Nutrition and Older Adults Issues among Community and







- Slides: 39
Nutrition and Older Adults: Issues among Community and Long-Term Care Residents Jean Helps, RD 1 and Christina Lengyel Ph. D, RD 2 1 Clinical Nutrition Manager, Long Term Care Sector, WRHA Nutrition and Food Services Professor, Human Nutritional Sciences, Faculty of Human Ecology, University of Manitoba 2 Assistant

Outline Canadian Demographics n Factors affecting Nutritional Intake n Long–Term Care Setting n Rural and Urban Communities n Nutritional Guidelines and Recommendations n Take Home Messages n
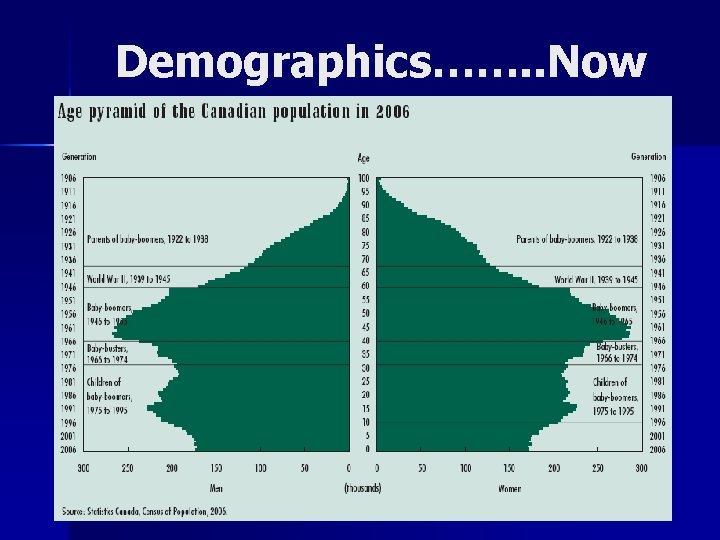
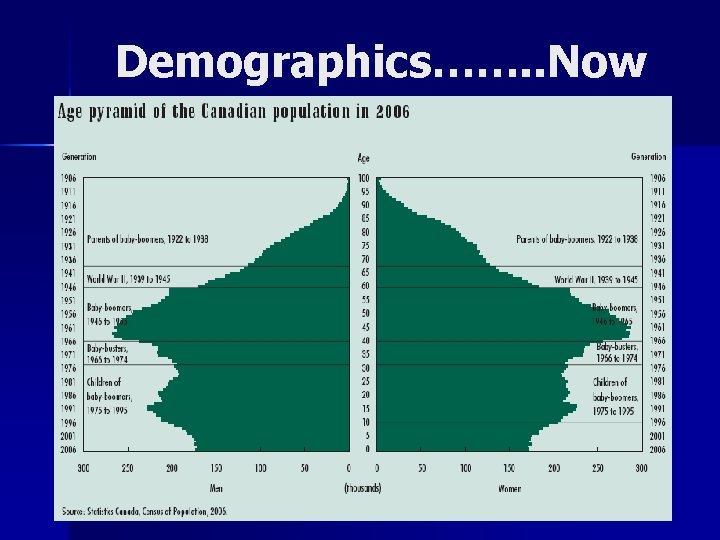
Demographics……. . Now

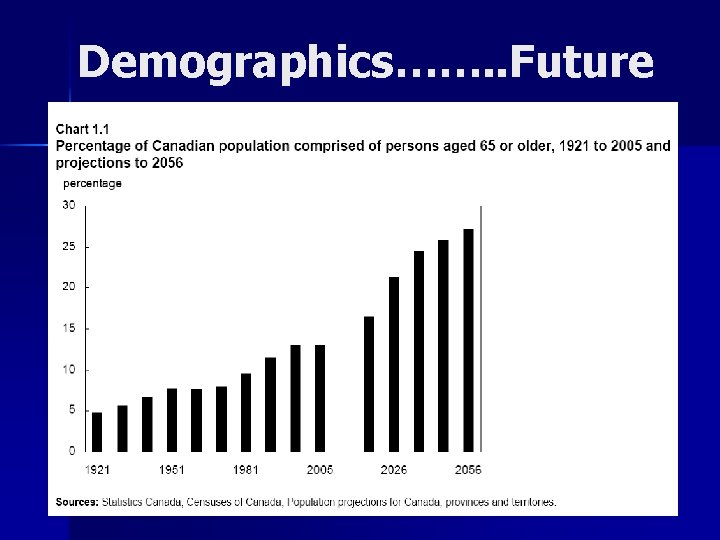
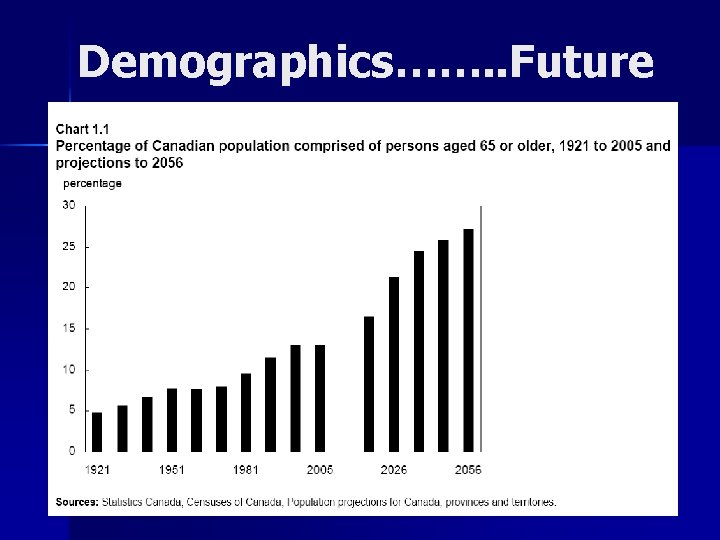
Demographics……. . Future
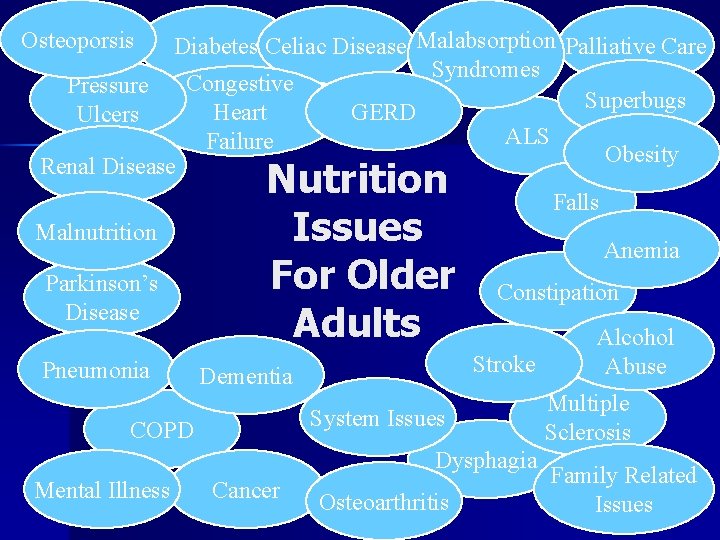
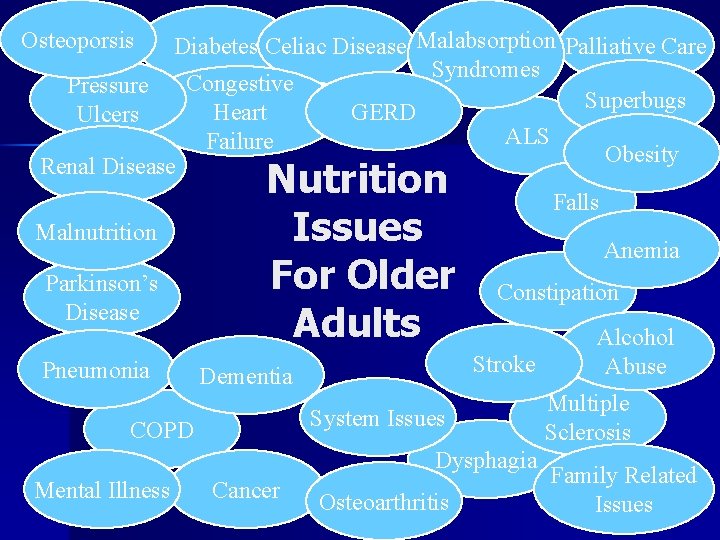
