KUWAIT UNIVERSITY FACULTY OF MEDICINE DEPARTMENT OF ANATOMY


- Slides: 47
KUWAIT UNIVERSITY FACULTY OF MEDICINE DEPARTMENT OF ANATOMY 210 -Anatomy T. Chacko Mathew, M. Sc. Ph. D. , FRCPath (UK)
The Vertebral Column
OBJECTIVES: • At the end of the lecture the students should be able to describe • The structure and functions of the vertebral column (regions, number of vertebrae in each region) • The primary and secondary curves of the vertebral column • Structure of a typical vertebra • Structure of atypical vertebrae • Zygapophyseal joint, atlanto-occipital joint and atlanto-axial joint • Structure and function of the inter-vertebral disc • Common injuries and deformities of the vertebral column
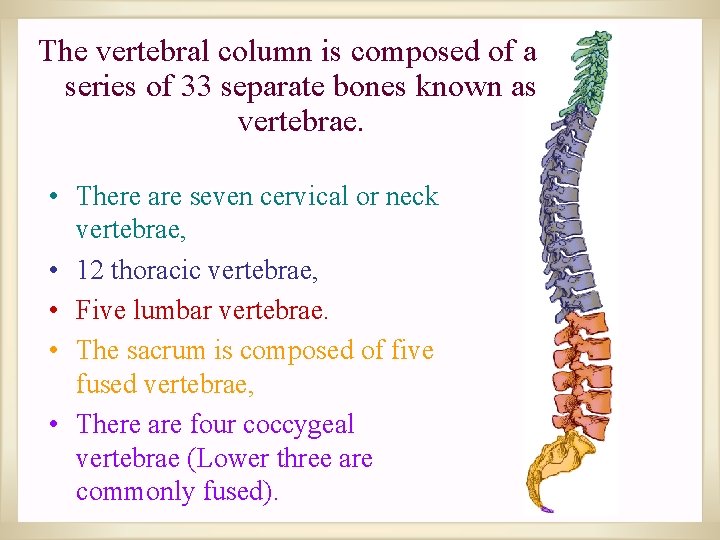
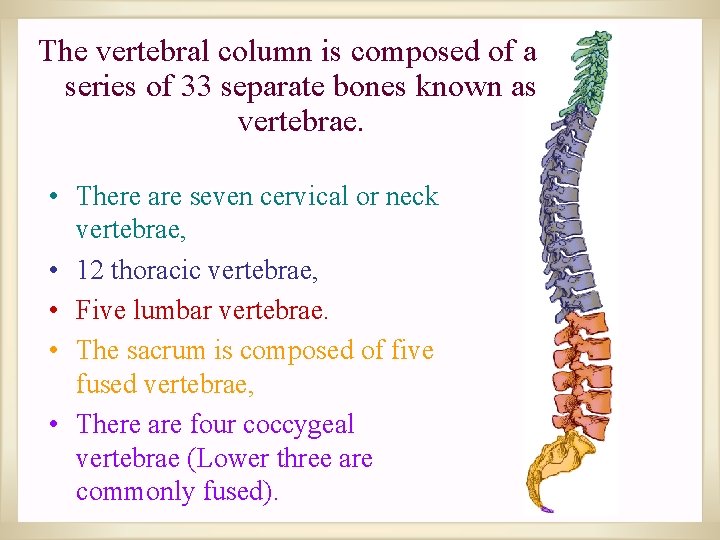
The vertebral column is composed of a series of 33 separate bones known as vertebrae. • There are seven cervical or neck vertebrae, • 12 thoracic vertebrae, • Five lumbar vertebrae. • The sacrum is composed of five fused vertebrae, • There are four coccygeal vertebrae (Lower three are commonly fused).
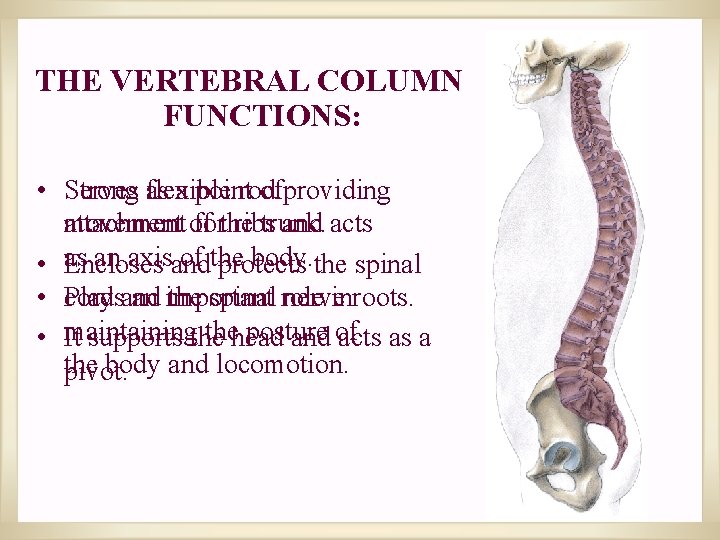
THE VERTEBRAL COLUMN FUNCTIONS: • Strong Serves as flexible a point rod ofproviding movement of attachment forthe ribs trunk. and acts an axisand of the body. the spinal • as Encloses protects • Plays cord an important the spinal role nerveinroots. thehead posture • maintaining It supports the and of acts as a the body and locomotion. pivot.
