Maternal Child health services MCH services Dr Muslim


- Slides: 22
Maternal & Child health services MCH services Dr. Muslim N. Saeed Family & Community Medicine Dept. Monday, February 26 th, 2019
Maternal & Child Heath (MCH) (including family planning): Mothers and children are both vulnerable groups of the community. Women in the childbearing period (15 -49 years) constitute about 25% of the population. Children on the other hand constitute about 40% to 45% of the population in developing countries. This group is characterized by relative high mortality and morbidity rates. MCH includes: 1 - Maternal care. 2 - Child care 3 - Family planning
MCH Definition: It is that aspect of health which is concerned with the special needs & problems of mother & child (problems that arise from the process of human reproduction growth & development), It includes care for pregnant women and family planning, growth monitoring and development of infant and children. MCH services are designed for the care of the mothers from time of conception to ensure that they have normal pregnancy, normal delivery and proper care in the postnatal period. They also include protection and supervision of health of children from time of conception to the time they enter the school.
General Objective of MCH: �To improve the health status of the largest and most vulnerable sector of the population by providing the best health care available. �The objectives of MCH services: o To ensure desired pregnancy. o To achieve the best possible outcome for the baby and the mother i. e. the services are unique in that they simultaneously provide care for two important clients, the mother and the fetus, balancing the needs of both.
o To prevent child health problems and to reduce the risk of adult health problems i. e. (Healthy child means healthy future adult). o Prevention and control of health hazards to children and females in child bearing age and to minimize morbidity and mortality. o Treatment of common problem and diseases arising in this period. o To optimize the normal developmental process to allow the child to achieve his fullest potential. o Rehabilitation of handicapped children. o Ensure secure relationship between parents themselves and parents with their children.
Importance of MCH services �Most of the problems of MCH are preventable. �Provide services to about two third of population. �Improve socioeconomic development. �Mother & children are high risk group; they are delicate & vulnerable group with special needs. �Good site for training and health education. �Important for future of the nations, since mothers are responsible for health promotion and culture of children and family welfare , and so must be healthy and aware of requirements of health
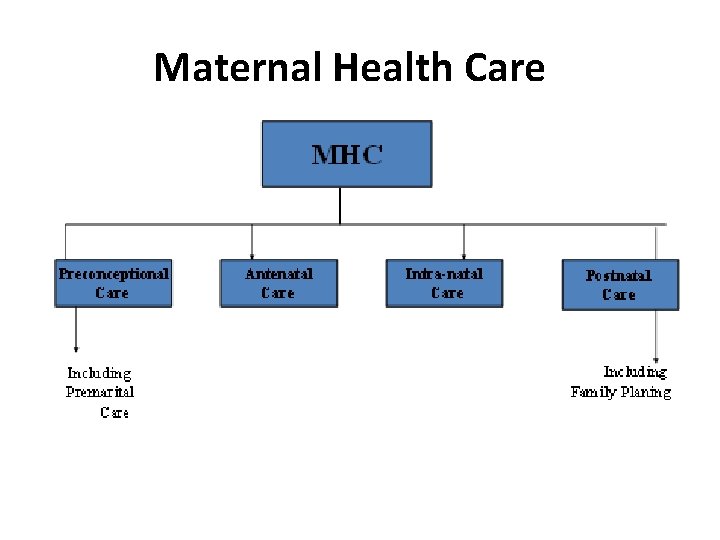
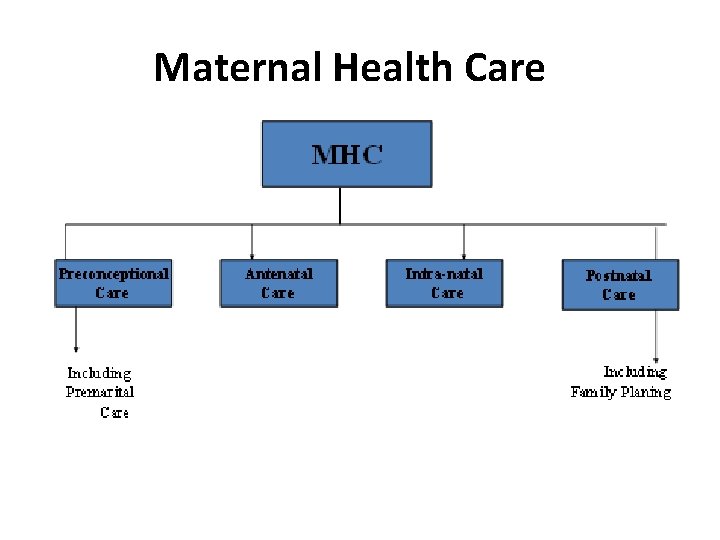
Maternal Health Care
Phases of maternal care: I. Pre-conception care: It is continued care for female, through all stages of growth and development, & until the time of conception (It is care of mother before pregnancy). Components of Pre-conception Care: 1) Health promotion and attention to health related behavior before conception such as smoking , alcohol consumption , drug abuse. 2) Regular health assessment for early case detection and management, and prevention of its complications: e. g. : �Sexually transmitted diseases. �diabetes mellitus & impaired glucose tolerance �pulmonary T. B �urinary tract infection
