Male Infertility Dr Firas Shakir 2019 2020 Definition


- Slides: 17
Male Infertility Dr. Firas Shakir 2019 -2020
Definition Failure of conception after at least 12 months of regular unprotected intercourse. Up to 50 % of infertility is due to male factors.
Pathophysiology Abnormalities of sperm morphology (teratospermia). Low sperm count (oligospermia). Abnormalities of sperm motility (asthenospermia). Absent sperms (azoospermia). Abnormal epididymal function.
Etiology Idiopathic. Varicocele. Cryptorchidism. Functional sperm disorders. Erectile or ejaculatory problems. Testicular injury. Endocrine disorders: Kallmann’s syndrome.
Etiology Hormone excess. Genetic disorders: Kleinfelter’s syndrome. Male genital tract obstruction. Systemic diseases. Drugs. Environmental factors. Infections.
Approach to infertile patients History : Examination: Investigations of male infertility :

Components of history Sexual and reproductive: Duration of problem; frequency and timing of intercourse; previous successful conception; birth control; erectile and ejaculatory disorders.
History Developmental: Age at puberty; history of cryptorchidism; gynaecomastia. Medical and surgical: Febrile illness ; orchitis; varicocele; testicular torsion; trauma or tumor; sexually transmitted diseases ; urinary tract infections; genitourinary and pelvic surgeries; radiotherapy; respiratory diseases; diabetes.
History Drug and environmental: Chemotherapy; nitrofurantoin; cimetidine; sulfasalazine; spironolactone; alpha blockers; exposure to heat; pesticides; dyes. Social: Ethanol, smoking/tobacco, cocaine, anabolic steroids. Family: Hypogonadism; cryptorchidism.
Physical Examination Full assessment of all systems. Signs of hypogonadism; secondary sexual development, gynaecomastia. Urogenital examination: examination of penis and testes; palpation of epididymis and vas deferense ; varicocele.
Investigations Semen analysis: 2 - 3 specimens are collected over several weeks collected after 2 -7 days of sexual abstinence. Deliver specimen to lab. within one hour.
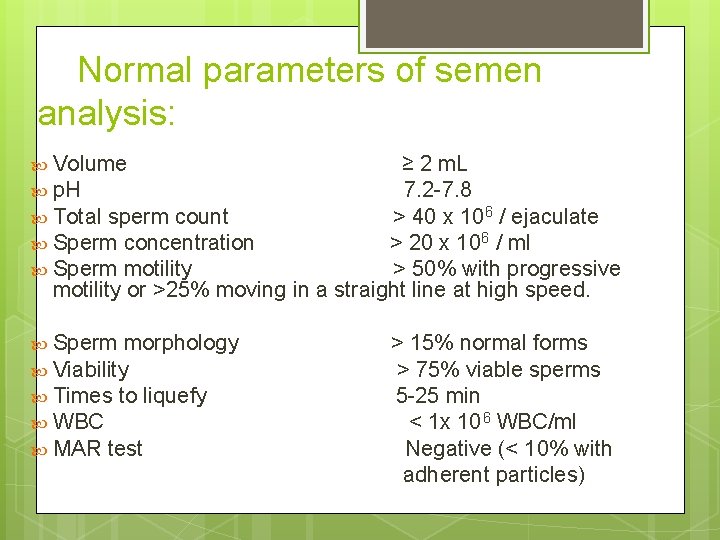
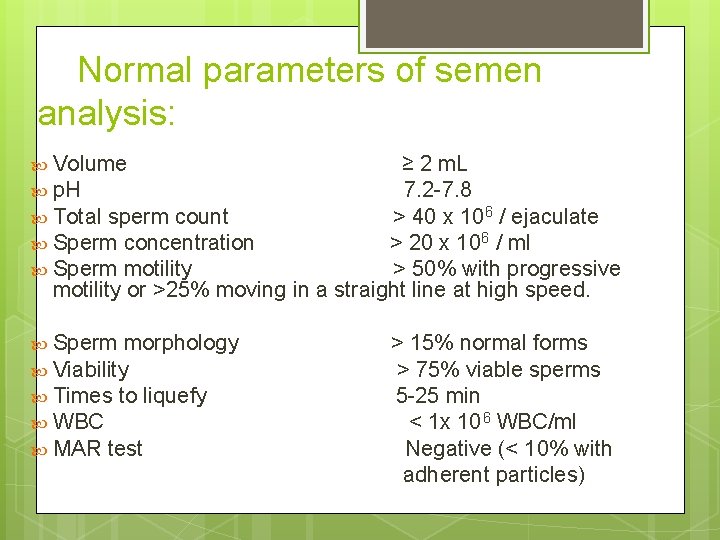
Normal parameters of semen analysis: Volume ≥ 2 m. L p. H 7. 2 -7. 8 Total sperm count > 40 x 10 6 / ejaculate Sperm concentration > 20 x 106 / ml Sperm motility > 50% with progressive motility or >25% moving in a straight line at high speed. Sperm morphology Viability Times to liquefy WBC MAR test > 15% normal forms > 75% viable sperms 5 -25 min < 1 x 10 6 WBC/ml Negative (< 10% with adherent particles)
Investigations Hormone analysis: Assessment of serum levels of FSH; LH; testosterone and prolactin. Testicular biopsy: In case of azoospermia to differentiate between obstructive and non obstructive type.
Investigations Imaging tests: 1. Scrotal ultrasound: to confirm a varicocele; and assess testicular abnormalities. 2. Transrectal ultrasound: to assess seminal vesicles and ejaculatory ducts. 3. Vasography : to visualize the vas deference for obstruction.
Options for male infertility Treatment General : modify life style and avoid risk factors. Medical treatment : 1. Antibiotics 2. Hormonal : h. CG 2000 IU sc 3 x a week. FSH Clomiphene citrate 25 mg. Hyperprolactinaemia is treated with dopamine agonists. 3. Antioxidants: vit. E , zinc , folic acid.
Surgical treatment Genital tract obstruction. By microsurgical reanastomosis. Varicocele repair.

Assisted reproductive techniques Sperm extraction from the testes and subsequent assisted conception by: Intrauterine insemination (IUI). In vitro fertilization (IVF). Gamete intrafallopian transfer (GIFT). Intracytoplasmic sperm injection (ICSI).
 Hijama points
Hijama points Cystic fibrosis male infertility
Cystic fibrosis male infertility Menses
Menses Dr firas obeidat
Dr firas obeidat Facs
Facs Firas 14/3
Firas 14/3 Adaptive cruise control
Adaptive cruise control Hijama for infertility
Hijama for infertility Female infertility
Female infertility Sherman j. silber
Sherman j. silber Dr mustafa shakir
Dr mustafa shakir Mustafa shakir contacts
Mustafa shakir contacts Dr mustafa shakir
Dr mustafa shakir Prof. dr. abdul sattar shakir
Prof. dr. abdul sattar shakir Syra shakir
Syra shakir Dr mustafa shakir
Dr mustafa shakir Dr mustafa shakir
Dr mustafa shakir Programmazione religione scuola infanzia 2019-2020
Programmazione religione scuola infanzia 2019-2020