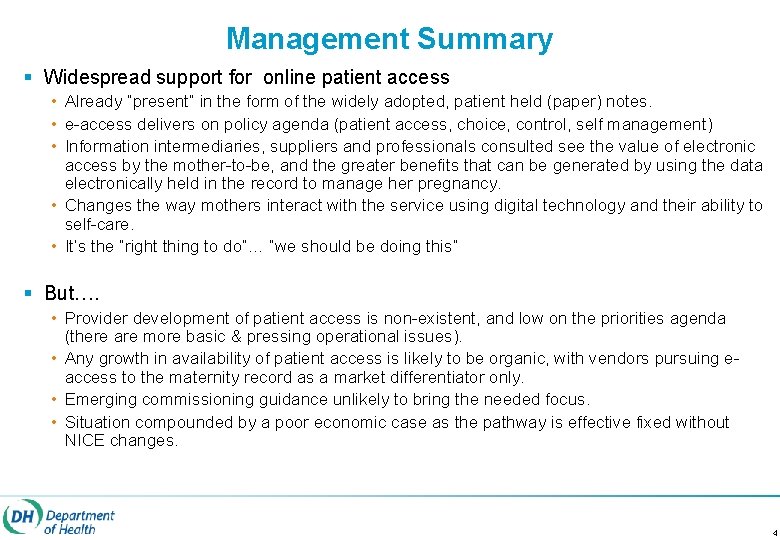
Management Summary § Widespread support for online patient access • Already “present” in the form of the widely adopted, patient held (paper) notes. • e-access delivers on policy agenda (patient access, choice, control, self management) • Information intermediaries, suppliers and professionals consulted see the value of electronic access by the mother-to-be, and the greater benefits that can be generated by using the data electronically held in the record to manage her pregnancy. • Changes the way mothers interact with the service using digital technology and their ability to self-care. • It’s the “right thing to do”… “we should be doing this” § But…. • Provider development of patient access is non-existent, and low on the priorities agenda (there are more basic & pressing operational issues). • Any growth in availability of patient access is likely to be organic, with vendors pursuing eaccess to the maternity record as a market differentiator only. • Emerging commissioning guidance unlikely to bring the needed focus. • Situation compounded by a poor economic case as the pathway is effective fixed without NICE changes. 4
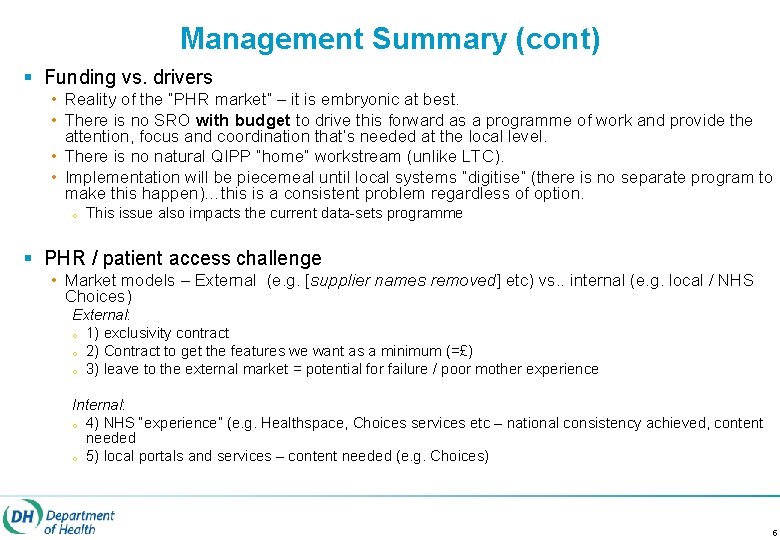
Management Summary (cont) § Funding vs. drivers • Reality of the “PHR market” – it is embryonic at best. • There is no SRO with budget to drive this forward as a programme of work and provide the attention, focus and coordination that’s needed at the local level. • There is no natural QIPP “home” workstream (unlike LTC). • Implementation will be piecemeal until local systems “digitise” (there is no separate program to make this happen)…this is a consistent problem regardless of option. o This issue also impacts the current data-sets programme § PHR / patient access challenge • Market models – External (e. g. [supplier names removed] etc) vs. . internal (e. g. local / NHS Choices) External: o 1) exclusivity contract o 2) Contract to get the features we want as a minimum (=£) o 3) leave to the external market = potential for failure / poor mother experience Internal: o 4) NHS “experience” (e. g. Healthspace, Choices services etc – national consistency achieved, content needed o 5) local portals and services – content needed (e. g. Choices) 5
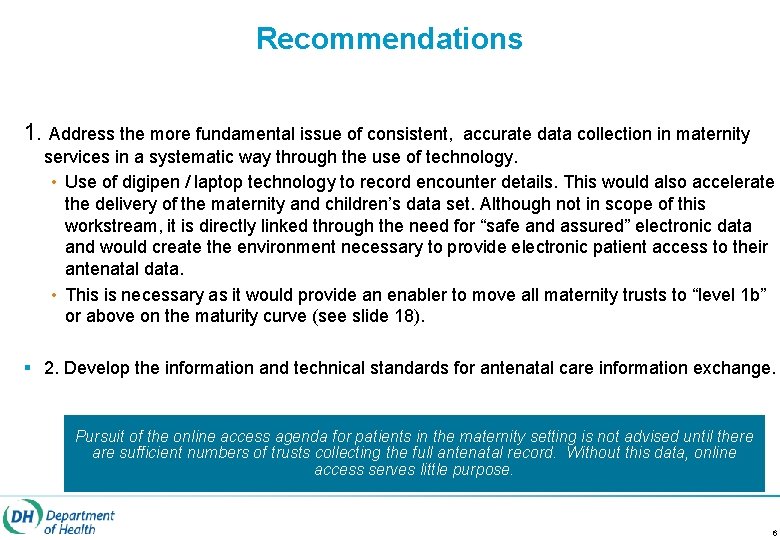
Recommendations 1. Address the more fundamental issue of consistent, accurate data collection in maternity services in a systematic way through the use of technology. • Use of digipen / laptop technology to record encounter details. This would also accelerate the delivery of the maternity and children’s data set. Although not in scope of this workstream, it is directly linked through the need for “safe and assured” electronic data and would create the environment necessary to provide electronic patient access to their antenatal data. • This is necessary as it would provide an enabler to move all maternity trusts to “level 1 b” or above on the maturity curve (see slide 18). § 2. Develop the information and technical standards for antenatal care information exchange. Pursuit of the online access agenda for patients in the maternity setting is not advised until there are sufficient numbers of trusts collecting the full antenatal record. Without this data, online access serves little purpose. 6

Scope and Vision
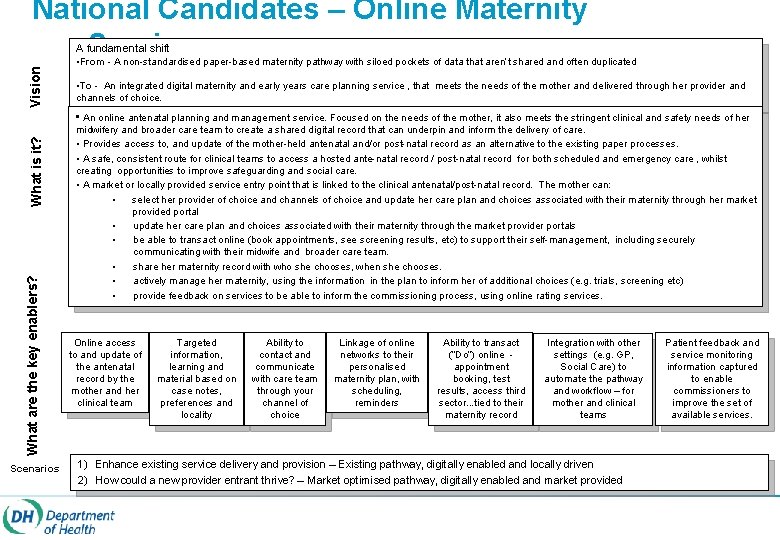
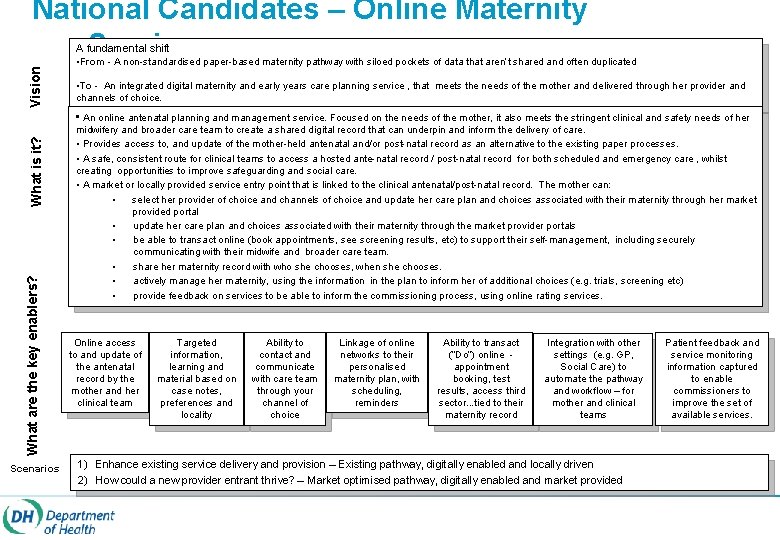
Vision National Candidates – Online Maternity Service A fundamental shift • From - A non-standardised paper-based maternity pathway with siloed pockets of data that aren’t shared and often duplicated • To - An integrated digital maternity and early years care planning service , that meets the needs of the mother and delivered through her provider and channels of choice. What are the key enablers? What is it? • An online antenatal planning and management service. Focused on the needs of the mother, it also meets the stringent clinical and safety needs of her Scenarios midwifery and broader care team to create a shared digital record that can underpin and inform the delivery of care. • Provides access to, and update of the mother-held antenatal and/or post-natal record as an alternative to the existing paper processes. • A safe, consistent route for clinical teams to access a hosted ante-natal record / post-natal record for both scheduled and emergency care , whilst creating opportunities to improve safeguarding and social care. • A market or locally provided service entry point that is linked to the clinical antenatal/post-natal record. The mother can: • select her provider of choice and channels of choice and update her care plan and choices associated with their maternity through her market provided portal • update her care plan and choices associated with their maternity through the market provider portals • be able to transact online (book appointments, see screening results, etc) to support their self-management, including securely communicating with their midwife and broader care team. • share her maternity record with who she chooses, when she chooses. • actively manage her maternity, using the information in the plan to inform her of additional choices (e. g. trials, screening etc) • provide feedback on services to be able to inform the commissioning process, using online rating services. Online access to and update of the antenatal record by the mother and her clinical team Targeted information, learning and material based on case notes, preferences and locality Ability to contact and communicate with care team through your channel of choice Linkage of online networks to their personalised maternity plan, with scheduling, reminders Ability to transact (“Do”) online appointment booking, test results, access third sector. . . tied to their maternity record Integration with other settings (e. g. GP, Social Care) to automate the pathway and workflow – for mother and clinical teams 1) Enhance existing service delivery and provision – Existing pathway, digitally enabled and locally driven 2) How could a new provider entrant thrive? – Market optimised pathway, digitally enabled and market provided Patient feedback and service monitoring information captured to enable commissioners to improve the set of available services.