�nutritional problems �rheumatic heart diseases �Endocrinological problems (e. g. thyroid problem) 3) Health education of young girls e. g. determinants and requirement of health, family planning…. . 4) Premarital care (for both partners).
II. Premarital Care: Health care given to girls and boys before they get married and is an essential part of adolescent health care. It include: �Health education concerning: Proper nutrition Healthy lifestyle, Safe sex, sexually transmitted diseases. History taking: regarding hereditary diseases. �Physical examination: for evaluation of health status and nutritional status, and screening of suspected cases. �Investigation includes: Blood for: ABO group &RH, Hb% level, VDRL, HIV test, test for hepatitis Chest X ray: to exclude pulmonary T. B. �Preventive services (immunization): Rubella vaccine is important before the female become pregnant (pregnancy should be avoided for the next 3 months after vaccination). �Counseling: Genetic counseling, family planning counseling (if requested by couples).

III. Antenatal Care ( prenatal care ) ANC: is complete health supervision of the pregnant women in order to maintain, promote & protect health & wellbeing of the mother, fetus and the newborn infant. General objectives of antenatal care: “The general objective of ANC is to prepare the mother both physically and psychologically to give birth to a healthy newborn and to be able to care for it. ”
Objectives of antenatal care: �Help to ensure best possible health status for mother & fetus �Early detection & timely referral of high risk pregnancy. �Education of the mother about : o Physiology of pregnancy. Adequate nutrition. Alarming symptoms& signs. o Infant care. Breast feeding. Child care. �Registration: During the booking visit, and record keeping. �Medical examination and investigations; for both the booking visit and continuing visits. �Health education. �Immunization. �Supplementations. �Clinical services. �Social services (outreach services).
When the Antenatal care started? Antenatal care started as soon as pregnancy is confirmed Confirmation of pregnancy: �History of missed period in otherwise normal cycle Symptoms of pregnancy: nausea, vomiting heartburn, hyperacidity. �Physical examination: 1) Breast changes 2) Pelvic changes 3) Abdominal changes �Investigation: 1) Urine examination ; pregnancy test: for detection of human chorionic gonadotropin (h. CG ), which is more accurate on first morning specimen & to be done after 7 -10 days from last missed menstrual period. 2) serum β – h. CG which is accurate within 10 – 14 days of conception or approximately within the date of menstrual cycle
Standards of ANC: (initial visit and subsequent visits) The initial visit (first visit) : The first antenatal visit should take place as early as possible during the first trimester , as soon as the pregnancy is confirmed. The initial visit should include: 1. Booking procedures (registration). 2. Physical examination. 3. Investigation. 4. Health education. Instructions: including frequency of visits
Registration (Booking): When primigravida visits MCH center for the first time a health record [file with serial number] is initiated to register all events concerning present pregnancy & it`s outcome. o Importance of record - keeping: 1. To be used as reference data in next pregnancies 2. For collection of statistical data used as health indicator for assessment & evaluation of MCH services.
