MCH Indicators MCH status is assessed through Mortality


- Slides: 39
MCH Indicators
MCH status is assessed through: Mortality indicators Morbidity indicators Growth and development.
Mortality indicators: Maternal mortality rate 1. 2. 3. 4. 5. 6. Mortality in infancy and childhood Perinatal mortality rate Neonatal mortality rate Post-neonatal mortality rate Infant mortality rate 1 -4 years mortality rate Under 5 mortality rate

Maternal Mortality Rate
Overview: Africa has the highest maternal mortality rate in the world Experts Only 42% of births in the African region are attended by skilled personnel. African governments' health budgets are inadequate to deal with obstetric cases.
Overview: 13% of all maternal deaths occur in adolescents The Millennium Development Goals call for a 75% reduction in maternal mortality by in the African Region within the next decade.
Overview: If nothing is done to arrest the trend it is estimated that 2. 5 million maternal deaths, 2. 5 million child deaths and 49 million maternal disabilities in the region over the next 10 years indicated that 70% of deliveries take place in the community where maternal and newborn births are usually not recorded.
Maternal mortality rate Definition The death of a woman while pregnant or within 42 days of termination of pregnancy irrespective of the duration and site of pregnancy , from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.
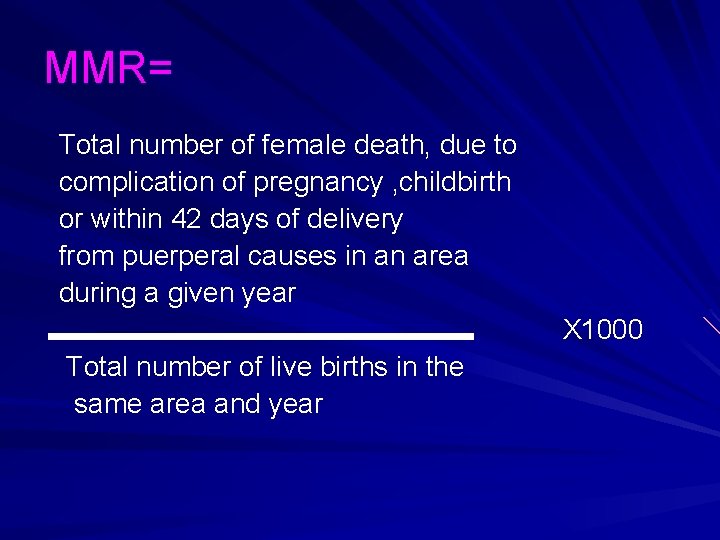
MMR= Total number of female death, due to complication of pregnancy , childbirth or within 42 days of delivery from puerperal causes in an area during a given year X 1000 Total number of live births in the same area and year