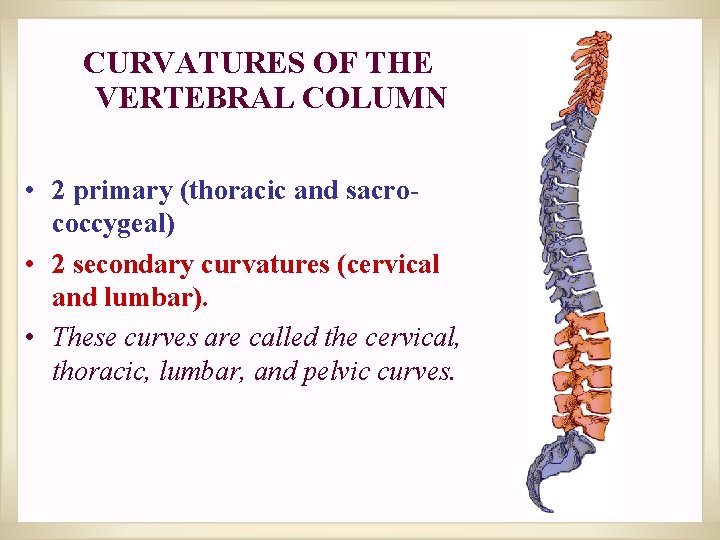
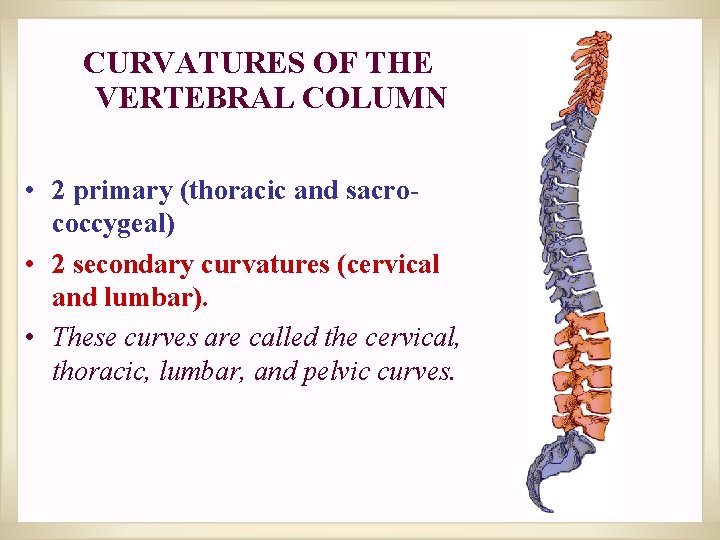
CURVATURES OF THE VERTEBRAL COLUMN • 2 primary (thoracic and sacrococcygeal) • 2 secondary curvatures (cervical and lumbar). • These curves are called the cervical, thoracic, lumbar, and pelvic curves.
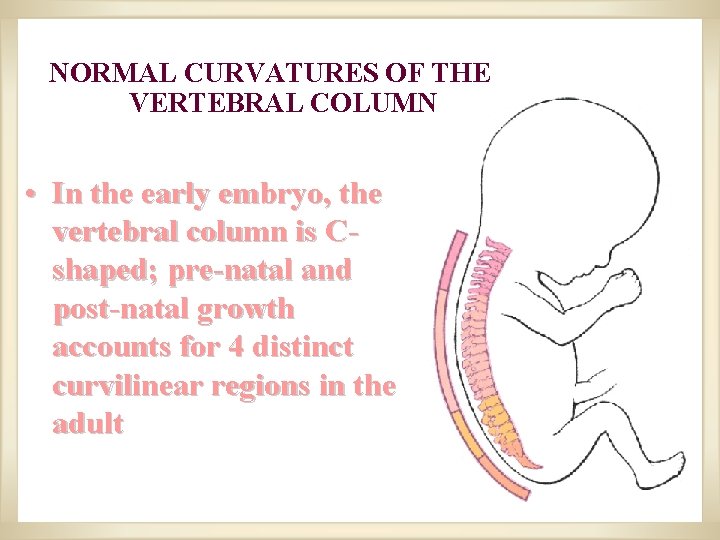
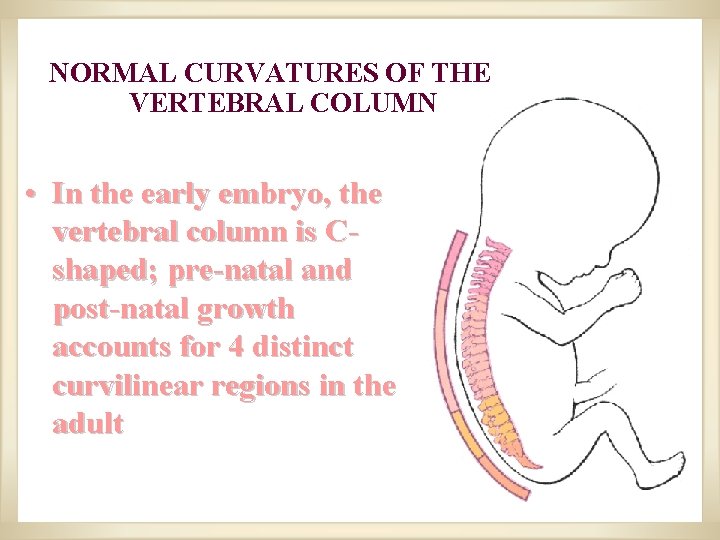
NORMAL CURVATURES OF THE VERTEBRAL COLUMN • In the early embryo, the vertebral column is Cshaped; pre-natal and post-natal growth accounts for 4 distinct curvilinear regions in the adult
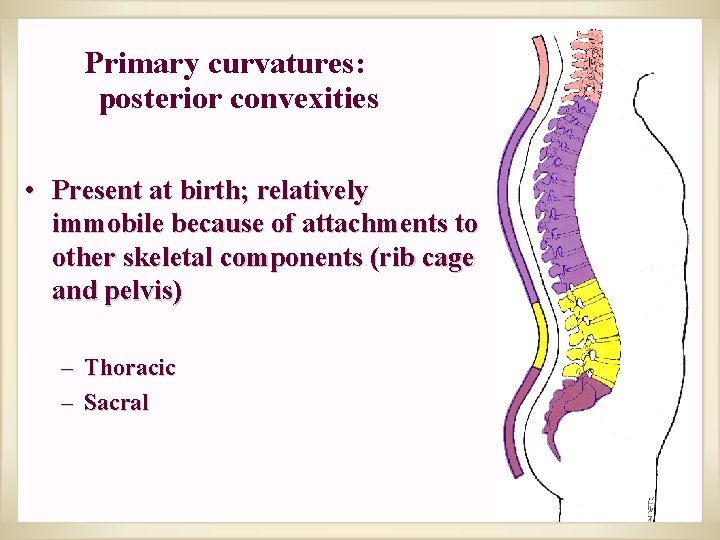
