Neonatal Medication and Fluid Calculations Sneha Sood MD


- Slides: 23
Neonatal Medication and Fluid Calculations Sneha Sood, MD
Fluid Compartments Extracellular (ECF) = intravascular and interstitial Intracellular (ICF) = within cells Total body water (TBW) = ECF + ICF
Body Composition Total body water preterm>adult (preterm 80% BW, term 70 -75% BW, adult 50 -60% BW) Greater ECF in neonate (40% vs 20%) ICF increases with proliferation of cells and maturation of organs
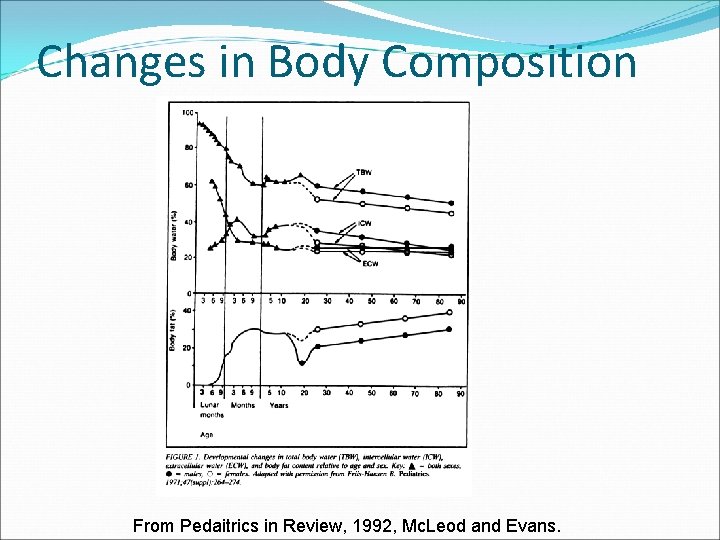
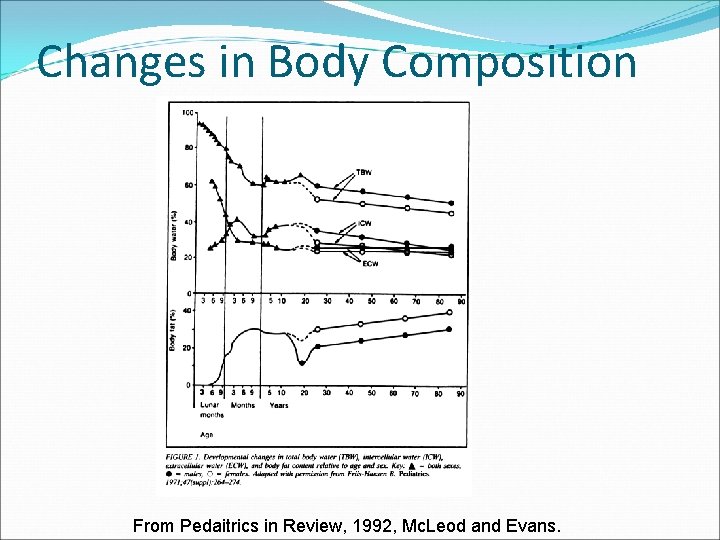
Changes in Body Composition From Pedaitrics in Review, 1992, Mc. Leod and Evans.