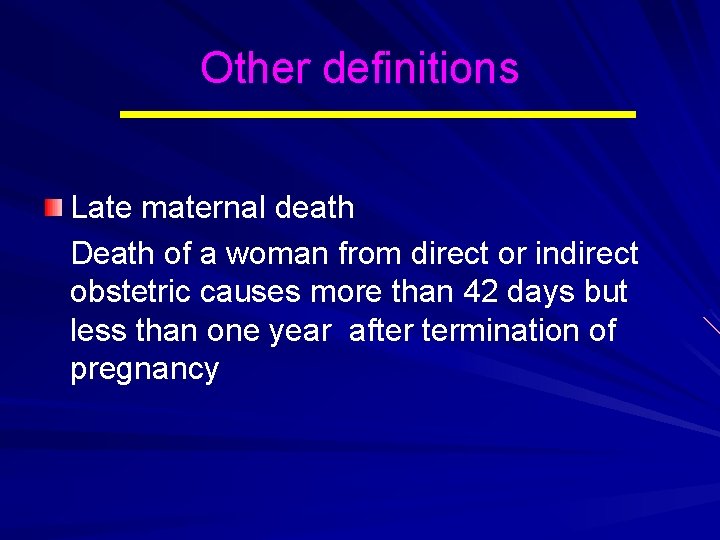
Other definitions Late maternal death Death of a woman from direct or indirect obstetric causes more than 42 days but less than one year after termination of pregnancy
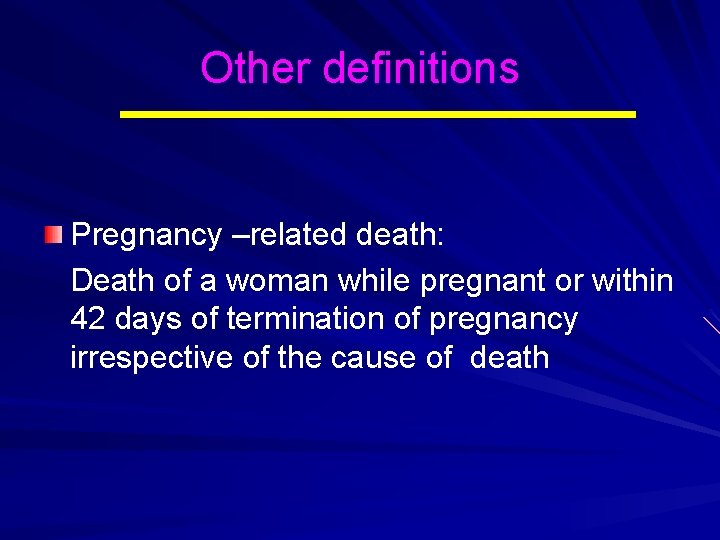
Other definitions Pregnancy –related death: Death of a woman while pregnant or within 42 days of termination of pregnancy irrespective of the cause of death
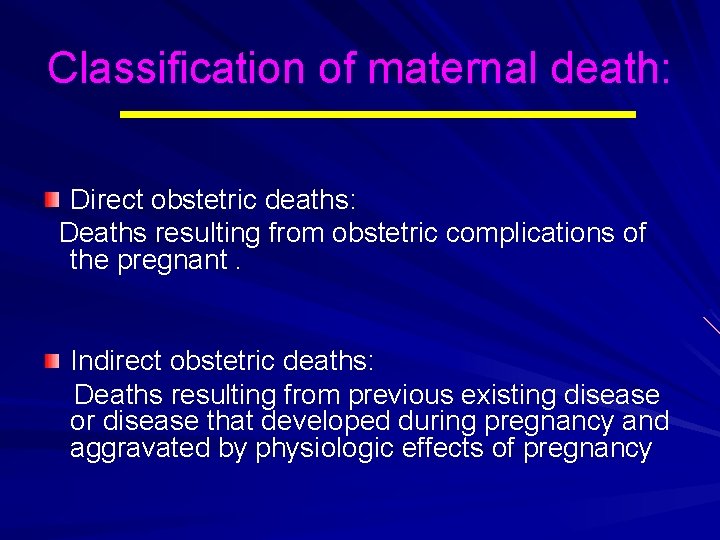
Classification of maternal death: Direct obstetric deaths: Deaths resulting from obstetric complications of the pregnant. Indirect obstetric deaths: Deaths resulting from previous existing disease or disease that developed during pregnancy and aggravated by physiologic effects of pregnancy
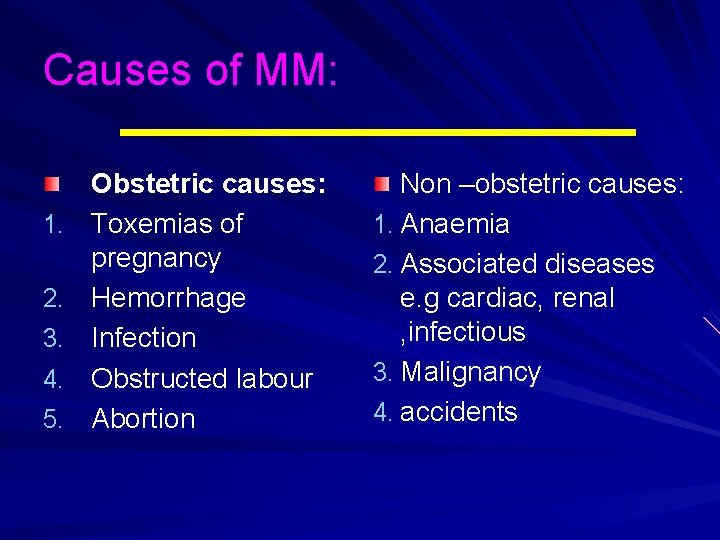
Causes of MM: 1. 2. 3. 4. 5. Obstetric causes: Toxemias of pregnancy Hemorrhage Infection Obstructed labour Abortion Non –obstetric causes: 1. Anaemia 2. Associated diseases e. g cardiac, renal , infectious 3. Malignancy 4. accidents
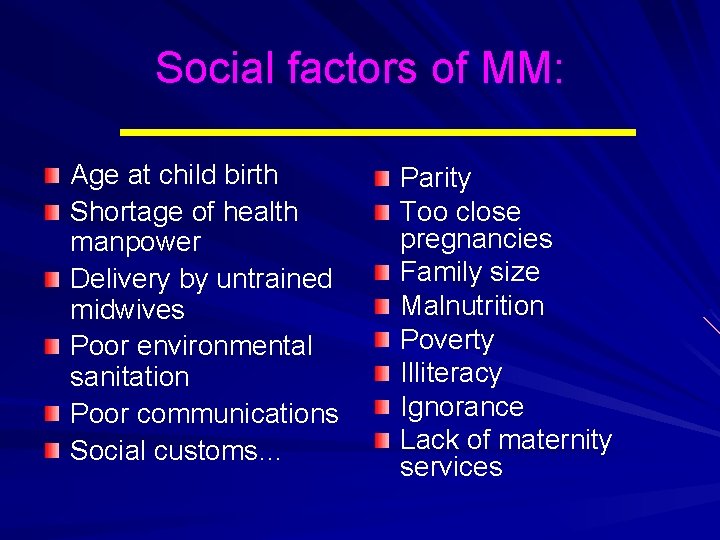
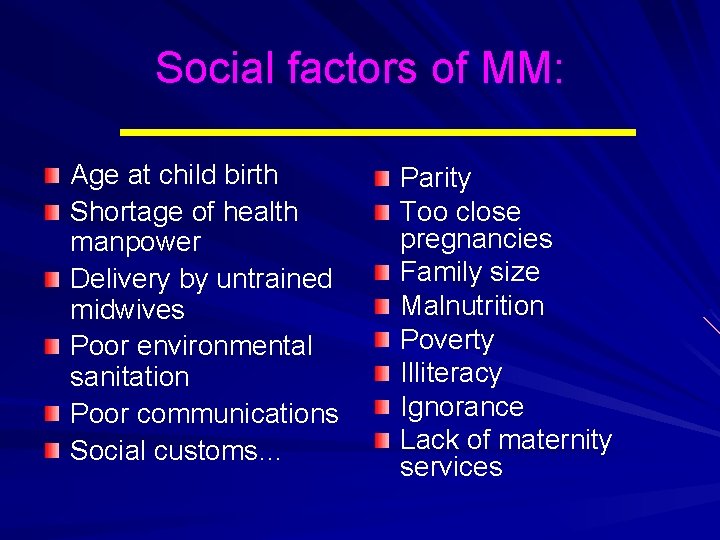
Social factors of MM: Age at child birth Shortage of health manpower Delivery by untrained midwives Poor environmental sanitation Poor communications Social customs… Parity Too close pregnancies Family size Malnutrition Poverty Illiteracy Ignorance Lack of maternity services
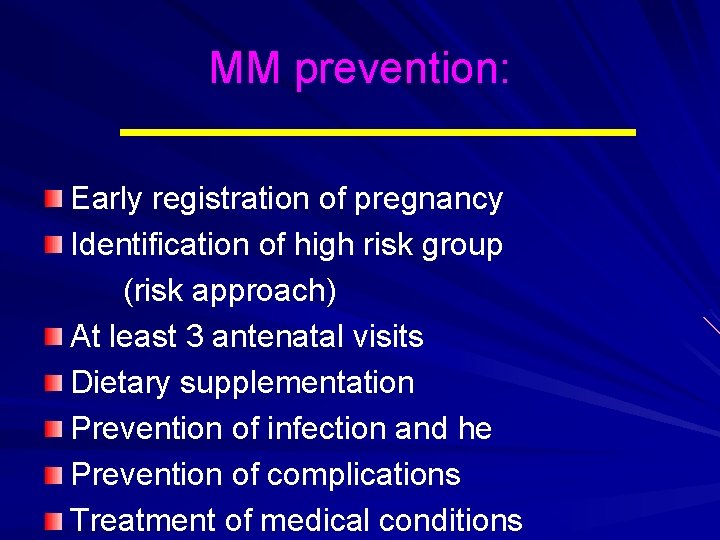
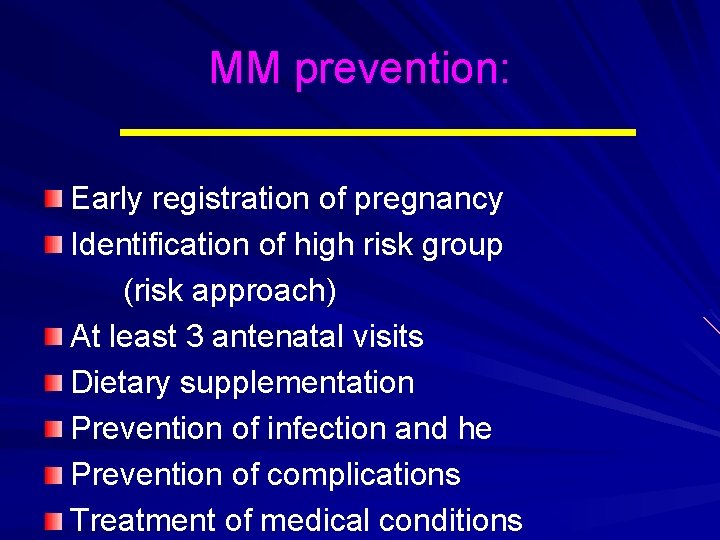
MM prevention: Early registration of pregnancy Identification of high risk group (risk approach) At least 3 antenatal visits Dietary supplementation Prevention of infection and he Prevention of complications Treatment of medical conditions
