Nutrition and the Pediatric Patient Dawn O Eckhoff

- Slides: 19
Nutrition and the Pediatric Patient Dawn O. Eckhoff, Ph. D, APRN, CPNP-PC
What are we going to cover? • • Nutritional Requirements and Dietary Intakes Nutritional Assessment Optimal Nutrition Strategies Age-Specific Considerations Disorders Adverse Reactions Controversies
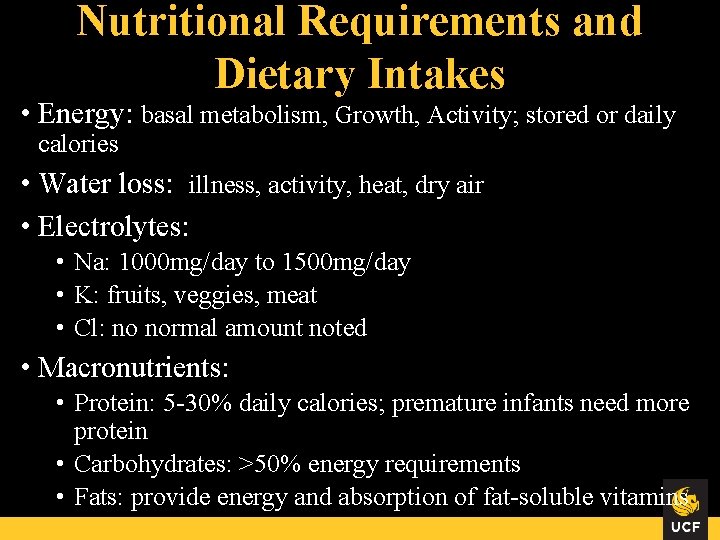
Nutritional Requirements and Dietary Intakes • Energy: basal metabolism, Growth, Activity; stored or daily calories • Water loss: illness, activity, heat, dry air • Electrolytes: • Na: 1000 mg/day to 1500 mg/day • K: fruits, veggies, meat • Cl: no normal amount noted • Macronutrients: • Protein: 5 -30% daily calories; premature infants need more protein • Carbohydrates: >50% energy requirements • Fats: provide energy and absorption of fat-soluble vitamins
Nutritional Requirements and Dietary Intakes • Micronutrients • Fat-Soluble Vitamins: stored in body tissues for long time • Water-Soluble Vitamins: stored in small amounts • Minerals and Elements • 3 major minerals • Ca: bone density • Mg • P • Supplements • Vitamin D: 400 -600 IU daily • Need nutrient rich diet
• History • • Nutritional Assessment Pregnancy nutrition Food and fluid intake-child and family Eating patterns/behaviors Reactions/attitudes Management of foods Health status and food Family history: HTN, DM, hyperlipidemia, obesity, heart disease, allergies, eating disorders • PE • Labs: Hgb, Hct, Iron studies, electrolytes, D, bone radiographs
Optimal Nutrition Strategies • Healthy Eating Habits • • • Positive Examples/Role Models Portions: 1 TBS per year of age Limits Routine mealtimes Appropriate supervision Adequate exercise, sleep, rest Offer foods when hungry Small taste Have them help • Nutrition Education • My. Plate, My. Plate for Kids, Super. Tracker
Age-Specific Considerations • Newborns - Infant • • Rapid growth = high calories Need fat intake Whole cow’s milk until 24 months Vitamin D until 1 year old Vitamin C after age 4 to 6 months Iron: fortified cereals Fluoride: starting at 6 months old where water is not fluorinated • GERD – resolved by 24 months • Solids at 6 months of age • Self-regulation