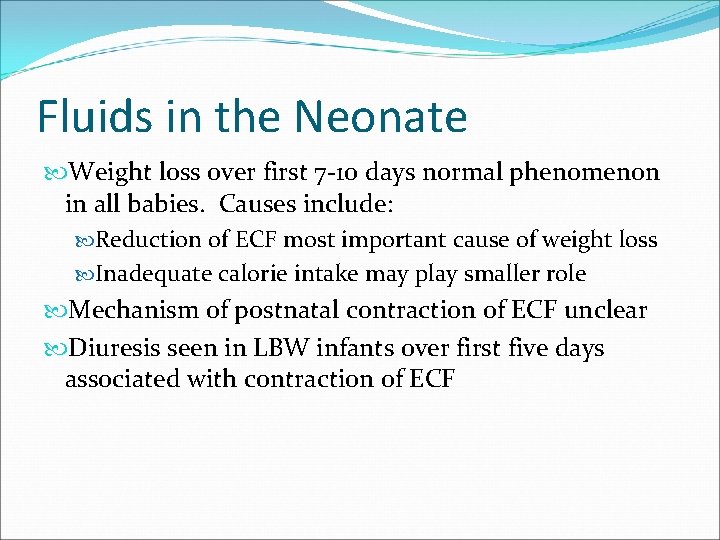
Fluids in the Neonate Weight loss over first 7 -10 days normal phenomenon in all babies. Causes include: Reduction of ECF most important cause of weight loss Inadequate calorie intake may play smaller role Mechanism of postnatal contraction of ECF unclear Diuresis seen in LBW infants over first five days associated with contraction of ECF
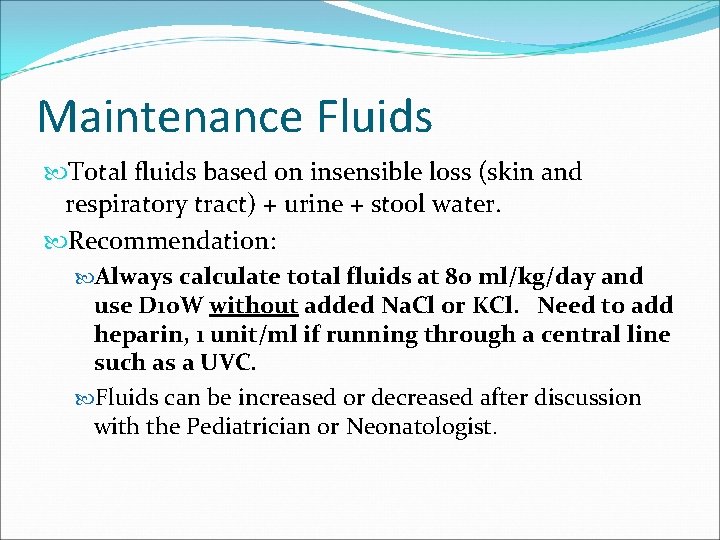
Maintenance Fluids Total fluids based on insensible loss (skin and respiratory tract) + urine + stool water. Recommendation: Always calculate total fluids at 80 ml/kg/day and use D 10 W without added Na. Cl or KCl. Need to add heparin, 1 unit/ml if running through a central line such as a UVC. Fluids can be increased or decreased after discussion with the Pediatrician or Neonatologist.
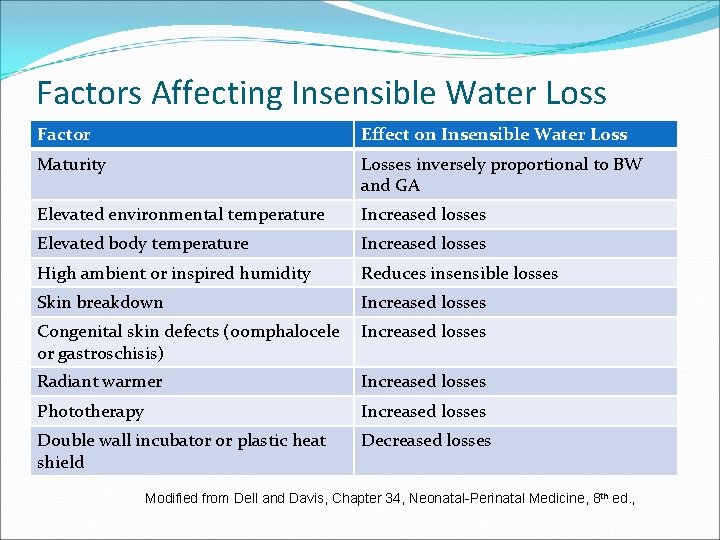
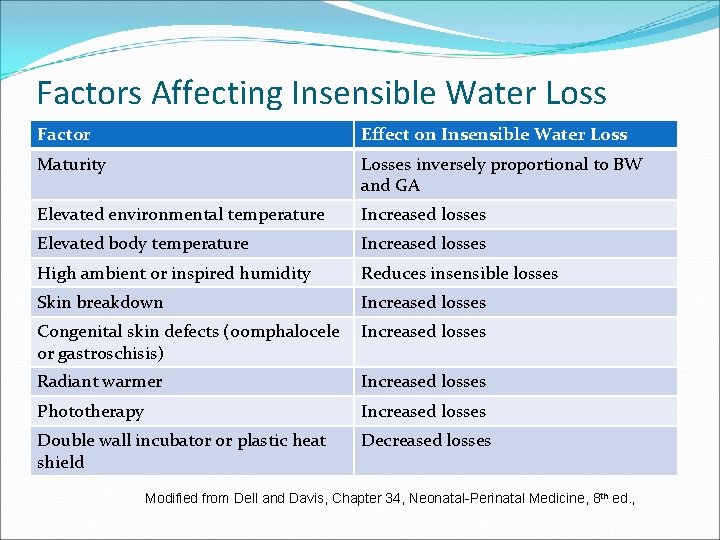
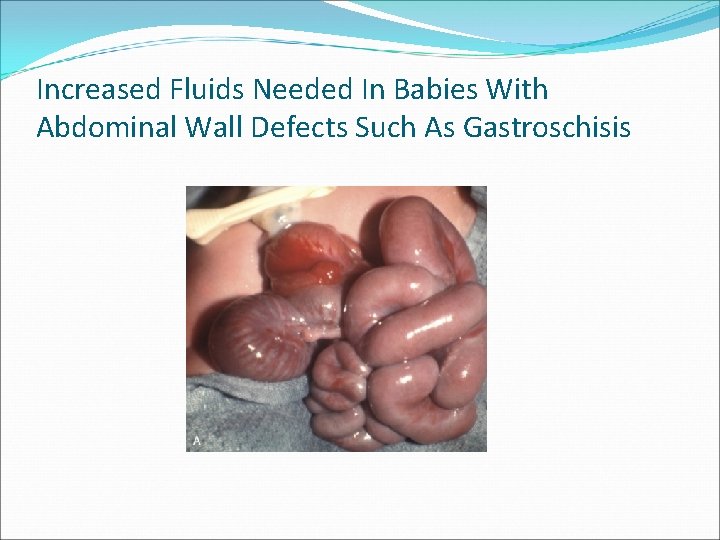