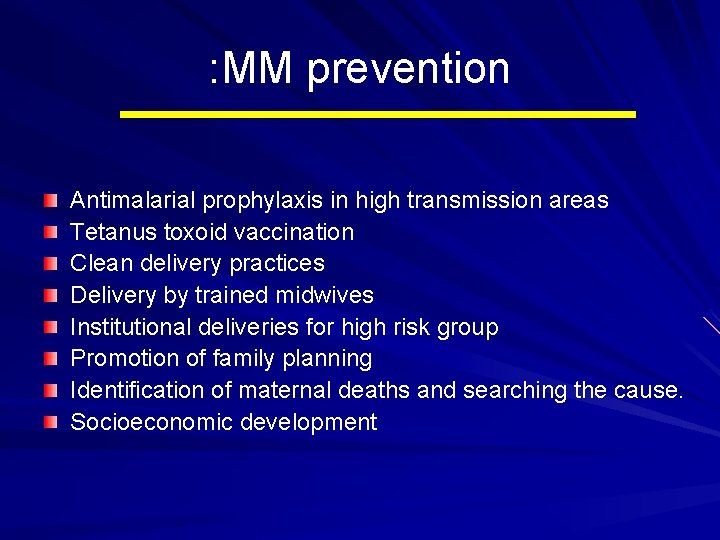
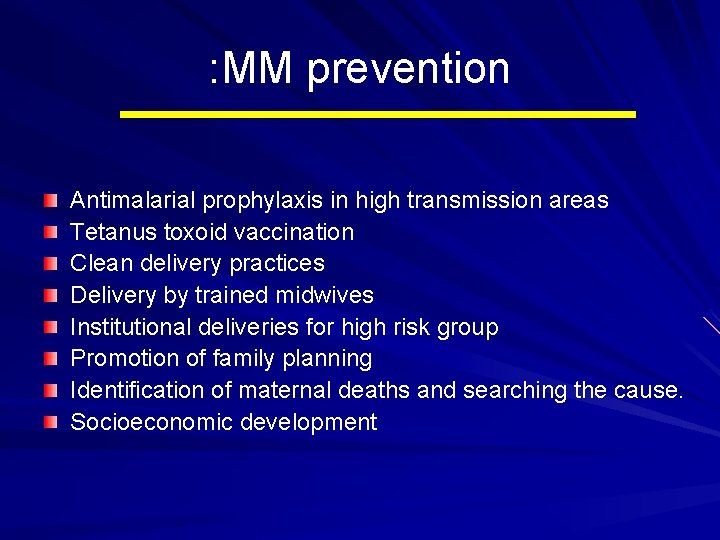
: MM prevention Antimalarial prophylaxis in high transmission areas Tetanus toxoid vaccination Clean delivery practices Delivery by trained midwives Institutional deliveries for high risk group Promotion of family planning Identification of maternal deaths and searching the cause. Socioeconomic development
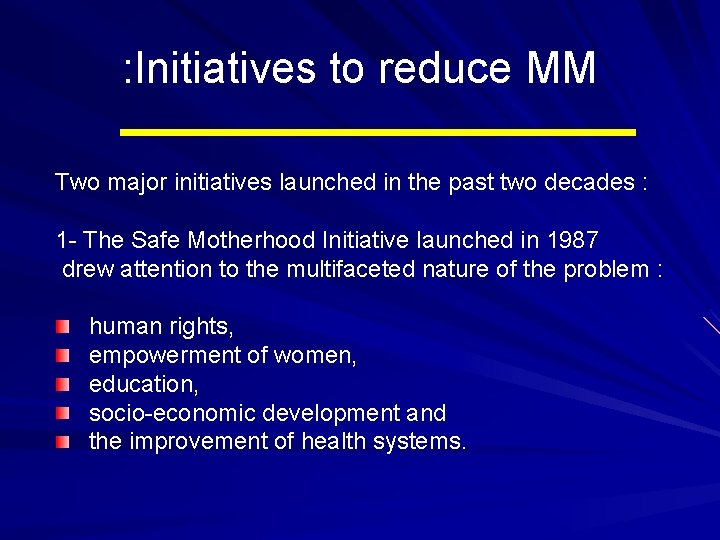
: Initiatives to reduce MM Two major initiatives launched in the past two decades : 1 - The Safe Motherhood Initiative launched in 1987 drew attention to the multifaceted nature of the problem : human rights, empowerment of women, education, socio-economic development and the improvement of health systems.
2 - The Making Pregnancy Safer Initiative, launched in 2000, focused on The health sector and its crucial role in accelerating maternal maternity reduction. Aim: to ensure that women and their newborns have access to the care they need through - the strengthening of health systems and - appropriate community-level actions
Mortality In Infancy And Childhood
Mortality in infancy and childhood Fetal death Is death prior to the complete expulsion or extraction from its mother of a product of conception irrespective of the duration of pregnancy; the death is indicated by the fact that after such separation the foetus does not breathe or show any evidence of life such as beating of the heart , pulsation of the umbilical cord or definite movement of the voluntary muscles.
