Maternal Health Interventions NRHMRCHII Maternal Health Division Ministry











- Slides: 32
Maternal Health Interventions NRHM/RCH-II Maternal Health Division Ministry of Health & Family Welfare Government of India

GOALS OF NRHM Universal Health Care • access • affordability • equity • quality

Maternal Mortality. Magnitude of the Problem • About 30 million pregnancies occur every year in India. • 27 million deliveries • 15% of these are likely to develop complications. • Complications cannot be predicted. • 77, 000 avoidable maternal deaths per year
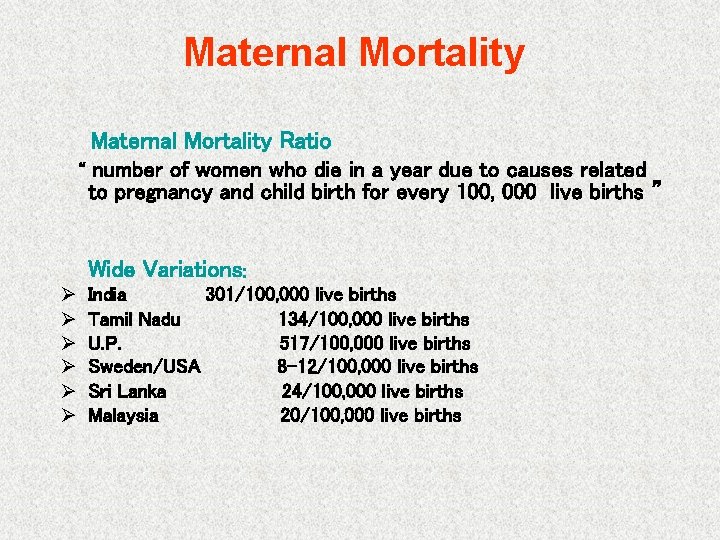
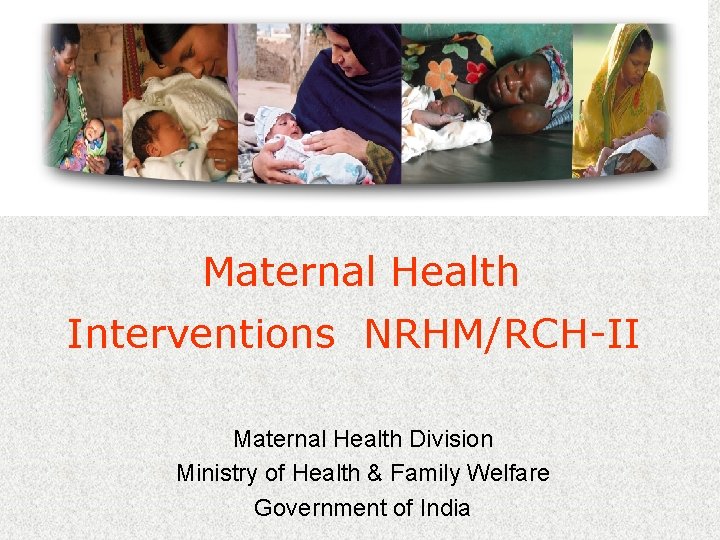
Maternal Mortality Ratio “ number of women who die in a year due to causes related to pregnancy and child birth for every 100, 000 live births ” Wide Variations: Ø Ø Ø India 301/100, 000 live births Tamil Nadu 