MALNUTRITION IN THE ACUTE CARE SETTING Mackenzie Martindale
- Slides: 21
MALNUTRITION IN THE ACUTE CARE SETTING Mackenzie Martindale, Silvia Lopez-Ross, Nicole Treas Aramark Distance Dietetic Internship Emerging Trends Research Project Spring 2016
Learning Objectives • Understand the meaning of malnutrition • Recognize the prevalence of malnutrition in the acute care setting • Understand the causes and consequences of the problem • Describe role of Registered Dietitian (RD) language in accurate coding of malnutrition • Learn the benefits of diagnosing malnutrition • Use of the Nutrition Focused Physical Exam • Hospital reimbursement for malnutrition
Malnutrition: What is it? Malnutrition is a state of nutrition in which a deficiency, excess, or imbalance of energy, protein and other nutrients cause adverse effects on body structure, function, and the clinical outcome of the patient. Malnutrition can be both undernutrition and overnutrition. § Starvation § Chronic Disease § Acute Disease/Injury § Kwashiorkor § Marasmus White JV, Guenter P, Jensen G, et al. Consensus Statement: Academy of Nutrition and Dietetics and America Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition), J Acad Nutr Diet. 2012; 112: 730 -783.
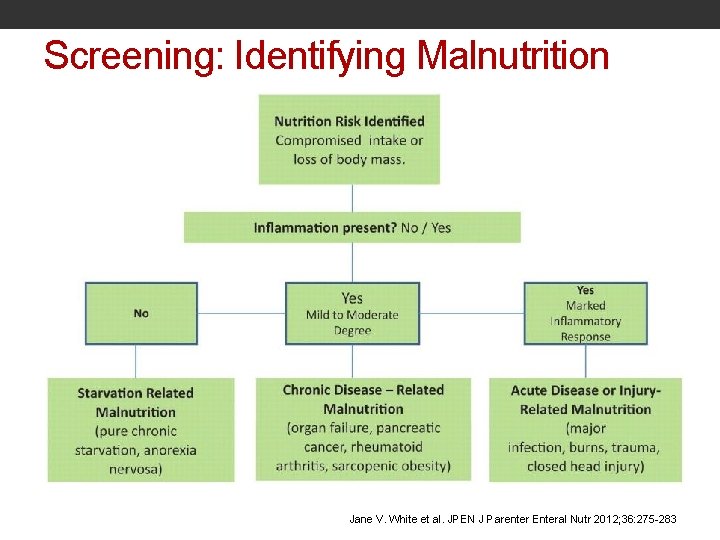
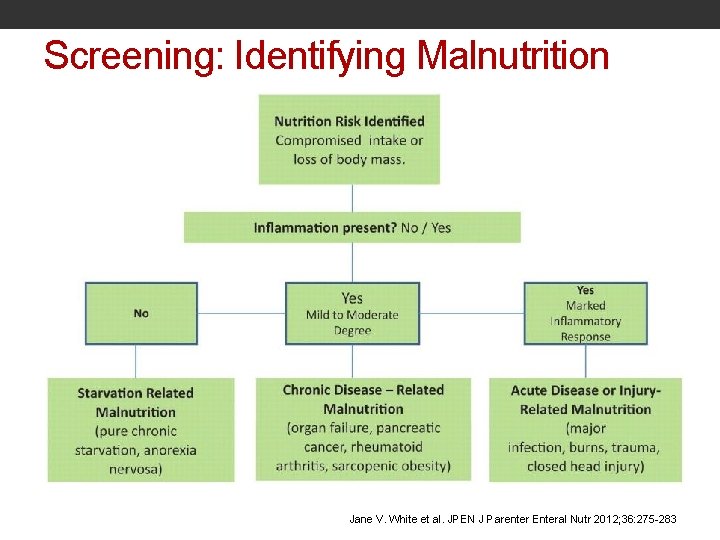
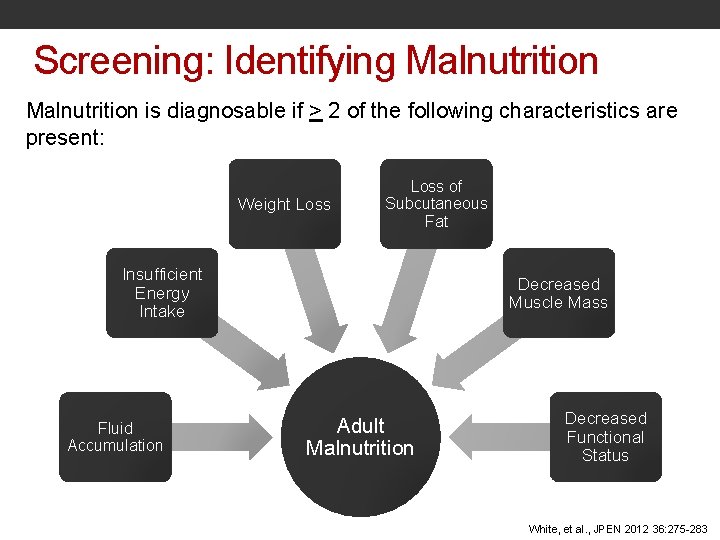
Screening: Identifying Malnutrition Jane V. White et al. JPEN J Parenter Enteral Nutr 2012; 36: 275 -283
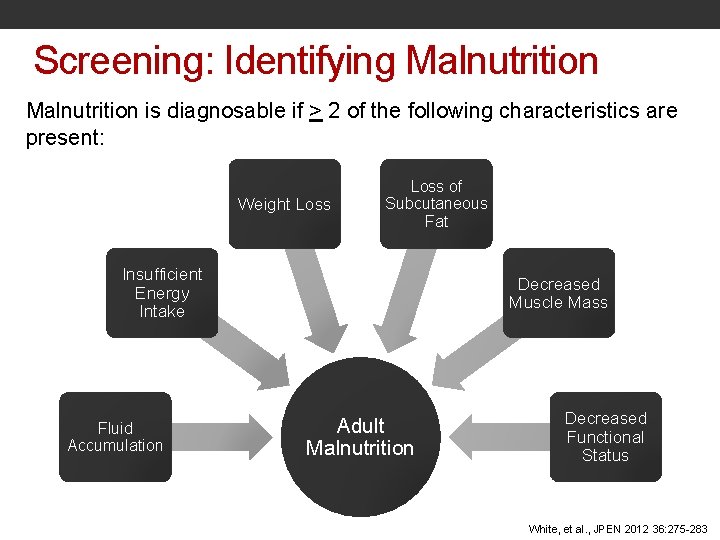
