Male Infertility and Impotence Definition n Infertility is












- Slides: 41
Male Infertility and Impotence
Definition n Infertility is “inability to conceive after one year of conjugal life without use of contraceptive methods. ” The term "primary infertility" is applied to “the couple who has never achieved a pregnancy. ” "secondary infertility" implies that “at least one previous conception has taken place. ”
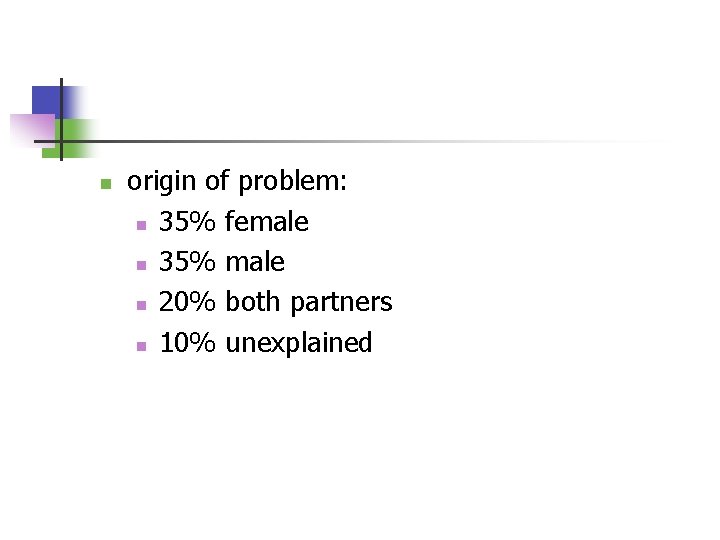
n origin of problem: n 35% female n 35% male n 20% both partners n 10% unexplained

Major Causes
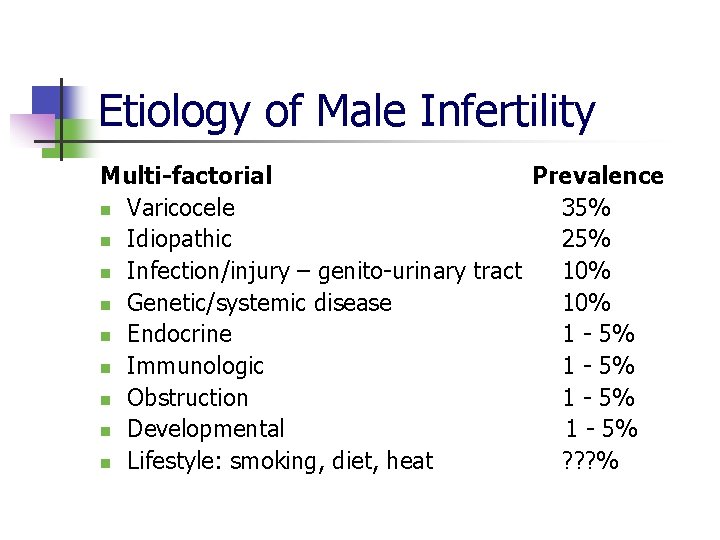
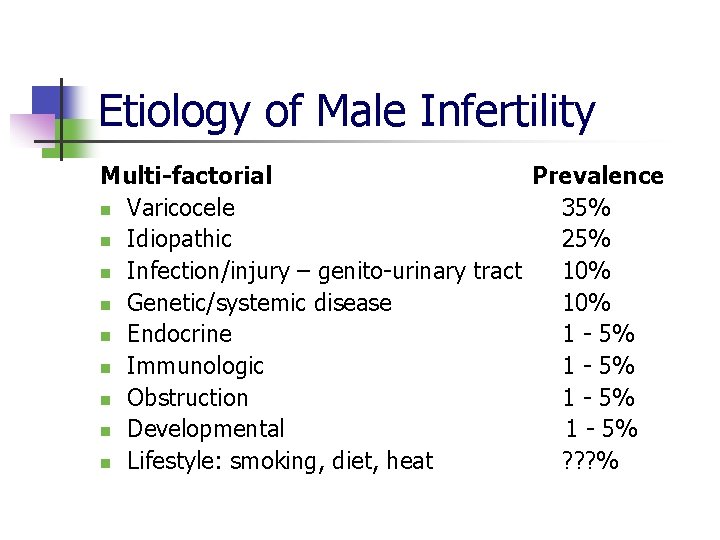
Etiology of Male Infertility Multi-factorial Prevalence n Varicocele 35% n Idiopathic 25% n Infection/injury – genito-urinary tract 10% n Genetic/systemic disease 10% n Endocrine 1 - 5% n Immunologic 1 - 5% n Obstruction 1 - 5% n Developmental 1 - 5% n Lifestyle: smoking, diet, heat ? ? ? %
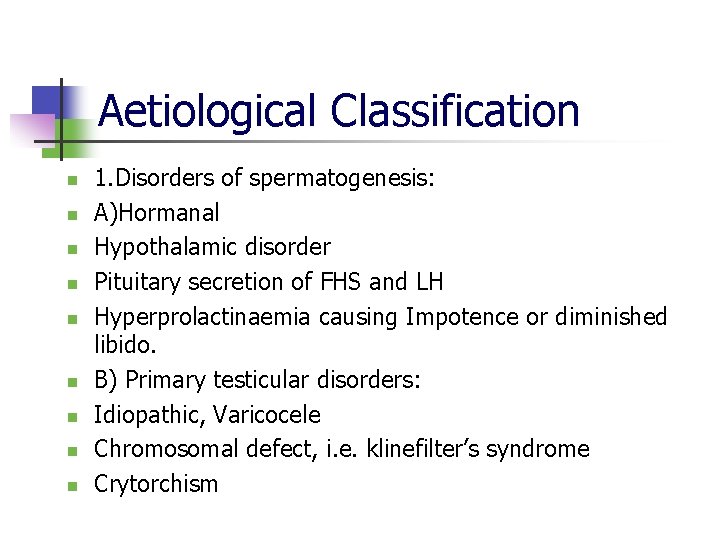
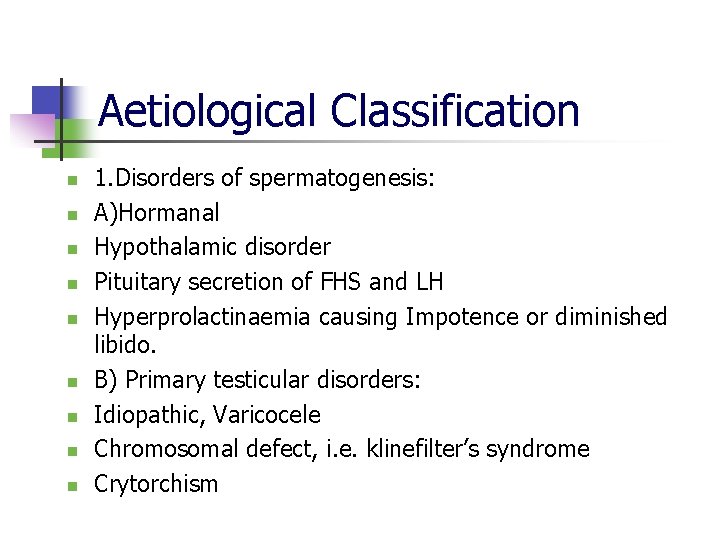