134/100, 000 live births U. P. 517/100, 000 live births Sweden/USA 8 -12/100, 000 live births Sri Lanka 24/100, 000 live births Malaysia 20/100, 000 live births

Maternal Mortality Ratio over the years NSS(1957 -60)* NSS(1963 -64)* SRS(1972 -76) SRS(1977 -81) SRS(1982 -86) NFHS I (1992 -93) NFHS II (1998 -99) RGI, SRS (1997 -98) RGI, SRS(1999 -01) RGI, SRS (2001 -03) 1321 1195 853 810 580 424** 540** 398 327 301 * Based on indirect time series estimates ** Based on small sample size Declining trend
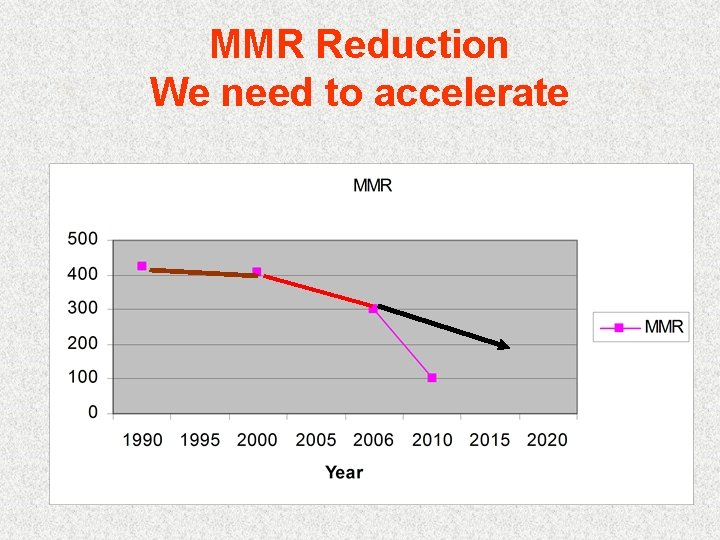
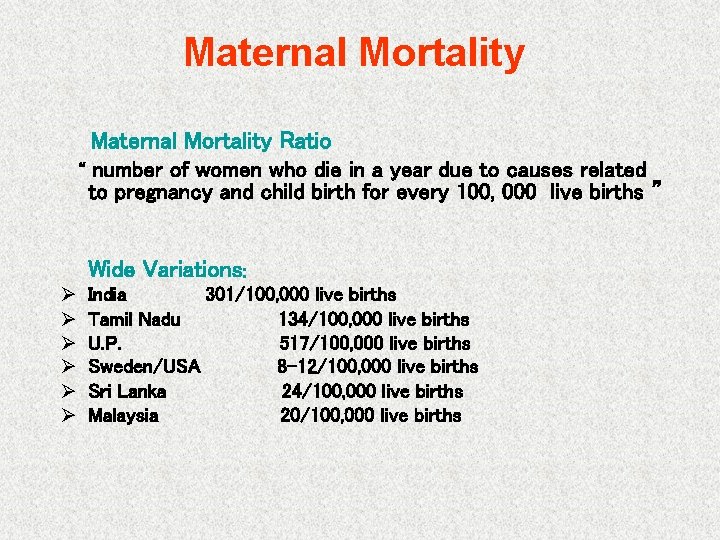
MMR Reduction We need to accelerate
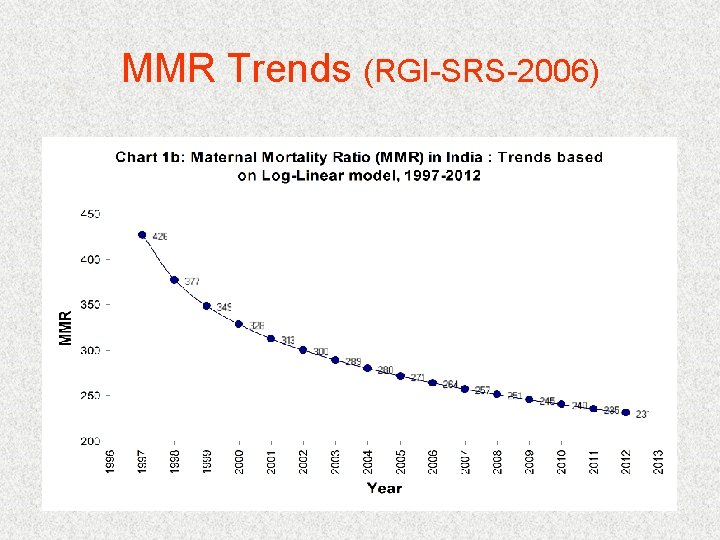
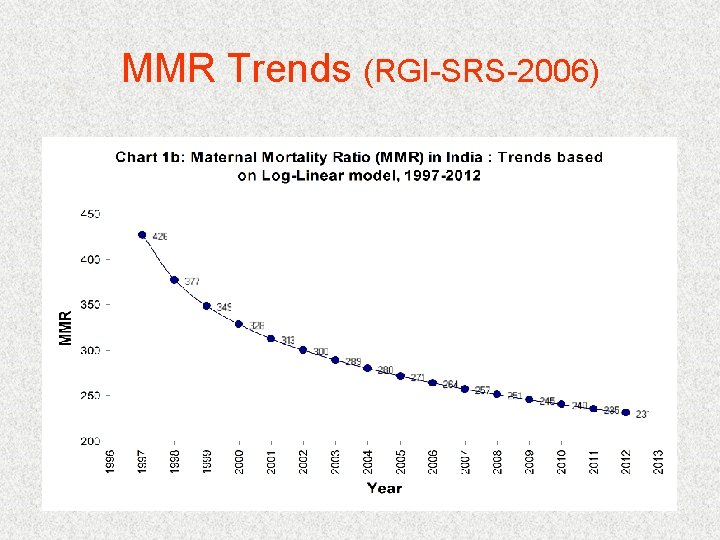
MMR Trends (RGI-SRS-2006)
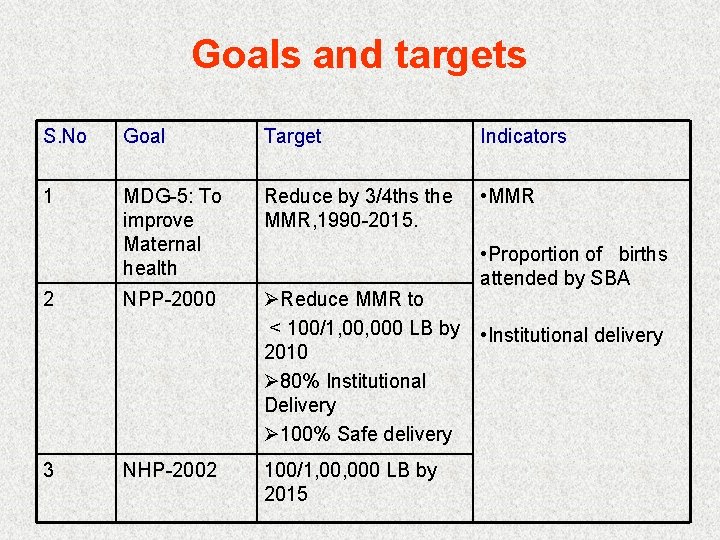
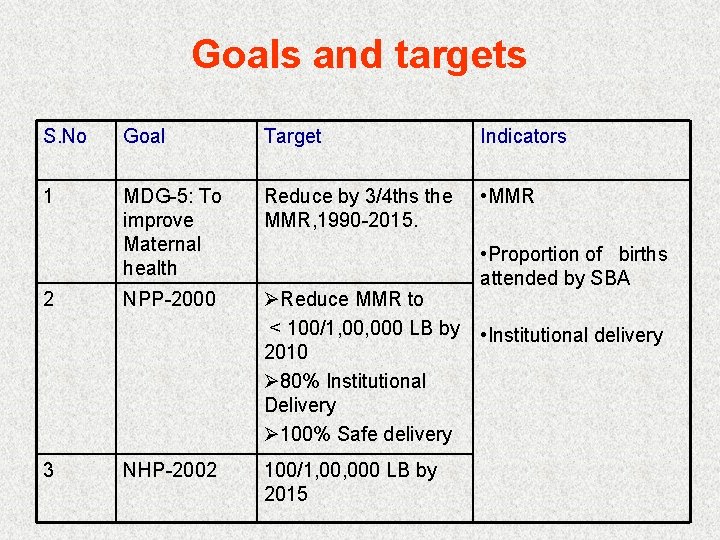