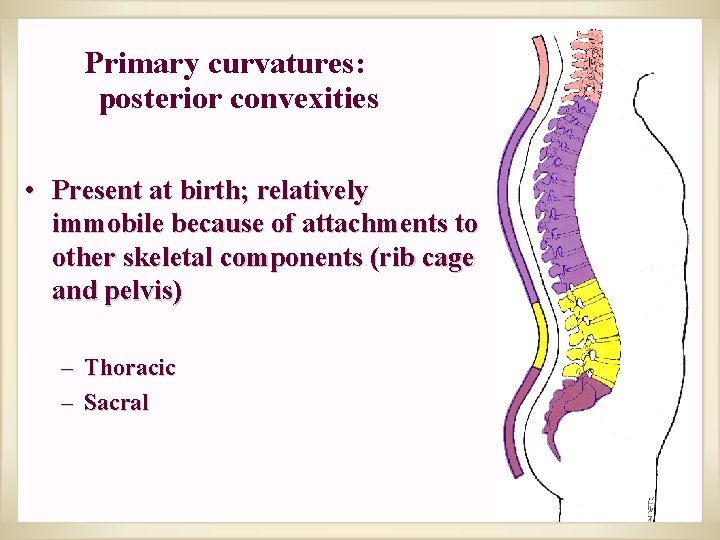
Primary curvatures: posterior convexities • Present at birth; relatively immobile because of attachments to other skeletal components (rib cage and pelvis) – Thoracic – Sacral
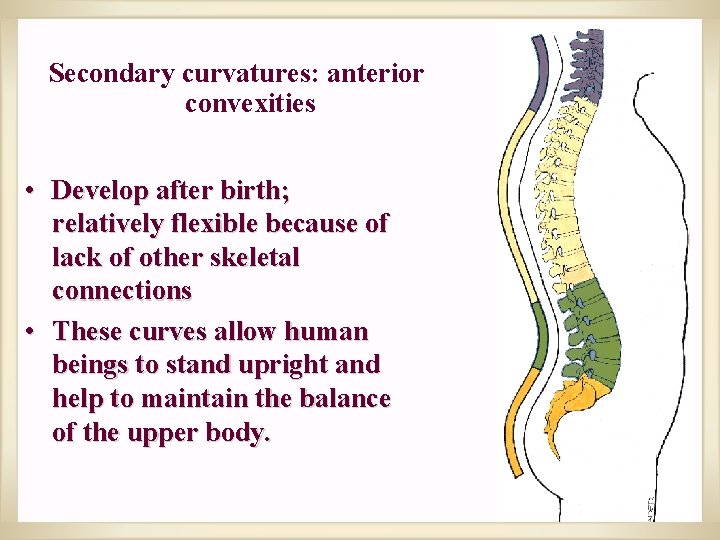
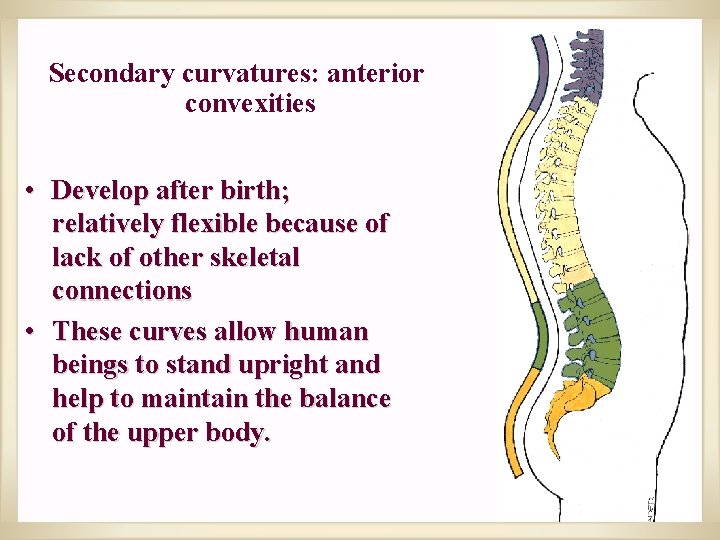
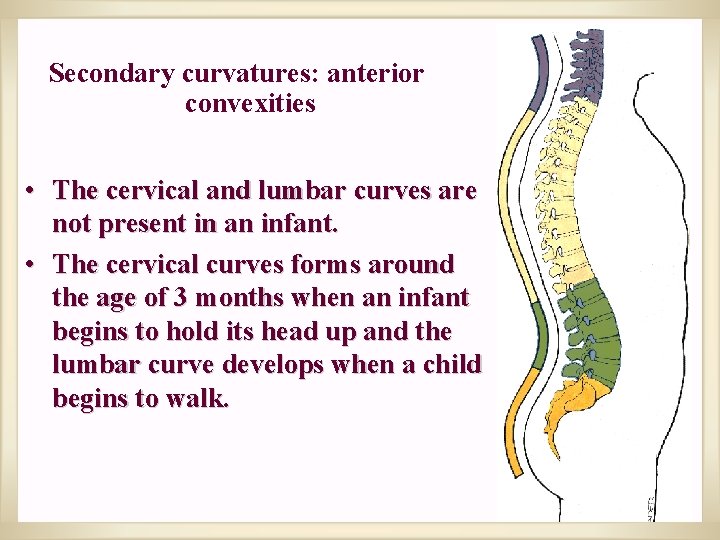
Secondary curvatures: anterior convexities • Develop after birth; relatively flexible because of lack of other skeletal connections • These curves allow human beings to stand upright and help to maintain the balance of the upper body.