Screening: Identifying Malnutrition is diagnosable if > 2 of the following characteristics are present: Weight Loss of Subcutaneous Fat Insufficient Energy Intake Fluid Accumulation Decreased Muscle Mass Adult Malnutrition Decreased Functional Status White, et al. , JPEN 2012 36: 275 -283
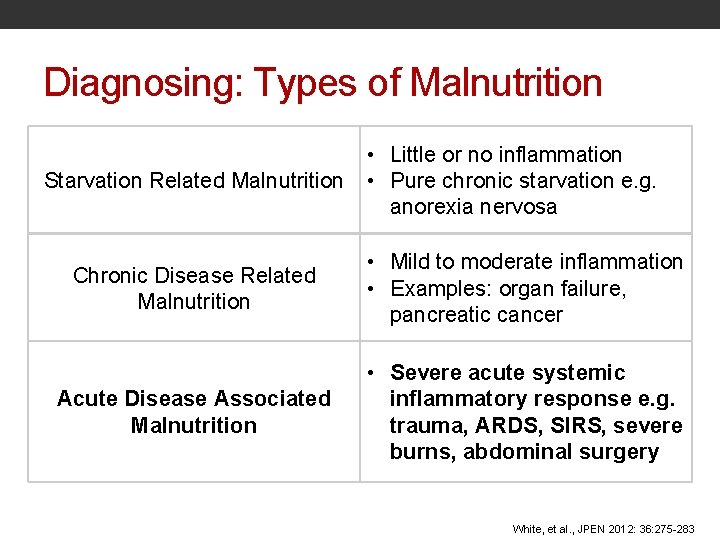
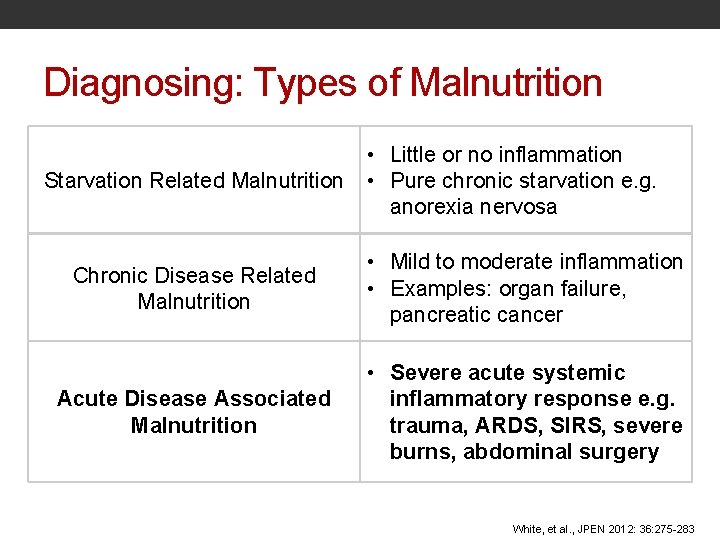
Diagnosing: Types of Malnutrition Starvation Related Malnutrition • Little or no inflammation • Pure chronic starvation e. g. anorexia nervosa Chronic Disease Related Malnutrition • Mild to moderate inflammation • Examples: organ failure, pancreatic cancer Acute Disease Associated Malnutrition • Severe acute systemic inflammatory response e. g. trauma, ARDS, SIRS, severe burns, abdominal surgery White, et al. , JPEN 2012: 36: 275 -283
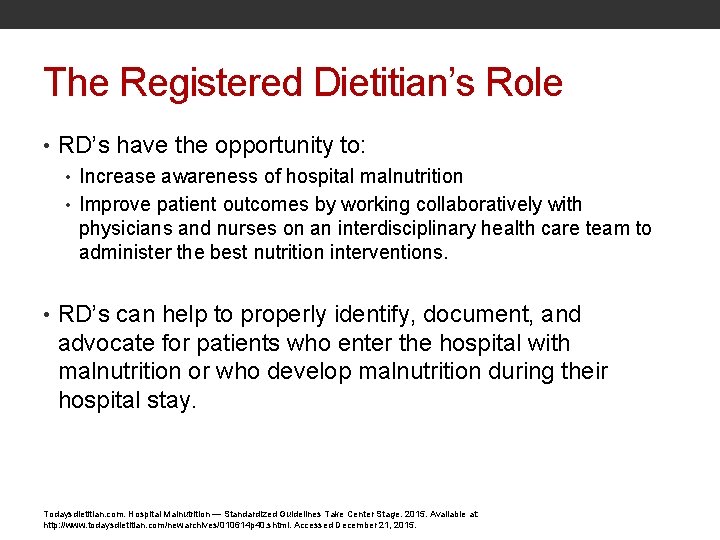
The Registered Dietitian’s Role • RD’s have the opportunity to: • Increase awareness of hospital malnutrition • Improve patient outcomes by working collaboratively with physicians and nurses on an interdisciplinary health care team to administer the best nutrition interventions. • RD’s can help to properly identify, document, and advocate for patients who enter the hospital with malnutrition or who develop malnutrition during their hospital stay. Todaysdietitian. com. Hospital Malnutrition — Standardized Guidelines Take Center Stage. 2015. Available at: http: //www. todaysdietitian. com/newarchives/010614 p 40. shtml. Accessed December 21, 2015.