Scope Summary § Enablement of patient access to an electronic version of their antenatal record. § Market and / or NHS (locally) provided access to the record by the mother-to-be, with the means to share the information with settings and organisations who are not part of the local community of interest. § The record will be populated from the data held within the antenatal notes as captured (in the same way as they are on paper – but recognising the sensitivity of some aspects such as social and domestic information) and shared with the mother via her access “portal”. § The service would operate on an “opt-in” basis by the mother, who would be advised of the availability by the clinical team / midwife at either first contact or the booking appointment. § The booking appointment could be used as an opportunity to assure the patient identity (in order to provide online access). Ideally patient identity would be aligned to the cross-government Identity Assurance approach (IDA). § Transactional services such as appointment booking (rather than “requesting” an appointment) would still be reliant on the capabilities of the local systems that control booking / scheduling – NHS or otherwise. 9
Business Focus – Rationale, Benefits, What is it, Who wants it? 10
Rationale for the Proposition – Why the focus on Maternity? § Maternity care is one of the most “personal” of care experiences and most emotional interactions a patient will have with the NHS. § Mothers are generally keen to engage and participate in their self-management and that of their unborn child, as has been demonstrated through the success of antenatal notes used by expecting mothers. § The age profile of mothers-to-be generally puts them in a group who are both familiar with digital technology, and readily incorporate it in to their daily lives. For excluded or at-risk groups, it can be a preferred mechanism. § There approximately 30000 midwives in England, managing ~650000 maternities per annum (ONS). Of those maternities, 42% of mothers used non-NHS online tools and websites to support them during their pregnancy and the early years of their child (NPEU). § Antenatal care generates very large amounts of paper and repetitive keying or notes between systems. The use of paper, and after the fact recording creates clinical safety issues and breaks in the pathway that can impact the health and well being of the mother and her child. Maternity services provides a target user group of mothers who are both willing and able to use digital technology in the delivery of their care, and broader management of their pregnancy. The digital service will provide an additional channel rather than be a complete replacement for existing support and management channels 11
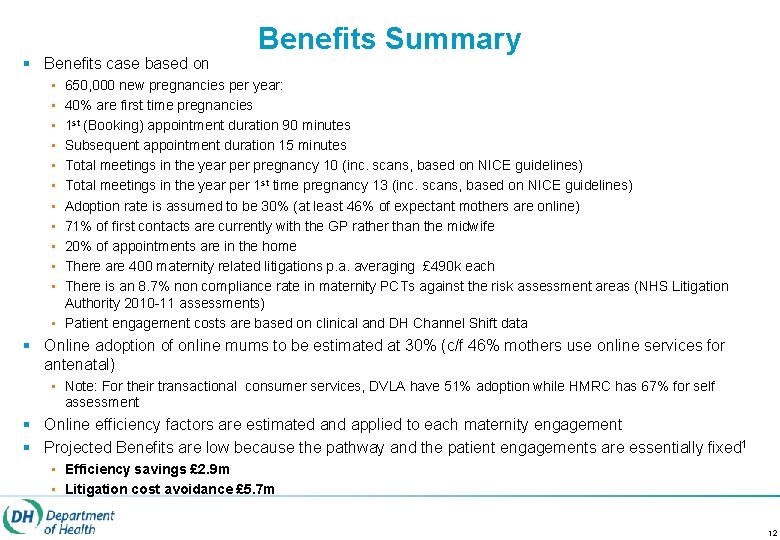
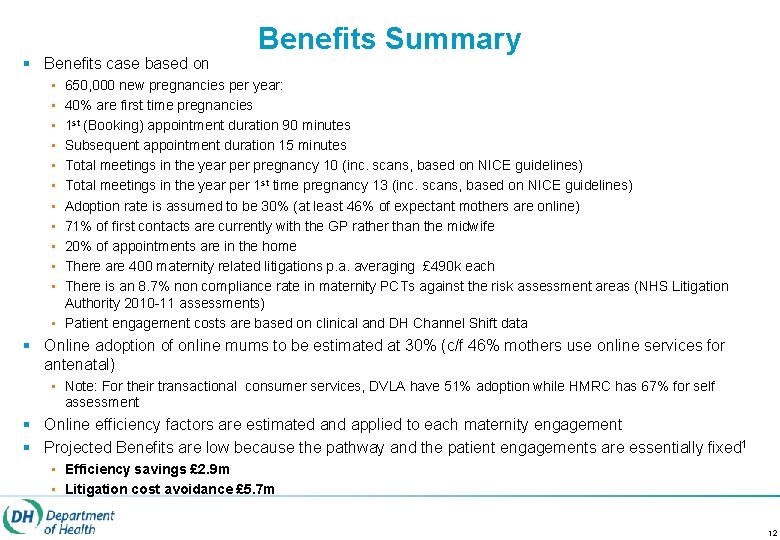
§ Benefits case based on Benefits Summary • • • 650, 000 new pregnancies per year: 40% are first time pregnancies 1 st (Booking) appointment duration 90 minutes Subsequent appointment duration 15 minutes Total meetings in the year per pregnancy 10 (inc. scans, based on NICE guidelines) Total meetings in the year per 1 st time pregnancy 13 (inc. scans, based on NICE guidelines) Adoption rate is assumed to be 30% (at least 46% of expectant mothers are online) 71% of first contacts are currently with the GP rather than the midwife 20% of appointments are in the home There are 400 maternity related litigations p. a. averaging £ 490 k each There is an 8. 7% non compliance rate in maternity PCTs against the risk assessment areas (NHS Litigation Authority 2010 -11 assessments) • Patient engagement costs are based on clinical and DH Channel Shift data § Online adoption of online mums to be estimated at 30% (c/f 46% mothers use online services for antenatal) • Note: For their transactional consumer services, DVLA have 51% adoption while HMRC has 67% for self assessment § Online efficiency factors are estimated and applied to each maternity engagement § Projected Benefits are low because the pathway and the patient engagements are essentially fixed 1 • Efficiency savings £ 2. 9 m • Litigation cost avoidance £ 5. 7 m 12
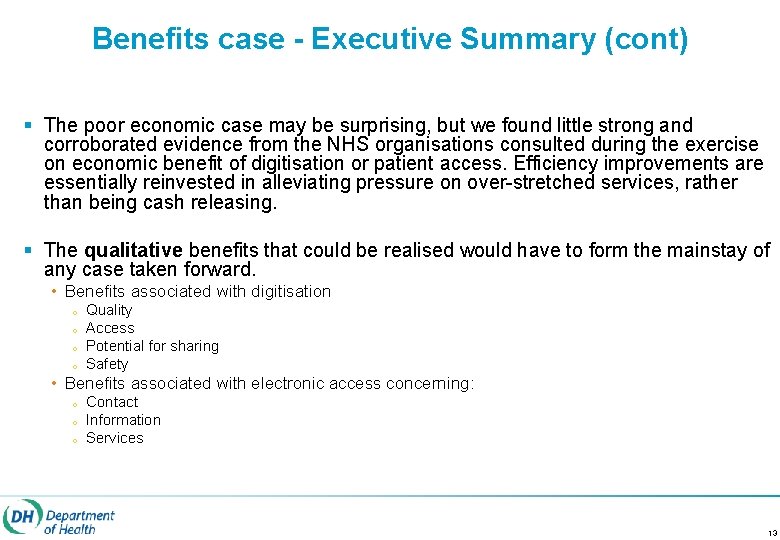
Benefits case - Executive Summary (cont) § The poor economic case may be surprising, but we found little strong and corroborated evidence from the NHS organisations consulted during the exercise on economic benefit of digitisation or patient access. Efficiency improvements are essentially reinvested in alleviating pressure on over-stretched services, rather than being cash releasing. § The qualitative benefits that could be realised would have to form the mainstay of any case taken forward. • Benefits associated with digitisation o o Quality Access Potential for sharing Safety • Benefits associated with electronic access concerning: o o o Contact Information Services 13
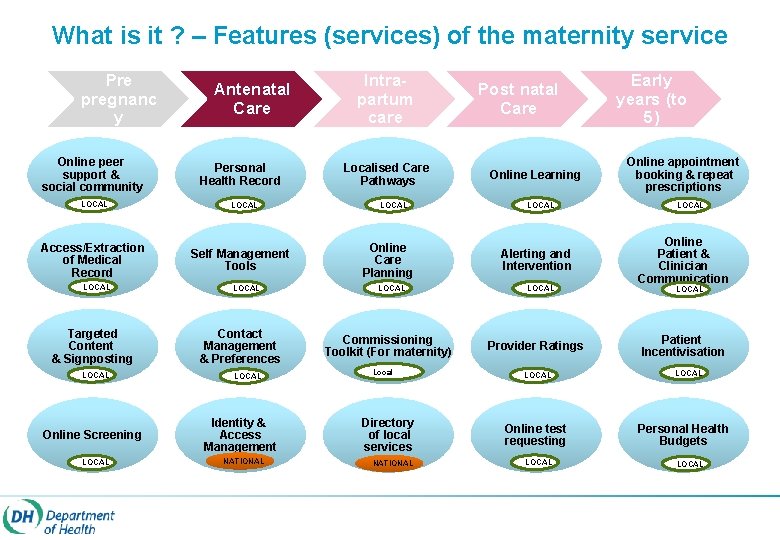
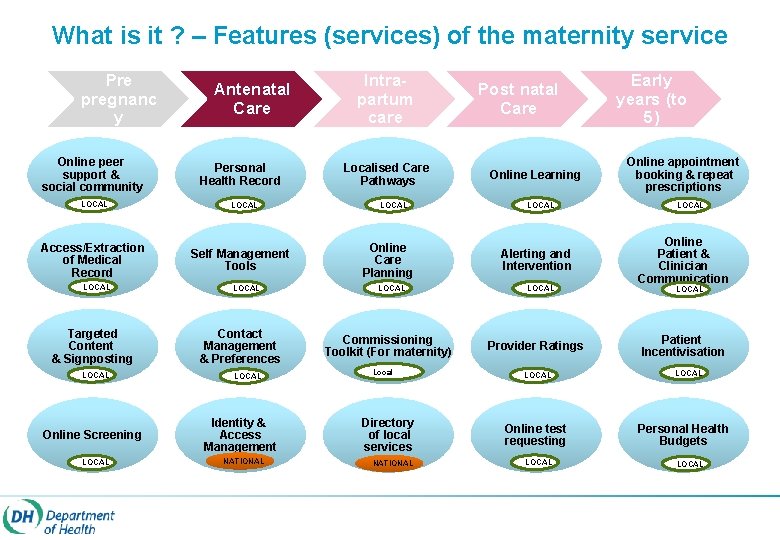