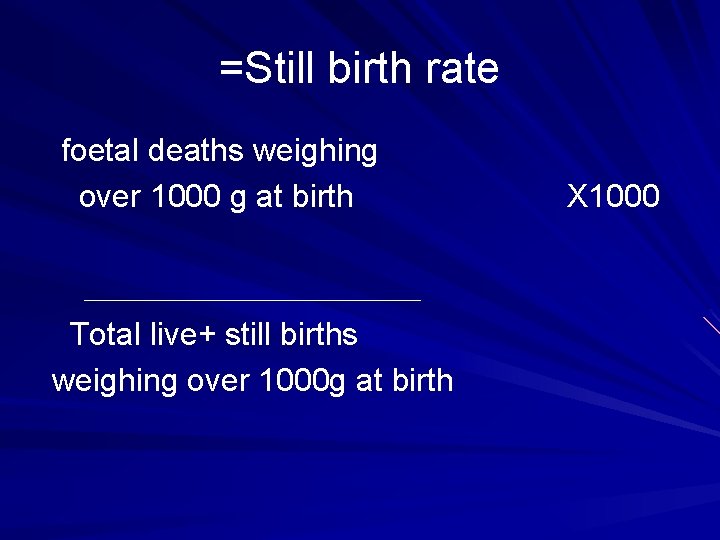
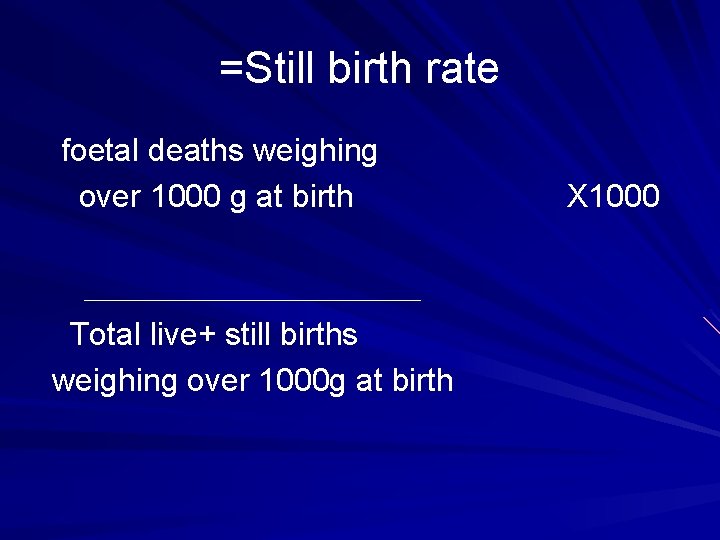
=Still birth rate foetal deaths weighing over 1000 g at birth Total live+ still births weighing over 1000 g at birth X 1000
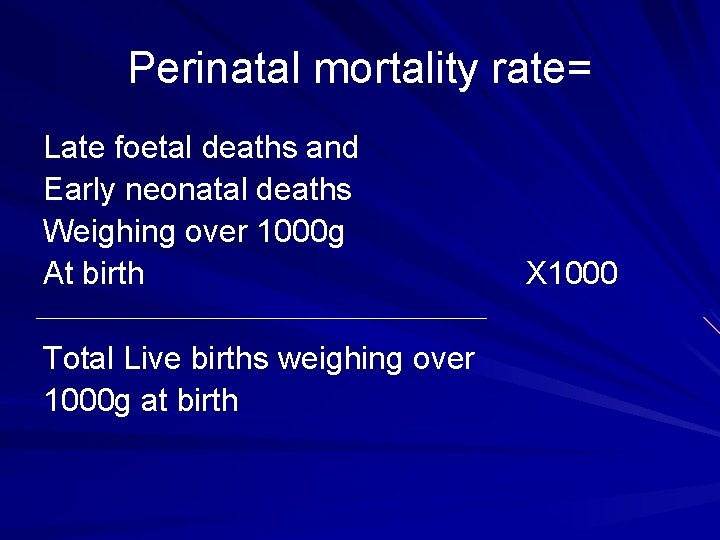
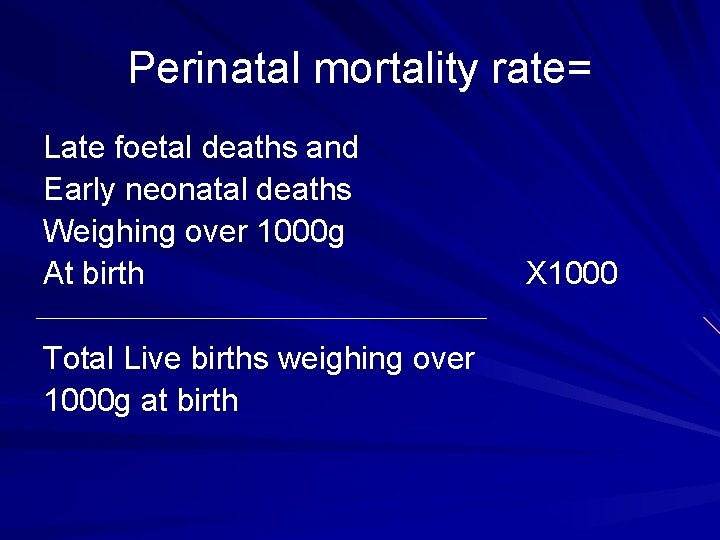
Perinatal mortality rate= Late foetal deaths and Early neonatal deaths Weighing over 1000 g At birth Total Live births weighing over 1000 g at birth X 1000
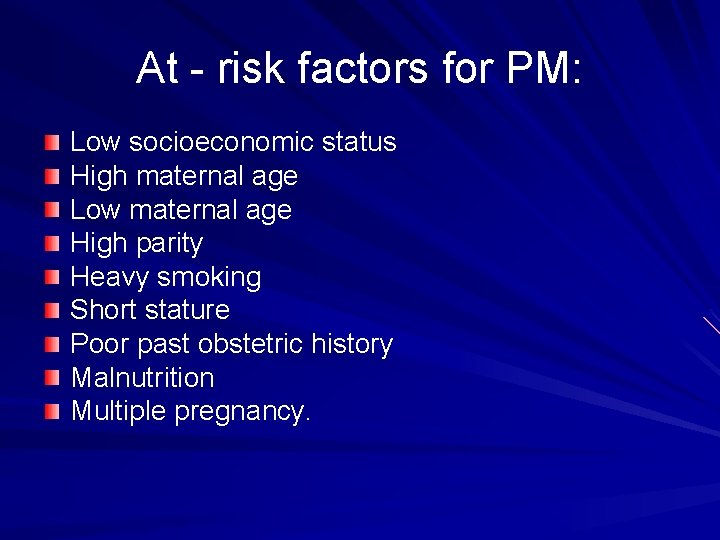
At - risk factors for PM: Low socioeconomic status High maternal age Low maternal age High parity Heavy smoking Short stature Poor past obstetric history Malnutrition Multiple pregnancy.