Osteoporsis Diabetes Celiac Disease Malabsorption Palliative Care Syndromes Congestive Pressure Superbugs GERD Heart Ulcers ALS Failure Obesity Renal Disease Falls Malnutrition Anemia Parkinson’s Constipation Disease Alcohol Stroke Abuse Pneumonia Dementia Multiple System Issues COPD Sclerosis Dysphagia Family Related Mental Illness Cancer Osteoarthritis Issues Nutrition Issues For Older Adults
Nutrition and Quality of Life n n Healthy food choices positively influence the quality of life of older adults. Older adults are at risk for inadequate dietary intakes which may lead to: – – – Poor nutritional status Decreased quality of life Functional disability Increased health care costs Greater risk for morbidity and mortality
Factors Affecting Nutrition Status n Physiological – Declining digestion and absorption – Reduced sensory perception n visual, olfactory, taste acuity, thirst – Anorexia of Aging n Physical – Chewing and swallowing difficulty – Affects on body systems n Integumentary (skin), renal, musculoskeletal, cardiovascular
Factors Affecting Nutrition Status (cont’d) n Psychological – – n Depression Loneliness Dementia Food likes/dislikes Social and Economical – – – Poverty Transportation availability Lack of knowledge of nutrition Inadequate cooking knowledge (men) ↓ Social support
Factors Affecting Nutrition Status (cont’d) n Cultural beliefs – Provision of culturally appropriate food and setting are both important (Wu and Barker, 2008) n Others – Medical conditions – Prescribed diets – Medication side effects
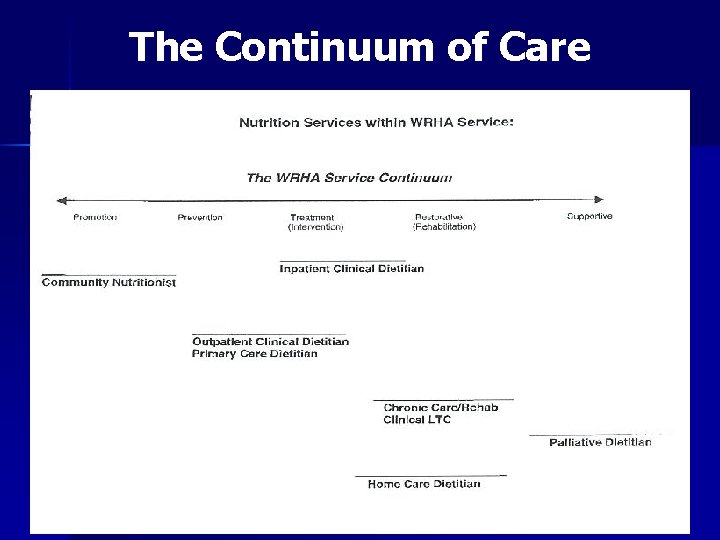
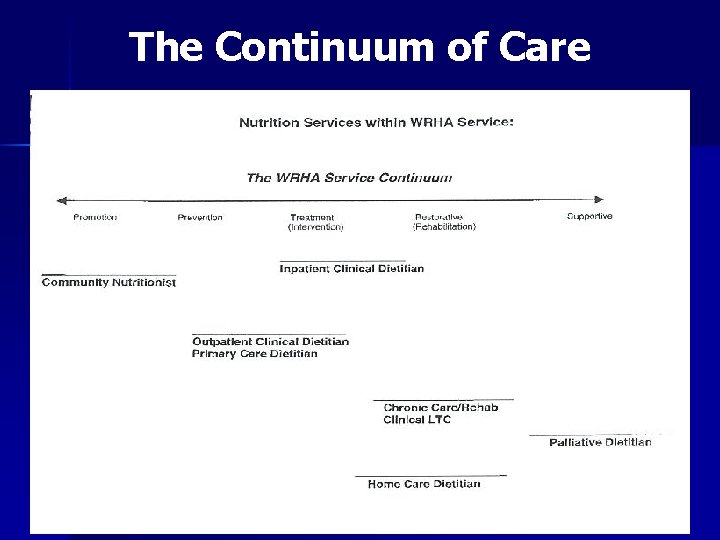
The Continuum of Care

Long-Term Care Setting

Malnutrition n Inappropriate amount of, or quality of nutrients comprising a healthy diet are not consumed for an extended period of time Undernutrition: n Often thought to be a problem of third world countries n Inadequate consumption, poor absorption, or excessive loss of nutrients Overnutrition: n Excessive intake of specific nutrients

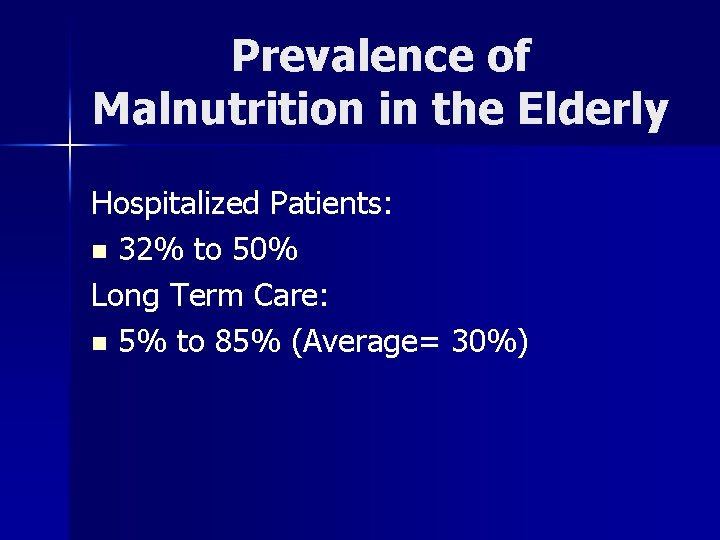