What is it ? – Features (services) of the maternity service Pre pregnanc y Online peer support & social community LOCAL Access/Extraction of Medical Record LOCAL Targeted Content & Signposting LOCAL Online Screening LOCAL Antenatal Care Personal Health Record LOCAL Self Management Tools LOCAL Contact Management & Preferences LOCAL Identity & Access Management NATIONAL Intrapartum care Localised Care Pathways LOCAL Online Care Planning LOCAL Commissioning Toolkit (For maternity) Local Directory of local services NATIONAL Post natal Care Online Learning LOCAL Alerting and Intervention LOCAL Provider Ratings LOCAL Online test requesting LOCAL Early years (to 5) Online appointment booking & repeat prescriptions LOCAL Online Patient & Clinician Communication LOCAL Patient Incentivisation LOCAL Personal Health Budgets LOCAL
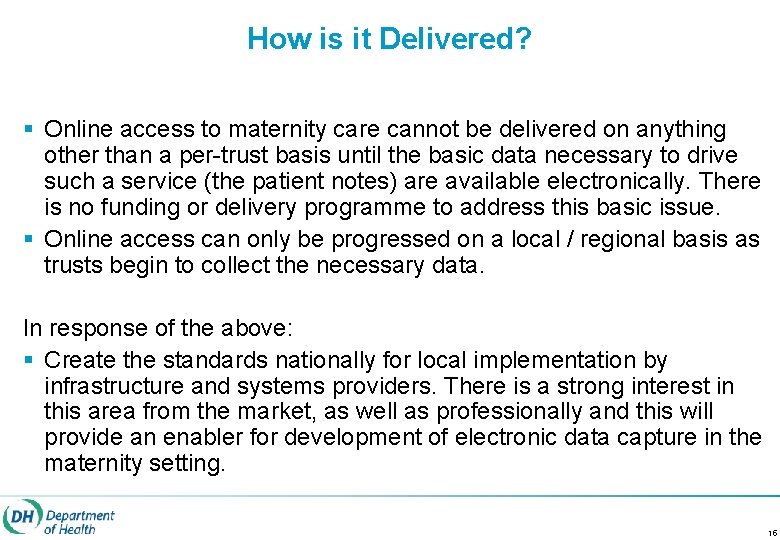
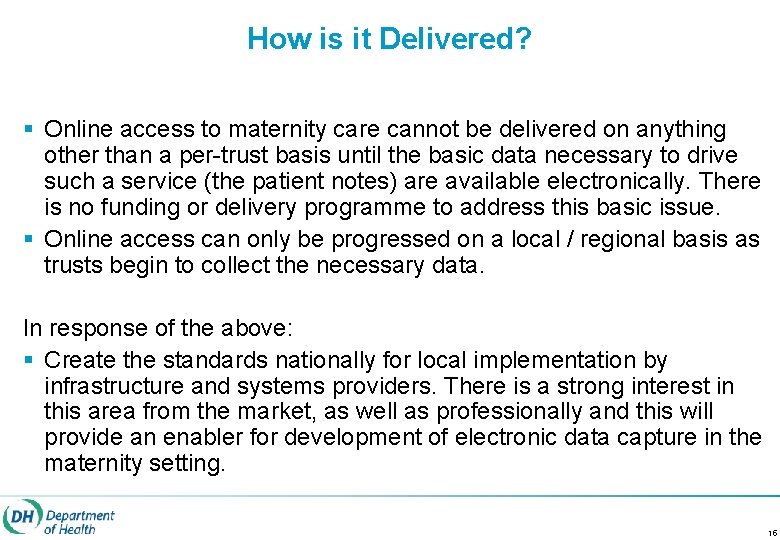
How is it Delivered? § Online access to maternity care cannot be delivered on anything other than a per-trust basis until the basic data necessary to drive such a service (the patient notes) are available electronically. There is no funding or delivery programme to address this basic issue. § Online access can only be progressed on a local / regional basis as trusts begin to collect the necessary data. In response of the above: § Create the standards nationally for local implementation by infrastructure and systems providers. There is a strong interest in this area from the market, as well as professionally and this will provide an enabler for development of electronic data capture in the maternity setting. 15
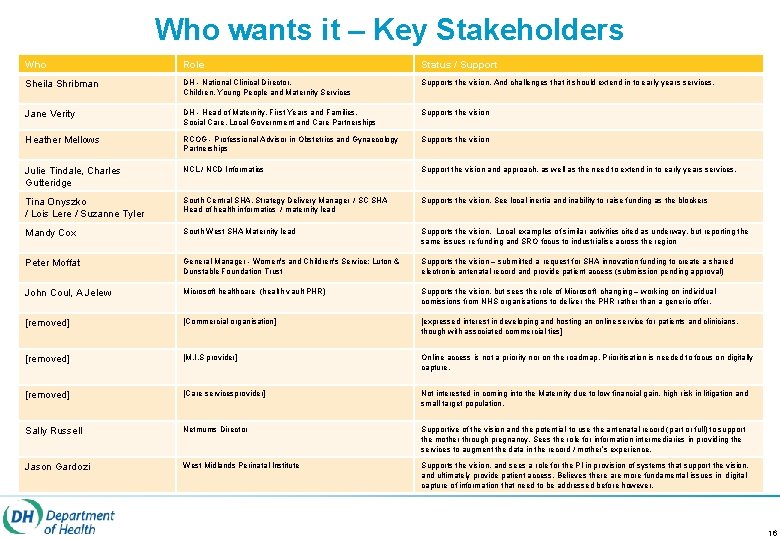
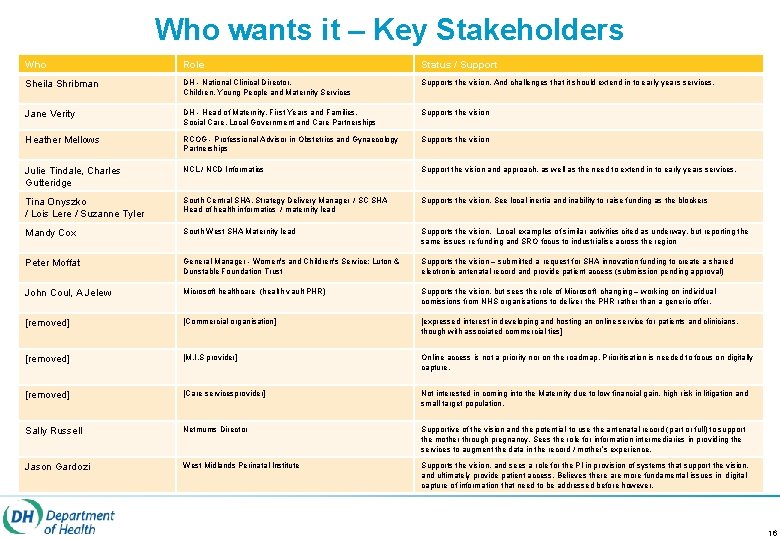
Who wants it – Key Stakeholders Who Role Status / Support Sheila Shribman DH - National Clinical Director, Children, Young People and Maternity Services Supports the vision. And challenges that it should extend in to early years services. Jane Verity DH - Head of Maternity, First Years and Families, Social Care, Local Government and Care Partnerships Supports the vision Heather Mellows RCOG - Professional Advisor in Obstetrics and Gynaecology Partnerships Supports the vision Julie Tindale, Charles Gutteridge NCL / NCD Informatics Support the vision and approach, as well as the need to extend in to early years services. Tina Onyszko / Lois Lere / Suzanne Tyler South Central SHA, Strategy Delivery Manager / SC SHA Head of health informatics / maternity lead Supports the vision. See local inertia and inability to raise funding as the blockers Mandy Cox South West SHA Maternity lead Supports the vision. Local examples of similar activities cited as underway, but reporting the same issues re funding and SRO focus to industrialise across the region Peter Moffat General Manager - Women's and Children's Service; Luton & Dunstable Foundation Trust Supports the vision – submitted a request for SHA innovation funding to create a shared electronic antenatal record and provide patient access (submission pending approval) John Coul, A Jelew Microsoft healthcare (health vault PHR) Supports the vision, but sees the role of Microsoft changing – working on individual comissions from NHS organisations to deliver the PHR rather than a generic offer. [removed] [Commercial organisation] [expressed interest in developing and hosting an online service for patients and clinicians, though with associated commercial ties] [removed] [M. I. S provider] Online access is not a priority nor on the roadmap. Prioritisation is needed to focus on digitally capture. [removed] [Care servicesprovider] Not interested in coming into the Maternity due to low financial gain, high risk in litigation and small target population. Sally Russell Netmums Director Supportive of the vision and the potential to use the antenatal record (part or full) to support the mother through pregnancy. Sees the role for information intermediaries in providing the services to augment the data in the record / mother’s experience. Jason Gardozi West Midlands Perinatal Institute Supports the vision, and sees a role for the PI in provision of systems that support the vision, and ultimately provide patient access. Believes there are more fundamental issues in digital capture of information that need to be addressed before however. 16
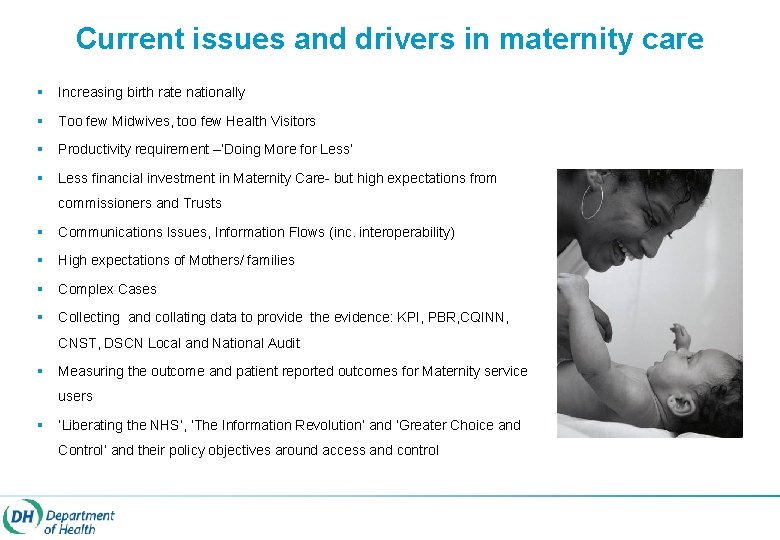
Current issues and drivers in maternity care § Increasing birth rate nationally § Too few Midwives, too few Health Visitors § Productivity requirement –’Doing More for Less’ § Less financial investment in Maternity Care- but high expectations from commissioners and Trusts § Communications Issues, Information Flows (inc. interoperability) § High expectations of Mothers/ families § Complex Cases § Collecting and collating data to provide the evidence: KPI, PBR, CQINN, CNST, DSCN Local and National Audit § Measuring the outcome and patient reported outcomes for Maternity service users § ‘Liberating the NHS’, ‘The Information Revolution’ and ‘Greater Choice and Control‘ and their policy objectives around access and control
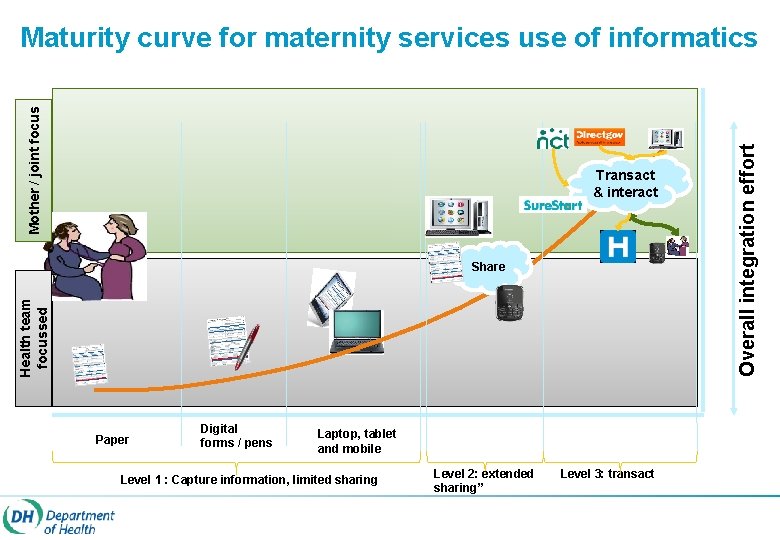