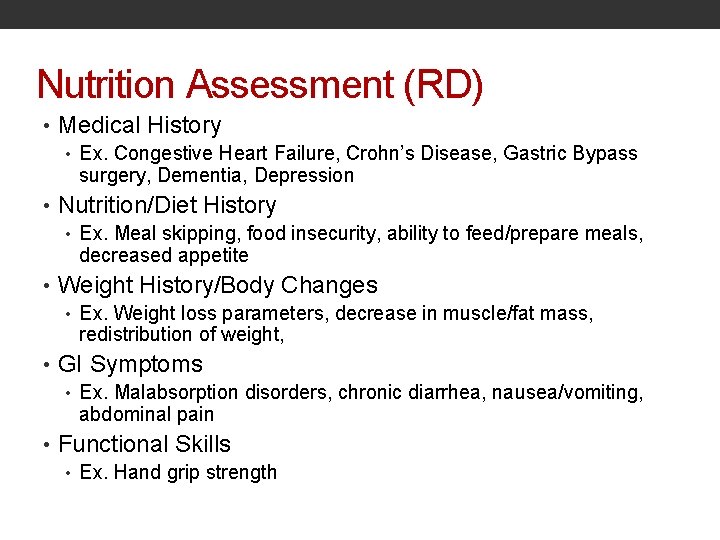
Nutrition Assessment (RD) • Medical History • Ex. Congestive Heart Failure, Crohn’s Disease, Gastric Bypass surgery, Dementia, Depression • Nutrition/Diet History • Ex. Meal skipping, food insecurity, ability to feed/prepare meals, decreased appetite • Weight History/Body Changes • Ex. Weight loss parameters, decrease in muscle/fat mass, redistribution of weight, • GI Symptoms • Ex. Malabsorption disorders, chronic diarrhea, nausea/vomiting, abdominal pain • Functional Skills • Ex. Hand grip strength
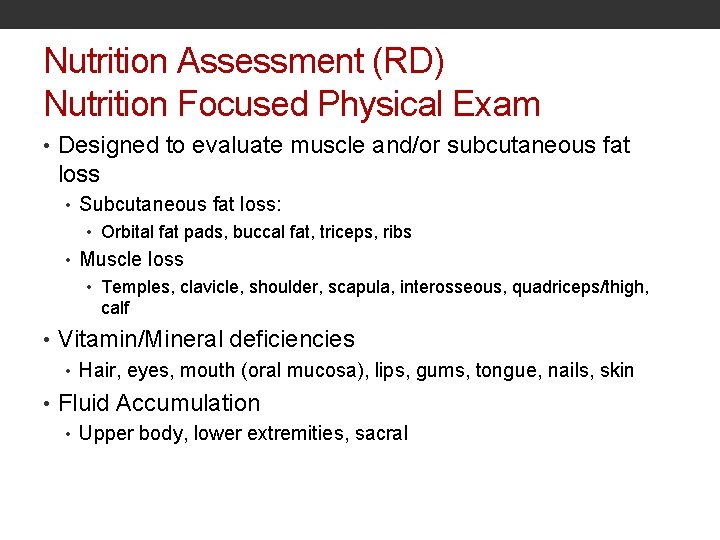
Nutrition Assessment (RD) Nutrition Focused Physical Exam • Designed to evaluate muscle and/or subcutaneous fat loss • Subcutaneous fat loss: • Orbital fat pads, buccal fat, triceps, ribs • Muscle loss • Temples, clavicle, shoulder, scapula, interosseous, quadriceps/thigh, calf • Vitamin/Mineral deficiencies • Hair, eyes, mouth (oral mucosa), lips, gums, tongue, nails, skin • Fluid Accumulation • Upper body, lower extremities, sacral
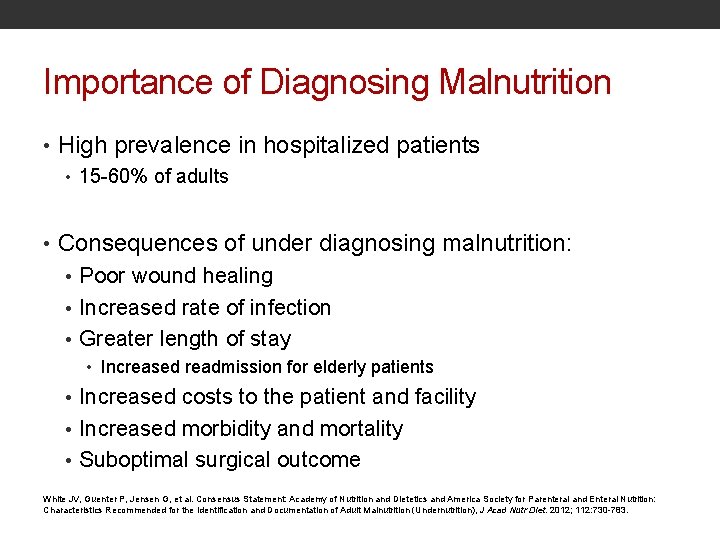
Importance of Diagnosing Malnutrition • High prevalence in hospitalized patients • 15 -60% of adults • Consequences of under diagnosing malnutrition: • Poor wound healing • Increased rate of infection • Greater length of stay • Increased readmission for elderly patients • Increased costs to the patient and facility • Increased morbidity and mortality • Suboptimal surgical outcome White JV, Guenter P, Jensen G, et al. Consensus Statement: Academy of Nutrition and Dietetics and America Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition), J Acad Nutr Diet. 2012; 112: 730 -783.
