Manual dipstick urinalysis Lynne Powell RN MSc I



- Slides: 37
Manual dipstick urinalysis Lynne Powell RN MSc I P Pg. CEd
INTRODUCTION URINALYSIS is a simple non-invasive diagnostic test which can provide a glimpse into a person’s health
Objectives § § Give an overview of the anatomy and physiology of the urinary system Explain how urine is produced and its components Describe the types of urine samples and tests Describe the requirements and procedure for dipstick urinalysis using the manual method
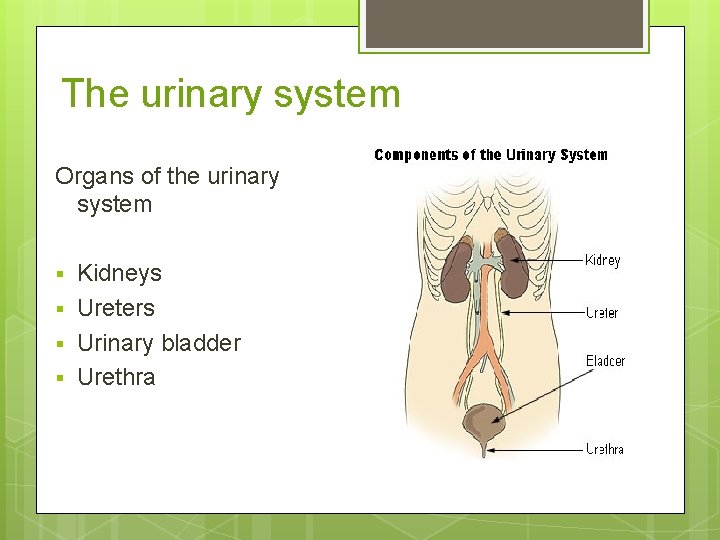
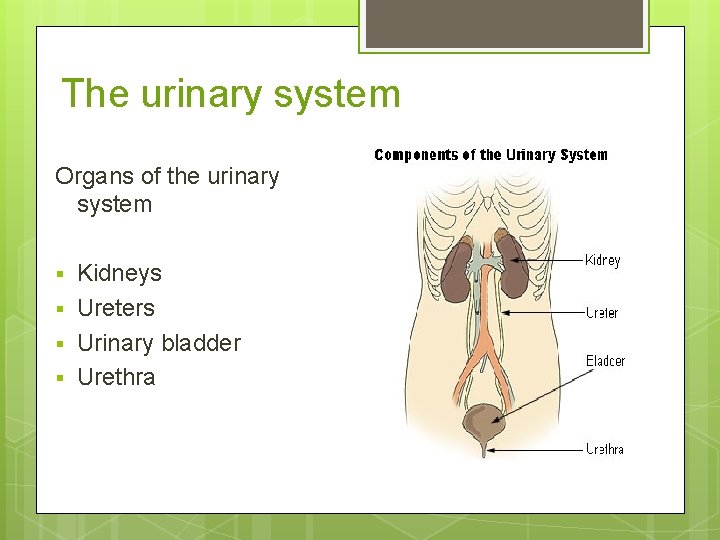
The urinary system Organs of the urinary system § § Kidneys Ureters Urinary bladder Urethra
The function of the urinary system § § The kidneys regulate: acid-base balance; electrolyte concentration; extracellular fluid volume (homeostasis). The kidneys remove waste & water from the blood stream and reabsorb vital nutrients. The kidneys regulate the blood pressure. The urinary bladder stores urine.