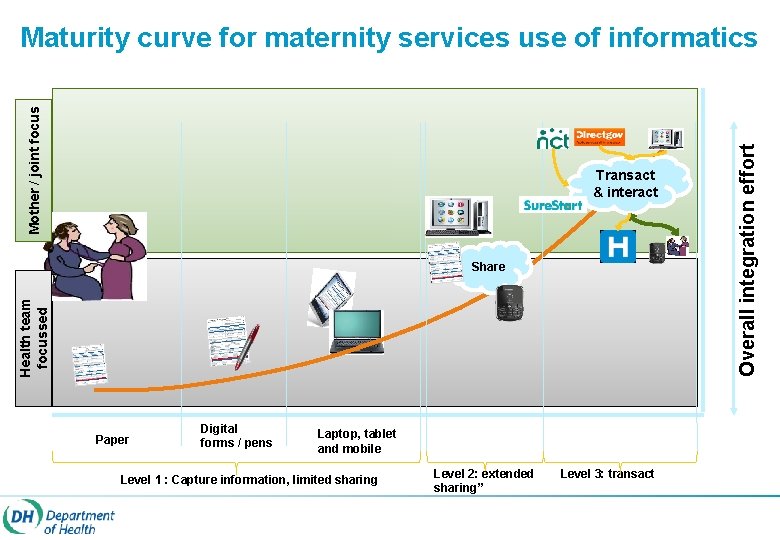
Transact & interact Health team focussed Share Paper Digital forms / pens Laptop, tablet and mobile Level 1 : Capture information, limited sharing Level 2: extended sharing” Level 3: transact Overall integration effort Mother / joint focus Maturity curve for maternity services use of informatics
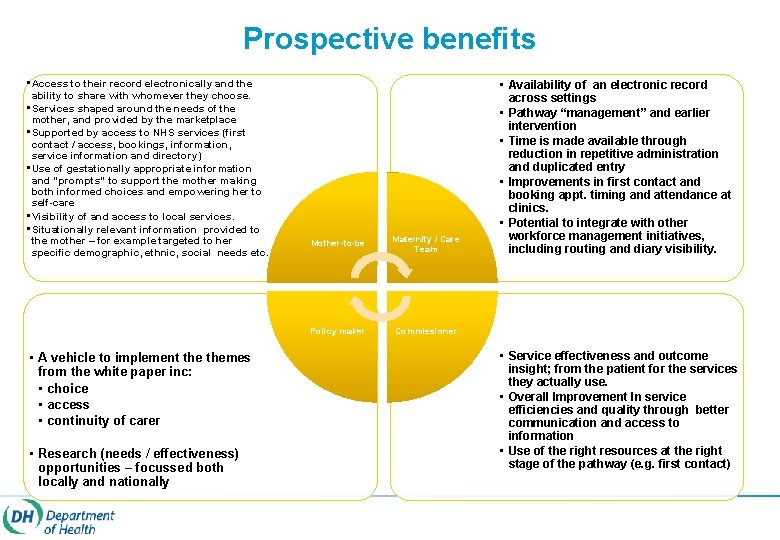
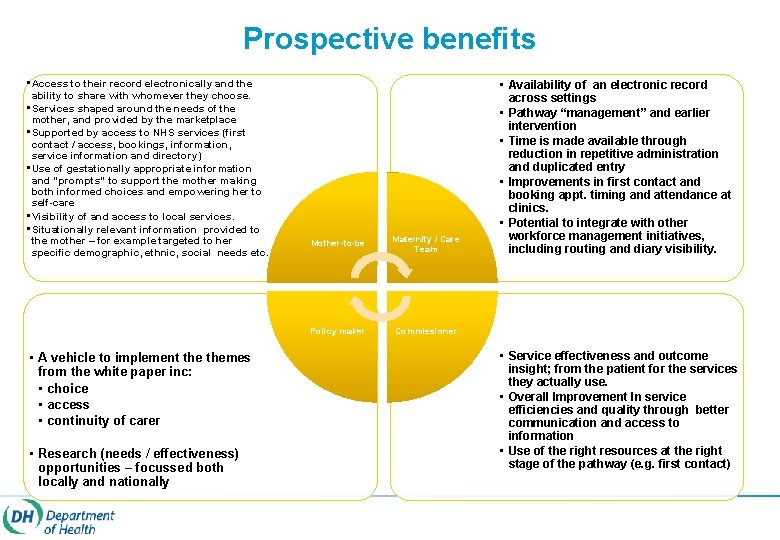
Prospective benefits • Access to their record electronically and the ability to share with whomever they choose. • Services shaped around the needs of the mother, and provided by the marketplace • Supported by access to NHS services (first contact / access, bookings, information, service information and directory) • Use of gestationally appropriate information and “prompts” to support the mother making both informed choices and empowering her to self-care • Visibility of and access to local services. • Situationally relevant information provided to the mother – for example targeted to her specific demographic, ethnic, social needs etc. • A vehicle to implement themes from the white paper inc: • choice • access • continuity of carer • Research (needs / effectiveness) opportunities – focussed both locally and nationally Mother-to-be Maternity / Care Team Policy maker Commissioner • Availability of an electronic record across settings • Pathway “management” and earlier intervention • Time is made available through reduction in repetitive administration and duplicated entry • Improvements in first contact and booking appt. timing and attendance at clinics. • Potential to integrate with other workforce management initiatives, including routing and diary visibility. • Service effectiveness and outcome insight; from the patient for the services they actually use. • Overall Improvement In service efficiencies and quality through better communication and access to information • Use of the right resources at the right stage of the pathway (e. g. first contact)
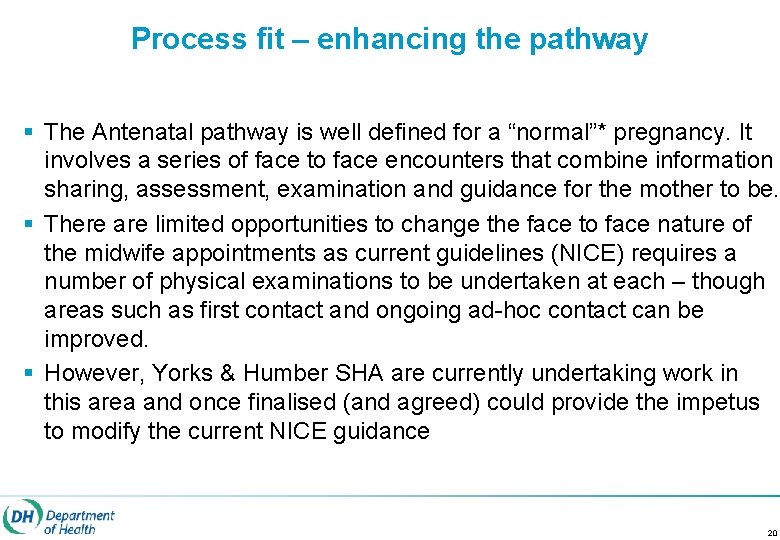
Process fit – enhancing the pathway § The Antenatal pathway is well defined for a “normal”* pregnancy. It involves a series of face to face encounters that combine information sharing, assessment, examination and guidance for the mother to be. § There are limited opportunities to change the face to face nature of the midwife appointments as current guidelines (NICE) requires a number of physical examinations to be undertaken at each – though areas such as first contact and ongoing ad-hoc contact can be improved. § However, Yorks & Humber SHA are currently undertaking work in this area and once finalised (and agreed) could provide the impetus to modify the current NICE guidance 20
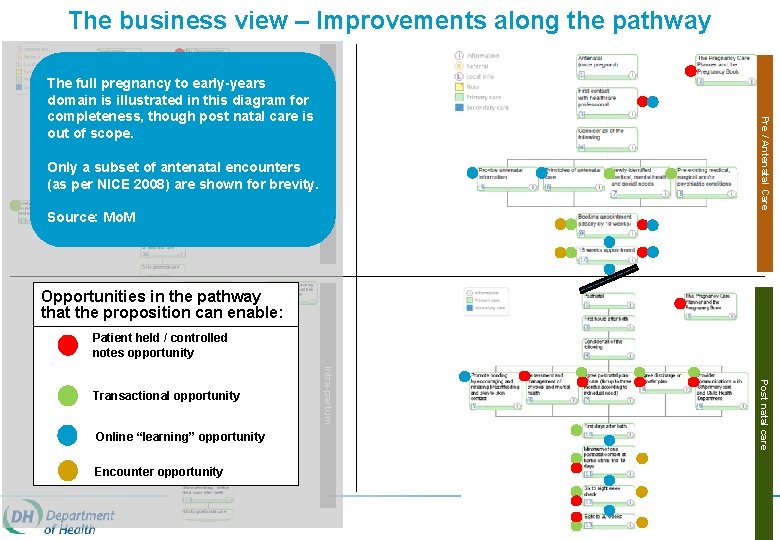
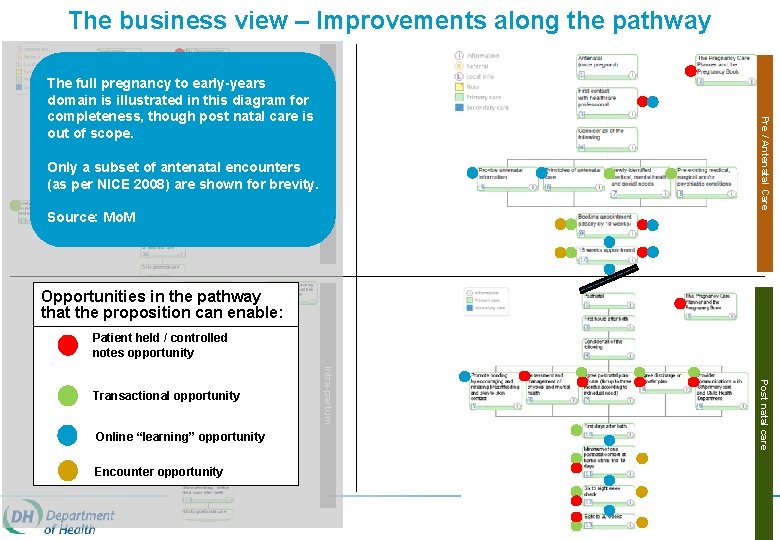
The business view – Improvements along the pathway Source: Mo. M Pre / Antenatal Care Only a subset of antenatal encounters (as per NICE 2008) are shown for brevity. Pre - pregnancy The full pregnancy to early-years domain is illustrated in this diagram for completeness, though post natal care is out of scope. Opportunities in the pathway that the proposition can enable: Patient held / controlled notes opportunity Encounter opportunity Post natal care Online “learning” opportunity Intra-partum Transactional opportunity
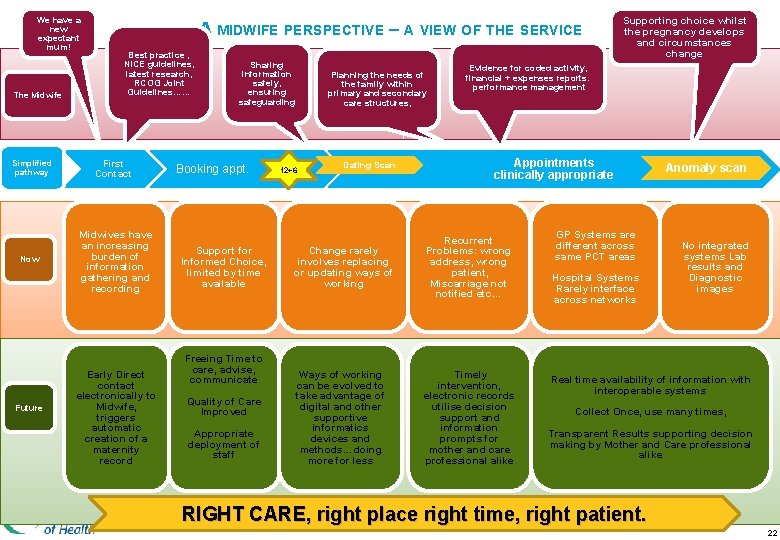
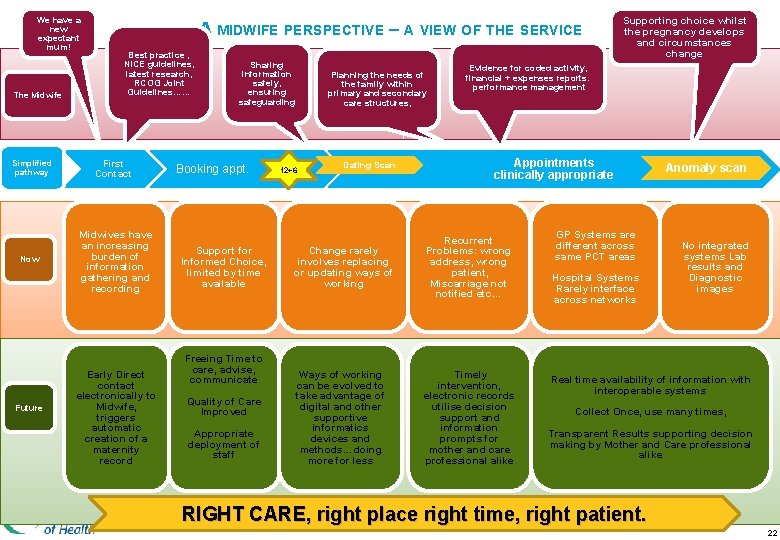
We have a new expectant mum! The Midwife Simplified pathway Now Future A MIDWIFE PERSPECTIVE – A VIEW OF THE SERVICE Best practice , NICE guidelines, latest research, RCOG Joint Guidelines…… First Contact Midwives have an increasing burden of information gathering and recording Early Direct contact electronically to Midwife, triggers automatic creation of a maternity record Sharing information safely, ensuring safeguarding Booking appt. Support for Informed Choice, limited by time available Freeing Time to care, advise, communicate Quality of Care Improved Appropriate deployment of staff Planning the needs of the family within primary and secondary care structures, 12+6 Dating Scan Supporting choice whilst the pregnancy develops and circumstances change Evidence for coded activity, financial + expenses reports. performance management Appointments clinically appropriate Change rarely involves replacing or updating ways of working Recurrent Problems: wrong address, wrong patient, Miscarriage notified etc… Ways of working can be evolved to take advantage of digital and other supportive informatics devices and methods…doing more for less Timely intervention, electronic records utilise decision support and information prompts for mother and care professional alike GP Systems are different across same PCT areas Hospital Systems Rarely interface across networks Anomaly scan No integrated systems Lab results and Diagnostic images Real time availability of information with interoperable systems Collect Once, use many times, Transparent Results supporting decision making by Mother and Care professional alike RIGHT CARE, right place right time, right patient. 22