: Causes of PM Anta natal causes Intranatal causes Postnatal causes Unknown causes.
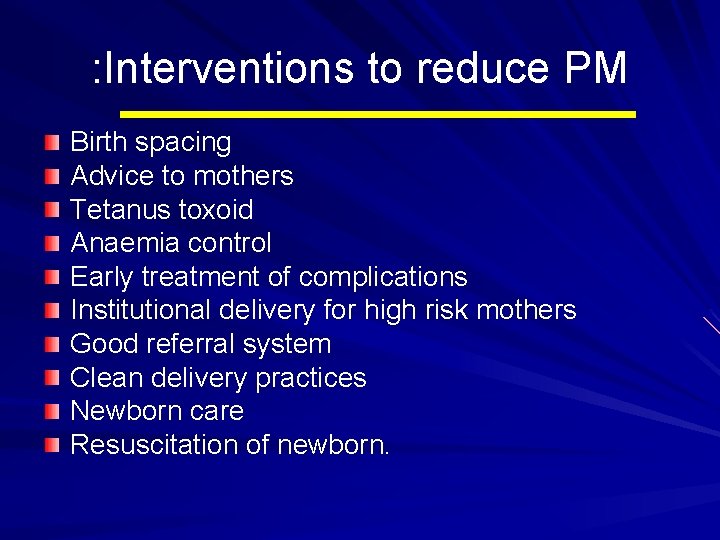
: Interventions to reduce PM Birth spacing Advice to mothers Tetanus toxoid Anaemia control Early treatment of complications Institutional delivery for high risk mothers Good referral system Clean delivery practices Newborn care Resuscitation of newborn.
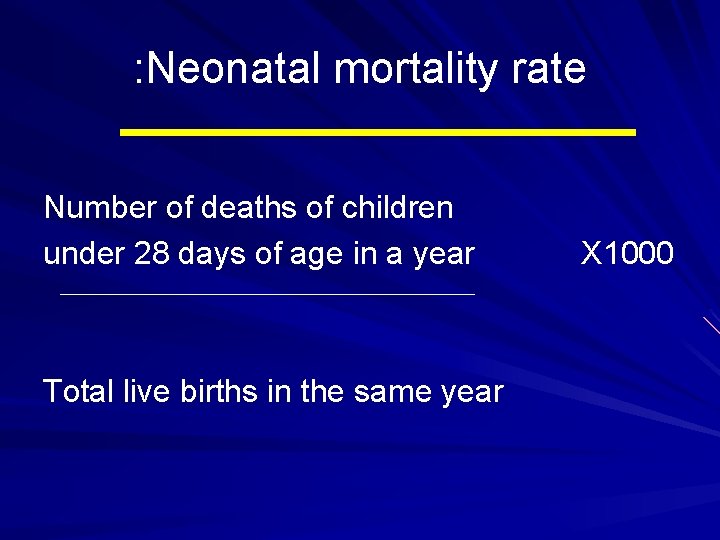
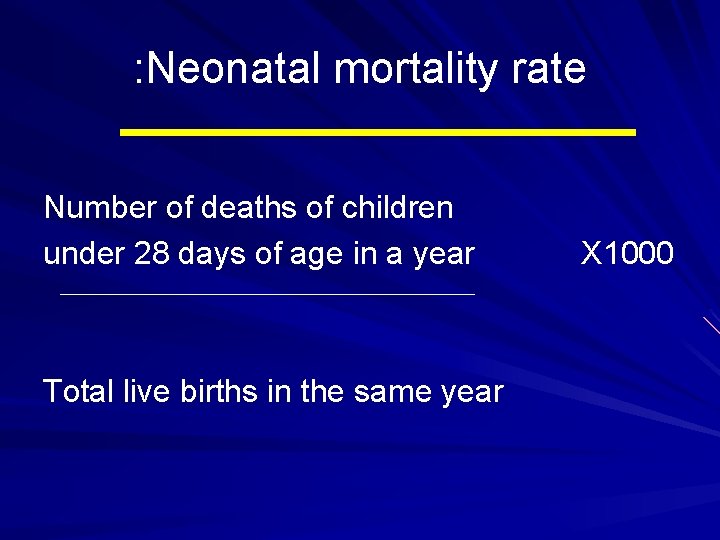
: Neonatal mortality rate Number of deaths of children under 28 days of age in a year Total live births in the same year X 1000
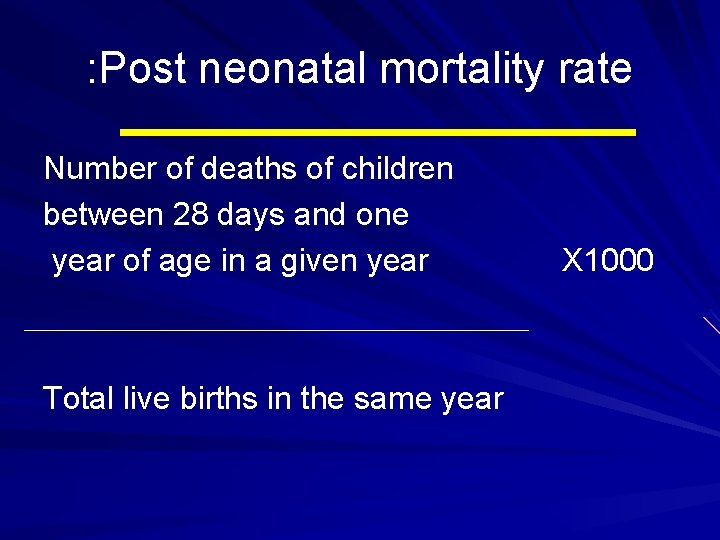
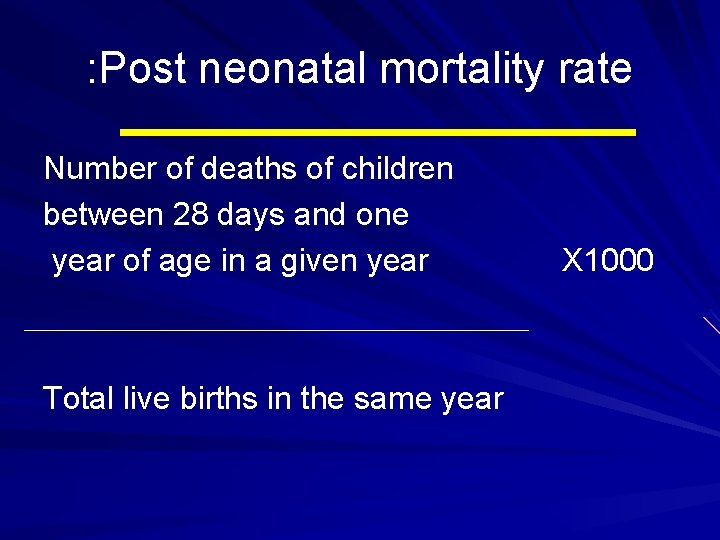