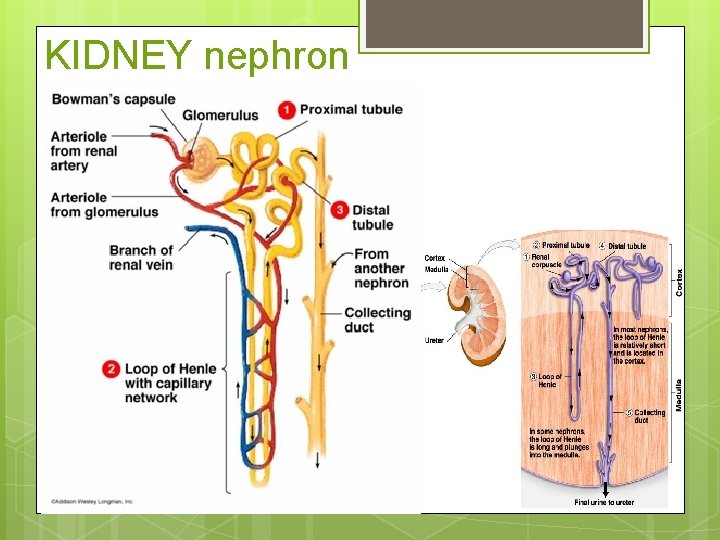
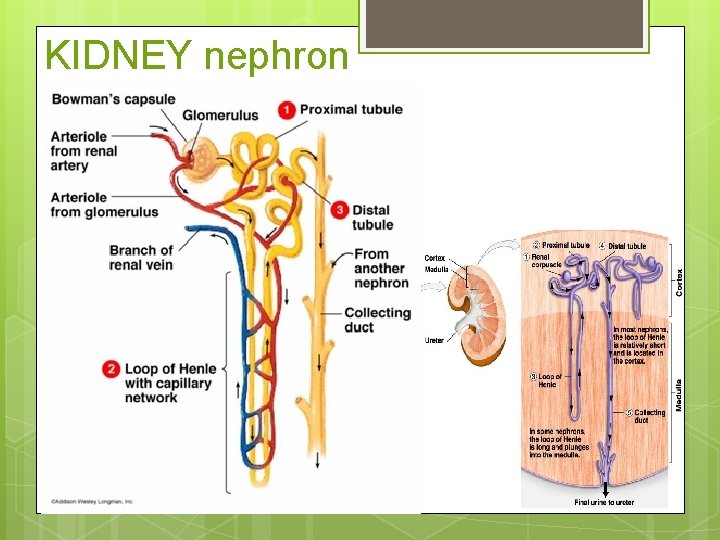
KIDNEY nephron
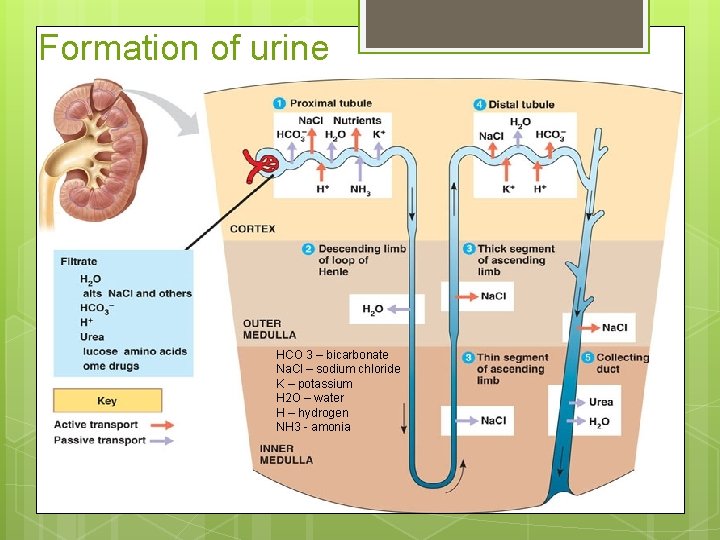
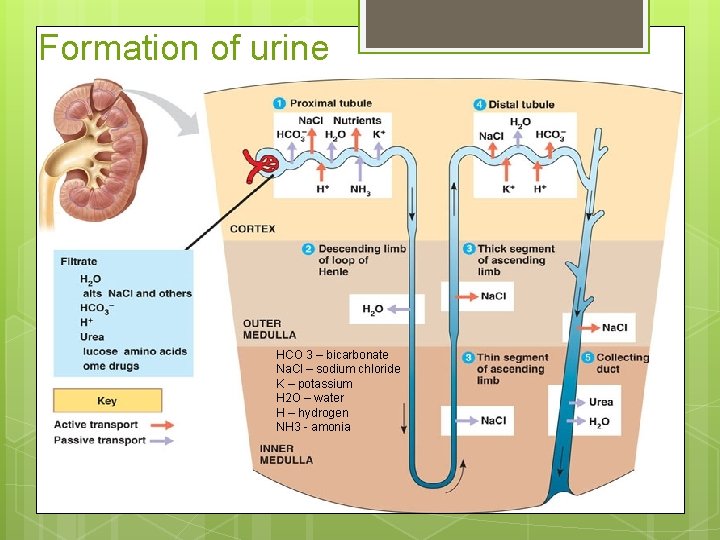
Formation of urine HCO 3 – bicarbonate Na. Cl – sodium chloride K – potassium H 2 O – water H – hydrogen NH 3 - amonia

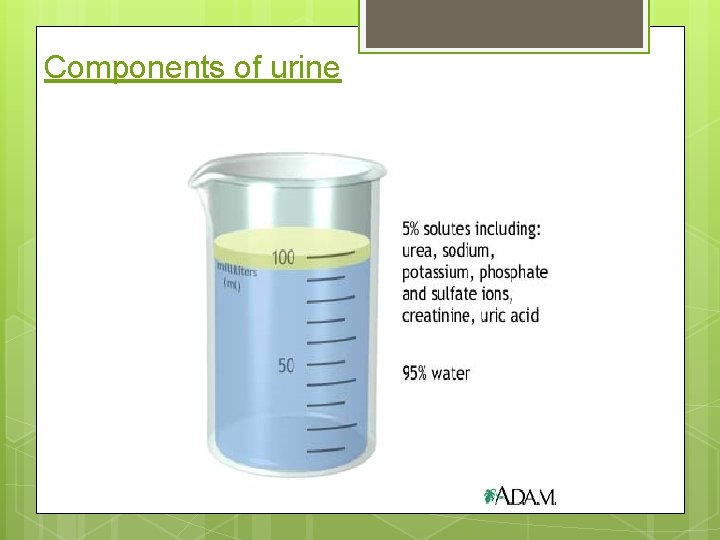
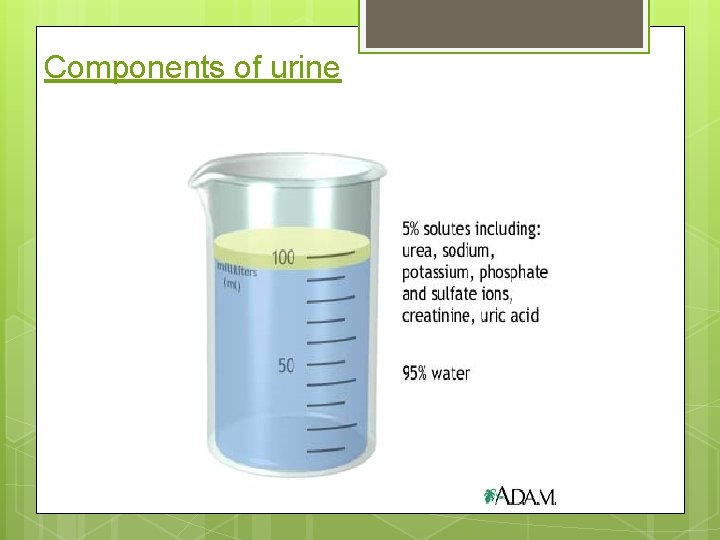
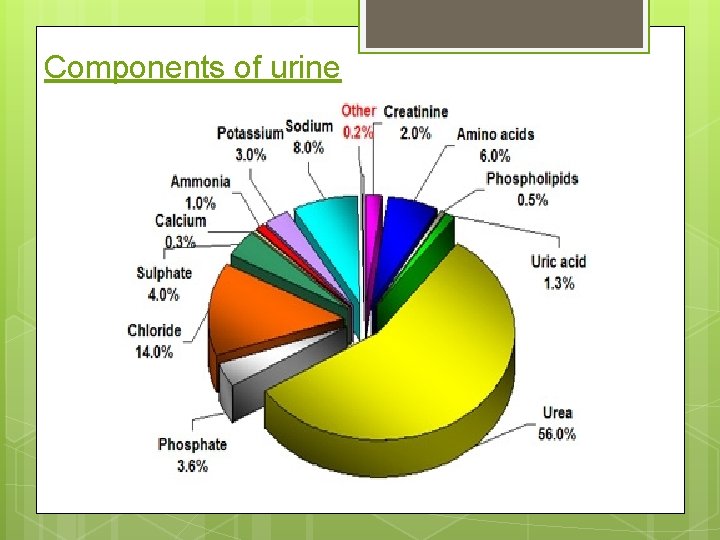
Components of urine
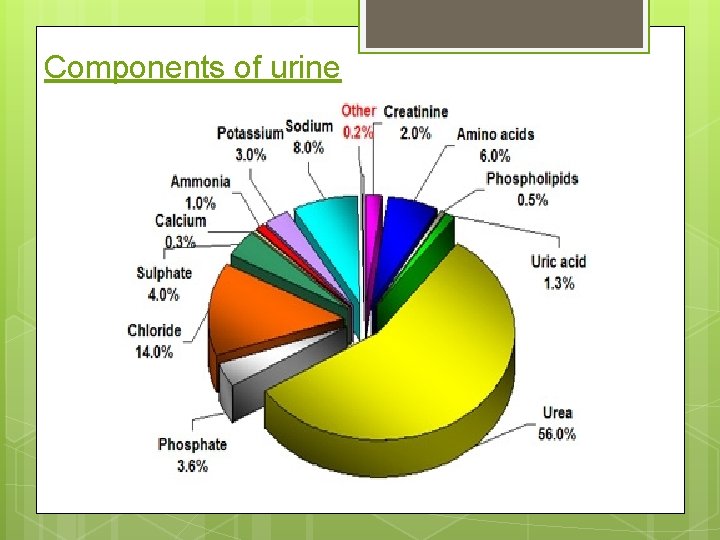
Components of urine
Collection requirements § § Containers – white/red/green topped Discuss. Mid stream Early morning Sample storage < 2 hrs or kept at 4 c out of direct sunlight - DISCUSS
Types of sample § § Random – most common for infection. Early morning urine (EMU) – has greater concentration of substances (micro-album. Inuria). § Clean catch midstream (MSU) – genitalia should be cleaned, urine is tested for micro-organisms for presence of infection (culture & sensitivity). § Timed – specific time of day, always discard the 1 st specimen before testing. § 24 hour – used for quantitative and qualitative analysis of substances.
Types of testing § § § Physical Chemical Microscopic
Physical examination of urine Done with the naked eye, a very important part of the test. Findings should be documented. § § Colour (affected by drugs, food, general condition). Turbidity (clear; cloudy, particles). Volume. Odour (affected by infection, diet)
Chemical testing of urine § Usually done with reagent strips. § Used to determine body processes such as carbohydrate metabolism, liver or kidney function. § Used to determine infection. § Can be used to determine presence of drug or toxic environmental substances.
Some chemicals that can be found in urine (not normal components) § Ketones. p. H – acid/alkaline balance. Blood Bilirubin (urobilinogen) Glucose Protein Nitrates Leukocytes drugs § Phenylketones – indicates PKU – a rare genetic disorder of one of the liver § § § § enzymes. If left, can cause a build up of the chemical in the blood and brain which can cause mental development issues and epilepsy – screened for in babies 1 st week of life with heel prick test.
Microscopic examination of urine § § Used to examine the elements not visible without a microscope. Centrifuge spins the urine to separate substances. • Cells • Crystal • Casts • Bacteria • Yeasts • Parasites
Other tests § Pregnancy tests – EIA (enzyme immunoassay test) used to detect human chorionic gonadotrophin (h. CG), secreted by the placenta. § STIs - chlamydia
The manual dipstick test
Do’s and don’ts DO § § § Follow manufacturers instruction. Ensure the sample is in the correct container for the test required (red/white top). Ensure correct reagent strips are selected for the required test. Discuss. Always check and record the appearance of the urine sample. Return the top on the reagent strip bottle. TIMING IS ESSENTIAL for reliable results.