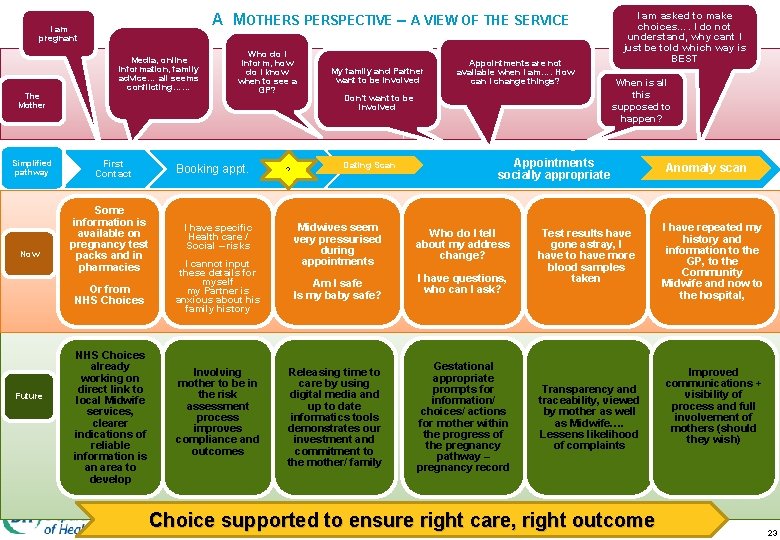
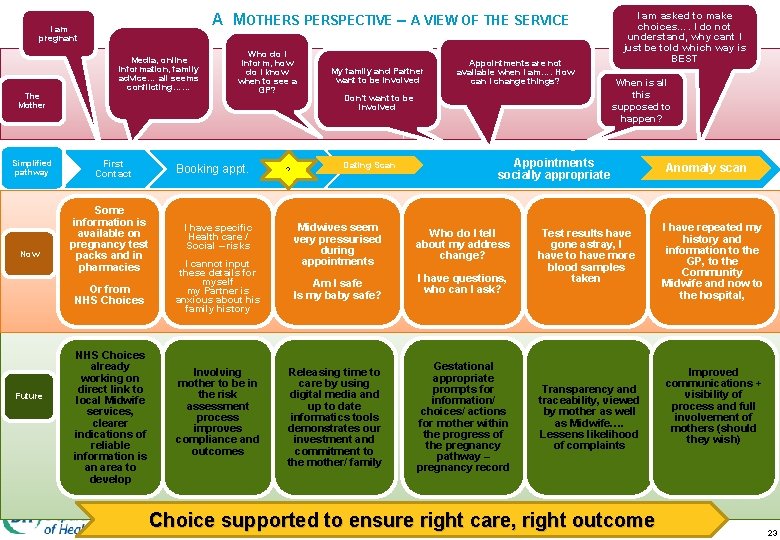
A MOTHERS PERSPECTIVE – A VIEW OF THE SERVICE I am pregnant The Mother Simplified pathway Now Media, online information, family advice… all seems conflicting…… First Contact Some information is available on pregnancy test packs and in pharmacies Or from NHS Choices Future NHS Choices already working on direct link to local Midwife services, clearer indications of reliable information is an area to develop Who do I inform, how do I know when to see a GP? Booking appt. I have specific Health care / Social – risks I cannot input these details for myself my Partner is anxious about his family history Involving mother to be in the risk assessment process improves compliance and outcomes ? My family and Partner want to be involved Appointments are not available when I am…. How can I change things? Don’t want to be involved Dating Scan Midwives seem very pressurised during appointments Am I safe Is my baby safe? Releasing time to care by using digital media and up to date informatics tools demonstrates our investment and commitment to the mother/ family I am asked to make choices…. I do not understand, why cant I just be told which way is BEST When is all this supposed to happen? Appointments socially appropriate Who do I tell about my address change? I have questions, who can I ask? Gestational appropriate prompts for information/ choices/ actions for mother within the progress of the pregnancy pathway – pregnancy record Test results have gone astray, I have to have more blood samples taken Transparency and traceability, viewed by mother as well as Midwife…. Lessens likelihood of complaints Choice supported to ensure right care, right outcome Anomaly scan I have repeated my history and information to the GP, to the Community Midwife and now to the hospital, Improved communications + visibility of process and full involvement of mothers (should they wish) 23
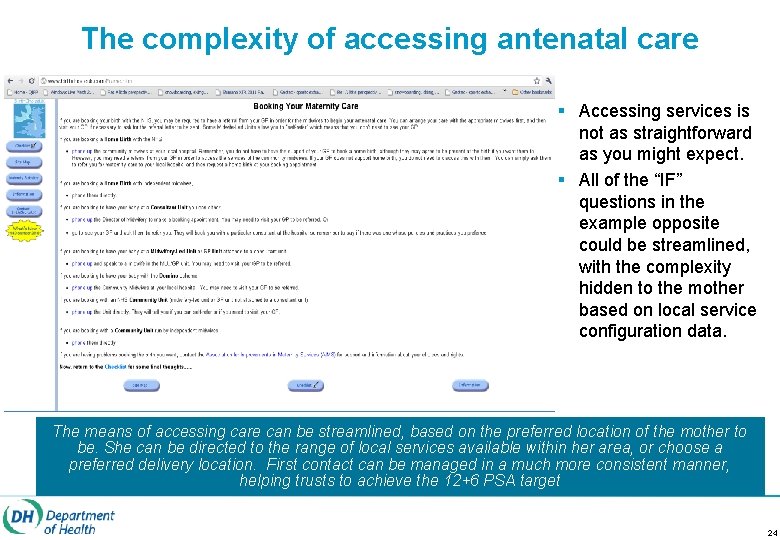
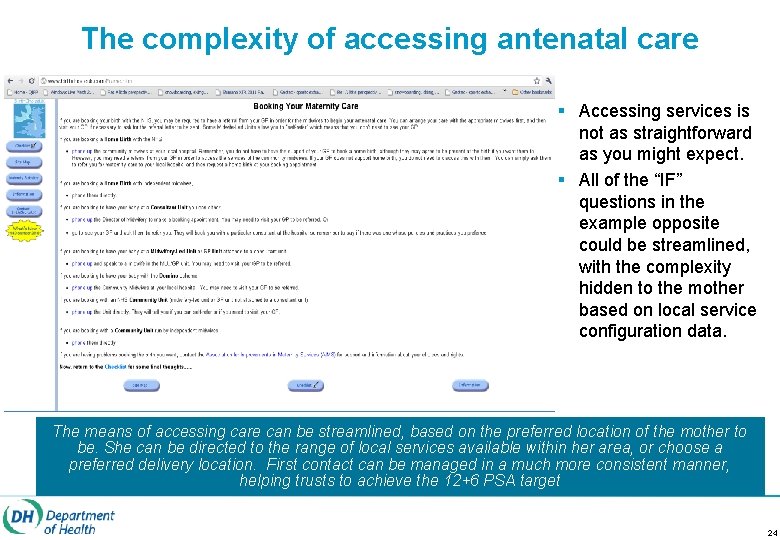
The complexity of accessing antenatal care § Accessing services is not as straightforward as you might expect. § All of the “IF” questions in the example opposite could be streamlined, with the complexity hidden to the mother based on local service configuration data. The means of accessing care can be streamlined, based on the preferred location of the mother to be. She can be directed to the range of local services available within her area, or choose a preferred delivery location. First contact can be managed in a much more consistent manner, helping trusts to achieve the 12+6 PSA target 24
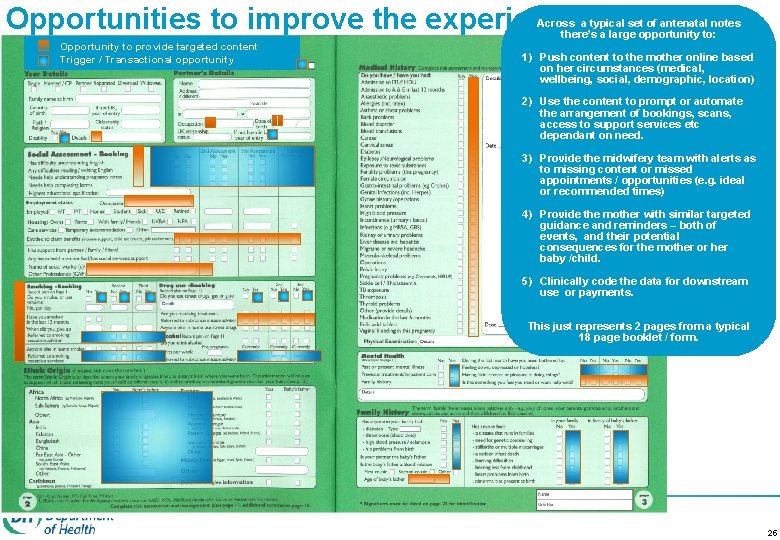
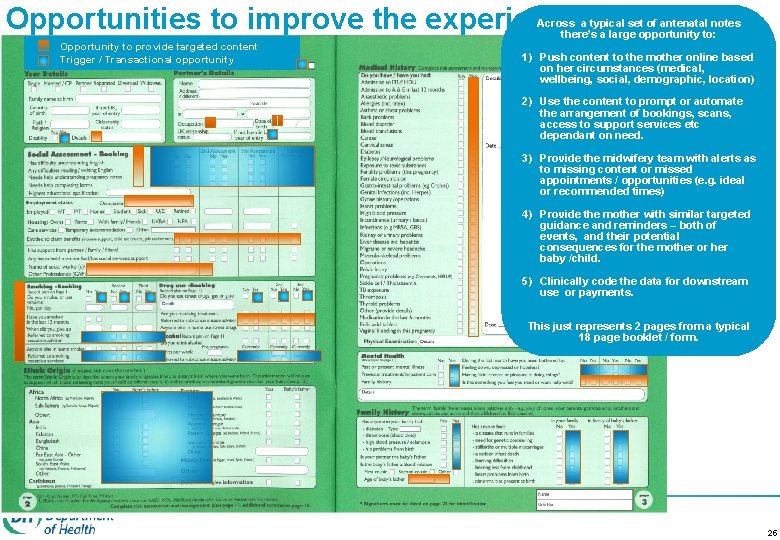
Opportunities to improve the experience Across a typical set of antenatal notes there’s a large opportunity to: Opportunity to provide targeted content Trigger / Transactional opportunity 1) Push content to the mother online based on her circumstances (medical, wellbeing, social, demographic, location) 2) Use the content to prompt or automate the arrangement of bookings, scans, access to support services etc dependant on need. 3) Provide the midwifery team with alerts as to missing content or missed appointments / opportunities (e. g. ideal or recommended times) 4) Provide the mother with similar targeted guidance and reminders – both of events, and their potential consequences for the mother or her baby /child. 5) Clinically code the data for downstream use or payments. This just represents 2 pages from a typical 18 page booklet / form. 25
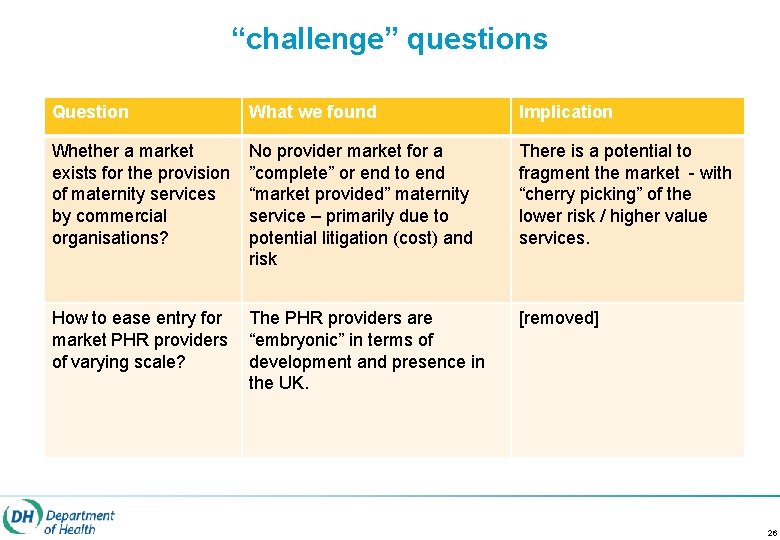
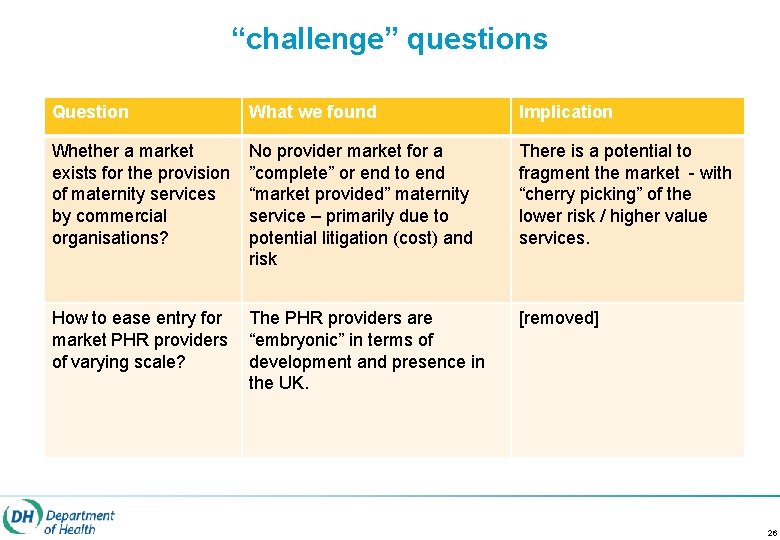
“challenge” questions Question What we found Implication Whether a market exists for the provision of maternity services by commercial organisations? No provider market for a ”complete” or end to end “market provided” maternity service – primarily due to potential litigation (cost) and risk There is a potential to fragment the market - with “cherry picking” of the lower risk / higher value services. How to ease entry for market PHR providers of varying scale? The PHR providers are “embryonic” in terms of development and presence in the UK. [removed] 26
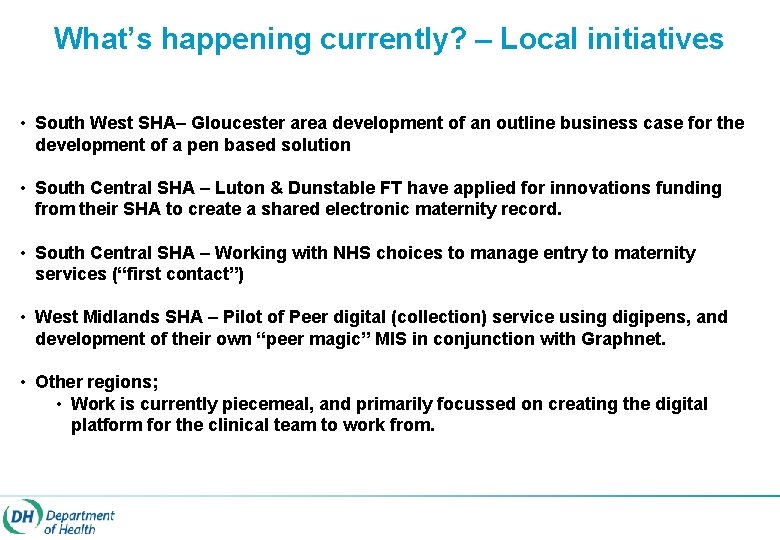
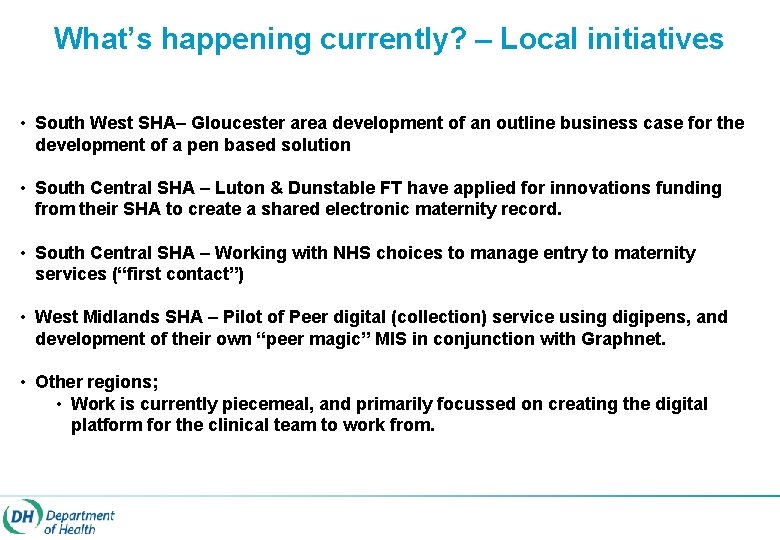
What’s happening currently? – Local initiatives • South West SHA– Gloucester area development of an outline business case for the development of a pen based solution • South Central SHA – Luton & Dunstable FT have applied for innovations funding from their SHA to create a shared electronic maternity record. • South Central SHA – Working with NHS choices to manage entry to maternity services (“first contact”) • West Midlands SHA – Pilot of Peer digital (collection) service using digipens, and development of their own “peer magic” MIS in conjunction with Graphnet. • Other regions; • Work is currently piecemeal, and primarily focussed on creating the digital platform for the clinical team to work from.