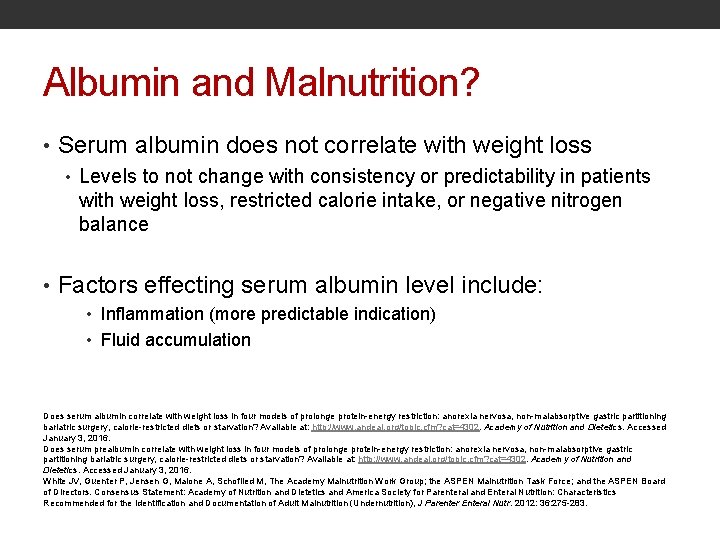
Albumin and Malnutrition? • Serum albumin does not correlate with weight loss • Levels to not change with consistency or predictability in patients with weight loss, restricted calorie intake, or negative nitrogen balance • Factors effecting serum albumin level include: • Inflammation (more predictable indication) • Fluid accumulation Does serum albumin correlate with weight loss in four models of prolonge protein-energy restriction: anorexia nervosa, non-malabsorptive gastric partitioning bariatric surgery, calorie-restricted diets or starvation? Available at: http: //www. andeal. org/topic. cfm? cat=4302. Academy of Nutrition and Dietetics. Accessed January 3, 2016. Does serum prealbumin correlate with weight loss in four models of prolonge protein-energy restriction: anorexia nervosa, non-malabsorptive gastric partitioning bariatric surgery, calorie-restricted diets or starvation? Available at: http: //www. andeal. org/topic. cfm? cat=4302. Academy of Nutrition and Dietetics. Accessed January 3, 2016. White JV, Guenter P, Jensen G, Malone A, Schofiled M, The Academy Malnutrition Work Group; the ASPEN Malnutrition Task Force; and the ASPEN Board of Directors. Consensus Statement: Academy of Nutrition and Dietetics and America Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition), J Parenter Enteral Nutr. 2012: 36: 275 -283.