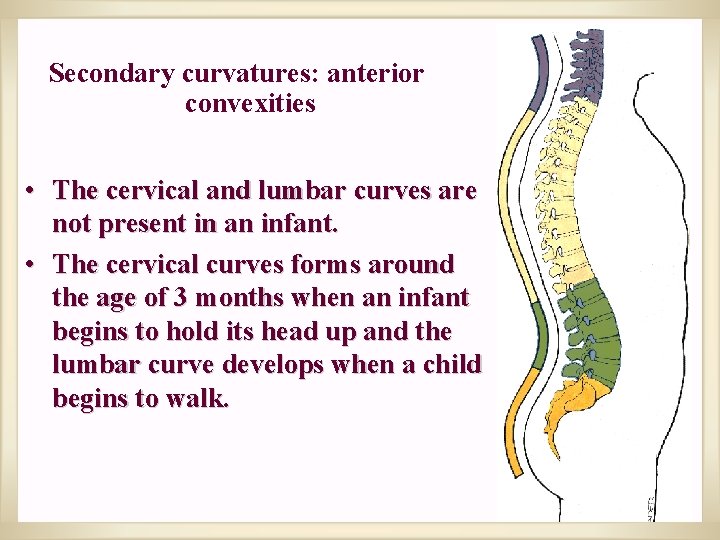
Secondary curvatures: anterior convexities • The cervical and lumbar curves are not present in an infant. • The cervical curves forms around the age of 3 months when an infant begins to hold its head up and the lumbar curve develops when a child begins to walk.
ABNORMAL CURVATURES OF THE VERTEBRAL COLUMN
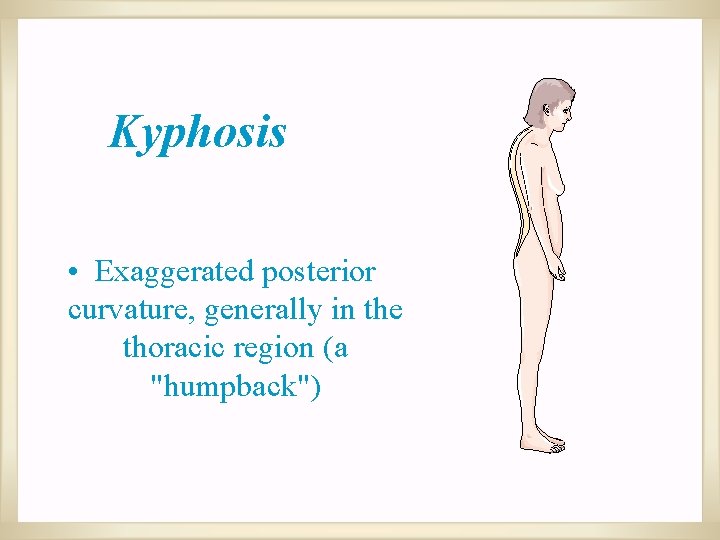
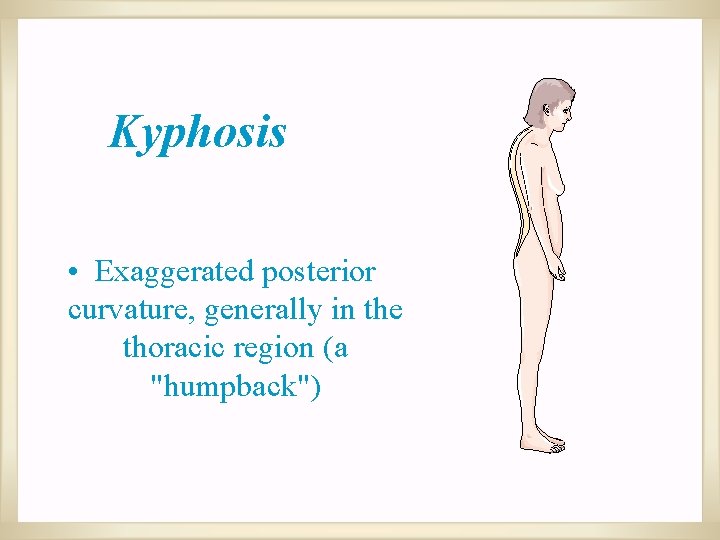
Kyphosis • Exaggerated posterior curvature, generally in the thoracic region (a "humpback")