Goals and targets S. No Goal Target Indicators 1 MDG-5: To improve Maternal health Reduce by 3/4 ths the MMR, 1990 -2015. • MMR NPP-2000 ØReduce MMR to < 100/1, 000 LB by 2010 Ø 80% Institutional Delivery Ø 100% Safe delivery 2 3 NHP-2002 100/1, 000 LB by 2015 • Proportion of births attended by SBA • Institutional delivery
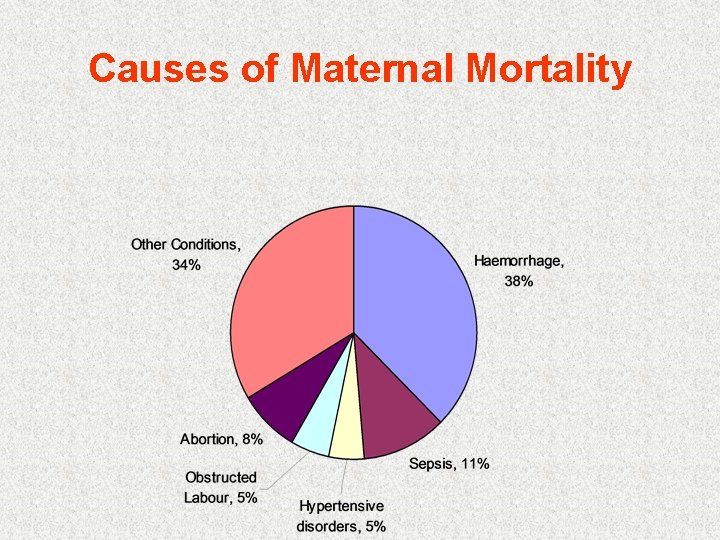
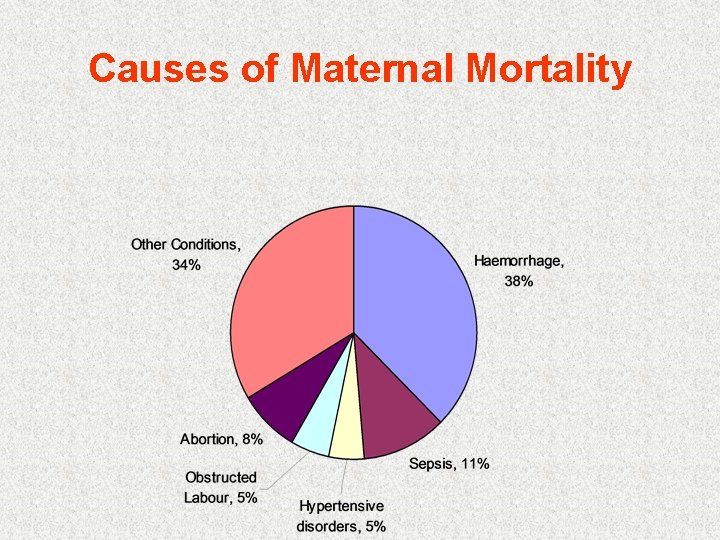
Causes of Maternal Mortality
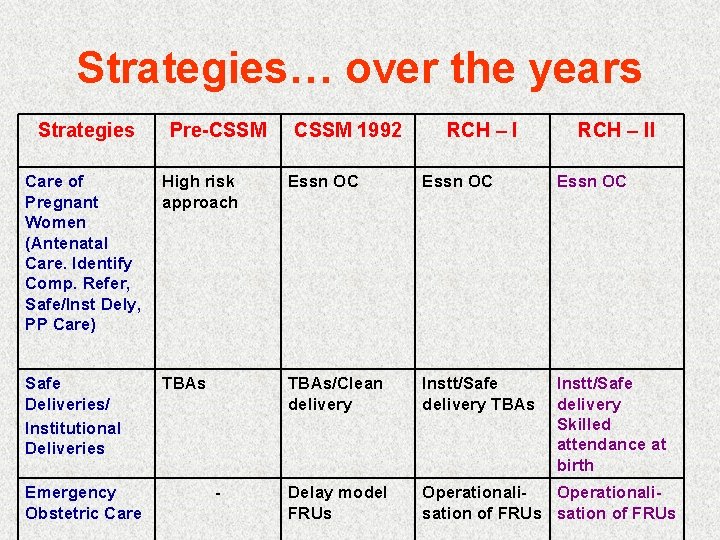
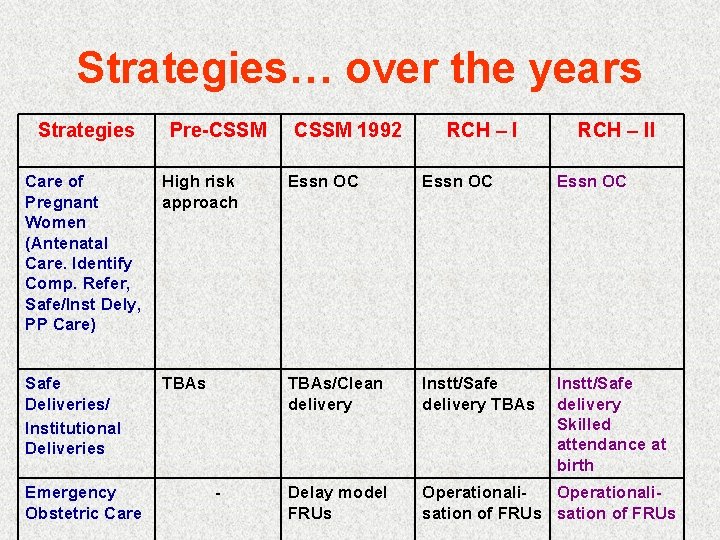
Strategies… over the years Strategies Pre-CSSM 1992 RCH – II Care of Pregnant Women (Antenatal Care. Identify Comp. Refer, Safe/Inst Dely, PP Care) High risk approach Essn OC Safe Deliveries/ Institutional Deliveries TBAs/Clean delivery Instt/Safe delivery TBAs Instt/Safe delivery Skilled attendance at birth Delay model FRUs Operationalisation of FRUs Emergency Obstetric Care -