Prevalence of Malnutrition in the Elderly Hospitalized Patients: n 32% to 50% Long Term Care: n 5% to 85% (Average= 30%)

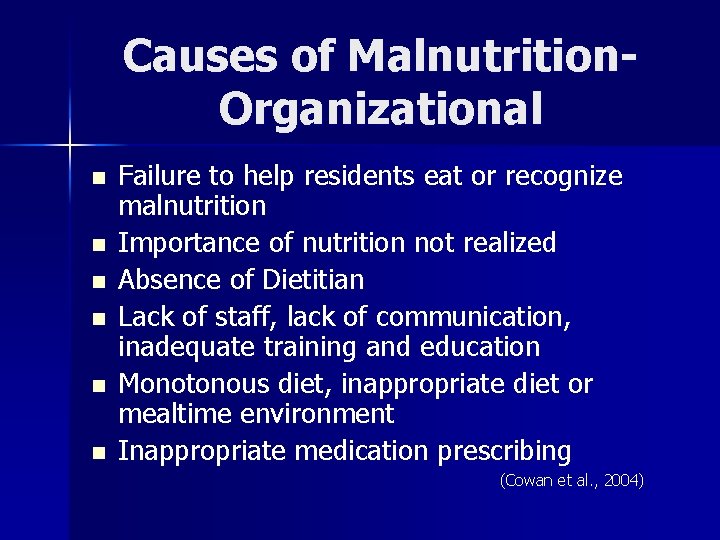
Causes of Malnutrition. Organizational n n n Failure to help residents eat or recognize malnutrition Importance of nutrition not realized Absence of Dietitian Lack of staff, lack of communication, inadequate training and education Monotonous diet, inappropriate diet or mealtime environment Inappropriate medication prescribing (Cowan et al. , 2004)
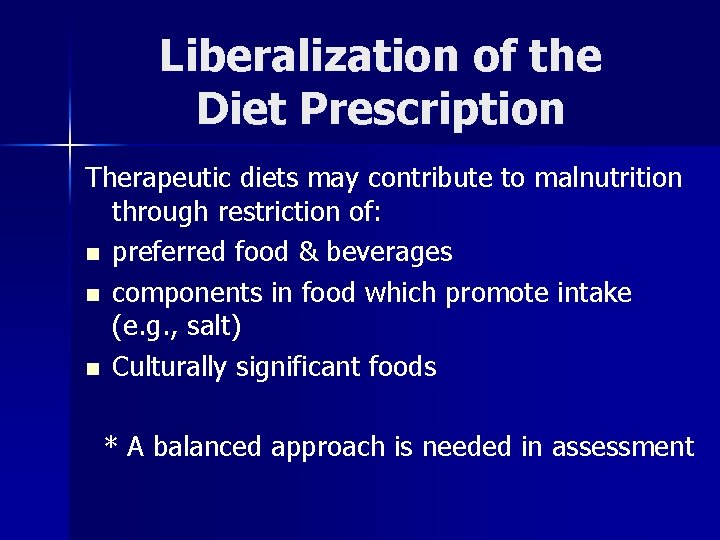
Liberalization of the Diet Prescription Therapeutic diets may contribute to malnutrition through restriction of: n preferred food & beverages n components in food which promote intake (e. g. , salt) n Culturally significant foods * A balanced approach is needed in assessment
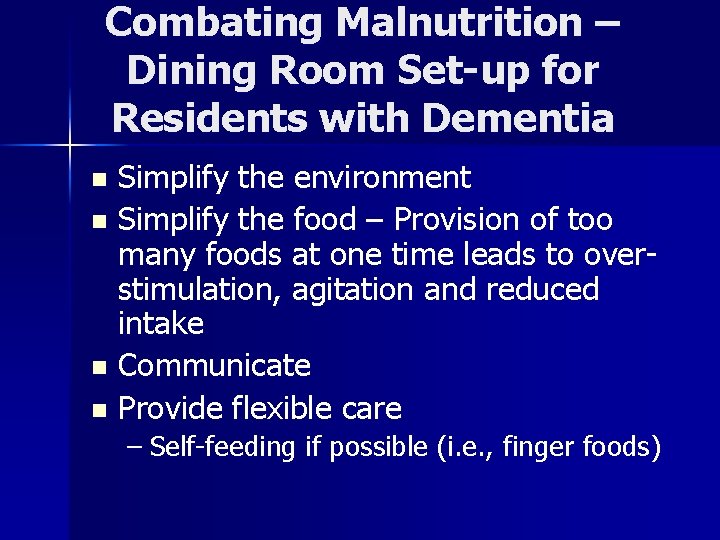