Factors Affecting Insensible Water Loss Factor Effect on Insensible Water Loss Maturity Losses inversely proportional to BW and GA Elevated environmental temperature Increased losses Elevated body temperature Increased losses High ambient or inspired humidity Reduces insensible losses Skin breakdown Increased losses Congenital skin defects (oomphalocele or gastroschisis) Increased losses Radiant warmer Increased losses Phototherapy Increased losses Double wall incubator or plastic heat shield Decreased losses Modified from Dell and Davis, Chapter 34, Neonatal-Perinatal Medicine, 8 th ed. ,
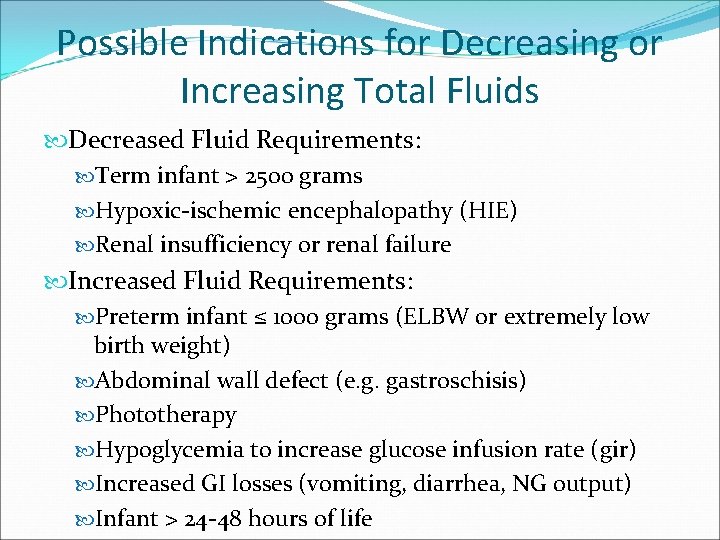
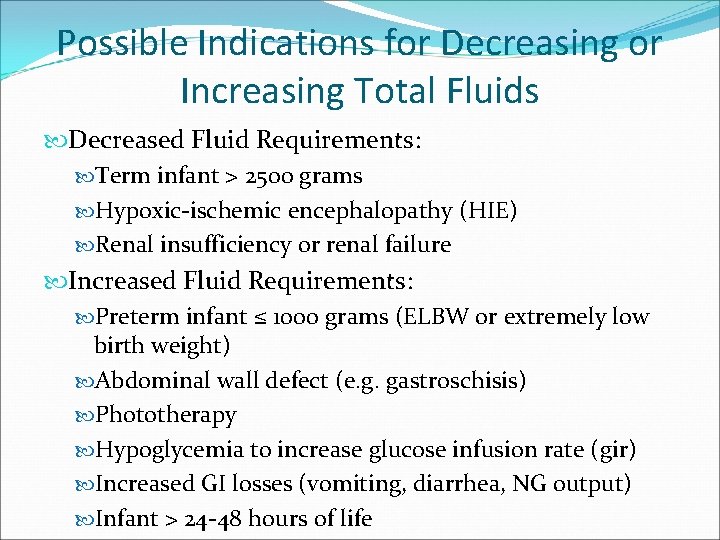
Possible Indications for Decreasing or Increasing Total Fluids Decreased Fluid Requirements: Term infant > 2500 grams Hypoxic-ischemic encephalopathy (HIE) Renal insufficiency or renal failure Increased Fluid Requirements: Preterm