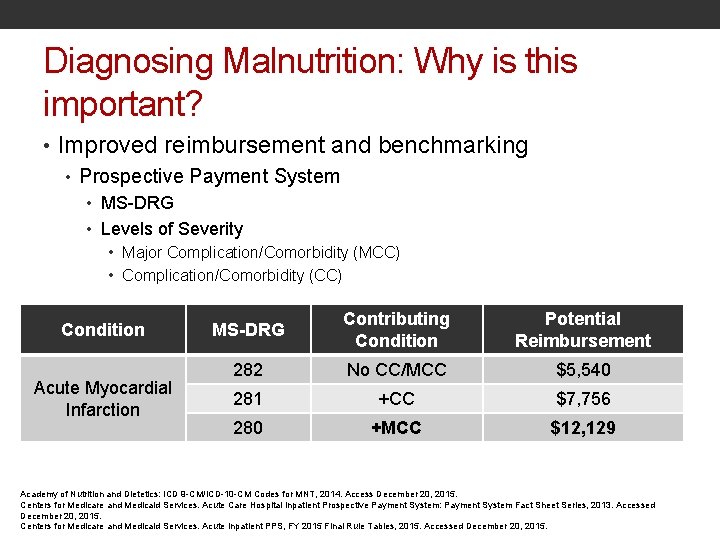
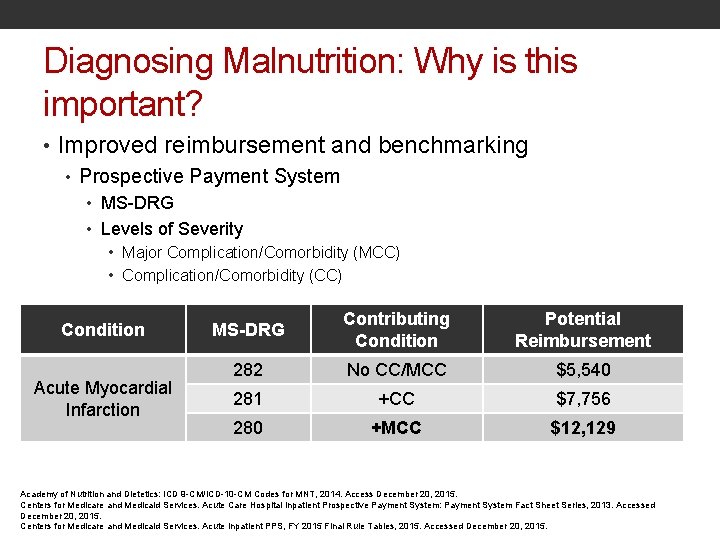
Diagnosing Malnutrition: Why is this important? • Improved reimbursement and benchmarking • Prospective Payment System • MS-DRG • Levels of Severity • Major Complication/Comorbidity (MCC) • Complication/Comorbidity (CC) Condition Acute Myocardial Infarction MS-DRG Contributing Condition Potential Reimbursement 282 No CC/MCC $5, 540 281 +CC $7, 756 280 +MCC $12, 129 Academy of Nutrition and Dietetics: ICD 9 -CM/ICD-10 -CM Codes for MNT, 2014. Access December 20, 2015. Centers for Medicare and Medicaid Services. Acute Care Hospital Inpatient Prospective Payment System: Payment System Fact Sheet Series, 2013. Accessed December 20, 2015. Centers for Medicare and Medicaid Services. Acute Inpatient PPS, FY 2015 Final Rule Tables, 2015. Accessed December 20, 2015.