: Post neonatal mortality rate Number of deaths of children between 28 days and one year of age in a given year Total live births in the same year X 1000
: Causes Neonatal mortality: Endogenous factors Post-neonatal mortality Exogenous causes
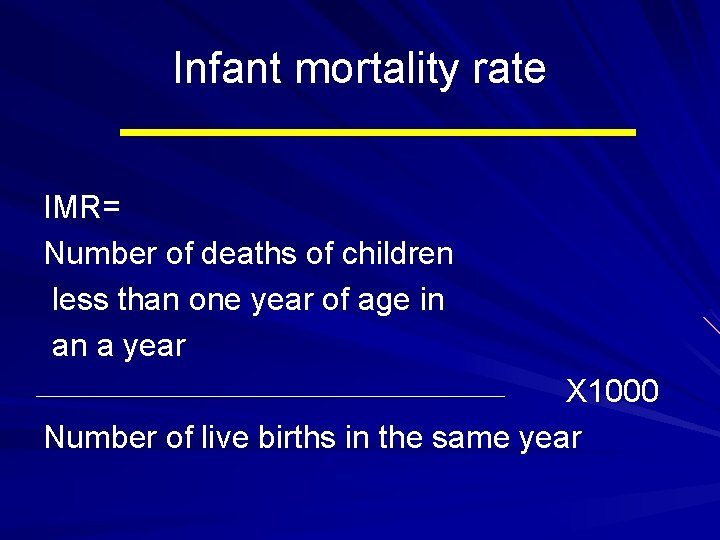
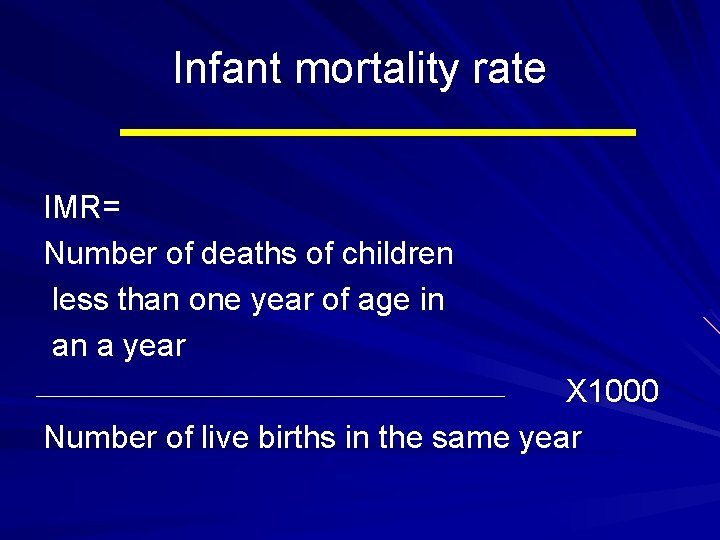
Infant mortality rate IMR= Number of deaths of children less than one year of age in an a year X 1000 Number of live births in the same year
What are the causes?
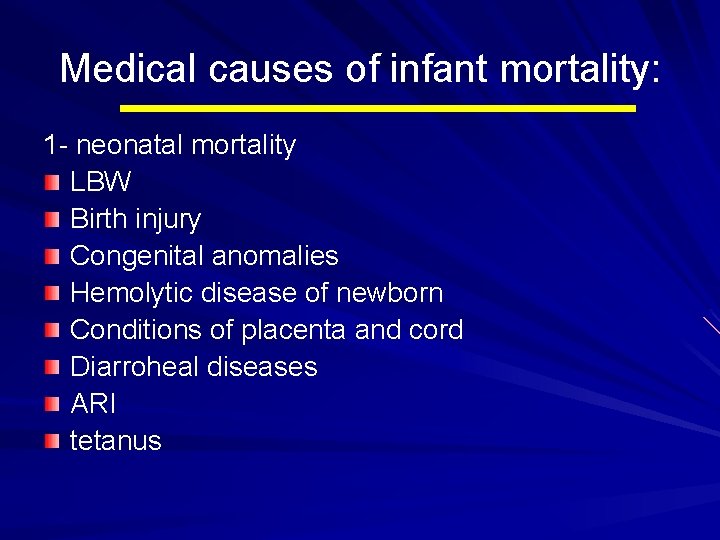
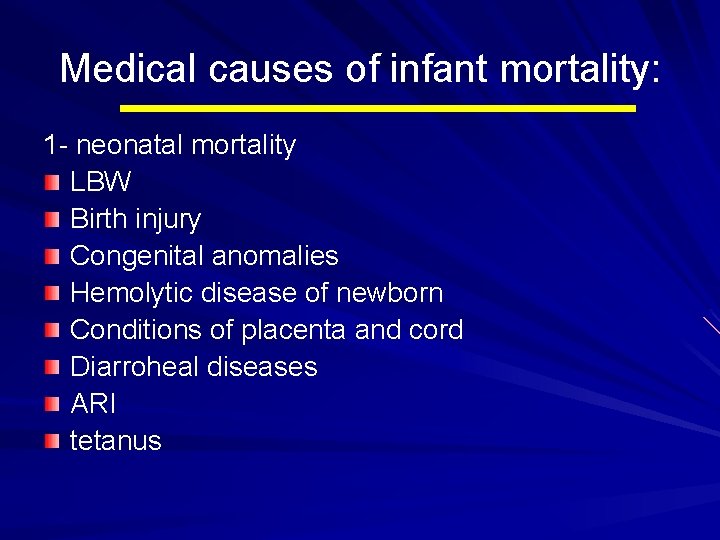
Medical causes of infant mortality: 1 - neonatal mortality LBW Birth injury Congenital anomalies Hemolytic disease of newborn Conditions of placenta and cord Diarroheal diseases ARI tetanus