Aetiological Classification n n n n 1. Disorders of spermatogenesis: A)Hormanal Hypothalamic disorder Pituitary secretion of FHS and LH Hyperprolactinaemia causing Impotence or diminished libido. B) Primary testicular disorders: Idiopathic, Varicocele Chromosomal defect, i. e. klinefilter’s syndrome Crytorchism

n n n n Drugs, radiations Orchitis (traumatic, mumps, TB, gonorrhoea) Chronic illness Immunological disorders. 2) Duct obstruction: Congenital absence, inflammatory block, surgical trauma, 3)Accessory glands disorders: Prostitis, vasiculitis, congenital absence of vas in cystic fibrosis.

n n n n n 4. Disorders of sperms and vesicular fluid: Sperms antibodies and low fructose in seminal plasma. Sperms acrosome defect Zona pellucida binding defect Zona penetrations defect Oocyte fusion defect 5. Sexual dysfunctions: Low frequency coitus- wrong time Impotence, hypospadias Premature Ejaculation, retrograte ejaculation

n n 6. Psychological factors and environmental factors like smoking, alcohol consumption, tobacco chewing, diabetes, Drugs: antihypertensive, antipsycotis, sex steroids, chemotherapy, beta-blockers, spirolactone, oestrogen
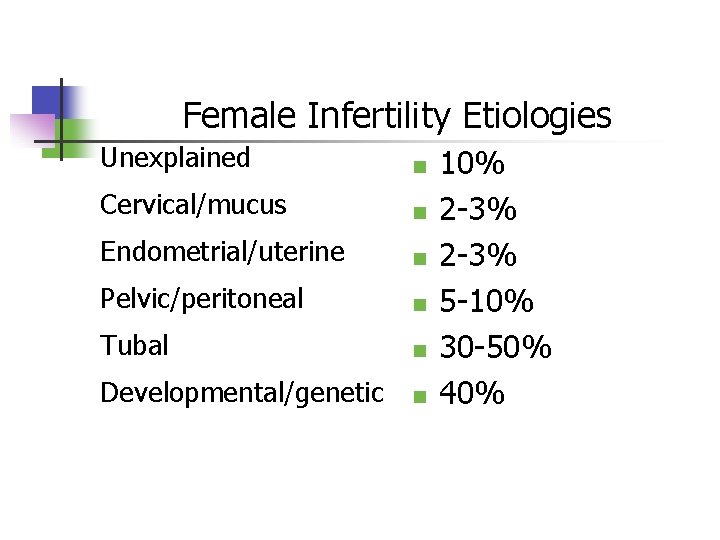