infant ≤ 1000 grams (ELBW or extremely low birth weight) Abdominal wall defect (e. g. gastroschisis) Phototherapy Hypoglycemia to increase glucose infusion rate (gir) Increased GI losses (vomiting, diarrhea, NG output) Infant > 24 -48 hours of life
Always wait for physician order before altering total fluids to anything other than 80 ml/kg/day

Babies with HIE are kept fluid restricted
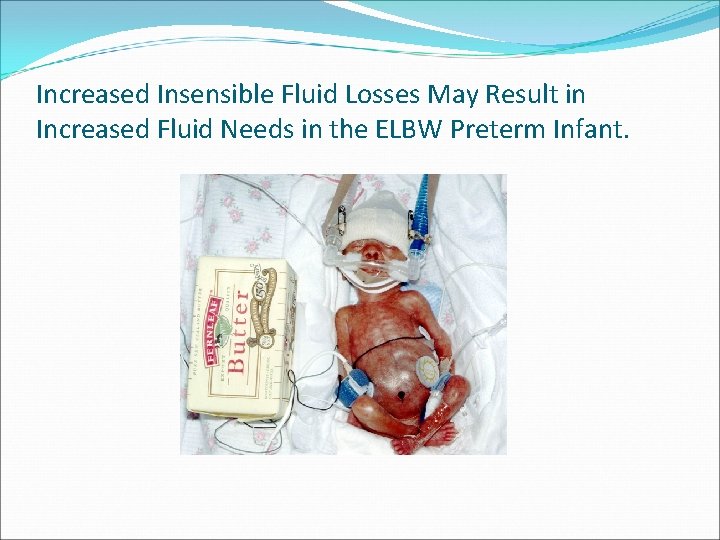
Increased Insensible Fluid Losses May Result in Increased Fluid Needs in the ELBW Preterm Infant.
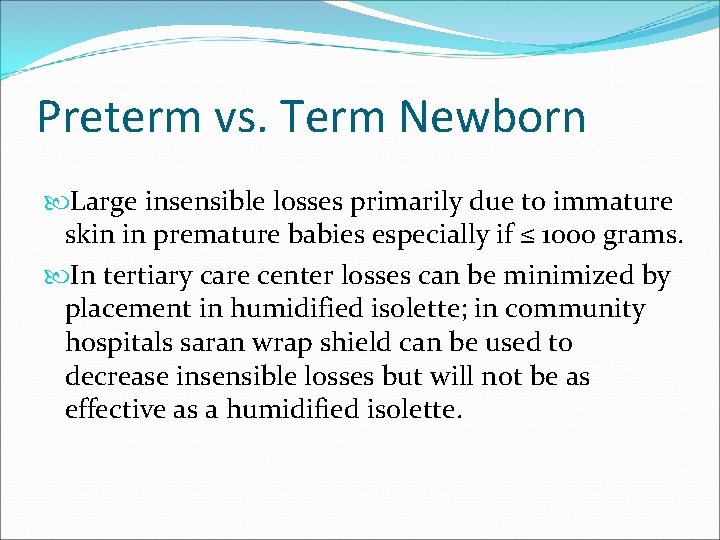
Preterm vs. Term Newborn Large insensible losses primarily due to immature skin in premature babies especially if ≤ 1000 grams. In tertiary care center losses can be minimized by placement in humidified isolette; in community hospitals saran wrap shield can be used to decrease insensible losses but will not be as effective as a humidified isolette.