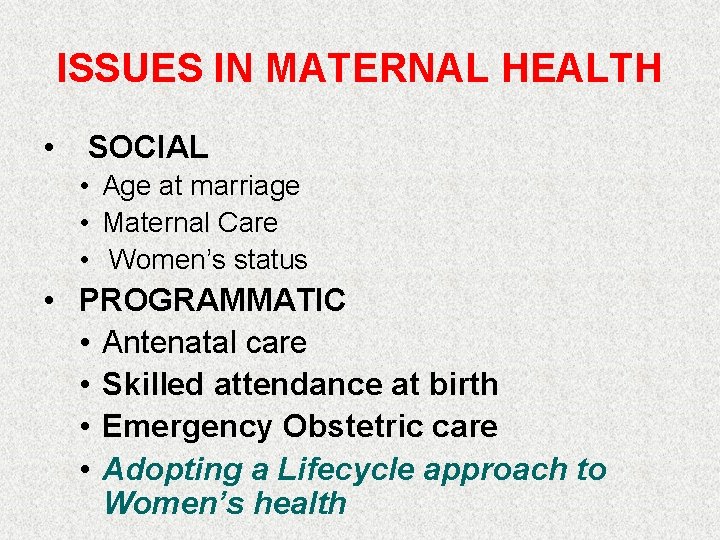
ISSUES IN MATERNAL HEALTH • SOCIAL • Age at marriage • Maternal Care • Women’s status • PROGRAMMATIC • Antenatal care • Skilled attendance at birth • Emergency Obstetric care • Adopting a Lifecycle approach to Women’s health

MH Indicators- India, NFHS II and III
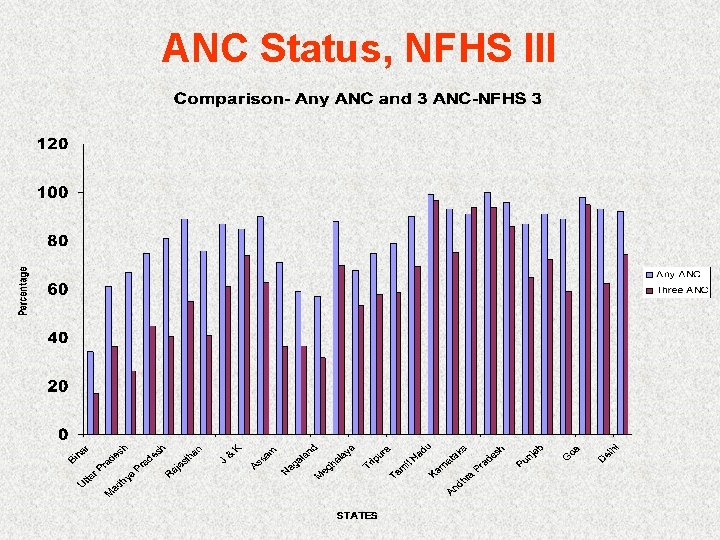
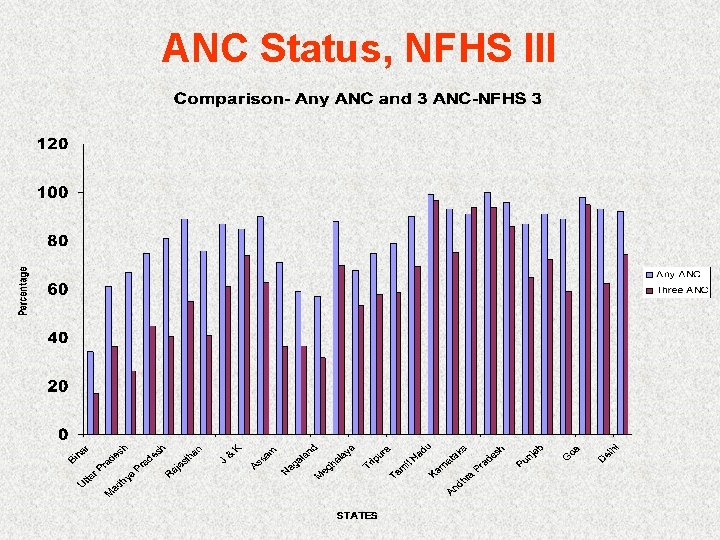
ANC Status, NFHS III

INSTITUTIONAL & SAFE DELIVERIES NFHS III

Key MH Strategies in RCH-II • Essential and Emergency Obstetric Care Ø Quality ANC, PNC, Institutional and Safe Delivery. Ø Skilled Attendance at birth (domiciliary & health facilities). Ø Operationalise FRUs, CHCs and 24 Hrs PHC. Ø Strengthen Referral Systems. • • • Management of RTIs & STIs at PHCs & CHCs/FRUs. Safe Abortion Services - MVA at PHC level. Infection Management and Environment Plan (IMEP).