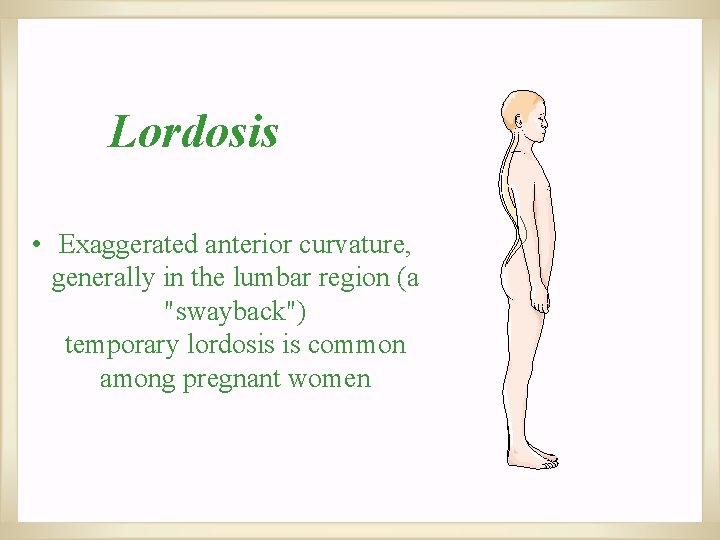
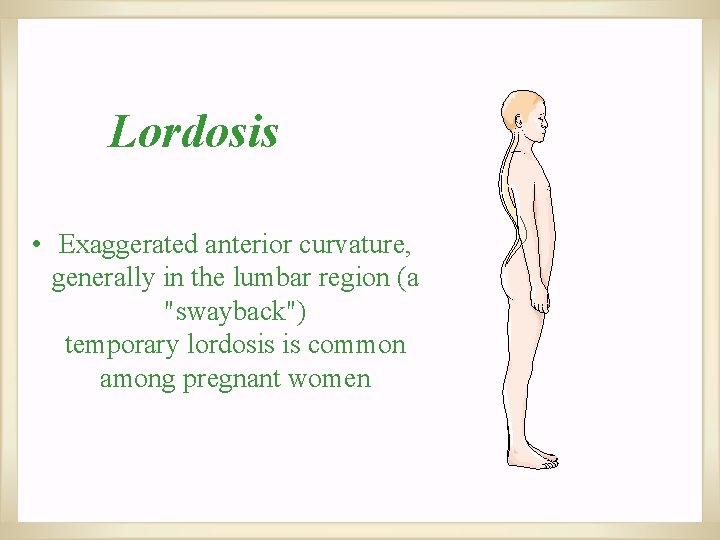
Lordosis • Exaggerated anterior curvature, generally in the lumbar region (a "swayback") temporary lordosis is common among pregnant women
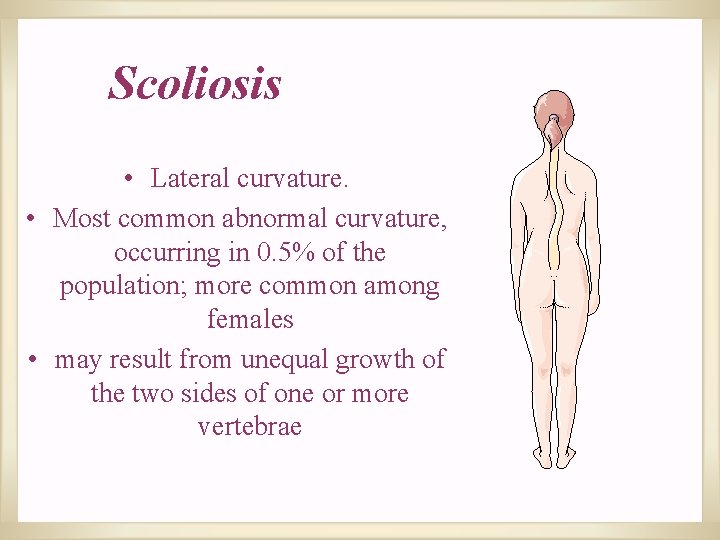
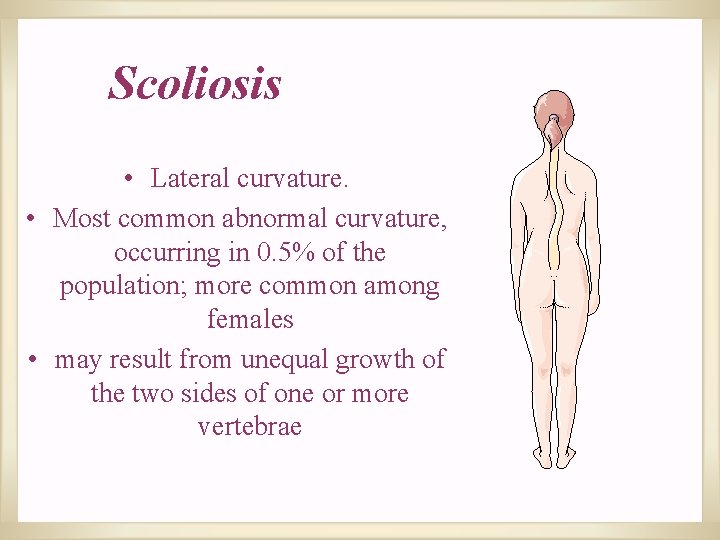
Scoliosis • Lateral curvature. • Most common abnormal curvature, occurring in 0. 5% of the population; more common among females • may result from unequal growth of the two sides of one or more vertebrae