Technical overview
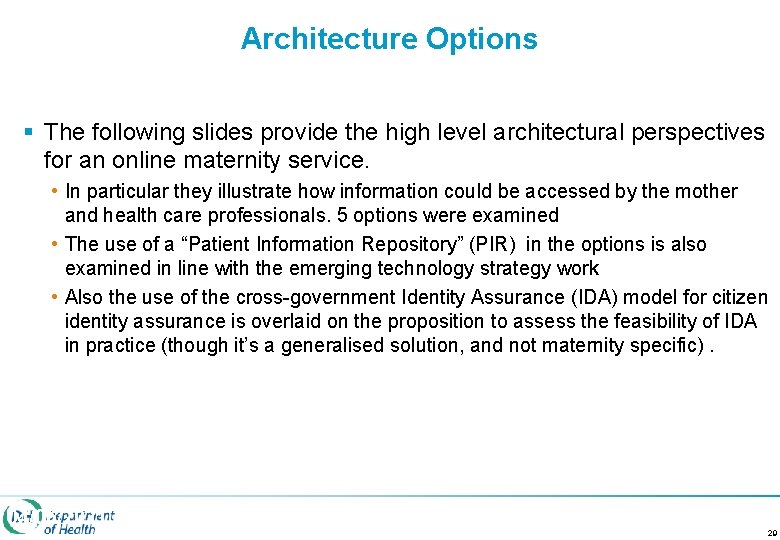
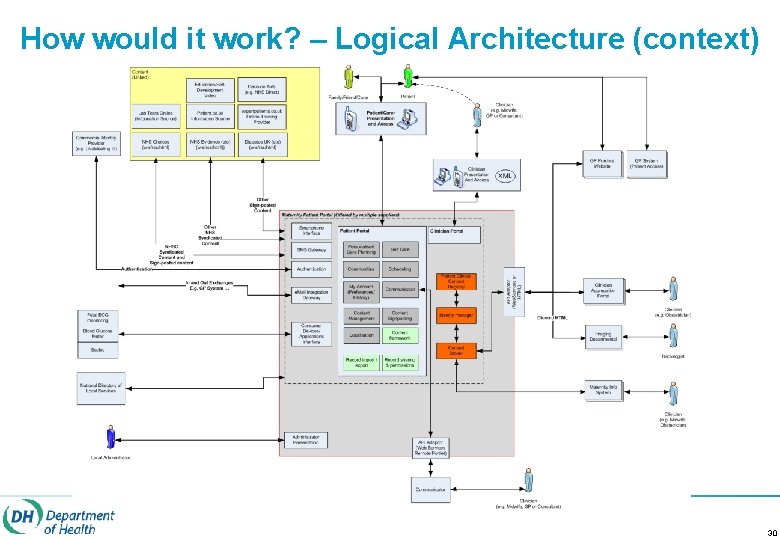
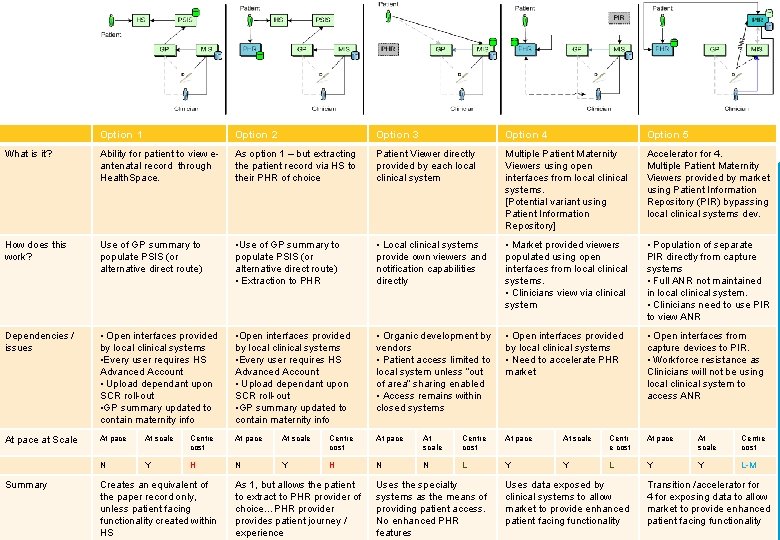
Architecture Options § The following slides provide the high level architectural perspectives for an online maternity service. • In particular they illustrate how information could be accessed by the mother and health care professionals. 5 options were examined • The use of a “Patient Information Repository” (PIR) in the options is also examined in line with the emerging technology strategy work • Also the use of the cross-government Identity Assurance (IDA) model for citizen identity assurance is overlaid on the proposition to assess the feasibility of IDA in practice (though it’s a generalised solution, and not maternity specific). 04/06/2021 29
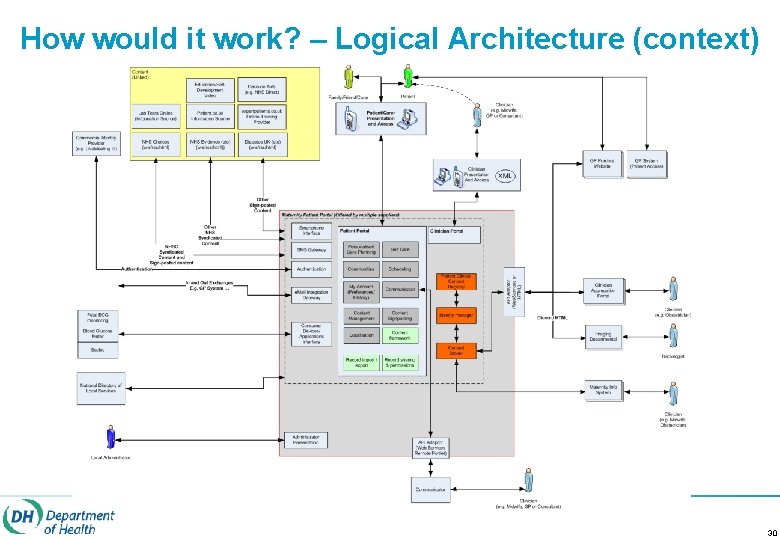
How would it work? – Logical Architecture (context) 30
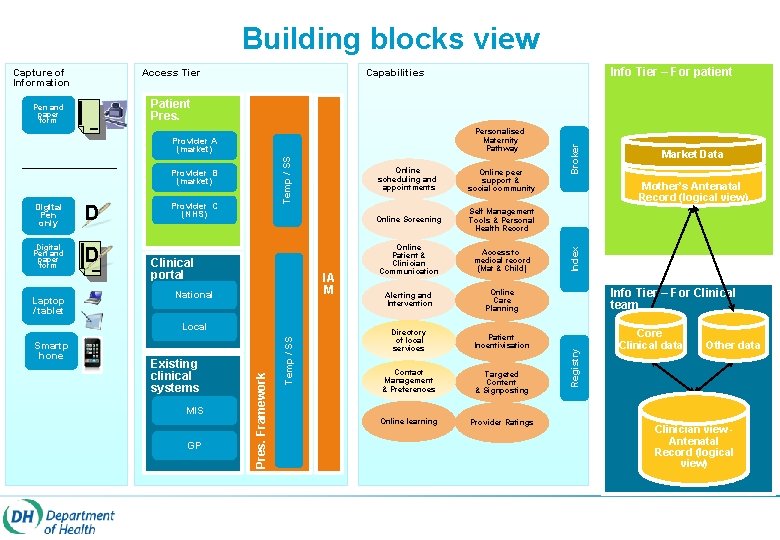
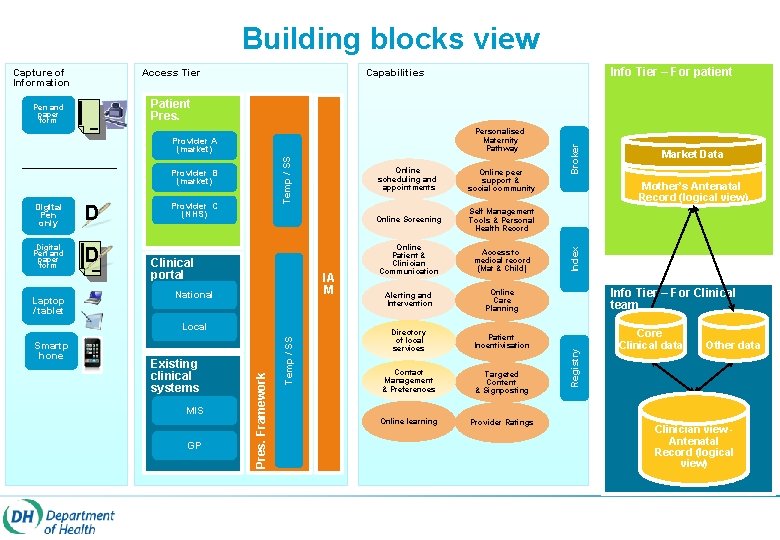
Building blocks view Capture of Information Access Tier Digital Pen only D Digital Pen and paper form D Provider C (NHS) Clinical portal IA M National Existing clinical systems MIS GP Temp / SS Smartp hone Pres. Framework Local Online scheduling and appointments Online peer support & social community Online Screening Self Management Tools & Personal Health Record Online Patient & Clinician Communication Access to medical record (Mat & Child) Alerting and Intervention Online Care Planning Directory of local services Patient Incentivisation Contact Management & Preferences Targeted Content & Signposting Online learning Provider Ratings Market Data Mother’s Antenatal Record (logical view) Index Temp / SS Provider B (market) Info Tier – For Clinical team Registry Personalised Maternity Pathway Provider A (market) Broker Patient Pres. Pen and paper form Laptop / tablet Info Tier – For patient Capabilities Core Clinical data Other data Clinician view Antenatal Record (logical view)

Logical – Access and flows +Repository +broker +orchestration 32
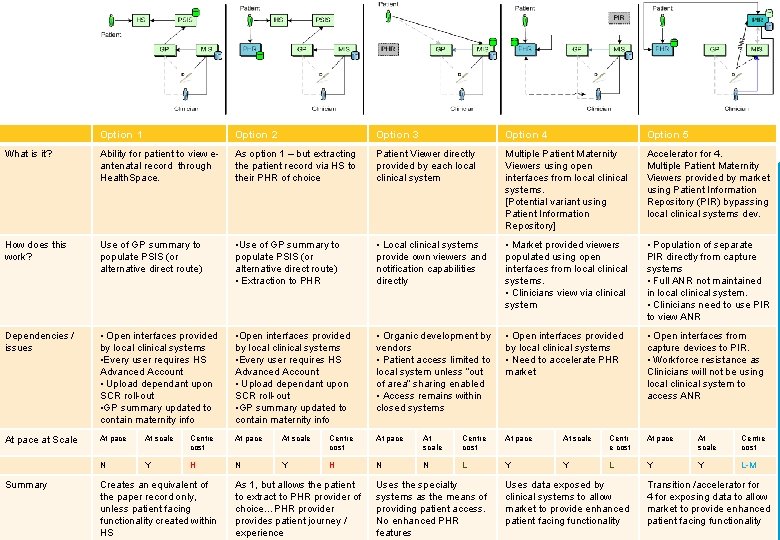
Option 1 Option 2 Option 3 Option 4 Option 5 What is it? Ability for patient to view eantenatal record through Health. Space. As option 1 – but extracting the patient record via HS to their PHR of choice Patient Viewer directly provided by each local clinical system Multiple Patient Maternity Viewers using open interfaces from local clinical systems. [Potential variant using Patient Information Repository] Accelerator for 4. Multiple Patient Maternity Viewers provided by market using Patient Information Repository (PIR) bypassing local clinical systems dev. How does this work? Use of GP summary to populate PSIS (or alternative direct route) • Use of GP summary to populate PSIS (or alternative direct route) • Extraction to PHR • Local clinical systems provide own viewers and notification capabilities directly • Market provided viewers populated using open interfaces from local clinical systems. • Clinicians view via clinical system • Population of separate PIR directly from capture systems • Full ANR not maintained in local clinical system. • Clinicians need to use PIR to view ANR Dependencies / issues • Open interfaces provided by local clinical systems • Every user requires HS Advanced Account • Upload dependant upon SCR roll-out • GP summary updated to contain maternity info • Organic development by vendors • Patient access limited to local system unless “out of area” sharing enabled • Access remains within closed systems • Open interfaces provided by local clinical systems • Need to accelerate PHR market • Open interfaces from capture devices to PIR. • Workforce resistance as Clinicians will not be using local clinical system to access ANR At pace at Scale At pace At scale Centre cost At pace At scale Centr e cost At pace At scale Centre cost N Y H N N L Y Y L-M Summary Creates an equivalent of the paper record only, unless patient facing functionality created within HS As 1, but allows the patient to extract to PHR provider of choice…PHR provider provides patient journey / experience Uses the specialty systems as the means of providing patient access. No enhanced PHR features Uses data exposed by clinical systems to allow market to provide enhanced patient facing functionality Transition /accelerator for 4 for exposing data to allow market to provide enhanced patient facing functionality