Combating Malnutrition – Dining Room Set-up for Residents with Dementia Simplify the environment n Simplify the food – Provision of too many foods at one time leads to overstimulation, agitation and reduced intake n Communicate n Provide flexible care n – Self-feeding if possible (i. e. , finger foods)
Nutrition Based Interventions Oral Nutritional Supplements n Changes to the meal pattern: n – Protein, energy enriched foods – Small, frequent meals (i. e. , between meal snacks) – Individualizing the meal pattern to accommodate social and cultural preferences
Nutritional Issues in Rural and Urban Communities
Prevalence of Malnutrition Undernutrition: n 5% to 20% prevalence of malnutrition n ~40% are at risk of malnutrition Overnutrition: n Increasing in all age groups n 25% obesity among adults 65+ and older

Baby Boomer and Nutrition Study 10 focus groups conducted in rural and urban Manitoba communities n 8 -12 participants/group recruited by MAFRI GO Team Representatives in specified areas n All participants completed a focus group questionnaire n Moderator facilitated the sessions for a 2 hour period n
Preliminary Key Findings n n n n Distrust in nutrition labeling Misleading advertising on packaging Importance of locally grown foods, their availability in local markets and supporting the local economy Portion control on packages Costs associated with healthier products Environmental concerns More nutrition education needed Importance of flavor, texture, taste and variety in food products
Nutritional Guidelines and Recommendations
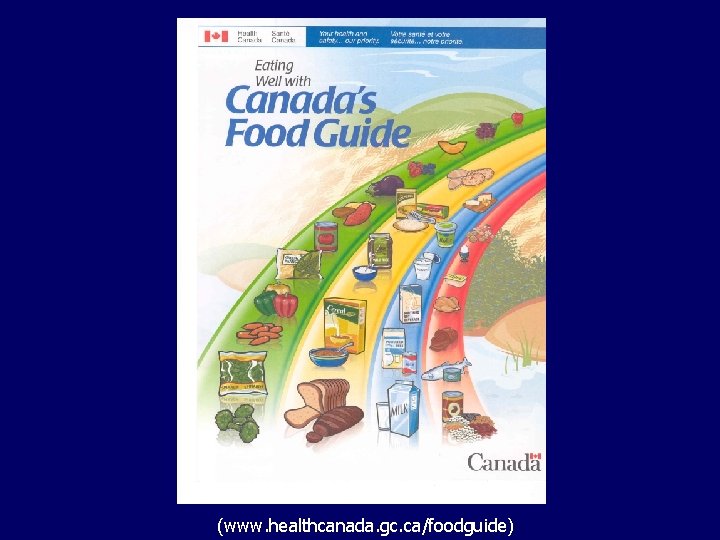
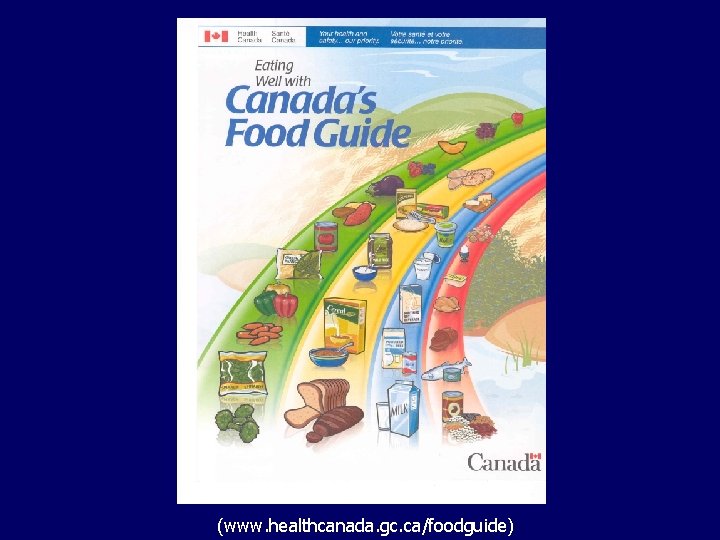
(www. healthcanada. gc. ca/foodguide)
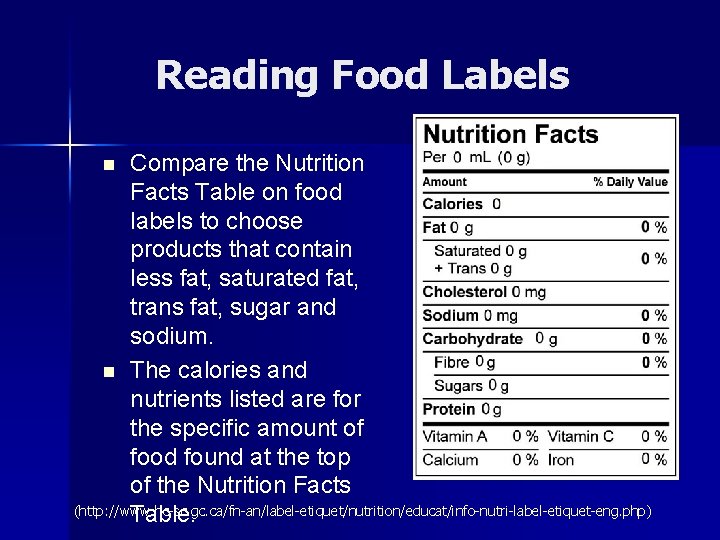
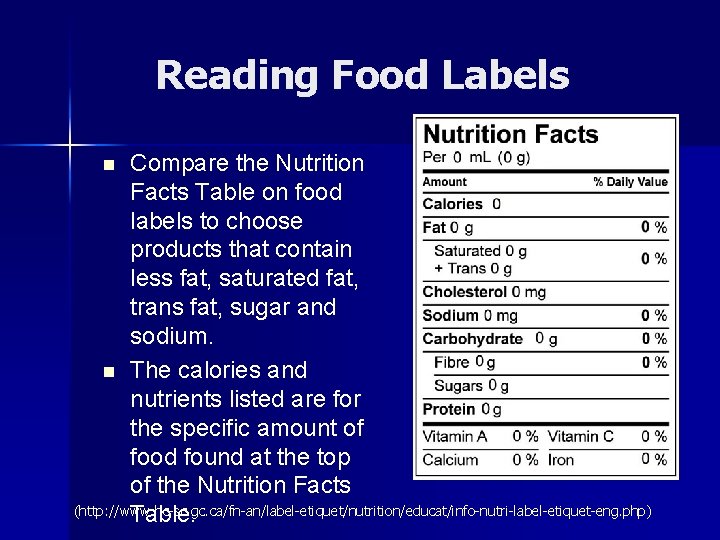
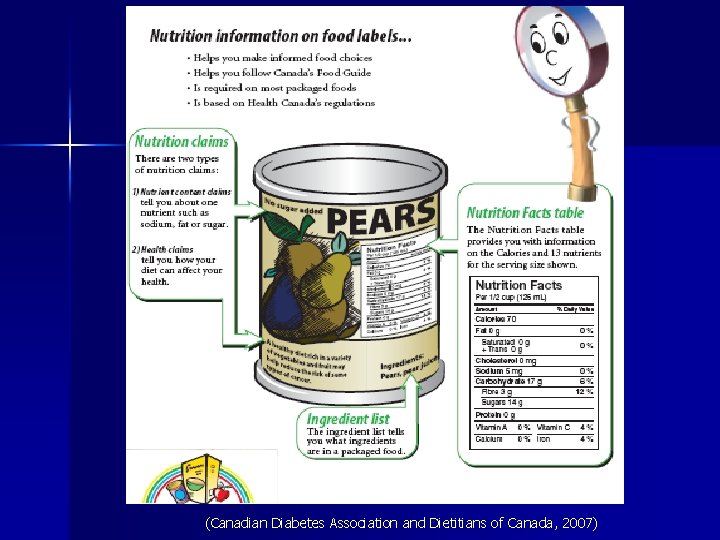
Reading Food Labels Compare the Nutrition Facts Table on food labels to choose products that contain less fat, saturated fat, trans fat, sugar and sodium. n The calories and nutrients listed are for the specific amount of food found at the top of the Nutrition Facts (http: //www. hc-sc. gc. ca/fn-an/label-etiquet/nutrition/educat/info-nutri-label-etiquet-eng. php) Table. n