Structure of a typical vertebra
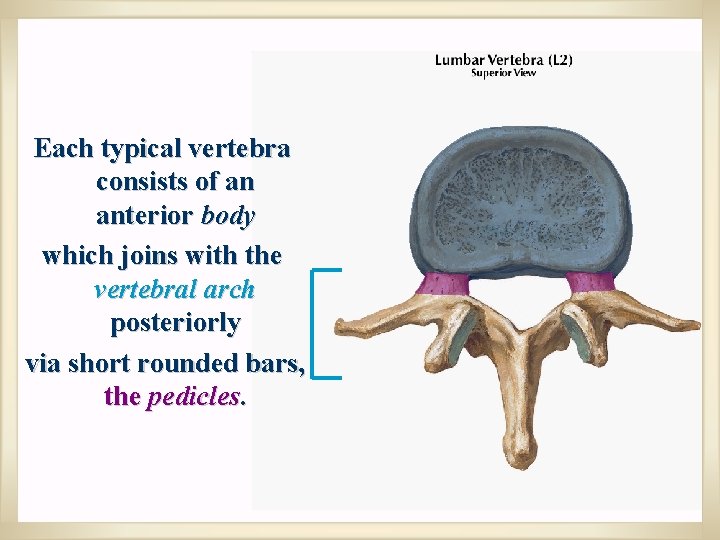
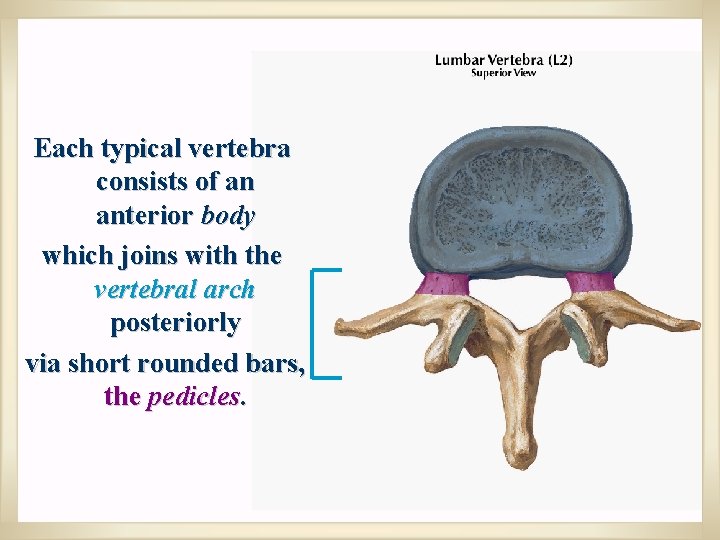
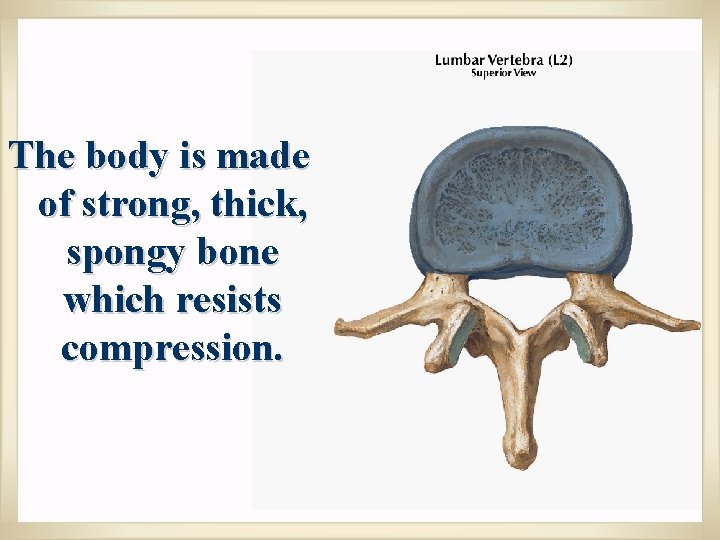
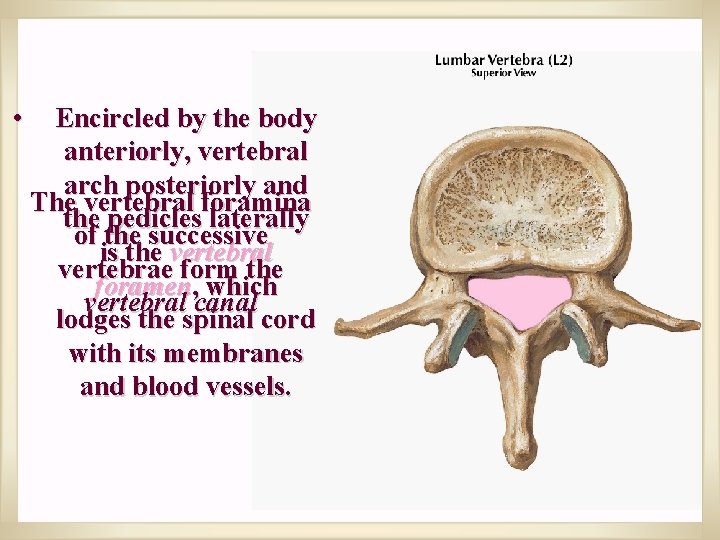
Each typical vertebra consists of an anterior body which joins with the vertebral arch posteriorly via short rounded bars, the pedicles.
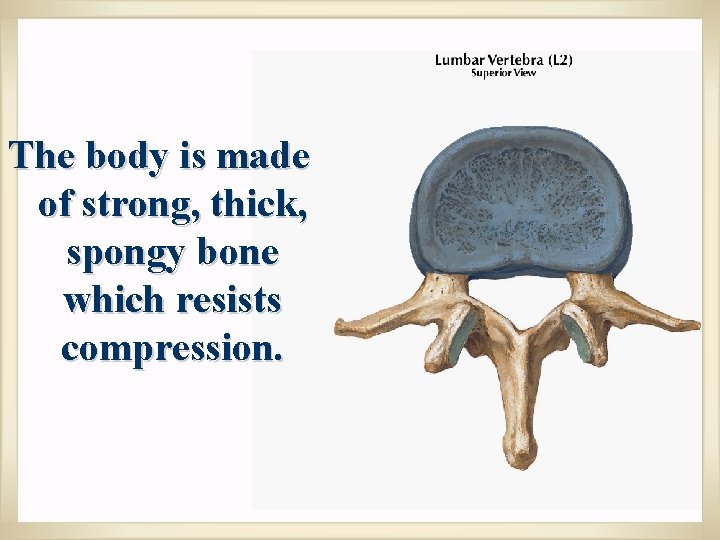
The body is made of strong, thick, spongy bone which resists compression.