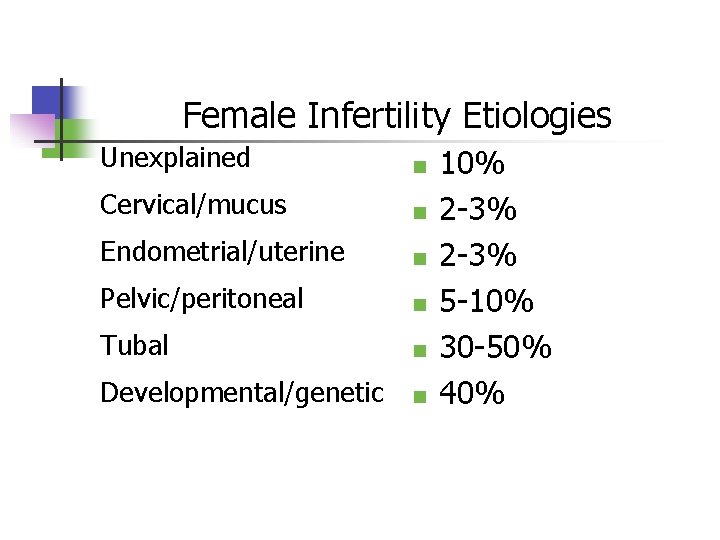
Female Infertility Etiologies Unexplained n Cervical/mucus n Endometrial/uterine n Pelvic/peritoneal n Tubal n Developmental/genetic n 10% 2 -3% 5 -10% 30 -50% 40%
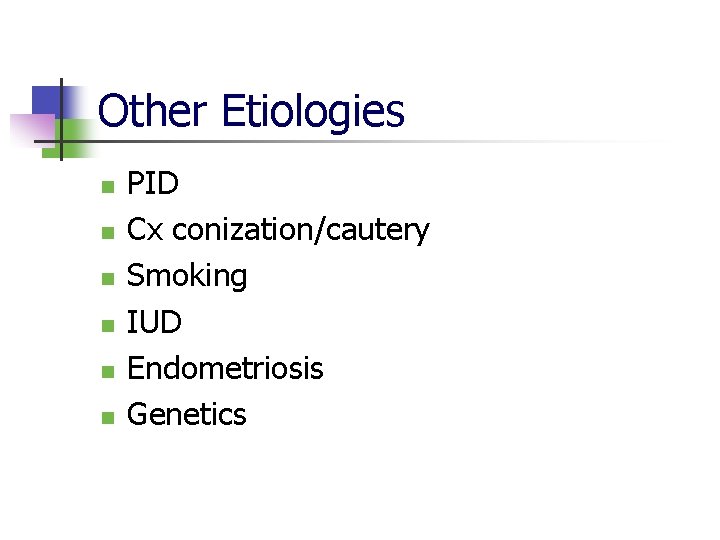
Other Etiologies n n n PID Cx conization/cautery Smoking IUD Endometriosis Genetics
Aetiology n n n n n 1. dyspareunia and vaginal causes 2. Congenital defect in the genital tract. 3. infection in the lower genital tract. 4. Cervical factors 5. Uterine causes 6. Tubal factors 7. Ovaries 8. Peritoneal causes 9. Chronic ill health – especially thyroid dysfuntion
The Most Important Factor in the Evaluation of the Infertile Couple Is: HISTORY
History-General n n n n n Both couples should be present Age Previous pregnancies by each partner Length of time without pregnancy Sexual history Frequency and timing of intercourse Use of lubricants Impotence, anorgasmia, dyspareunia Contraceptive history
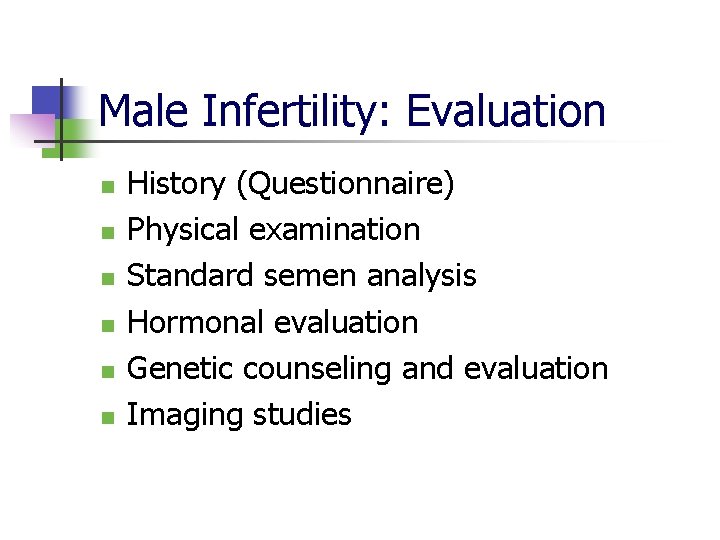
Male Infertility: Evaluation n n n History (Questionnaire) Physical examination Standard semen analysis Hormonal evaluation Genetic counseling and evaluation Imaging studies