Do’s and don’ts DON’T § § § Remove the desiccant from the reagant strip bottle. Touch the test areas of the strip. Take out more strips than are required for immediate use.
Quality control
Sample requirements § § § Patients should instructed on how to collect the sample. Sterile containers should be used to collect the sample All samples must be properly labelled with the patient ID. Ensure the sample is in the correct container for the test required. The first sample on waking should be used for microalbum. Inuria as other samples may be less concentrated.
Patient instruction ‘How should I collect and store a urine sample? ” NHS choices (11/10/2013) To collect a clean urine sample: § § § § label the container with your name, date of birth and the date wash your hands men should wash their penis women should wash their genitals, including between the labia (lips around the entrance to the vagina) start to urinate but don’t collect the first part of urine that comes out collect a sample of urine ‘mid-stream’ (see below) in a sterile screw-top container screw the lid of the container shut wash your hands thoroughly http: //www. nhs. uk/chq/pages/how-should-i-collect-and-store-a-urinesample. aspx? Category. ID=69&Sub. Category. ID=692
Materials/equipment required for dipstick testing § § § § Reagent/test strips – in-date and stored correctly Watch Urine sample in suitable container Gloves Good lighting Access to hand washing and drying Suitable room (sluice) for testing Suitable waste disposal - discuss
Manual Test procedure ① ② ③ ④ ⑤ Wear gloves. Ensure the sample is in the correct container. Check the appearance of the sample and record results. Ensure the strips have been stored properly & are in-date. Remove the cap, take out strip and replace the cap on the bottle.
Manual Test procedure ⑥ ⑦ ⑧ Using the appropriate reagent strip completely immerse all reagent areas into the sample. Dip briefly and remove immediately to avoid dissolving out the reagents. While removing the strip, run the edge against the rim of the urine container to remove excess urine. Hold the strip in a horizontal position to prevent possible mixing of chemicals from the adjacent areas.
Manual Test procedure ⑨ ⑩ After the appropriate time, compare test areas closely with the corresponding colour chart on the bottle label at the specified time. Hold the strip close to the colour blocks and match carefully. Always record results.


Sources of error § § § § § Incorrect dipping of reagent strip. Incomplete wetting of strip. Incorrect storage of strips – always check manufacturers instructions. Sample error – sample must be allowed to return to room temperature, non sterile containers; sample needs to be fresh for best results. Contamination of the reagant pad by handling or non sterile container. p. H may be falsely elevated if the urine is stale. Some medication can affect some of the reagents on the strips (e. g. cephalosporins; L-dopa; high levels of salicylates; chlorhexadine; ferrous sulphate) Strips out of date. Vegetarians may have a urine p. H >8.
Visual significance of urinalysis § Colour: The colour and clarity of the urine has significant implications and should always be noted. The colour of normal urine varies with its concentration, from deep yellow to almost clear. In disease, the colour may be abnormal due to excretion of the endogenous pigments as well as drugs and their metabolites. § Odour: Odour in the urine of patients who have a urinary tract infection, is often due to the urea-splitting organisms. This makes it smell ammonia. The presence of urinary ketones, as in diabetic ketoacidosis, leads to an acetone smell. The presence of malodorous urine does not indicate the presence of infection and does not negate the need for testing.