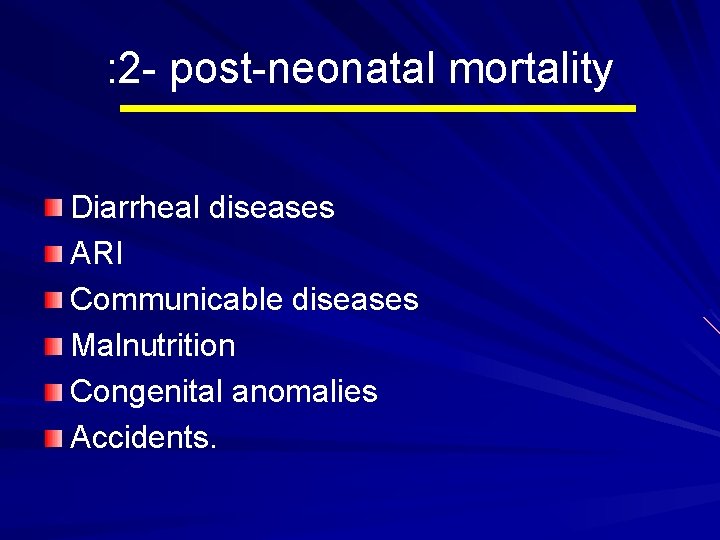
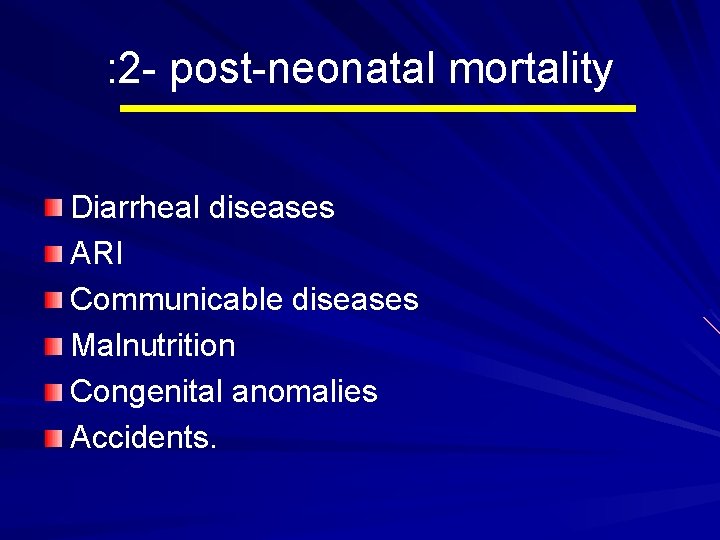
: 2 - post-neonatal mortality Diarrheal diseases ARI Communicable diseases Malnutrition Congenital anomalies Accidents.
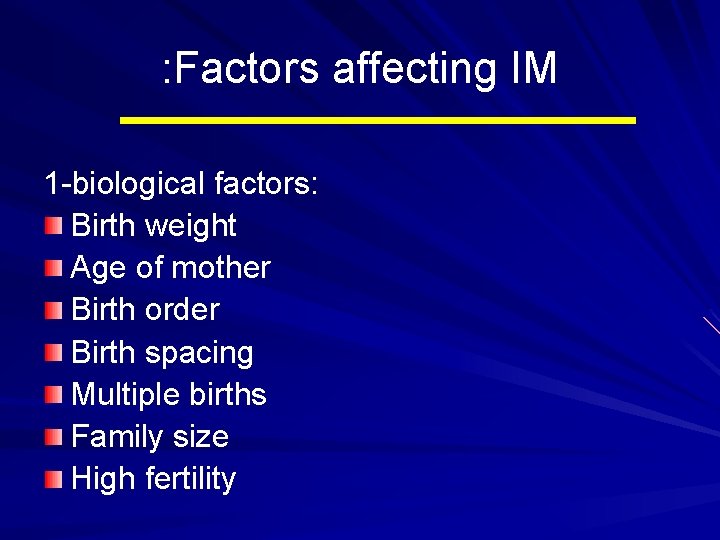
: Factors affecting IM 1 -biological factors: Birth weight Age of mother Birth order Birth spacing Multiple births Family size High fertility
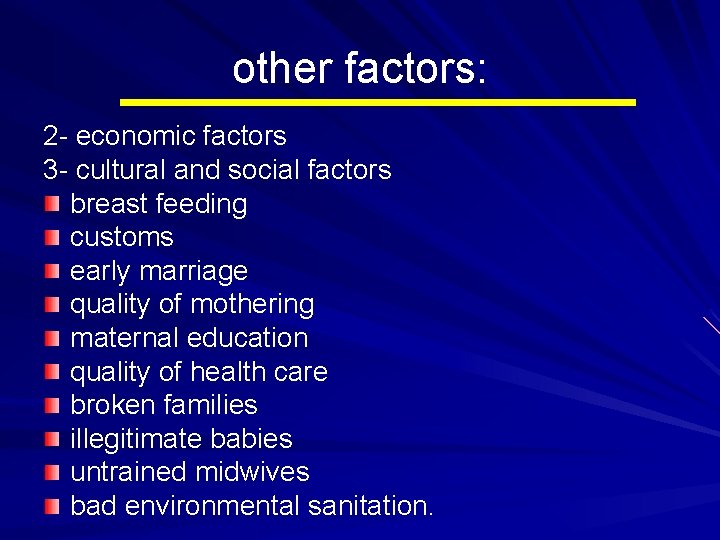
other factors: 2 - economic factors 3 - cultural and social factors breast feeding customs early marriage quality of mothering maternal education quality of health care broken families illegitimate babies untrained midwives bad environmental sanitation.