History-Male n n n History of pelvic infection Radiation, toxic exposures (include drugs) Mumps Testicular surgery/injury Excessive heat exposure (spermicidal)

Physical Exam-Male n n Size of testicles Testicular descent Varicocoele Outflow abnormalities (hypospadias, etc)
Male Factors-Semen Analysis n n n Collected after 3 days of abstinence Evaluated within one hour of ejaculation If abnormal parameters, repeat twice, 2 weeks apart
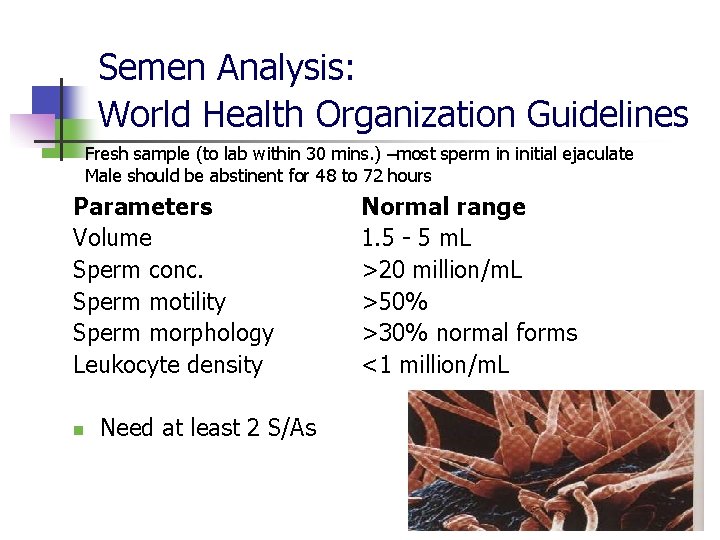
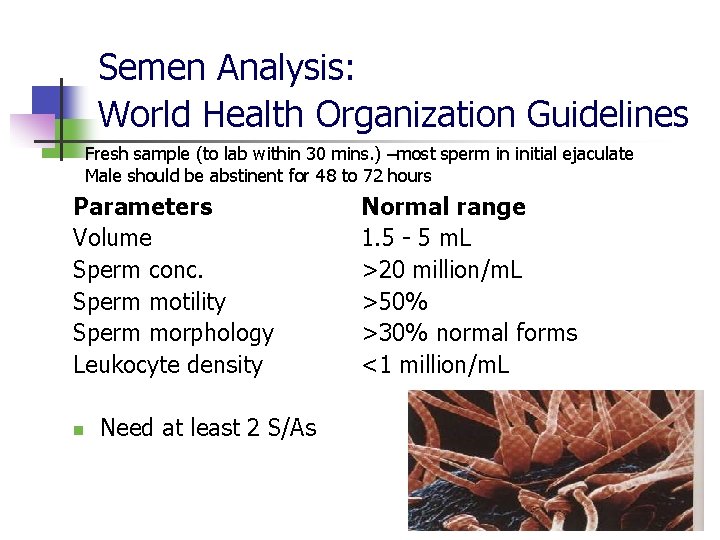
Semen Analysis: World Health Organization Guidelines Fresh sample (to lab within 30 mins. ) –most sperm in initial ejaculate Male should be abstinent for 48 to 72 hours Parameters Volume Sperm conc. Sperm motility Sperm morphology Leukocyte density n Need at least 2 S/As Normal range 1. 5 - 5 m. L >20 million/m. L >50% >30% normal forms <1 million/m. L
Semen Analysis Abnormal semen results n n Azospermia Oligospermia Athenospermia Teratospermia
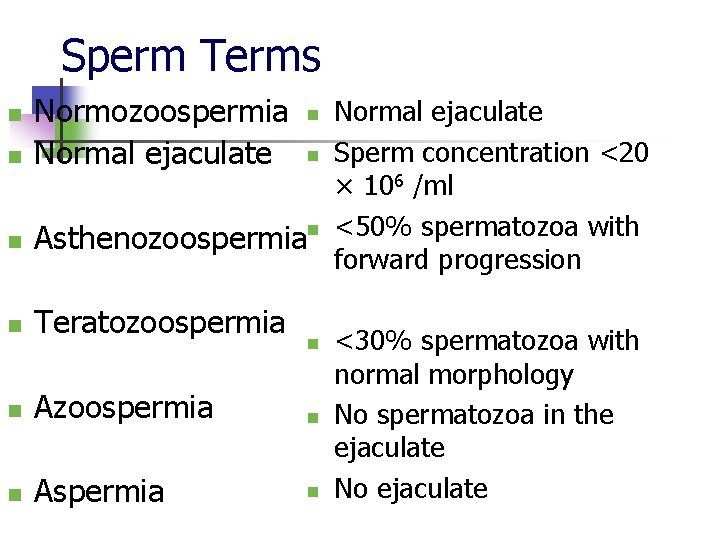
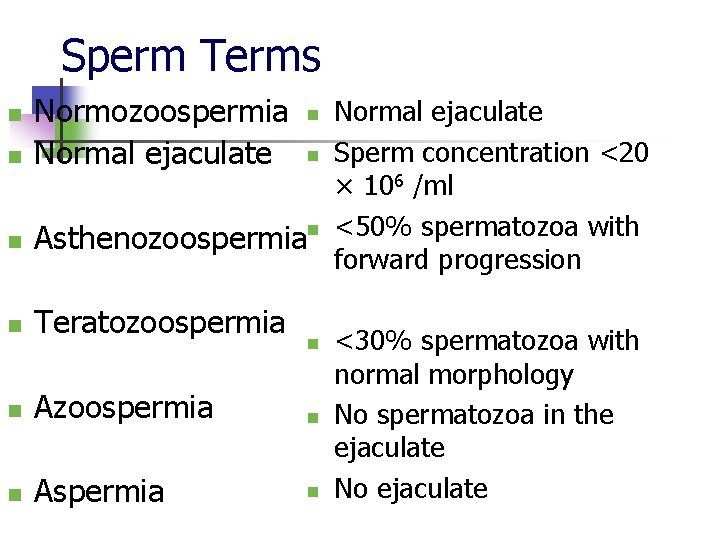