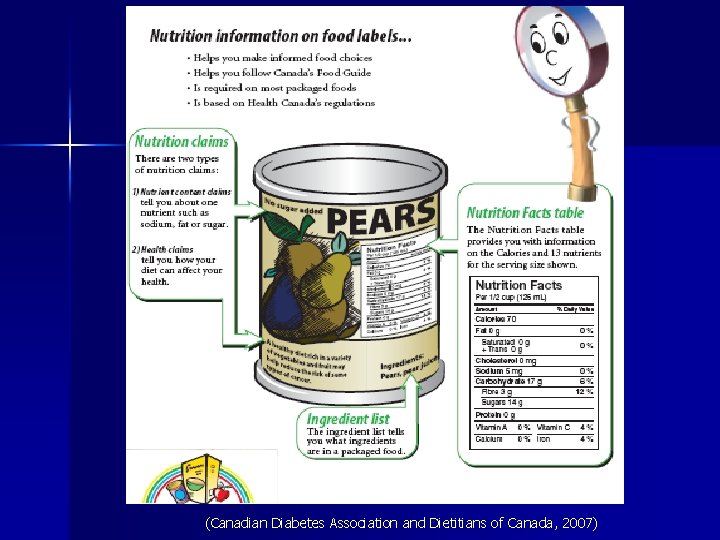
(Canadian Diabetes Association and Dietitians of Canada, 2007)
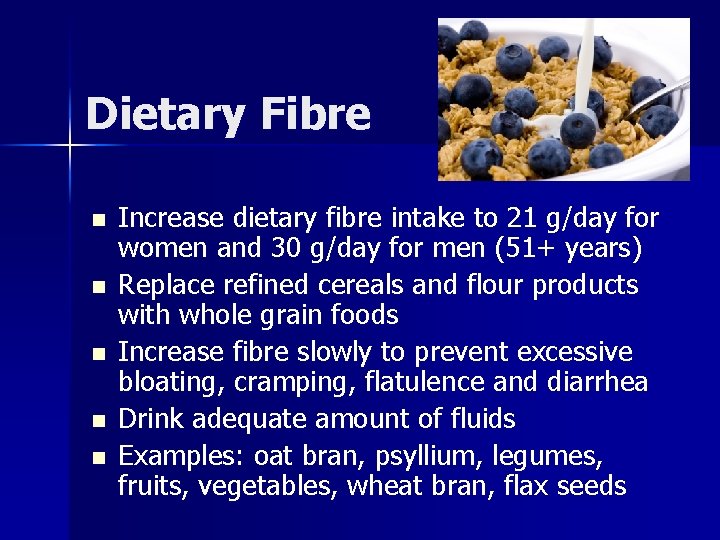
Dietary Fibre n n n Increase dietary fibre intake to 21 g/day for women and 30 g/day for men (51+ years) Replace refined cereals and flour products with whole grain foods Increase fibre slowly to prevent excessive bloating, cramping, flatulence and diarrhea Drink adequate amount of fluids Examples: oat bran, psyllium, legumes, fruits, vegetables, wheat bran, flax seeds
Fluid Intake Dietary Reference Intake (DRIs) (51+ years) n Females: 2. 7 L/day total water (2. 2 L = 9 cups total beverages) n Males: 3. 7 L/day total water (3. 0 L = 13 cups total beverages) n NOTE: these values may be difficult to achieve for older adults due to reduced food intake. Aim for 6 -8 cups per day.