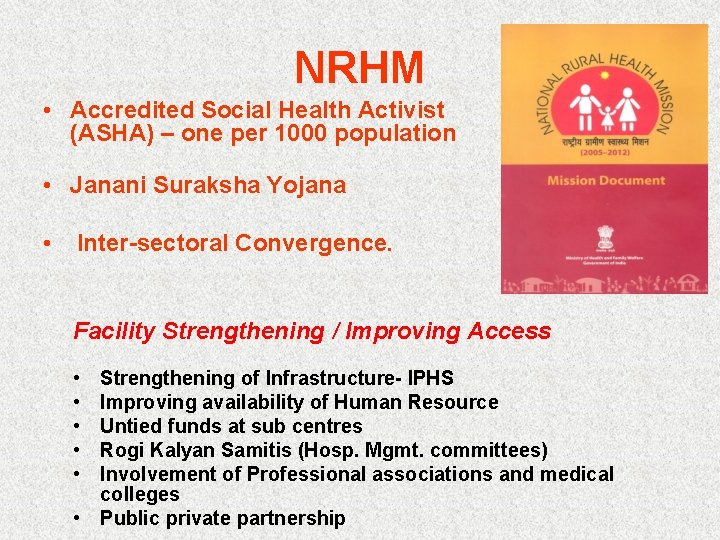
NRHM • Accredited Social Health Activist (ASHA) – one per 1000 population • Janani Suraksha Yojana • Inter-sectoral Convergence. Facility Strengthening / Improving Access • • • Strengthening of Infrastructure- IPHS Improving availability of Human Resource Untied funds at sub centres Rogi Kalyan Samitis (Hosp. Mgmt. committees) Involvement of Professional associations and medical colleges • Public private partnership

Essential Obstetric Care • • • Early Registration (12 -16 wks) 3 Antenatal Check-ups Prevention & Treatment of anemia Institutional /Safe Delivery Postnatal Check-up

Basic. Em. OC • • Parenteral A/B Parent. Oxytocics Anticonvulsants Digital removal of POC • MRP • Assisted vaginal delivery Comp. Em. OC • • All functions of Basic. Em. OC + Cs sections Blood transfusion
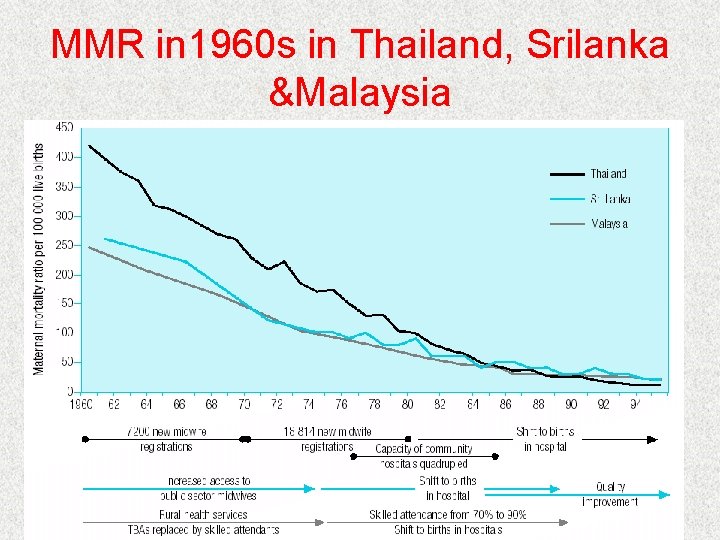
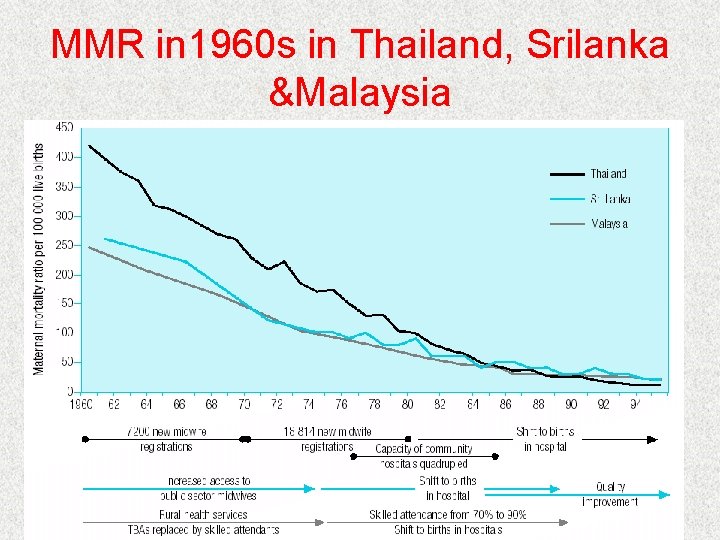
MMR in 1960 s in Thailand, Srilanka &Malaysia
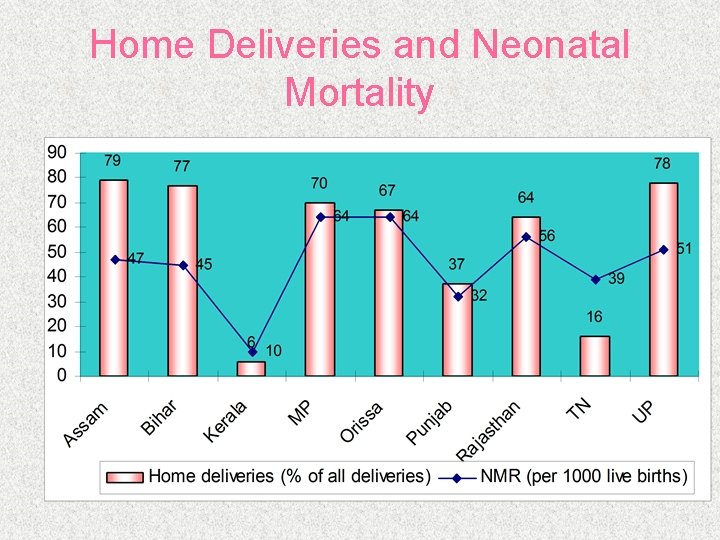
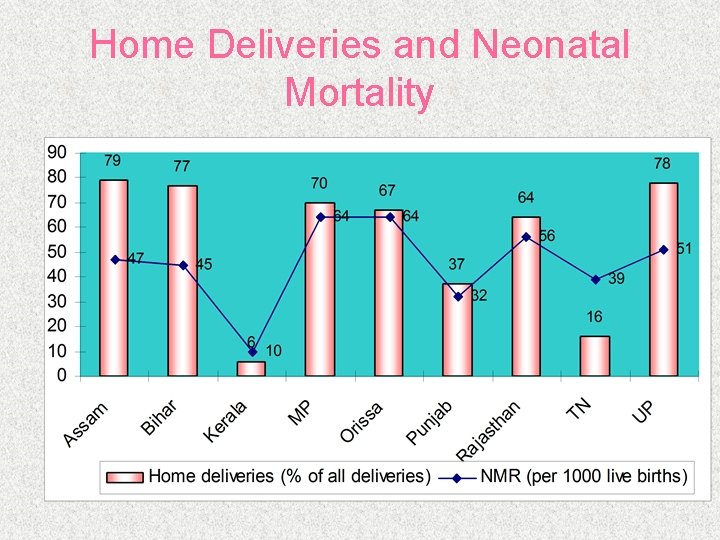
Home Deliveries and Neonatal Mortality
SKILLED BIRTH ATTENDANCE • Skilled Birth Attendant • Enabling Environment
Issues related to Skilled attendance at Birth • Reorienting Medical Officers • Preservice & inservice training for SNs/LHVs/ANMs • Operationalising SCs/ PHCs/CHCs/FRUs for skilled attendance at birth. (Enabling Environment)
Skilled Birth Attendance POLICY DECISIONS Empower Health Worker for some Basic Em. O. C. interventions • Permission to use drugs for prevention of PPH. • Permission to use drugs in emergency situations before referral • Permission to perform basic procedures at community level in emergency situations

Emergency Obstetric Care § Critical factor- TIME: 3 delay model. ü Decision to seek care ü Arrival at health facility ü Provision of adequate care at health facility § 24 X 7 PHCs First Referral Units (FRUs) at sub-district level.