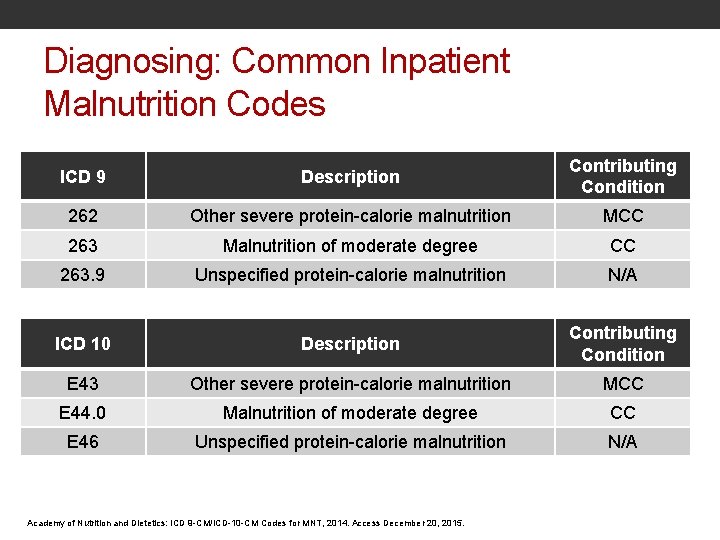
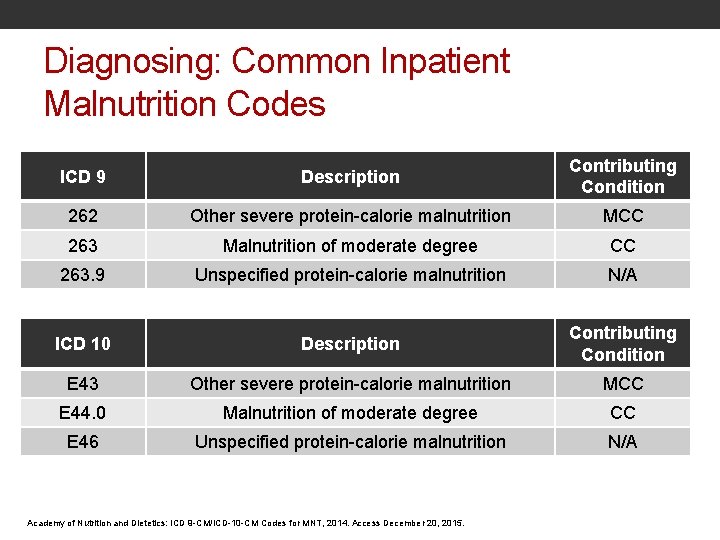
Diagnosing: Common Inpatient Malnutrition Codes ICD 9 Description Contributing Condition 262 Other severe protein-calorie malnutrition MCC 263 Malnutrition of moderate degree CC 263. 9 Unspecified protein-calorie malnutrition N/A ICD 10 Description Contributing Condition E 43 Other severe protein-calorie malnutrition MCC E 44. 0 Malnutrition of moderate degree CC E 46 Unspecified protein-calorie malnutrition N/A Academy of Nutrition and Dietetics: ICD 9 -CM/ICD-10 -CM Codes for MNT, 2014. Access December 20, 2015.
Treatment of Malnutrition in Hospitalized Patients • 1996: Joint Commission mandated nutritional screening within 24 hours of admission • Referral to RD • Encourage PO intake upon admission (if medically feasible) • Allow least restrictive diet if PO intake is decreased • Offer nutritional drink supplements when applicable • Administer EN/TPN as soon as medically feasible (when necessary) Barker LA, Gout BS, Crowe TC. Hospital Malnutrition: Prevalence, Identification and Impact on Patients and the Healthcare System. International Journal of Environmental Research and Public Health. 2011; 8(2): 514 -527. doi: 10. 3390/ijerph 8020514.
Treatment: Desired Outcomes • Improved early identification of patients at-risk for malnutrition • Precise classification and coding of malnourished patients • Earlier and more aggressive interventions for malnourished patients • Increased physician support for nutrition recommendations Kathryn Chiles RD, LD, CNSC
What’s Next? • How we determine if appropriate to complete nutrition focused physical exam: • Meet two other criteria (% PO intake, % Wt. loss, fluid status, functional status) • Current treatment plan and/or goals of care • Challenges within different hospital settings • Inpatient • Outpatient • Intensive Care Unit • Co-managed documentation with physicians • We have to work together as a care team
Review of Key Points • Acute malnutrition in hospitals related to inadequate intake is prevalent • Feeding protocols can successfully reduce calorie deficits when implemented. • However, they are not a “One Size Fits All” approach • Continuous education, monitoring, and modification of protocol • Identify opportunities for multidisciplinary involvement and investment to maximize success • Malnutrition Diagnosis increase hospital reimbursement
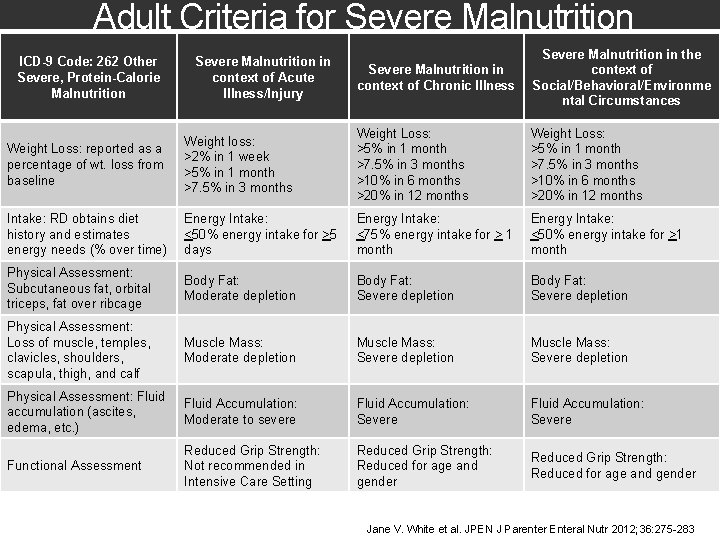
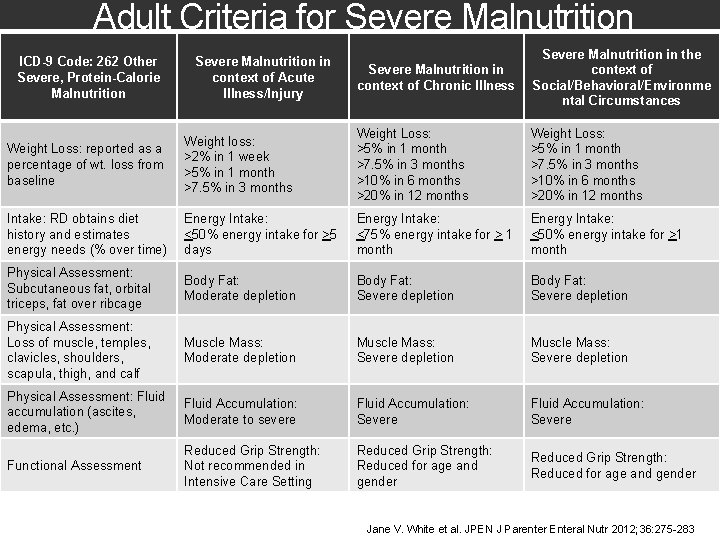