Vitamins and Minerals n Vitamin D – Current DRI’s are: n Males and Females 51 -70 years: 10 ug (400 IU) n Males and Females 70 +years: 15 ug (600 IU) – Canada’s Food Guide recommends an additional daily vitamin D supplement of 10 ug (400 IU) for everyone over the age of 50 – New research is demonstrating a need for increasing vitamin D requirements for older adults
Canada’s Physical Activity Guide to Healthy Active Living for Older Adults (www. phac-aspc. gc. ca/pau-uap/paguide/older/index. html)
Take Home Messages n n Nutrition is one of the major determinants of healthy aging Individualized care – Ensuring effects of aging are considered n n High quality diet is important across the lifespan Consume a variety of nutrient dense foods from the four food groups Nutrient supplementation with low-dose multivitamin and mineral supplements can be useful in achieving recommended intake levels Enjoy your meals!
Resources n Dietitians of Canada – www. dietitians. ca n Eating Well with Canada’s Food Guide – www. hc-sc. gc. ca/fn-an/food-guide-aliment/index-eng. php n Canada’s Physical Activity Guide for Older Adults – www. phac-aspc. gc. ca/pau-uap/fitness/pdf/guide_older_e. pdf n Nutrition Labelling – www. healthcanada. gc. ca/nutritionlabelling n Alzheimer Society of Canada – www. alzheimer. ca/english/care/dailyliving-mealtime. htm
“If we knew what it was we were doing, it would not be called research, would it? ” Albert Einstein
Any Questions?
 Life is older than the trees
Life is older than the trees Mental health and older adults
Mental health and older adults Mental health and older adults
Mental health and older adults Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to Shingles older adults
Shingles older adults Older adults
Older adults Covids older adults
Covids older adults Older adults mental health
Older adults mental health Dynamic stretching for older adults
Dynamic stretching for older adults Younger shorter older old
Younger shorter older old Community nutrition assessment
Community nutrition assessment Community nutrition program planning
Community nutrition program planning Community problem
Community problem Ethical and legal issues in community health nursing
Ethical and legal issues in community health nursing Older persons act norms and standards
Older persons act norms and standards Downsizing and divesting older business
Downsizing and divesting older business Module 11 studying the brain and older brain structures
Module 11 studying the brain and older brain structures Trends in community development
Trends in community development Web accessibility for older users
Web accessibility for older users Syncope in the older patient is
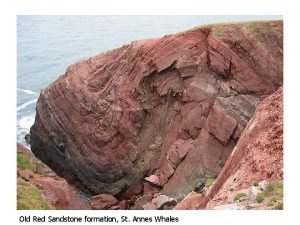
Syncope in the older patient is Td st annes
Td st annes Intellectual development in older adulthood
Intellectual development in older adulthood Older individuals who are blind program
Older individuals who are blind program As people grow older
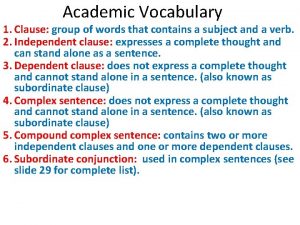
As people grow older Juan continued playing although he injured his knee
Juan continued playing although he injured his knee The older brother in the prodigal son
The older brother in the prodigal son Nipołomice
Nipołomice Sos spelling for older students
Sos spelling for older students My rotten redheaded older brother
My rotten redheaded older brother Ajayan is ten years older than vijayan
Ajayan is ten years older than vijayan Future medical
Future medical Hoa/receive/letter/her friend nien/today
Hoa/receive/letter/her friend nien/today Moses older sister
Moses older sister Superlativo de helado
Superlativo de helado The virtues of growing older
The virtues of growing older Sos spelling for older students
Sos spelling for older students Taller younger sister shorter older brother
Taller younger sister shorter older brother 59 swans poem
59 swans poem Pseudostratified vs simple columnar
Pseudostratified vs simple columnar What is parvana's mother's name
What is parvana's mother's name