Janani Suraksha Yojana • 100% centrally sponsored scheme • Promotes institutional delivery among poor pregnant women • Cash assistance to eligible women for delivery • Special dispensation for 10 states with low institutional delivery ( LPS) • ASHA- Link between beneficiary & govt. in LPS—other states are HPS
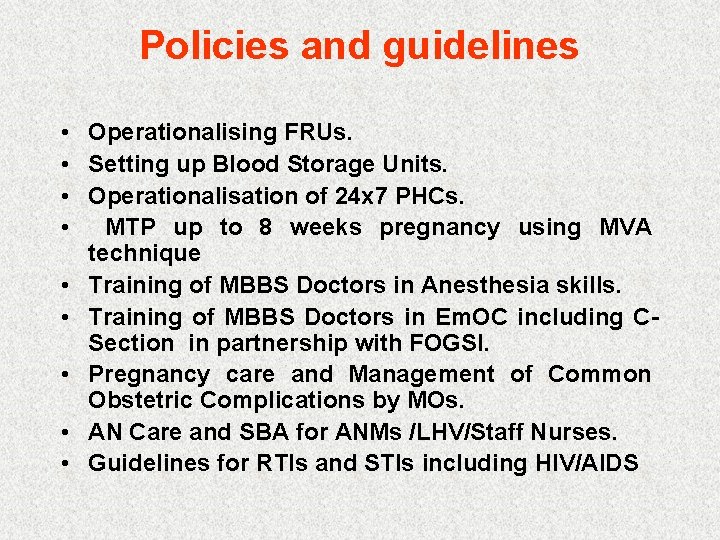
Policies and guidelines • Operationalising FRUs. • Setting up Blood Storage Units. • Operationalisation of 24 x 7 PHCs. • MTP up to 8 weeks pregnancy using MVA technique • Training of MBBS Doctors in Anesthesia skills. • Training of MBBS Doctors in Em. OC including CSection in partnership with FOGSI. • Pregnancy care and Management of Common Obstetric Complications by MOs. • AN Care and SBA for ANMs /LHV/Staff Nurses. • Guidelines for RTIs and STIs including HIV/AIDS
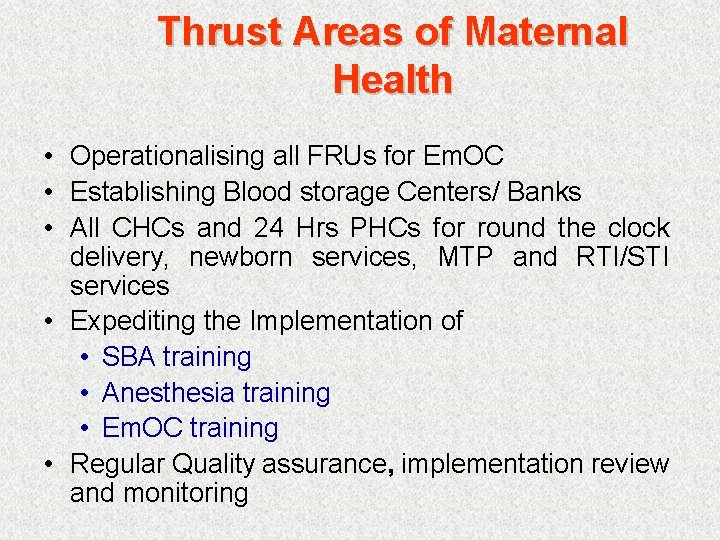
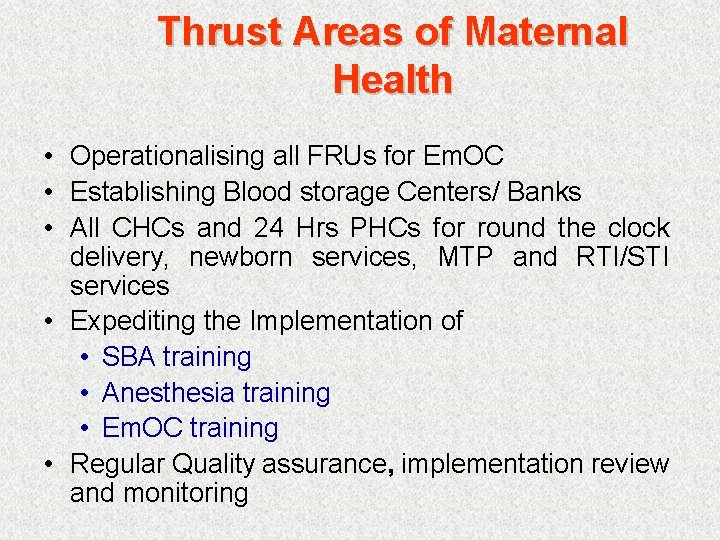
Thrust Areas of Maternal Health • Operationalising all FRUs for Em. OC • Establishing Blood storage Centers/ Banks • All CHCs and 24 Hrs PHCs for round the clock delivery, newborn services, MTP and RTI/STI services • Expediting the Implementation of • SBA training • Anesthesia training • Em. OC training • Regular Quality assurance, implementation review and monitoring
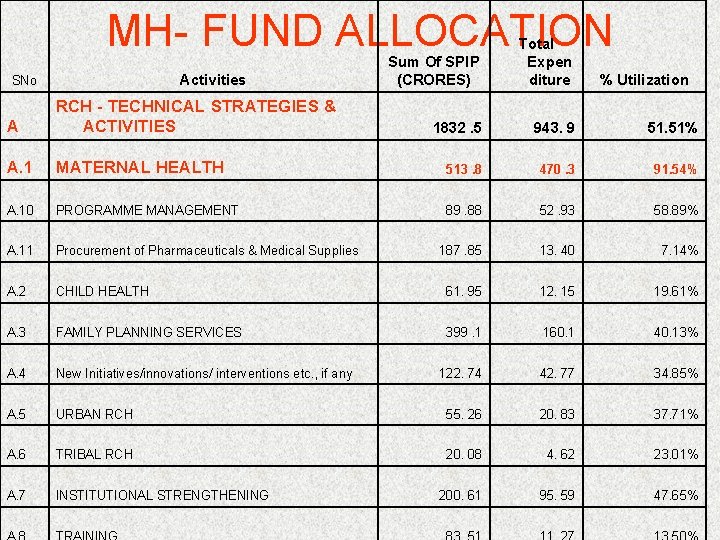
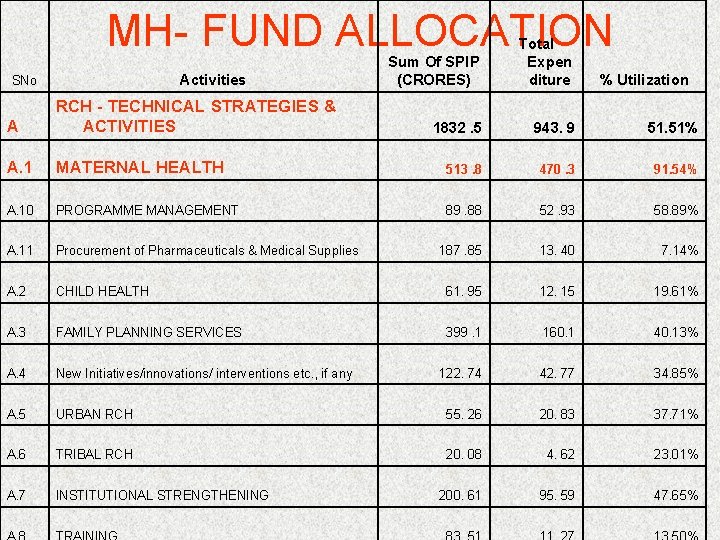