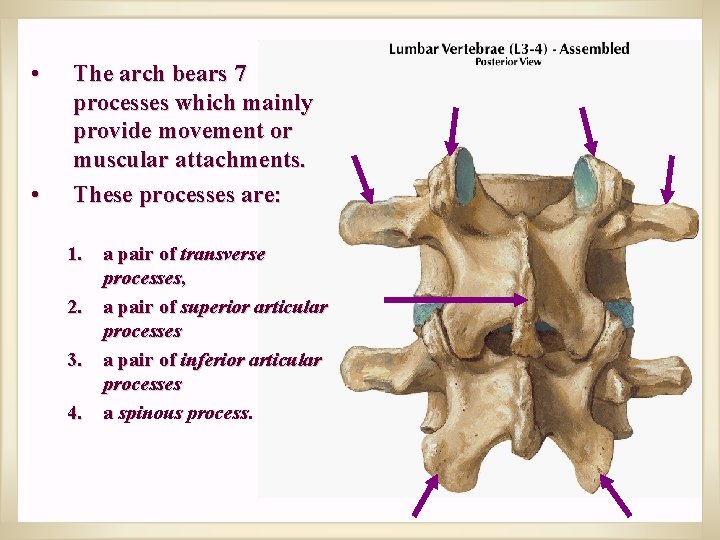
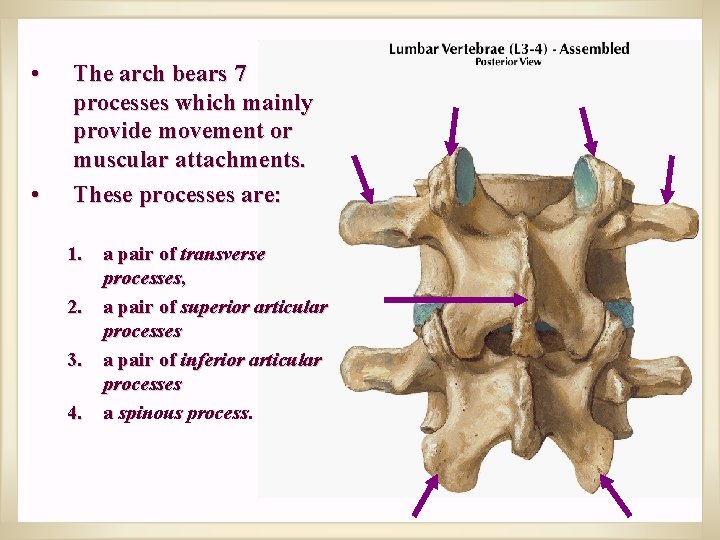
• • The arch bears 7 processes which mainly provide movement or muscular attachments. These processes are: 1. a pair of transverse processes, 2. a pair of superior articular processes 3. a pair of inferior articular processes 4. a spinous process.
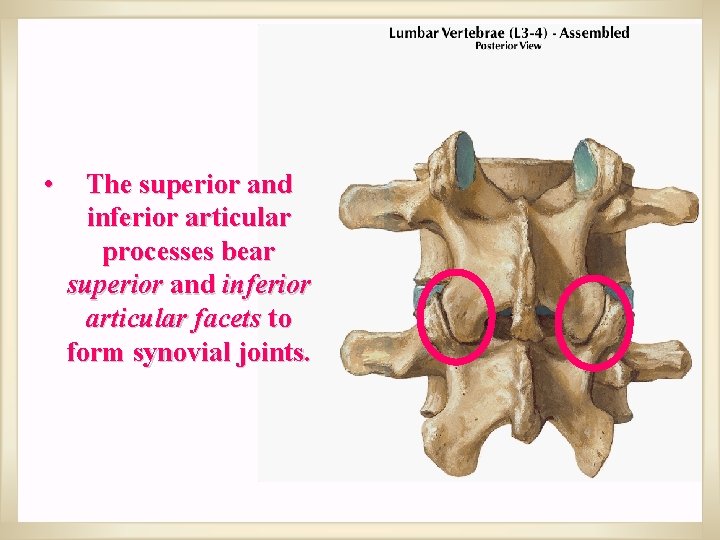
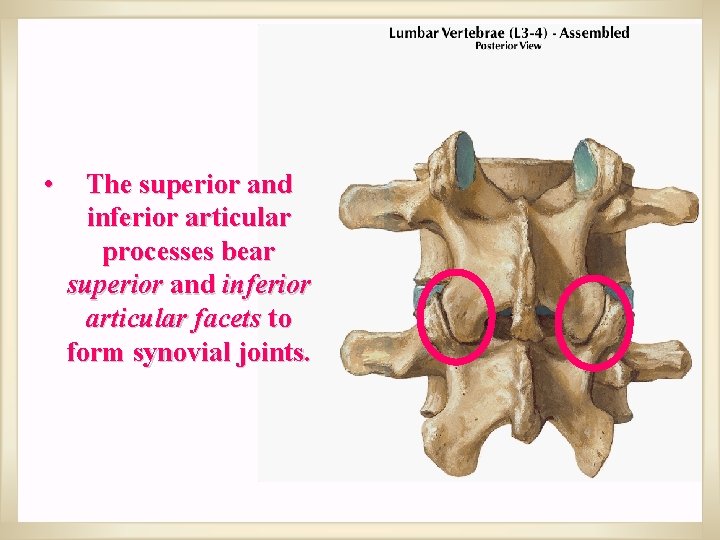
• The superior and inferior articular processes bear superior and inferior articular facets to form synovial joints.