Age-Specific Considerations • Early Childhood • Decreased energy needs • Vitamin D supplement • Learn to eat by observing
Age-Specific Considerations • Middle Childhood • • • Increase protein with growth Encourage good eating habits and mealtime routines Vitamin D Multivitamin for poor diets Vegans need B 12
Age-Specific Considerations • Adolescents • Rapid growth needs increase calories • Increase protein for muscle mass • Increase need for thiamin, riboflavin, niacin, folate, iron, zinc, calcium • Irregular eating habits or limited diets may need supplements • Vitamin D for all • B 12 for vegans • Eating habits influenced by independence and social activities
Physical Activity • 60 minutes every day, moderate to vigorous activity • 3 days a week; muscle and bone strengthening • 3 days a week; vigorous activity
Vegetarian and Vegan Diets • • Vegan: only plant-based foods Lactovegetarians: add milk and dairy Lacto-ovovegetarians: add eggs Macrobiotic diets: add whole grains, white meats or white fish (minimally) • Pescatarians: only meat is fish • Flexitarians: mostly plant-based with occasional fish, chicken, seafood
Management of Diets • Labs: B 12, Zinc, Fe and D • Make sure of high fiber
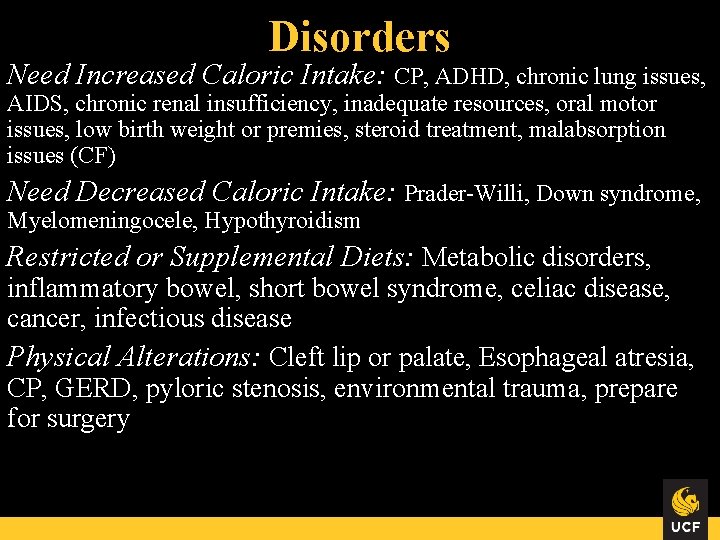
Disorders Need Increased Caloric Intake: CP, ADHD, chronic lung issues, AIDS, chronic renal insufficiency, inadequate resources, oral motor issues, low birth weight or premies, steroid treatment, malabsorption issues (CF) Need Decreased Caloric Intake: Prader-Willi, Down syndrome, Myelomeningocele, Hypothyroidism Restricted or Supplemental Diets: Metabolic disorders, inflammatory bowel, short bowel syndrome, celiac disease, cancer, infectious disease Physical Alterations: Cleft lip or palate, Esophageal atresia, CP, GERD, pyloric stenosis, environmental trauma, prepare for surgery
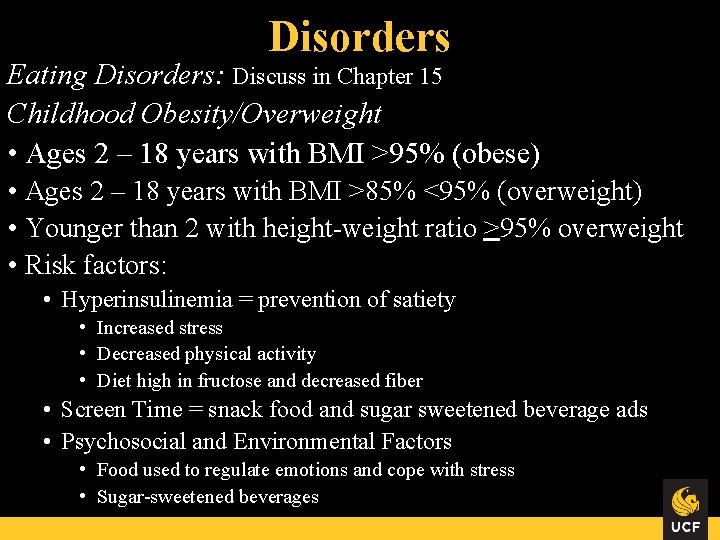