MH- FUND ALLOCATION Activities SNo Sum Of SPIP (CRORES) Total Expen diture 1832. 5 943. 9 51. 51% % Utilization A RCH - TECHNICAL STRATEGIES & ACTIVITIES A. 1 MATERNAL HEALTH 513. 8 470. 3 91. 54% A. 10 PROGRAMME MANAGEMENT 89. 88 52. 93 58. 89% A. 11 Procurement of Pharmaceuticals & Medical Supplies 187. 85 13. 40 7. 14% A. 2 CHILD HEALTH 61. 95 12. 15 19. 61% A. 3 FAMILY PLANNING SERVICES 399. 1 160. 1 40. 13% A. 4 New Initiatives/innovations/ interventions etc. , if any 122. 74 42. 77 34. 85% A. 5 URBAN RCH 55. 26 20. 83 37. 71% A. 6 TRIBAL RCH 20. 08 4. 62 23. 01% A. 7 INSTITUTIONAL STRENGTHENING 200. 61 95. 59 47. 65%
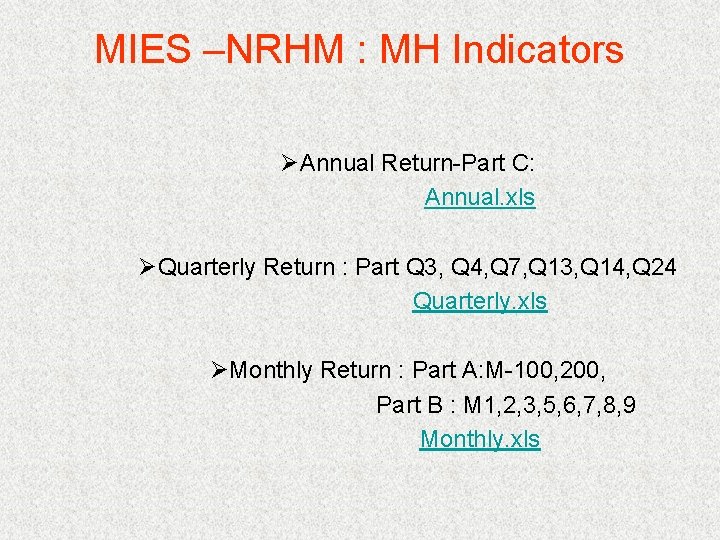
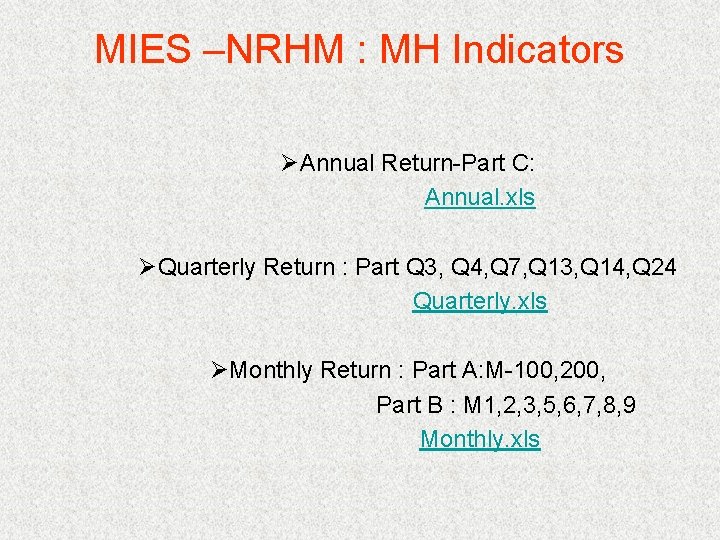
MIES –NRHM : MH Indicators ØAnnual Return-Part C: Annual. xls ØQuarterly Return : Part Q 3, Q 4, Q 7, Q 13, Q 14, Q 24 Quarterly. xls ØMonthly Return : Part A: M-100, 200, Part B : M 1, 2, 3, 5, 6, 7, 8, 9 Monthly. xls
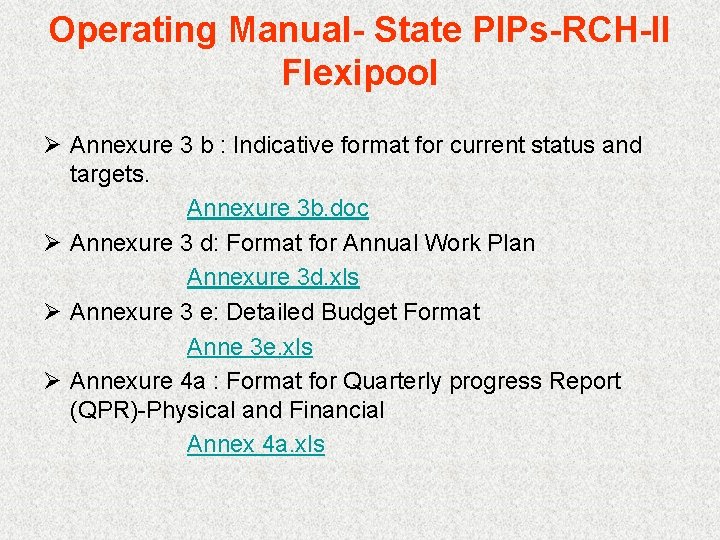
Operating Manual- State PIPs-RCH-II Flexipool Ø Annexure 3 b : Indicative format for current status and targets. Annexure 3 b. doc Ø Annexure 3 d: Format for Annual Work Plan Annexure 3 d. xls Ø Annexure 3 e: Detailed Budget Format Anne 3 e. xls Ø Annexure 4 a : Format for Quarterly progress Report (QPR)-Physical and Financial Annex 4 a. xls
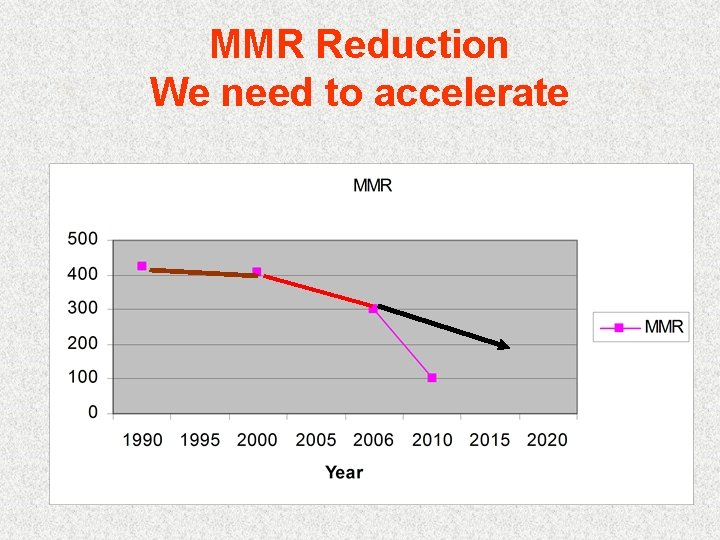
Maternal Health Division- Reporting formats Ø Maternal health activities : Monitoring Format for MH Activities. doc Ø Anesthesia Training: Reporting Format for States for Anesthesia. Trg. Final. doc Ø SBA Training : SBAplanmatrix( Final). doc Ø Em. OC Training : Reporting format for FOGSI Training. doc

 Non nuclear inheritance
Non nuclear inheritance Maternal effect and maternal inheritance
Maternal effect and maternal inheritance Veterinary services division