Clinical significance of test results § § § Glucose - is found when its concentration in plasma exceed the renal threshold (may indicate diabetes) Bilirubin/urobilinogen – indicates an excess in the plasma. Commonest cause of positive results is liver cell injury e. g. hepatitis, paracetamol overdose, latestage cirrhosis. Ketones – due to excessive breakdown of body fat. Common in fasting, may indicate low carbohydrate diet, vomiting & fever, present in starvation
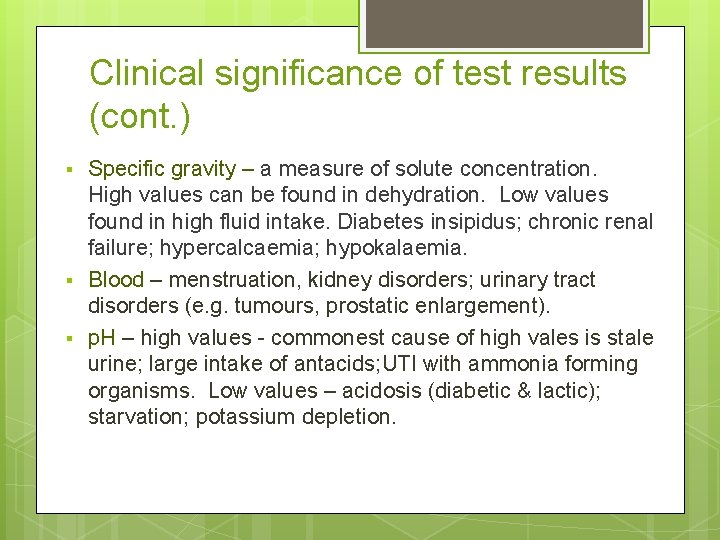
Clinical significance of test results (cont. ) § § § Specific gravity – a measure of solute concentration. High values can be found in dehydration. Low values found in high fluid intake. Diabetes insipidus; chronic renal failure; hypercalcaemia; hypokalaemia. Blood – menstruation, kidney disorders; urinary tract disorders (e. g. tumours, prostatic enlargement). p. H – high values - commonest cause of high vales is stale urine; large intake of antacids; UTI with ammonia forming organisms. Low values – acidosis (diabetic & lactic); starvation; potassium depletion.
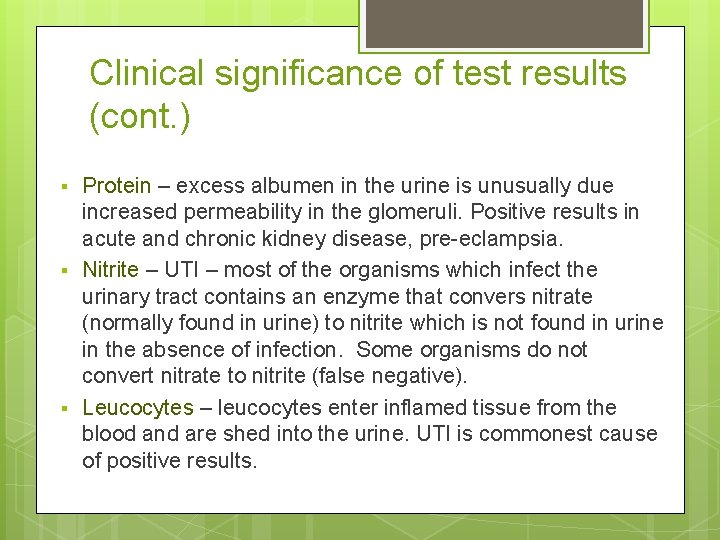
Clinical significance of test results (cont. ) § § § Protein – excess albumen in the urine is unusually due increased permeability in the glomeruli. Positive results in acute and chronic kidney disease, pre-eclampsia. Nitrite – UTI – most of the organisms which infect the urinary tract contains an enzyme that convers nitrate (normally found in urine) to nitrite which is not found in urine in the absence of infection. Some organisms do not convert nitrate to nitrite (false negative). Leucocytes – leucocytes enter inflamed tissue from the blood and are shed into the urine. UTI is commonest cause of positive results.