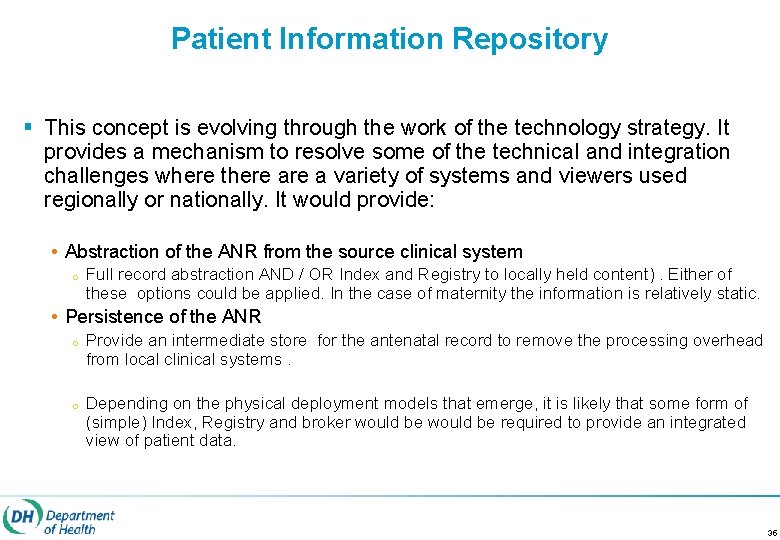
Patient Information Repository § This concept is evolving through the work of the technology strategy. It provides a mechanism to resolve some of the technical and integration challenges where there a variety of systems and viewers used regionally or nationally. It would provide: • Abstraction of the ANR from the source clinical system o Full record abstraction AND / OR Index and Registry to locally held content). Either of these options could be applied. In the case of maternity the information is relatively static. • Persistence of the ANR o o Provide an intermediate store for the antenatal record to remove the processing overhead from local clinical systems. Depending on the physical deployment models that emerge, it is likely that some form of (simple) Index, Registry and broker would be required to provide an integrated view of patient data. 35
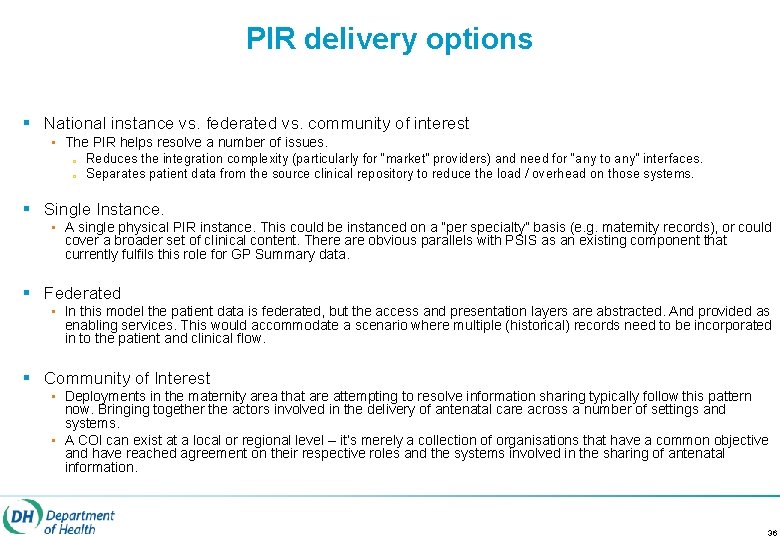
PIR delivery options § National instance vs. federated vs. community of interest • The PIR helps resolve a number of issues. o o Reduces the integration complexity (particularly for “market” providers) and need for “any to any” interfaces. Separates patient data from the source clinical repository to reduce the load / overhead on those systems. § Single Instance. • A single physical PIR instance. This could be instanced on a “per specialty” basis (e. g. maternity records), or could cover a broader set of clinical content. There are obvious parallels with PSIS as an existing component that currently fulfils this role for GP Summary data. § Federated • In this model the patient data is federated, but the access and presentation layers are abstracted. And provided as enabling services. This would accommodate a scenario where multiple (historical) records need to be incorporated in to the patient and clinical flow. § Community of Interest • Deployments in the maternity area that are attempting to resolve information sharing typically follow this pattern now. Bringing together the actors involved in the delivery of antenatal care across a number of settings and systems. • A COI can exist at a local or regional level – it’s merely a collection of organisations that have a common objective and have reached agreement on their respective roles and the systems involved in the sharing of antenatal information. 36
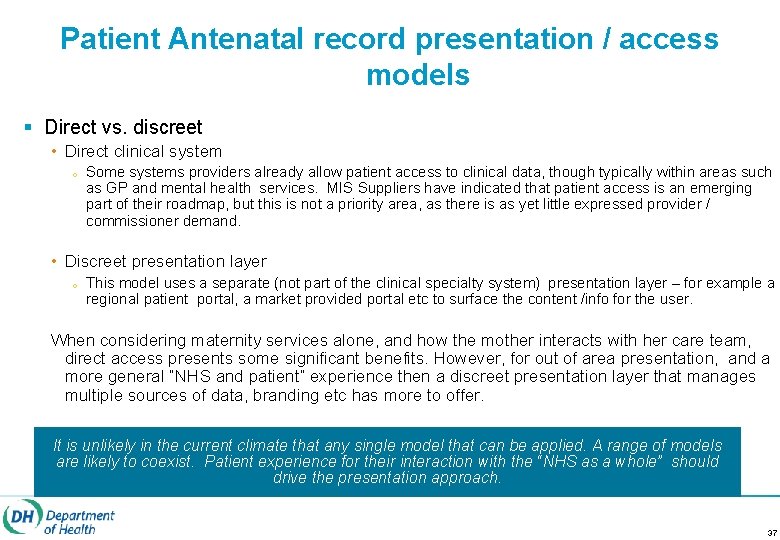
Patient Antenatal record presentation / access models § Direct vs. discreet • Direct clinical system o Some systems providers already allow patient access to clinical data, though typically within areas such as GP and mental health services. MIS Suppliers have indicated that patient access is an emerging part of their roadmap, but this is not a priority area, as there is as yet little expressed provider / commissioner demand. • Discreet presentation layer o This model uses a separate (not part of the clinical specialty system) presentation layer – for example a regional patient portal, a market provided portal etc to surface the content /info for the user. When considering maternity services alone, and how the mother interacts with her care team, direct access presents some significant benefits. However, for out of area presentation, and a more general “NHS and patient” experience then a discreet presentation layer that manages multiple sources of data, branding etc has more to offer. It is unlikely in the current climate that any single model that can be applied. A range of models are likely to coexist. Patient experience for their interaction with the “NHS as a whole” should drive the presentation approach. 37
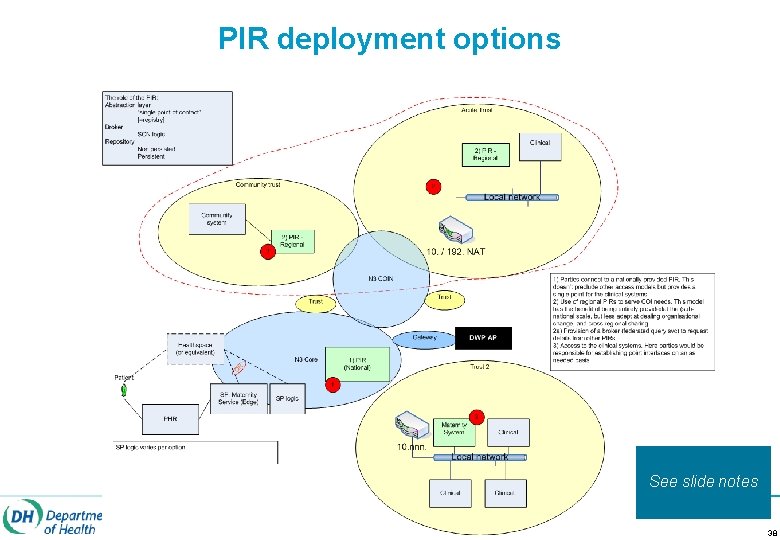
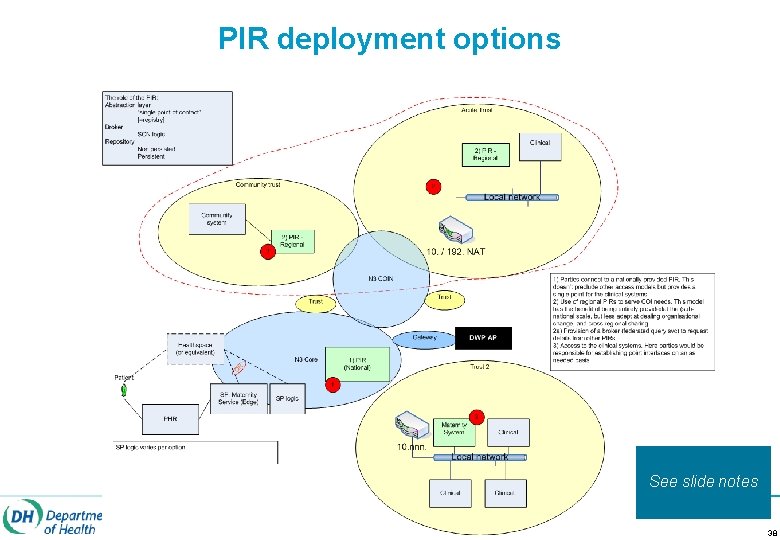
PIR deployment options See slide notes 38
Message Payload For each of the messages defined: § CDA document based on the content of existing (mother held) paper antenatal records. • Comprised of a core, nationally agreed data set [ ideally sponsored by RCOG / RCM – though noting the timescale implications] • Optional information extensions to meet the needs of individual trusts. The content and structure of the payload, as well as the messaging specifications and requirements are being addressed in a parallel workstream. 39