Adult Criteria for Severe Malnutrition in context of Chronic Illness Severe Malnutrition in the context of Social/Behavioral/Environme ntal Circumstances Weight Loss: reported as a percentage of wt. loss from baseline Weight loss: >2% in 1 week >5% in 1 month >7. 5% in 3 months Weight Loss: >5% in 1 month >7. 5% in 3 months >10% in 6 months >20% in 12 months Intake: RD obtains diet history and estimates energy needs (% over time) Energy Intake: <50% energy intake for >5 days Energy Intake: <75% energy intake for > 1 month Energy Intake: <50% energy intake for >1 month Physical Assessment: Subcutaneous fat, orbital triceps, fat over ribcage Body Fat: Moderate depletion Body Fat: Severe depletion Physical Assessment: Loss of muscle, temples, clavicles, shoulders, scapula, thigh, and calf Muscle Mass: Moderate depletion Muscle Mass: Severe depletion Physical Assessment: Fluid accumulation (ascites, edema, etc. ) Fluid Accumulation: Moderate to severe Fluid Accumulation: Severe Functional Assessment Reduced Grip Strength: Not recommended in Intensive Care Setting Reduced Grip Strength: Reduced for age and gender ICD-9 Code: 262 Other Severe, Protein-Calorie Malnutrition Severe Malnutrition in context of Acute Illness/Injury Jane V. White et al. JPEN J Parenter Enteral Nutr 2012; 36: 275 -283
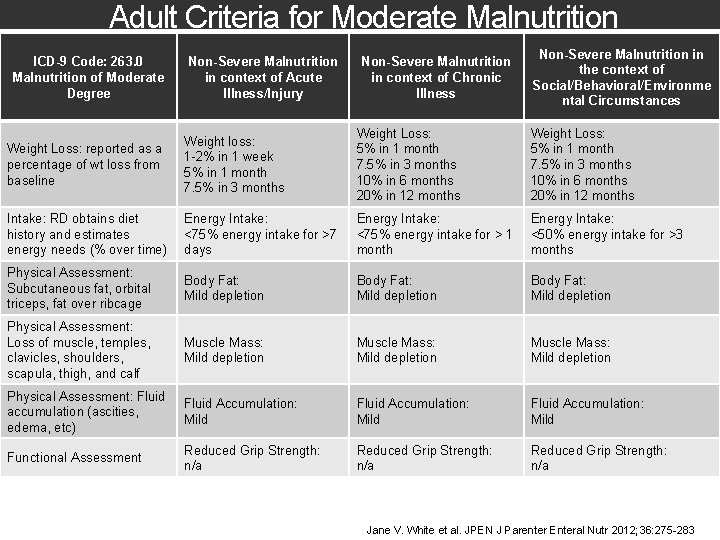
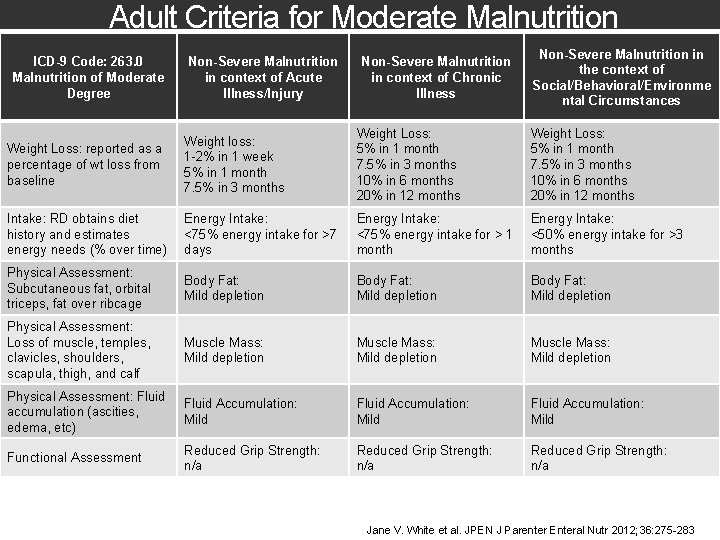
Adult Criteria for Moderate Malnutrition ICD-9 Code: 263. 0 Malnutrition of Moderate Degree Non-Severe Malnutrition in context of Acute Illness/Injury Non-Severe Malnutrition in context of Chronic Illness Non-Severe Malnutrition in the context of Social/Behavioral/Environme ntal Circumstances Weight Loss: reported as a percentage of wt loss from baseline Weight loss: 1 -2% in 1 week 5% in 1 month 7. 5% in 3 months Weight Loss: 5% in 1 month 7. 5% in 3 months 10% in 6 months 20% in 12 months Intake: RD obtains diet history and estimates energy needs (% over time) Energy Intake: <75% energy intake for >7 days Energy Intake: <75% energy intake for > 1 month Energy Intake: <50% energy intake for >3 months Physical Assessment: Subcutaneous fat, orbital triceps, fat over ribcage Body Fat: Mild depletion Physical Assessment: Loss of muscle, temples, clavicles, shoulders, scapula, thigh, and calf Muscle Mass: Mild depletion Physical Assessment: Fluid accumulation (ascities, edema, etc) Fluid Accumulation: Mild Functional Assessment Reduced Grip Strength: n/a Jane V. White et al. JPEN J Parenter Enteral Nutr 2012; 36: 275 -283
Thank you! If you have questions please email us at: martindale-mackenzie@aramark. com (CHI St. Luke’s Medical Center) Treas-nicole 2@aramark. com (Williamsport Regional Medical Center) Lopezross-silvia@aramark. com (Bronx Lebanon Medical Center, Wycoff Hospital)