Sperm Terms n n n Normozoospermia Normal ejaculate n Sperm concentration <20 × 106 /ml n <50% spermatozoa with Asthenozoospermia forward progression n n Teratozoospermia n Azoospermia n n Aspermia n n <30% spermatozoa with normal morphology No spermatozoa in the ejaculate No ejaculate
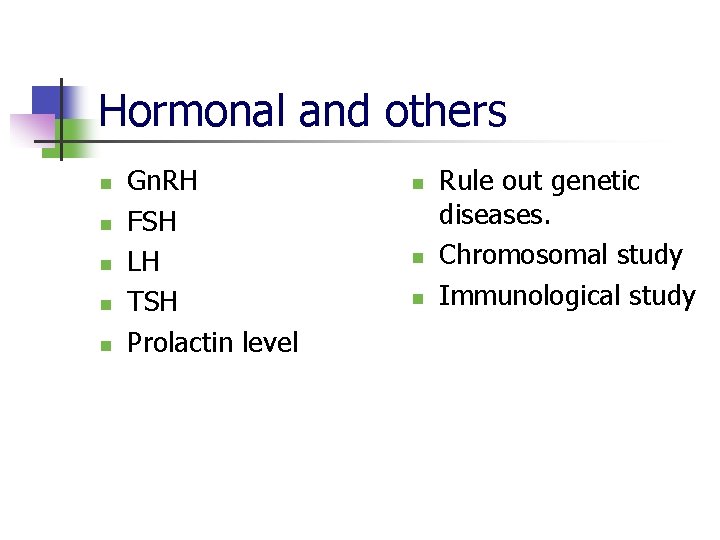
Hormonal and others n n n Gn. RH FSH LH TSH Prolactin level n n n Rule out genetic diseases. Chromosomal study Immunological study
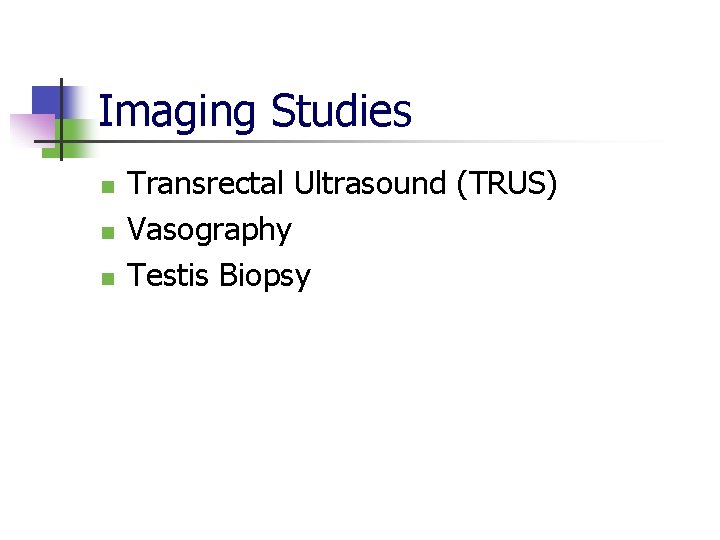
Imaging Studies n n n Transrectal Ultrasound (TRUS) Vasography Testis Biopsy
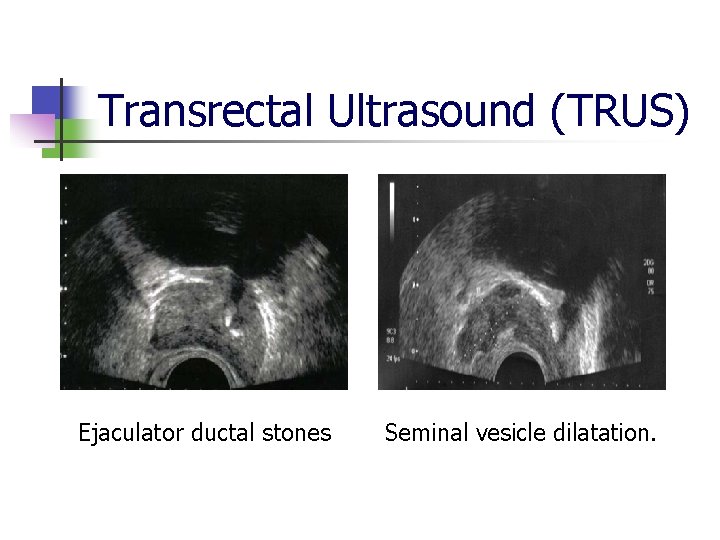
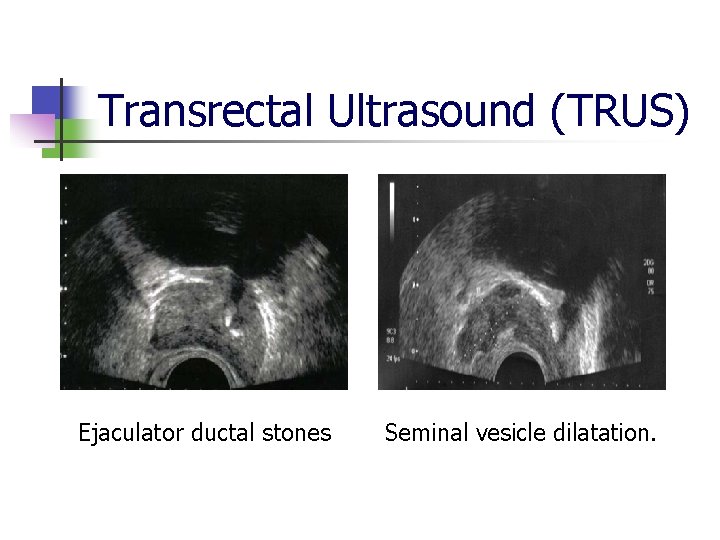
Transrectal Ultrasound (TRUS) Ejaculator ductal stones Seminal vesicle dilatation.
Vasography n Indication n n Assessment of vasal obstruction or ejaculatory duct obstruction. An inguinal vasal obstruction should be suspected in an azoospermic patient with normal spermatogenesis and a history of prior inguinal or scrotal surgery.
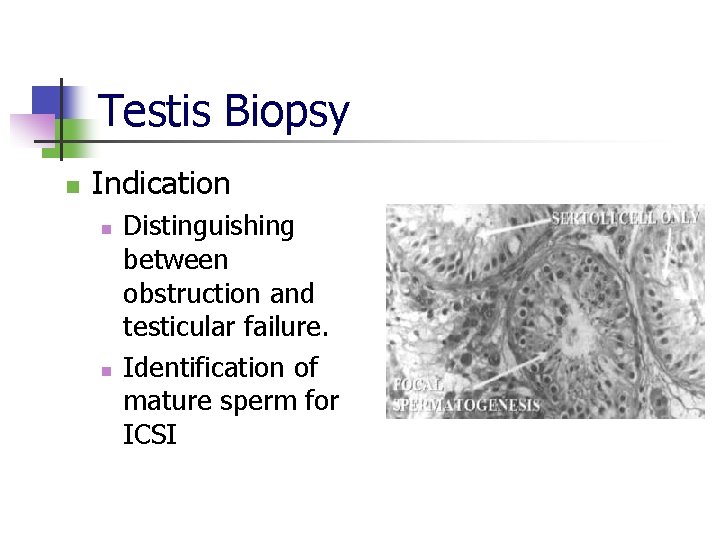
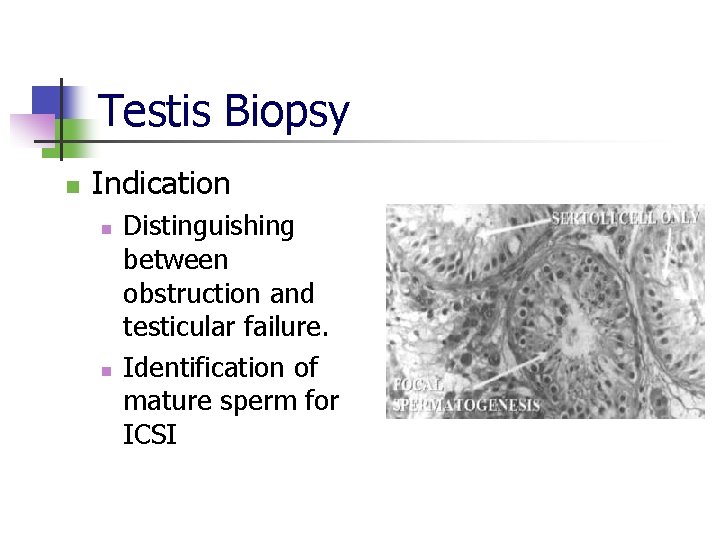