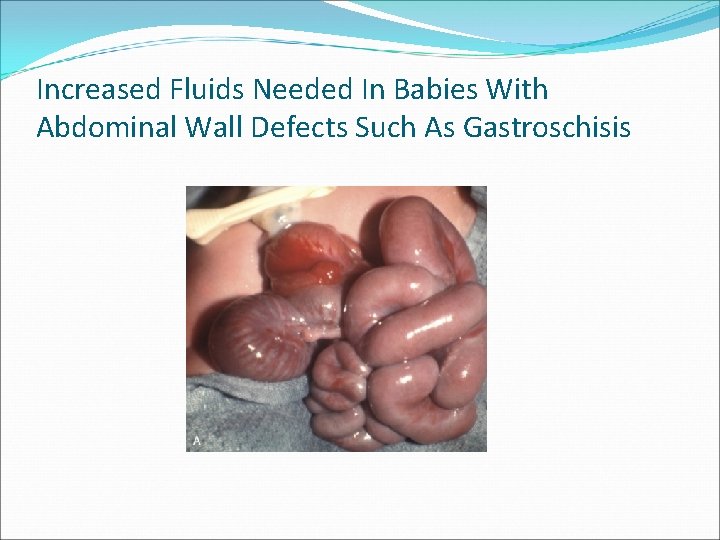
Increased Fluids Needed In Babies With Abdominal Wall Defects Such As Gastroschisis
Dextrose Concentration D 10 W is the standard dextrose concentration in newborns Glucose Infusion Rate (GIR) expressed as mg/kg/min Ideal GIR 4 -8 mg/kg/min In hypoglycemic infants higher GIR may be necessary; this can be achieved by increasing the dextrose concentration or by increasing total fluids. Maximum dextrose concentration in peripheral IV fluids = D 12. 5 ELBW babies may require lower dextrose concentration due to hyperglycemia because of increased fluid requirements due to high insensible losses.
Electrolytes No maintenance Na, K, or Cl necessary during the first 1 -2 days of life. Generally electrolytes do not need to be checked until 24 hours of life. More frequent monitoring of electrolytes may be required in premature babies or sick babies with excessive fluid shifts.
Urine Output Urine output is a measure of fluid and electrolyte balance Adequate urine output in the first few days of life: 1 -3 ml/kg/hour
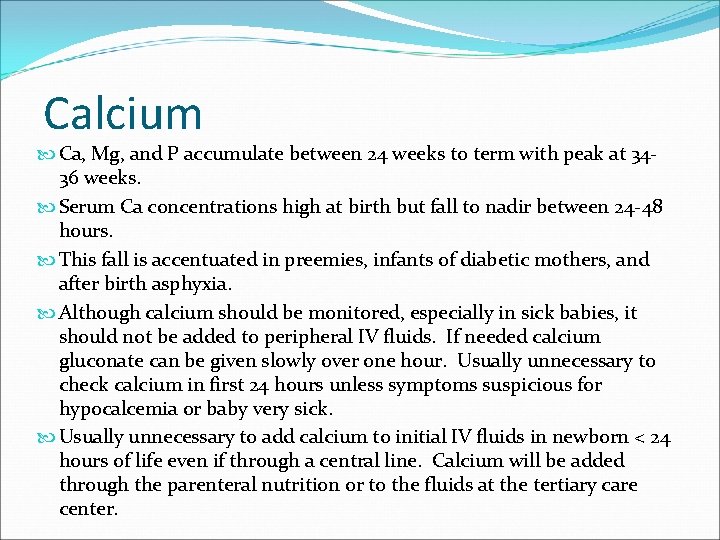
Calcium Ca, Mg, and P accumulate between 24 weeks to term with peak at 3436 weeks. Serum Ca concentrations high at birth but fall to nadir between 24 -48 hours. This fall is accentuated in preemies, infants of diabetic mothers, and after birth asphyxia. Although calcium should be monitored, especially in sick babies, it should not be added to peripheral IV fluids. If needed calcium gluconate can be given slowly over one hour. Usually unnecessary to check calcium in first 24 hours unless symptoms suspicious for hypocalcemia or baby very sick. Usually unnecessary to add calcium to initial IV fluids in newborn < 24 hours of life even if through a central line. Calcium will be added through the parenteral nutrition or to the fluids at the tertiary care center.