Disorders Eating Disorders: Discuss in Chapter 15 Childhood Obesity/Overweight • Ages 2 – 18 years with BMI >95% (obese) • Ages 2 – 18 years with BMI >85% <95% (overweight) • Younger than 2 with height-weight ratio >95% overweight • Risk factors: • Hyperinsulinemia = prevention of satiety • Increased stress • Decreased physical activity • Diet high in fructose and decreased fiber • Screen Time = snack food and sugar sweetened beverage ads • Psychosocial and Environmental Factors • Food used to regulate emotions and cope with stress • Sugar-sweetened beverages
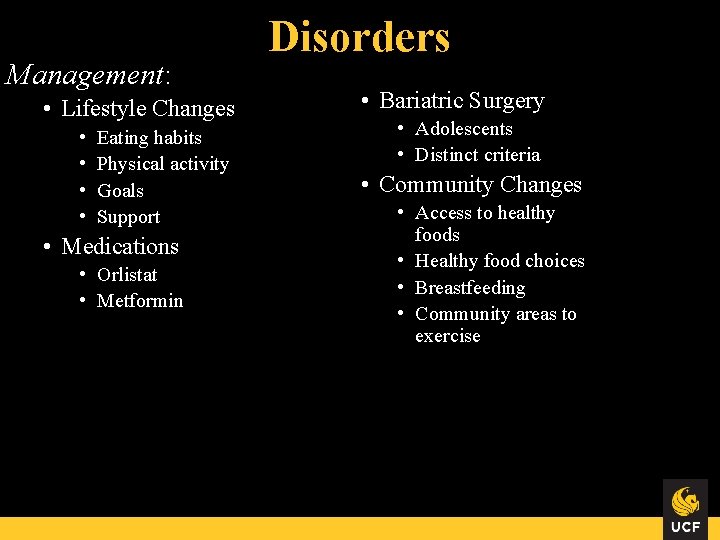
Management: • Lifestyle Changes • • Eating habits Physical activity Goals Support • Medications • Orlistat • Metformin Disorders • Bariatric Surgery • Adolescents • Distinct criteria • Community Changes • Access to healthy foods • Healthy food choices • Breastfeeding • Community areas to exercise
Adverse Reactions Food allergy: hypersensitivity to food or food additive Food intolerance: nonimmunologic inability to process food Contributing Factors: • Heredity • Infant diet: include allergenic foods • Compromised GI tract • Type of food

Adverse Reactions Management: • Elimination diet • Oral immunotherapy • Food Challenge • Medication • Education
Controversies Sugar Consumption: • 4 to 8 year olds: 3 tsp • 9 to adult: 5 to 8 tsp Gluten-Free Diets: • Celiac disease • Often highly processed and not enriched with Fe or folate
 Ude
Ude Patient 2 patient
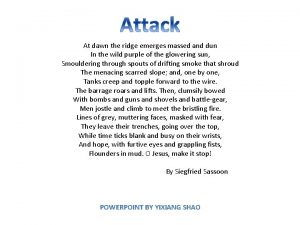
Patient 2 patient At dawn the ridge emerges massed and dun
At dawn the ridge emerges massed and dun At dawn the ridge emerges massed and dun
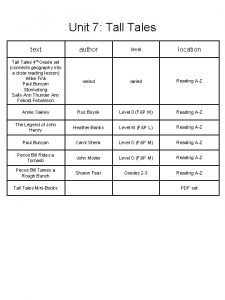
At dawn the ridge emerges massed and dun Tall tale story
Tall tale story Jillian and dawn are playing a game
Jillian and dawn are playing a game And his tune is heard on the distant hill
And his tune is heard on the distant hill Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Thang điểm glasgow
Thang điểm glasgow Chúa yêu trần thế
Chúa yêu trần thế Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5