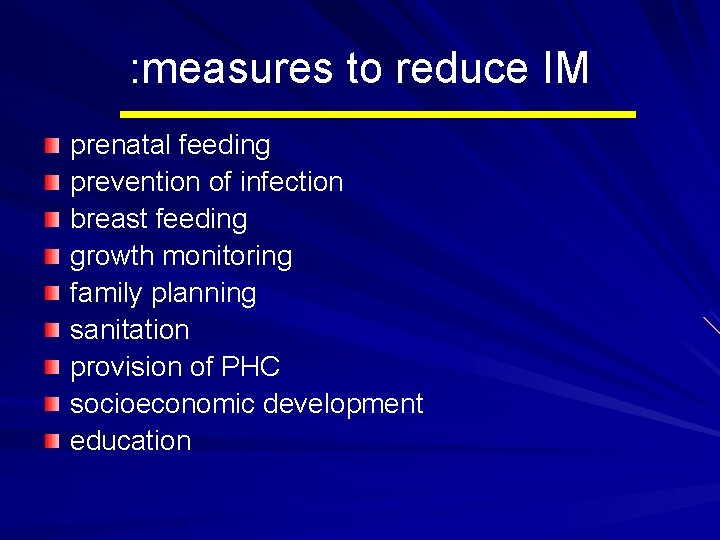
: measures to reduce IM prenatal feeding prevention of infection breast feeding growth monitoring family planning sanitation provision of PHC socioeconomic development education
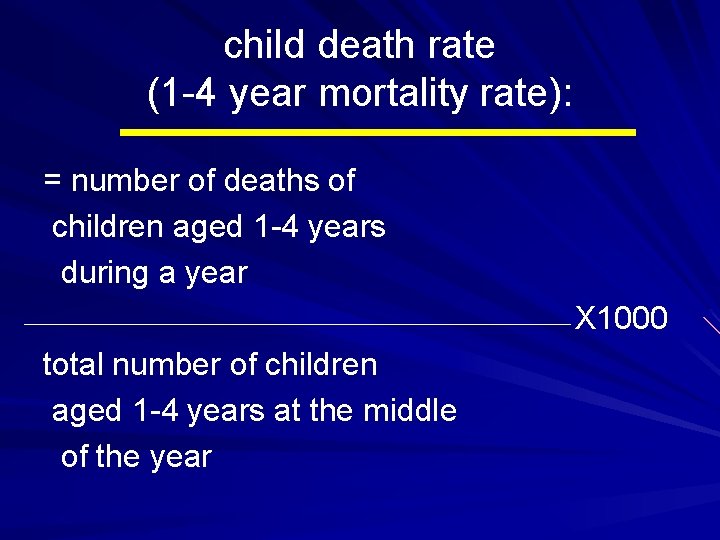
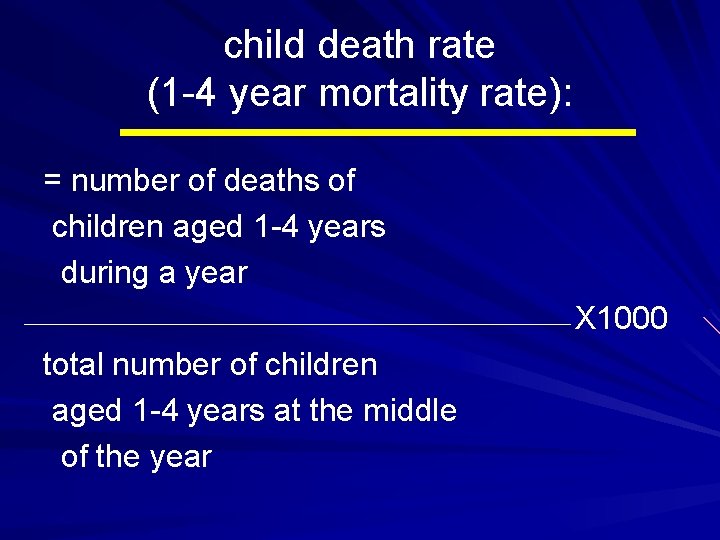
child death rate (1 -4 year mortality rate): = number of deaths of children aged 1 -4 years during a year X 1000 total number of children aged 1 -4 years at the middle of the year
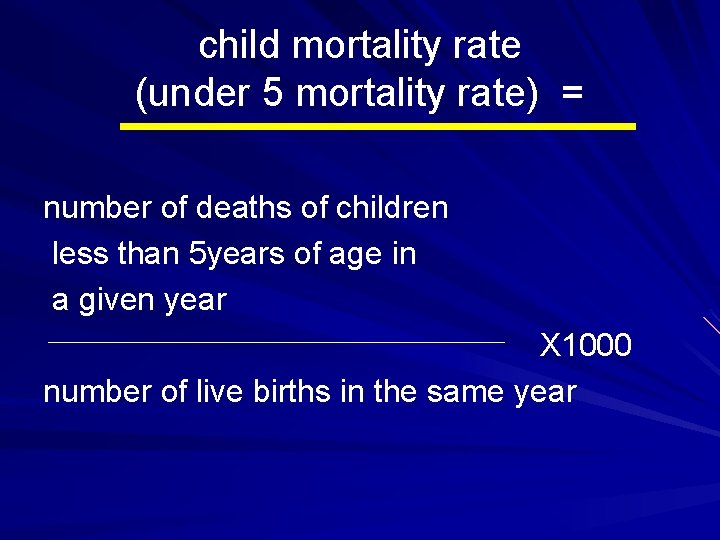
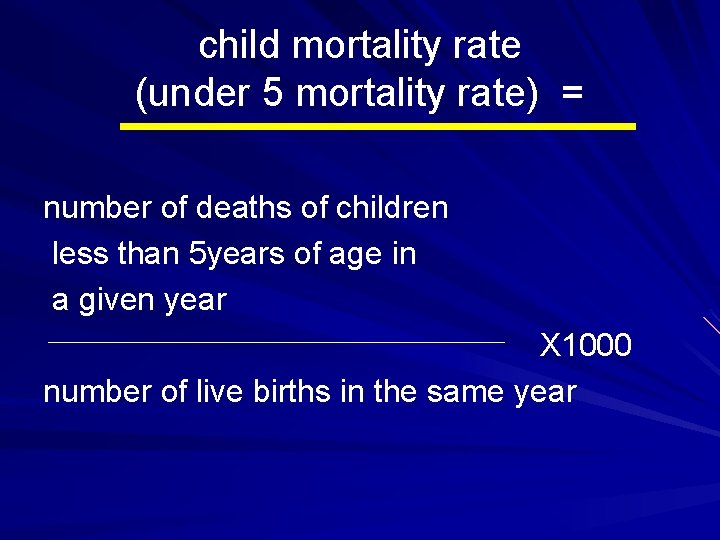
child mortality rate (under 5 mortality rate) = number of deaths of children less than 5 years of age in a given year X 1000 number of live births in the same year
Thank you