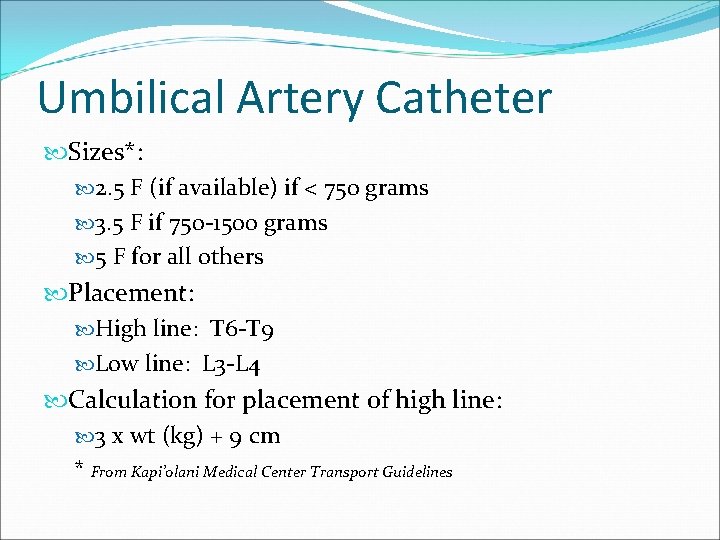
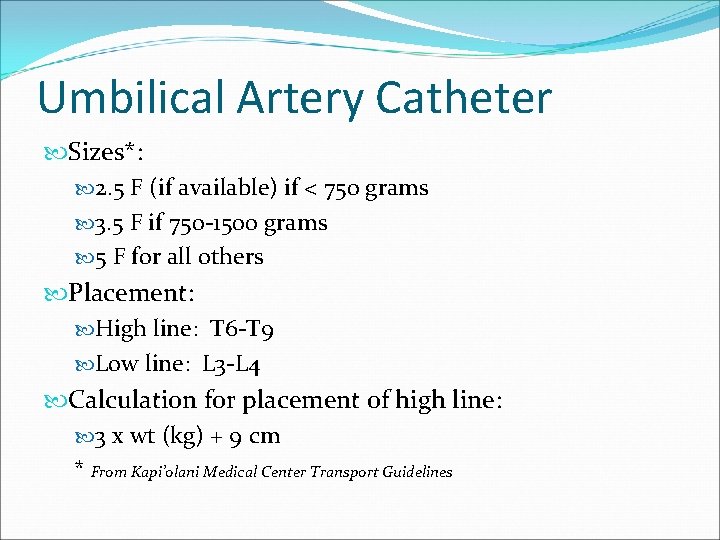
Umbilical Artery Catheter Sizes*: 2. 5 F (if available) if < 750 grams 3. 5 F if 750 -1500 grams 5 F for all others Placement: High line: T 6 -T 9 Low line: L 3 -L 4 Calculation for placement of high line: 3 x wt (kg) + 9 cm * From Kapi’olani Medical Center Transport Guidelines
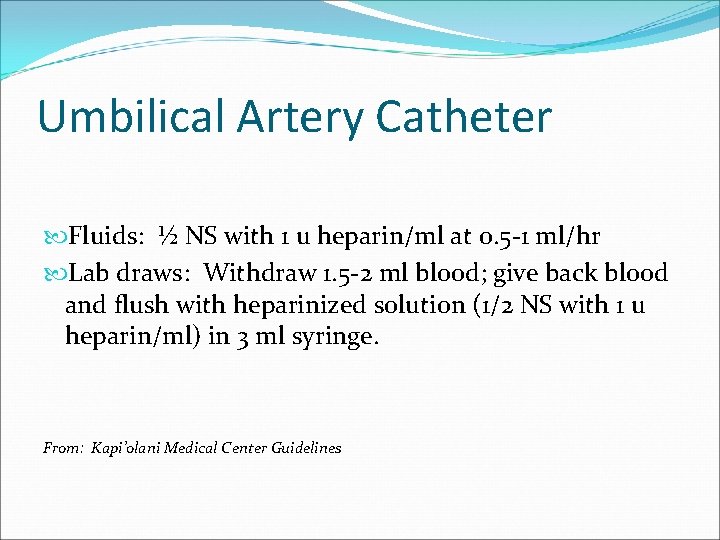
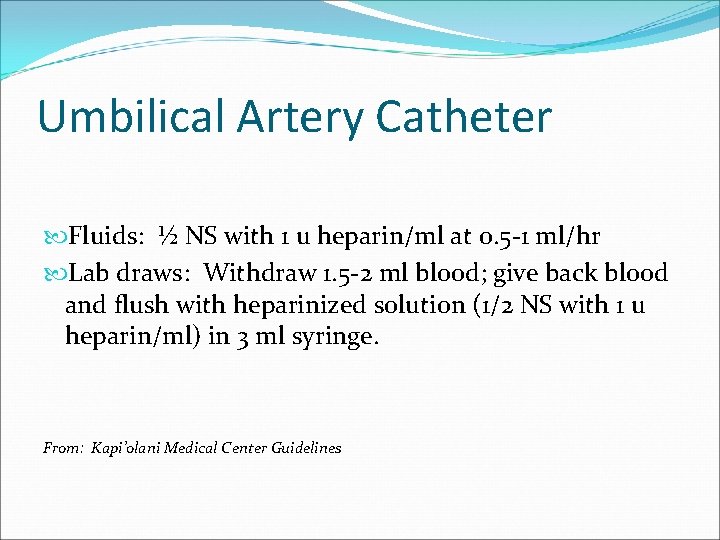
Umbilical Artery Catheter Fluids: ½ NS with 1 u heparin/ml at 0. 5 -1 ml/hr Lab draws: Withdraw 1. 5 -2 ml blood; give back blood and flush with heparinized solution (1/2 NS with 1 u heparin/ml) in 3 ml syringe. From: Kapi’olani Medical Center Guidelines
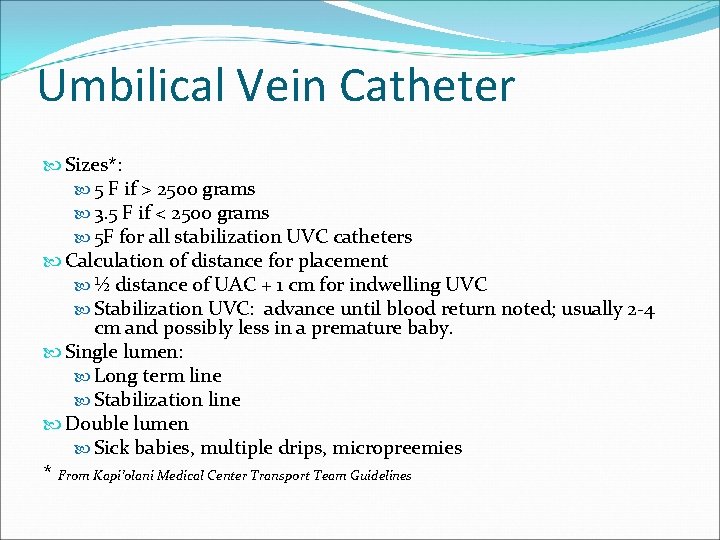
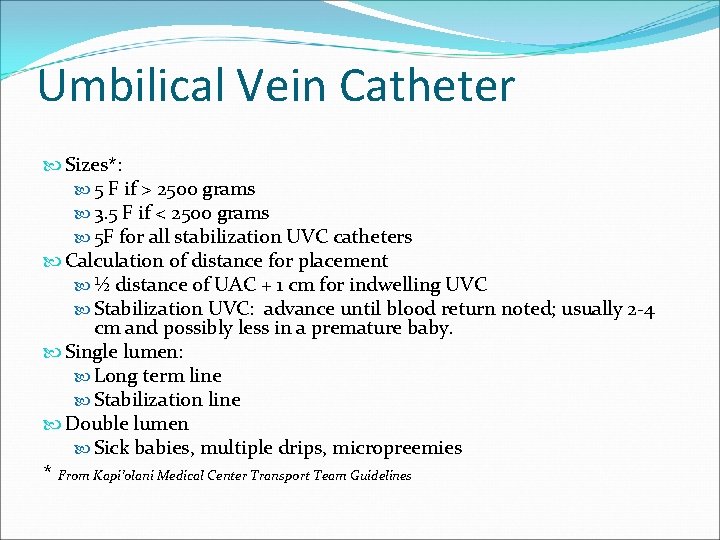
Umbilical Vein Catheter Sizes*: 5 F if > 2500 grams 3. 5 F if < 2500 grams 5 F for all stabilization UVC catheters Calculation of distance for placement ½ distance of UAC + 1 cm for indwelling UVC Stabilization UVC: advance until blood return noted; usually 2 -4 cm and possibly