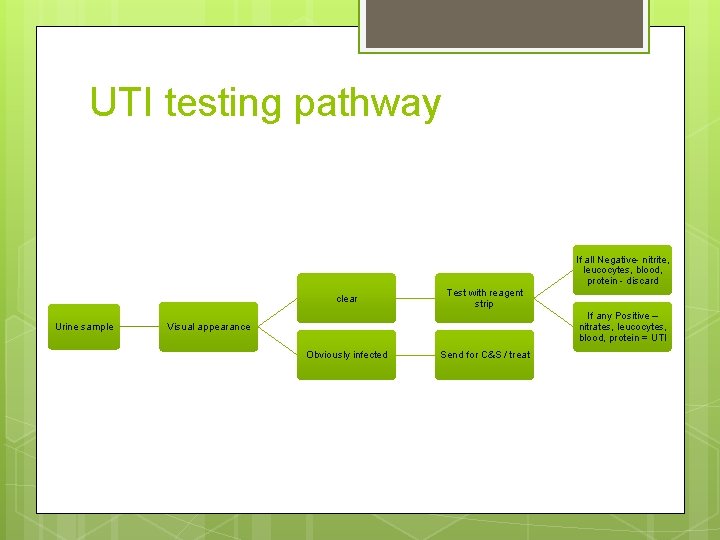
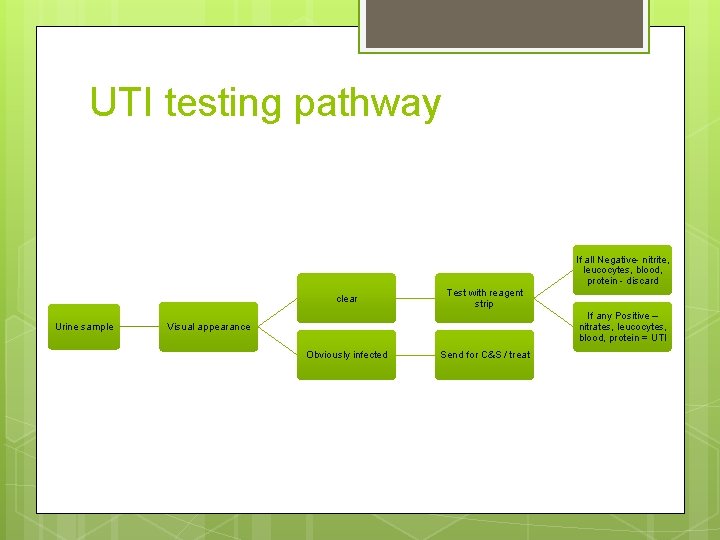
UTI testing pathway If all Negative- nitrite, leucocytes, blood, protein - discard clear Urine sample Test with reagent strip If any Positive – nitrates, leucocytes, blood, protein = UTI Visual appearance Obviously infected Send for C&S / treat
Any questions?
 Dipstick test
Dipstick test Dipstick 1+
Dipstick 1+ Pyuria leukocytes urine
Pyuria leukocytes urine Urine cast
Urine cast Urinalysis lab
Urinalysis lab Why urinalysis is done
Why urinalysis is done Urinalysis context clues
Urinalysis context clues Urinalysis case study
Urinalysis case study Microscopic observations data sheet answers
Microscopic observations data sheet answers Decreased specific gravity of urine
Decreased specific gravity of urine Urinalysis sediment
Urinalysis sediment Mneme pronunciation
Mneme pronunciation Dtp lite usmc
Dtp lite usmc Urinalysis result interpretation chart
Urinalysis result interpretation chart Treatments for acute renal failure
Treatments for acute renal failure Lynne korte
Lynne korte Pixel. com
Pixel. com Lynne hillenbrand
Lynne hillenbrand Lynne barasch
Lynne barasch Lynne russell
Lynne russell Dr lynne drummond
Dr lynne drummond Joe tinning today
Joe tinning today Birthday present by lynne reid banks
Birthday present by lynne reid banks Lynne abruzzo
Lynne abruzzo Lynne finley district clerk
Lynne finley district clerk Lynne hybels
Lynne hybels Vance jennings
Vance jennings The great kapok tree vocabulary
The great kapok tree vocabulary Bayard powell
Bayard powell Discus login
Discus login Brooks secondary
Brooks secondary Isomorfismo powell di maggio
Isomorfismo powell di maggio John powell escritor
John powell escritor Powell agenda
Powell agenda Cancas osu
Cancas osu Goldie hawn mbti
Goldie hawn mbti Recursos interpretativos
Recursos interpretativos Colegio baden powell preparatoria
Colegio baden powell preparatoria