References White JV, Guenter P, Jensen G, Malone A, Schofiled M, The Academy Malnutrition Work Group; the ASPEN Malnutrition Task Force; and the ASPEN Board of Directors. Consensus Statement: Academy of Nutrition and Dietetics and America Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition), J Parenter Enteral Nutr. 2012: 36: 275 -283. Etiology-based malnutrition definitions. Adapted with permission from Jensen GL, Bistrian B, Roubenoff R, Heimburger DC. Malnutrition syndromes: a conundrum vs continuum. JPEN J Parenter Enteral Nutr. 2009; 33: 710. Does serum albumin correlate with weight loss in four models of prolonge protein-energy restriction: anorexia nervosa, nonmalabsorptive gastric partitioning bariatric surgery, calorie-restricted diets or starvation? Available at: http: //www. andeal. org/topic. cfm? cat=4302. Academy of Nutrition and Dietetics. Accessed January 3, 2016. Does serum prealbumin correlate with weight loss in four models of prolonge protein-energy restriction: anorexia nervosa, nonmalabsorptive gastric partitioning bariatric surgery, calorie-restricted diets or starvation? Available at: http: //www. andeal. org/topic. cfm? cat=4302. Academy of Nutrition and Dietetics. Accessed January 3, 2016. Barker LA, Gout BS, Crowe TC. Hospital Malnutrition: Prevalence, Identification and Impact on Patients and the Healthcare System. International Journal of Environmental Research and Public Health. 2011; 8(2): 514 -527. doi: 10. 3390/ijerph 8020514.
 Moderate acute malnutrition
Moderate acute malnutrition Malnutrition case presentation
Malnutrition case presentation Martindale medicines complete
Martindale medicines complete Liz martindale
Liz martindale Primary secondary tertiary health care definition
Primary secondary tertiary health care definition Acute care collaboration
Acute care collaboration Acute care toolkit
Acute care toolkit Chronic pancreatitis nursing care plan
Chronic pancreatitis nursing care plan Mackenzie mbai
Mackenzie mbai Colonel mackenzie comanche
Colonel mackenzie comanche Jessica rowling
Jessica rowling Chremamorphism
Chremamorphism Mackenzie gorman
Mackenzie gorman Quantos jogadores formam uma equipe de futsal? *
Quantos jogadores formam uma equipe de futsal? * Principios iluministas
Principios iluministas Dr monique mackenzie
Dr monique mackenzie Act 4 scene 3 macbeth
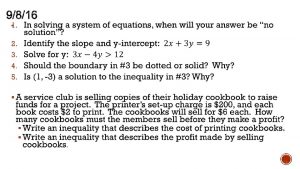
Act 4 scene 3 macbeth Each week mackenzie can make 10 to 25 necklaces
Each week mackenzie can make 10 to 25 necklaces Language
Language Alexander mackenzie
Alexander mackenzie (mackenzie) não caracteriza a estética parnasiana: *
(mackenzie) não caracteriza a estética parnasiana: * Mackenzie hollister bedroom
Mackenzie hollister bedroom