less in a premature baby. Single lumen: Long term line Stabilization line Double lumen Sick babies, multiple drips, micropreemies * From Kapi’olani Medical Center Transport Team Guidelines
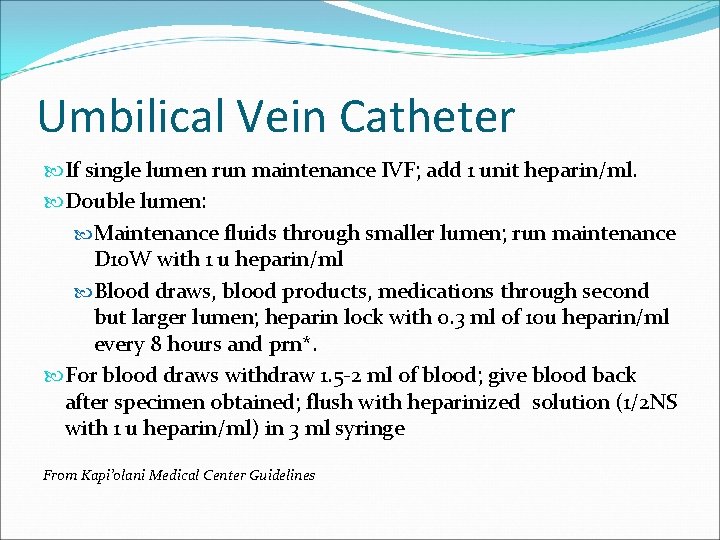
Umbilical Vein Catheter If single lumen run maintenance IVF; add 1 unit heparin/ml. Double lumen: Maintenance fluids through smaller lumen; run maintenance D 10 W with 1 u heparin/ml Blood draws, blood products, medications through second but larger lumen; heparin lock with 0. 3 ml of 10 u heparin/ml every 8 hours and prn*. For blood draws withdraw 1. 5 -2 ml of blood; give blood back after specimen obtained; flush with heparinized solution (1/2 NS with 1 u heparin/ml) in 3 ml syringe From Kapi’olani Medical Center Guidelines
Umbilical Catheters While umbilical lines can be pulled back, never advance an umbilical catheter that has slipped out—use a clean line instead unless still under sterile prep and drape!

 Neonatal resuscitation definition
Neonatal resuscitation definition Sneha rajiv
Sneha rajiv Dopamine iv dose
Dopamine iv dose Nursing dosage calculations cheat sheet
Nursing dosage calculations cheat sheet Dose calculation formula
Dose calculation formula Parenteral medication formula
Parenteral medication formula Amoxicillin pediatric dosing chart
Amoxicillin pediatric dosing chart Structural steel connection calculations calculations
Structural steel connection calculations calculations Meera sood
Meera sood Body fluid compartments
Body fluid compartments Extracellular fluid and interstitial fluid
Extracellular fluid and interstitial fluid Sneha fotedar
Sneha fotedar Gmail
Gmail House of siby
House of siby Viscoseal
Viscoseal Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Fluid statics deals with fluid at rest
Fluid statics deals with fluid at rest Ecf icf and interstitial fluid
Ecf icf and interstitial fluid Hypoosmotic
Hypoosmotic Fluid kinematics example
Fluid kinematics example Shifting dullness procedure
Shifting dullness procedure Yorkshire neonatal network
Yorkshire neonatal network Lenticulo
Lenticulo Circulação neonatal
Circulação neonatal