Testis Biopsy n Indication n n Distinguishing between obstruction and testicular failure. Identification of mature sperm for ICSI

Treatment- Male Factor n n n n Hypogonadotrophism: -Gn. RH Ligation Retrograde ejaculation Testosterone for spermatogenesis Clomiphene 50 mg daily for 3 months for oligospermia. Empierical medical therapy by administration of vit. c , B 12, folic acid. Varicocele: - surgical treatment Obstruction: -short-cut operation IVF/IUI : - last option.
Female Infertility: Evaluation n n n History (Questionnaire) Physical examination Ovarian factor Tubal factors Hormonal analysis Immunological test Postcoital test
History-Female n n n n Previous female pelvic surgery PID/Infection Medical diseases: -TB, diabetes, STD IUD use/MR done Ectopic pregnancy history Proven fertility Endometriosis
History-Female n n n Irregular menses, amenorrhea, detailed menstrual history Vasomotor symptoms Stress Weight changes Exercise Cervical and uterine surgery
Physical Exam-Female n n n n Pelvic masses Uterosacral nodularity Abdominopelvic tenderness Uterine enlargement Thyroid exam Uterine mobility Cervical abnormalities

Ovarian factors n n n Fern test Endometrial biopsy in secretory phase Serial USG Serum progesterone Laparoscopy D & C.

Tubal factor Tubal patency test by: n n Tubal insufflation test Hystero-salphingo-graphy Laproscopy dye insufflation test Hydrotubation
Hormonal n n n n FSH LH Estrogen Progesterone TSH Prolactin Testosterone Immunological n Antisperm antibody
Treatment for female factor n n n Anovular : - clomiphene citrate bromocriptine D&C: - histopathology, bacteriology Reconstructive surgery: - developmental defect Surgery: - tubal block If all method fails, then go for….

Assisted Reproductive Technologies n n n Intrauterine Insemination(IUI) In Vitro Fertilization(IVF) IVF and Intra Cytoplasmic Injection of Sperms(ICSI)
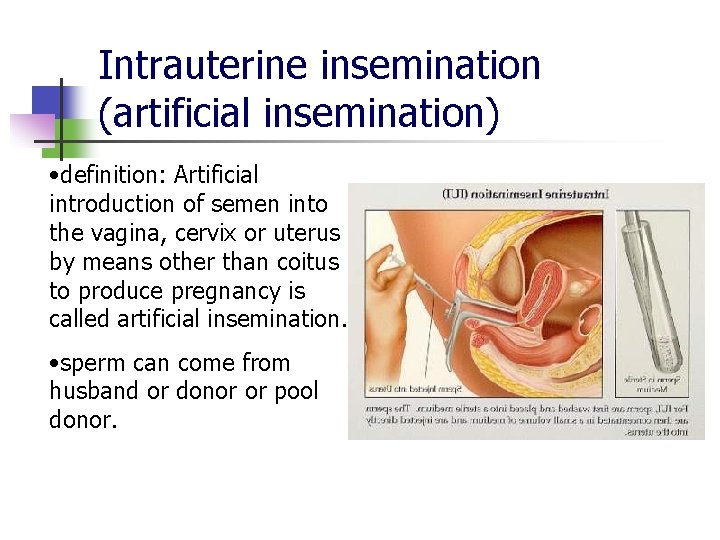
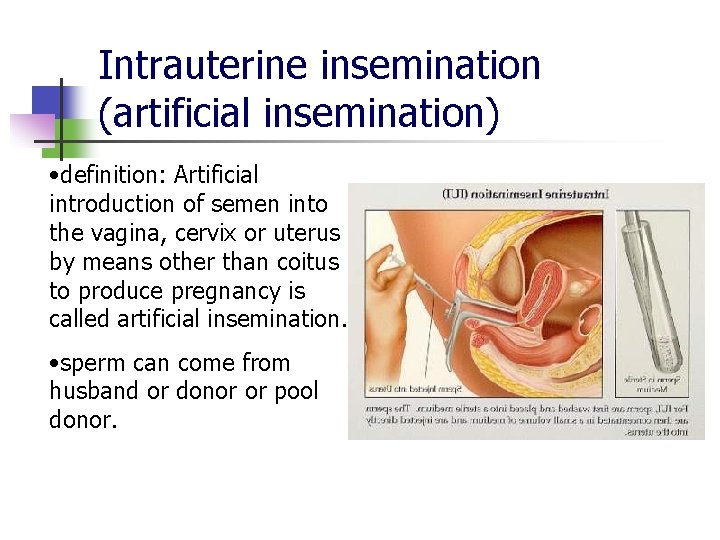
Intrauterine insemination (artificial insemination) • definition: Artificial introduction of semen into the vagina, cervix or uterus by means other than coitus to produce pregnancy is called artificial insemination. • sperm can come from husband or donor or pool donor.