Booking procedures: History: (personal, family, medical, drug , allergy, blood transfusion. , surgical, menstrual, obstetrical ) �Personal history: name, age, occupation, level of education (of both parents), address, duration of marriage, Consanguinity, Potentially harmful habits ( e. g smoking , alcohol ) �Family history: D. M, HP, multiple pregnancy, congenital anomalies, mental retardation �Medical history: Diseases: DM, HP, UTI, Heart diseases, Infectious disease �Drugs or allergy �History of blood transfusion, Rh incompatibility �Surgical history: history of previous operation �Menstrual history: age of menarche, regularity , length of cycle, usual duration of each period , amount of blood loss, last menstrual period LMP, & expected day of delivery EDD is calculated accordingly , use of contraception , if she is lactating now
Obstetrical history: history of all previous pregnancies in chronological order including: - Number of pregnancies - Date of birth or termination of each pregnancy - Duration of each pregnancy - Outcome of each pregnancy ( abortion or stillbirth or live birth) - Type of delivery: normal , assisted or caesarian section (CS) - Presentation - Complications during: pregnancy, labour, and postnatal. - Weight of newborn - Place of delivery : home , or hospital - Birth attendant : doctor , nurse, midwife , or traditional birth attendant ( TBA )
2) Physical examination: �General (systemic) - Vital signs: pulse, temperature, blood pressure (Bp ) which is best measured with the client sitting or in recumbent position (not lying). - Weight (with indoor clothing). - Height (without shoes). - Body mass index BMI is calculated = weight (kg) height (m) 2. - Pallor. - Jaundice. �Head & neck including thyroid gland (goiter). �Chest & heart examination. �Breast examination. �Lower limb edema. �Skeletal or neurological abnormalities.
�Abdominal (Obstetric) examination. - Inspection: �Size & shape of abdomen, Scars of previous operations. �Signs of pregnancy (linea nigra, striae gravidarm). �Fetal movement, dilated veins, Edema. - Palpation: Tenderness, rigidity or any palpable organs, Fundal level. - Auscultation: fetal heart, from 10 weeks fetal heart rate detector is used. From 20 weeks Pinard fetal stethoscope is used. - Pelvic examination: vaginal examination is not recommended routinely unless in cases of vaginal discharge.

3) Investigation: Blood analysis: complete blood picture. - ABO grouping & Rh. - Screening for diabetes, RBS, 2 HPP (2 hours post prandial), GTT if needed. - VDRL �Urine analysis : GUE for albumin urea , microscopic examination for bacteriurea & pus cell. culture & sensitivity (C&S) if recommended �Arrange for pelvic ultrasound: if the women is not sure of gestational age or if her period is not reliable.
Schedule of antenatal care visits: For low – risk pregnancy the following schedule of visits should be followed: -up to 28 weeks gestation every 4 weeks -28 – 36 weeks gestation every 2 weeks -After 36 weeks gestation every one week �In a low – risk pregnancy with no complication , a minimum number of antenatal visits (recommended by the Royal College of Obstetricians & Gynecologists) is five visits, including the booking visit, is acceptable. The quality of care is more important than the frequency of visits.
End
 Mch indicators full form
Mch indicators full form Transovarial transmission คือ
Transovarial transmission คือ Extranuclear inheritance
Extranuclear inheritance History of maternal and child health
History of maternal and child health National programs
National programs Z score for malnutrition
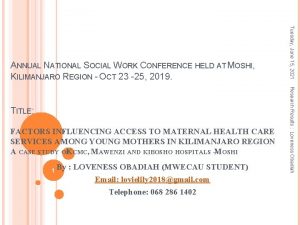
Z score for malnutrition Factors influencing maternal health
Factors influencing maternal health What is maternal health
What is maternal health Maternal and infant health disparities
Maternal and infant health disparities Menghitung mcv mch mchc
Menghitung mcv mch mchc Indicators of mch
Indicators of mch Mch indicators full form
Mch indicators full form übad
übad Fsu computer science
Fsu computer science Menghitung mcv mch mchc
Menghitung mcv mch mchc Northbridge que es
Northbridge que es Mch blood test high
Mch blood test high Mch high
Mch high Rumus mch
Rumus mch 7/8 - 45%
7/8 - 45% Mch card
Mch card Trofozoiet
Trofozoiet Muslim housing services
Muslim housing services