Veterinary services division History of maternal and child health
History of maternal and child health Factors influencing maternal health
Factors influencing maternal health Maternal and child health services
Maternal and child health services What is maternal health
What is maternal health Jama 2017
Jama 2017 Example of emotional health
Example of emotional health Amanda bleckmann
Amanda bleckmann Health ministry uk
Health ministry uk Israel ministry of health
Israel ministry of health Kristiina rebane
Kristiina rebane Ardita baraku
Ardita baraku 369 times 2
369 times 2 Synthetic dicision
Synthetic dicision Long division examples
Long division examples Long division objectives
Long division objectives Rubin's stages of maternal adaptation
Rubin's stages of maternal adaptation Plasenta patoloji raporu
Plasenta patoloji raporu Maternal effect
Maternal effect Cmqcc maternal data center
Cmqcc maternal data center Causes polyhydramnios
Causes polyhydramnios National programmes
National programmes Difference between maternal and paternal chromosomes
Difference between maternal and paternal chromosomes Sanford maternal fetal medicine
Sanford maternal fetal medicine Mild polyhydramnios range
Mild polyhydramnios range Rubin psychological phases
Rubin psychological phases Ramona mercer
Ramona mercer Maternal death reporting format
Maternal death reporting format Choose the correct option. d4t:h4p:l5r:
Choose the correct option. d4t:h4p:l5r: Perfil maternal eduardo kingman
Perfil maternal eduardo kingman The way some of these cranks talk
The way some of these cranks talk