IUI, cont’d. n 6000 babies / year born in US. as result of artificial insemination INDICATION OF ARTIFICIAL INSEMINATION: 1. 2. 3. 4. Impotent husband. Sterile husband. Husband suffering from hereditary disease. Rh-incompatibility between husband wife.

In vitro fertilization n test - tube babies” 1 st performed in 1978 (Louise Joy Brown) often performed on infertile women with tubal blockage
Test tube babies/ in-vitro fertilization Techniques: I. The ovum is removed from ovary through abdominal wall and is fertilized with the sperm in a small laboratory dish in artificial medium. . II. At the stage of blastocyst, the embryo is return to uterus through cervix. III. Blastocyst is implanted in endometrium.

Artificial insemination in laboratory disc Blastocyst
 Hijama points for male infertility
Hijama points for male infertility Cystic fibrosis male infertility
Cystic fibrosis male infertility Imotency
Imotency Cul de sacs meaning
Cul de sacs meaning Cupping therapy and infertility
Cupping therapy and infertility Female infertility
Female infertility Sherman j. silber
Sherman j. silber Male gaze définition
Male gaze définition Universal male suffrage definition
Universal male suffrage definition What is sterility
What is sterility Malegaze
Malegaze Male genital hygiene
Male genital hygiene Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Major endocrine glands male and female
Major endocrine glands male and female Chapter 16 matching questions 1-5
Chapter 16 matching questions 1-5 Female and male reproductive system
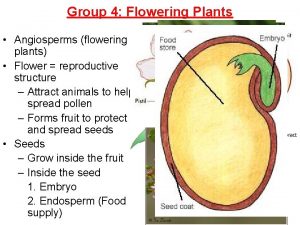
Female and male reproductive system Parts of female plant
Parts of female plant X-linked recessive punnett square
X-linked recessive punnett square Female and male parts of a flower
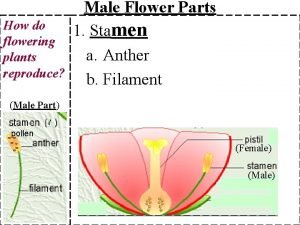
Female and male parts of a flower Produces pollen
Produces pollen Difference between male and female drosophila
Difference between male and female drosophila Difference between male and female skulls
Difference between male and female skulls Male and female skeleton differences
Male and female skeleton differences Male parts of flower
Male parts of flower Linea terminalis
Linea terminalis Androgen insensitivity
Androgen insensitivity Bone bonanza lab
Bone bonanza lab Difference between male and female sharks
Difference between male and female sharks All flowers photo
All flowers photo What do male ladybugs look like
What do male ladybugs look like Lesson 14.2 male and female urinary structures
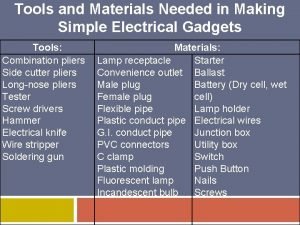
Lesson 14.2 male and female urinary structures Tools and materials in making simple electrical gadgets
Tools and materials in making simple electrical gadgets Differences between male and female reproductive organ
Differences between male and female reproductive organ Male and female tortoise
Male and female tortoise Male and female hormones
Male and female hormones Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Male and female hormones
Male and female hormones Codominance
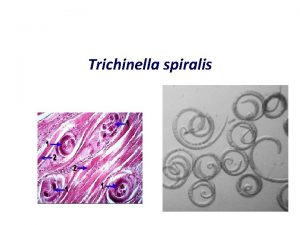
Codominance Trichinella
Trichinella Why is momentum p
Why is momentum p Filo nematelmintos
Filo nematelmintos Uterine orifice
Uterine orifice