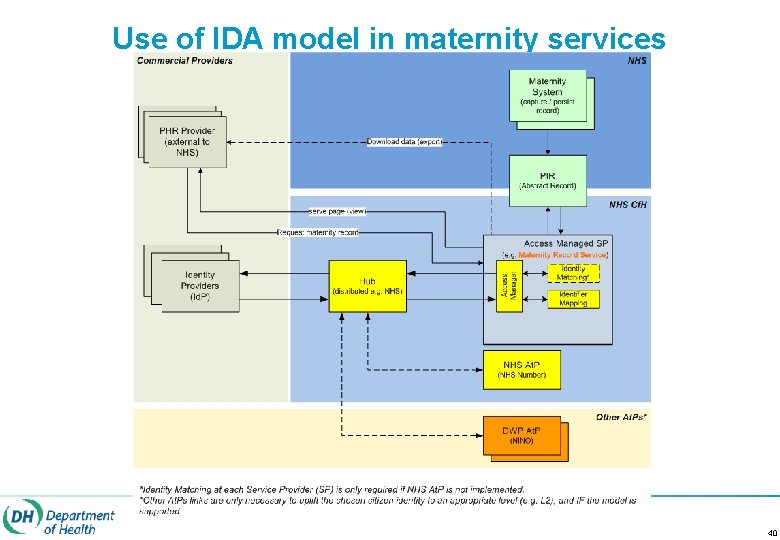
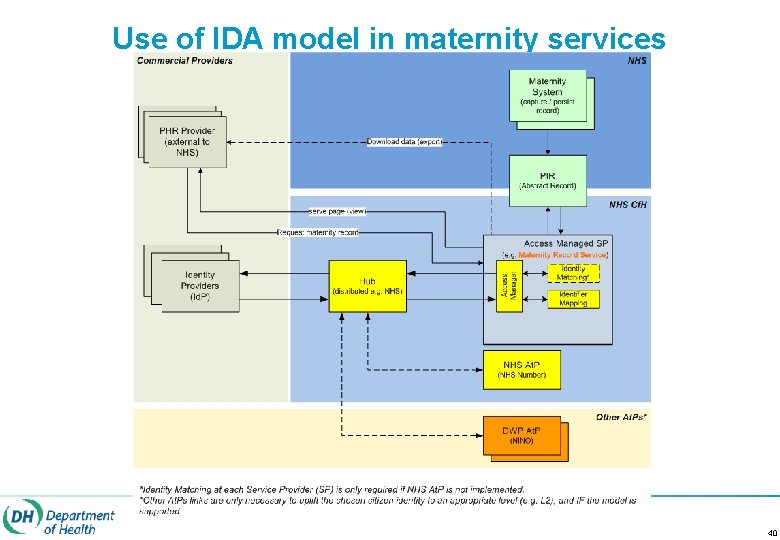
Use of IDA model in maternity services 40
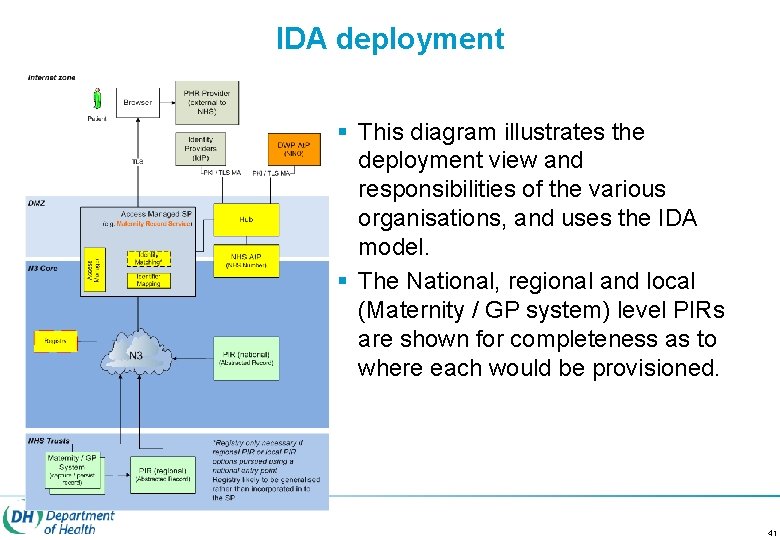
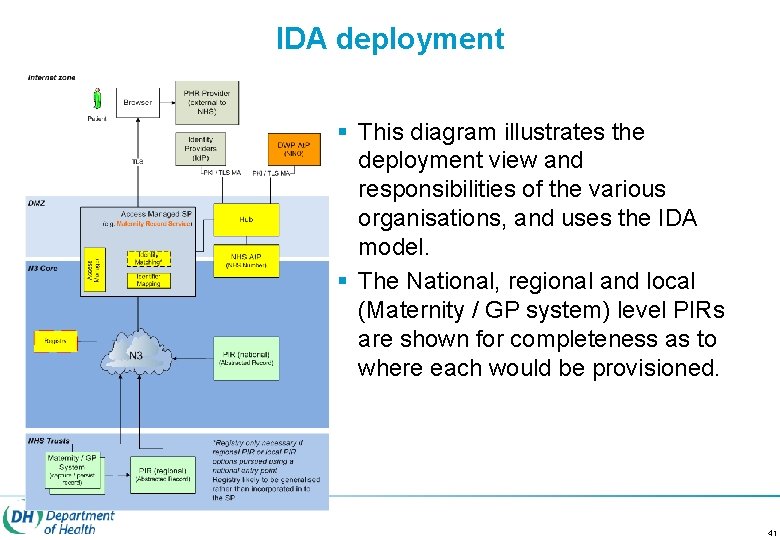
IDA deployment § This diagram illustrates the deployment view and responsibilities of the various organisations, and uses the IDA model. § The National, regional and local (Maternity / GP system) level PIRs are shown for completeness as to where each would be provisioned. 41
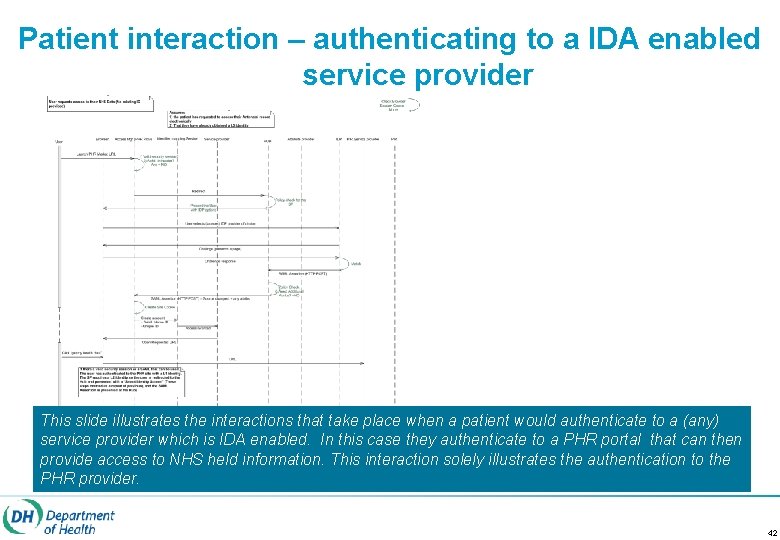
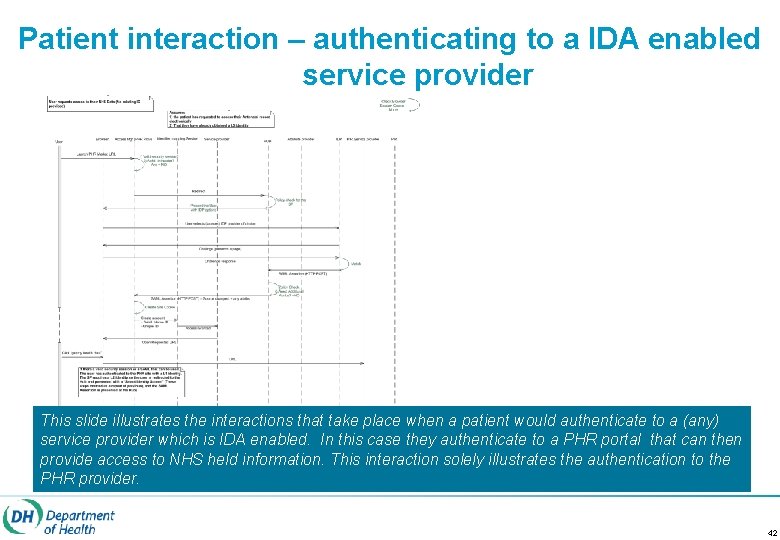
Patient interaction – authenticating to a IDA enabled service provider This slide illustrates the interactions that take place when a patient would authenticate to a (any) service provider which is IDA enabled. In this case they authenticate to a PHR portal that can then provide access to NHS held information. This interaction solely illustrates the authentication to the PHR provider. 42
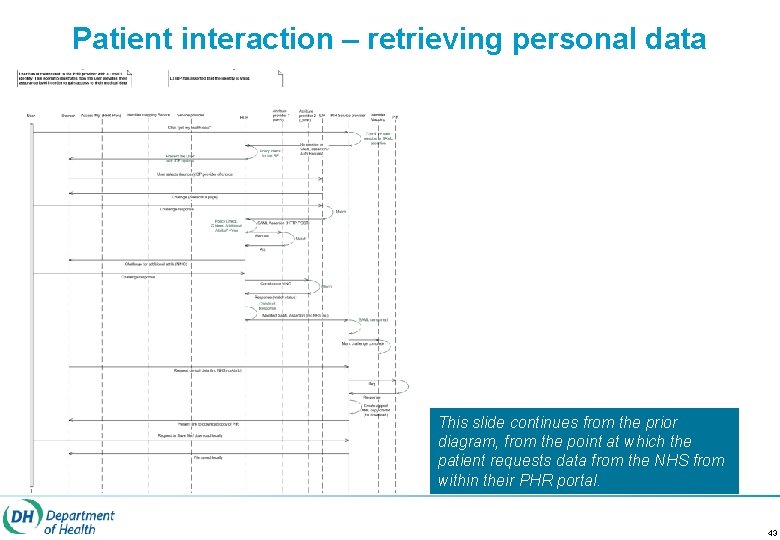
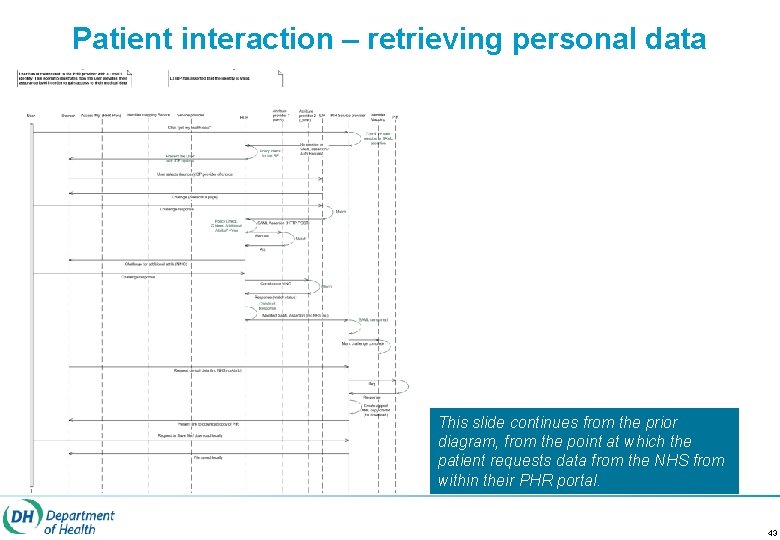
Patient interaction – retrieving personal data This slide continues from the prior diagram, from the point at which the patient requests data from the NHS from within their PHR portal. 43

Summary of Deployment Options
![Slide Removed 04062021 45 § [Slide Removed] 04/06/2021 45](https://slidetodoc.com/presentation_image_h2/56548a1d0ea897863d915ff22498d9ec/image-44.jpg)
§ [Slide Removed] 04/06/2021 45
 Early obstetric warning system chart
Early obstetric warning system chart Comprehensive model of personalised care
Comprehensive model of personalised care Personalised care operating model
Personalised care operating model Comprehensive model of personalised care
Comprehensive model of personalised care James sanderson nhs
James sanderson nhs Qipp programme
Qipp programme How to report project progress
How to report project progress Personalised mobile search engine
Personalised mobile search engine Medolac
Medolac General motors
General motors How many years is four score and seven years
How many years is four score and seven years Walmart sedgwick number
Walmart sedgwick number Ar 600-8-10 maternity leave
Ar 600-8-10 maternity leave Legislation related to maternity benefits
Legislation related to maternity benefits Objectives of maternity ward
Objectives of maternity ward Wessex maternity academy
Wessex maternity academy Maternity leave poland
Maternity leave poland Ut austin maternity leave
Ut austin maternity leave Why is maternity leave important
Why is maternity leave important Maternity bitmoji
Maternity bitmoji Maternity benefit act 1961 notes
Maternity benefit act 1961 notes Antenatal assessment format
Antenatal assessment format There is a practical joker in the maternity ward
There is a practical joker in the maternity ward Woman within maternity
Woman within maternity Homerton maternity helpline
Homerton maternity helpline Female nude (for the decoration of bristol club)
Female nude (for the decoration of bristol club) Goat years to human years
Goat years to human years 300 solar years to lunar years
300 solar years to lunar years Primary secondary and tertiary care
Primary secondary and tertiary care Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * Shakespeare early years
Shakespeare early years Jean baptiste louis gros
Jean baptiste louis gros Summarise types of early years provision
Summarise types of early years provision Medway early years
Medway early years Effects of transitions in early years
Effects of transitions in early years Bristol early years characteristics of effective learning
Bristol early years characteristics of effective learning Hudson 1509 route
Hudson 1509 route Services for young children hampshire
Services for young children hampshire Early years learning framework overview
Early years learning framework overview Eye early years evaluation
Eye early years evaluation Early adulthood 20 to 40 years
Early adulthood 20 to 40 years Pgce early years
Pgce early years Glasgow counts tracker
Glasgow counts tracker Coventry early years portal
Coventry early years portal Block play early years
Block play early years