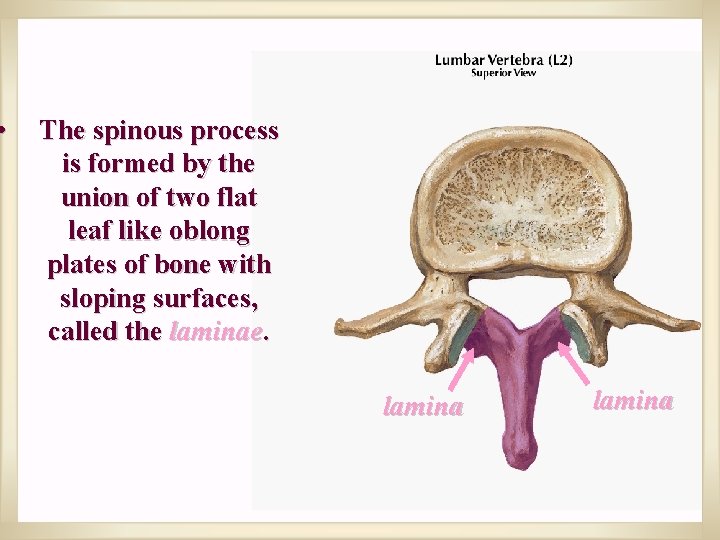
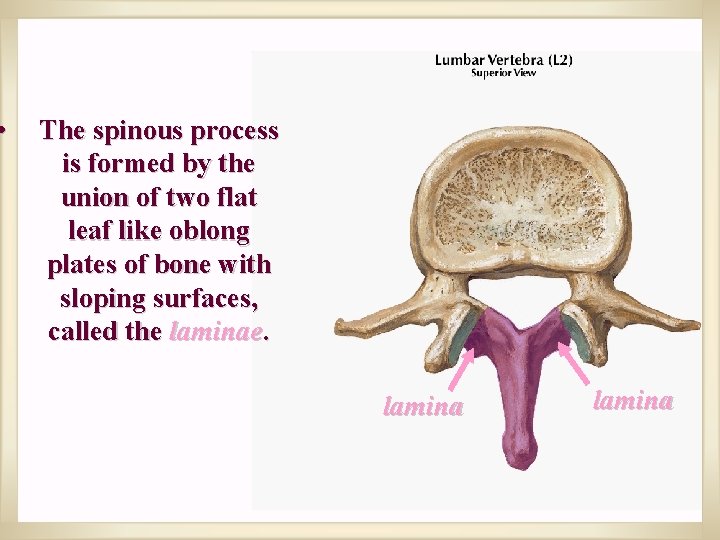
• The spinous process is formed by the union of two flat leaf like oblong plates of bone with sloping surfaces, called the laminae. lamina
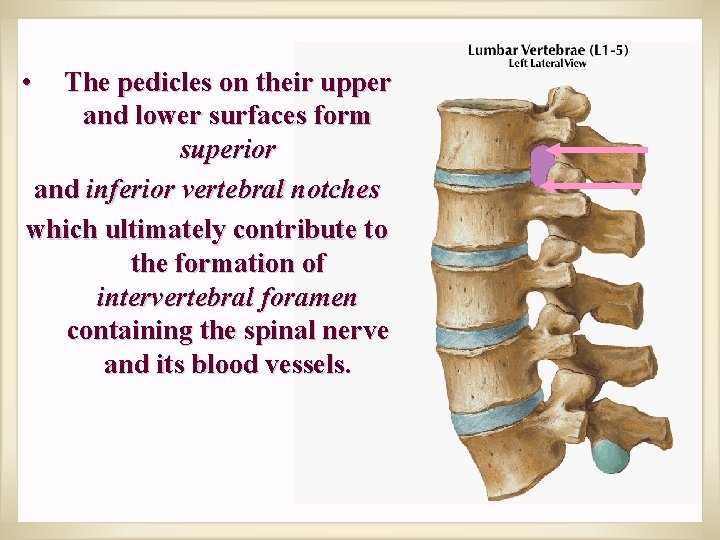
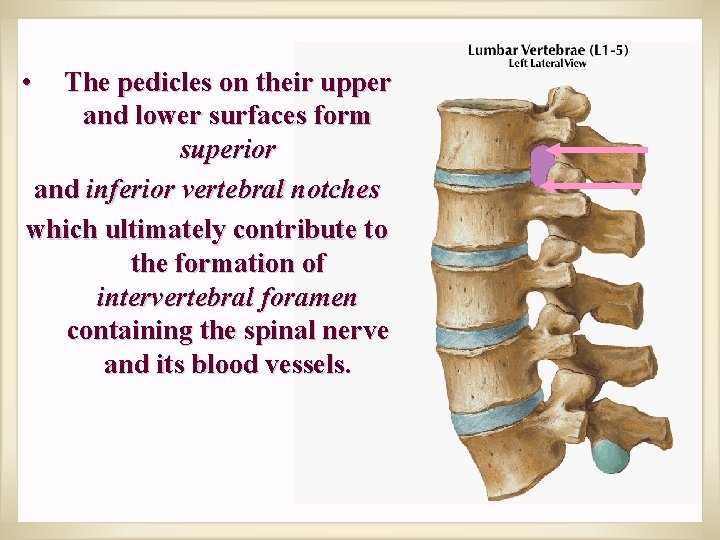
• The pedicles on their upper and lower surfaces form superior and inferior vertebral notches which ultimately contribute to the formation of intervertebral foramen containing the spinal nerve and its blood vessels.
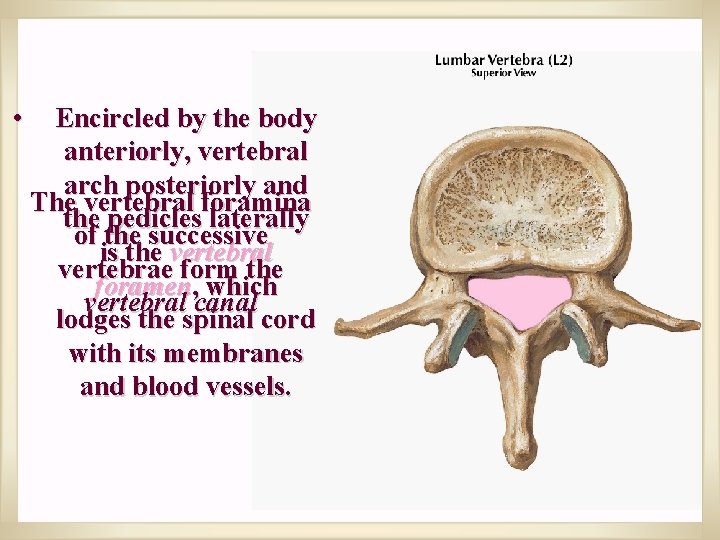
• Encircled by the body anteriorly, vertebral arch posteriorly and The vertebral foramina the pedicles laterally of the successive is the vertebral vertebrae form the foramen, which vertebral canal lodges the spinal cord with its membranes and blood vessels.

ATYPICAL VERTEBRAE
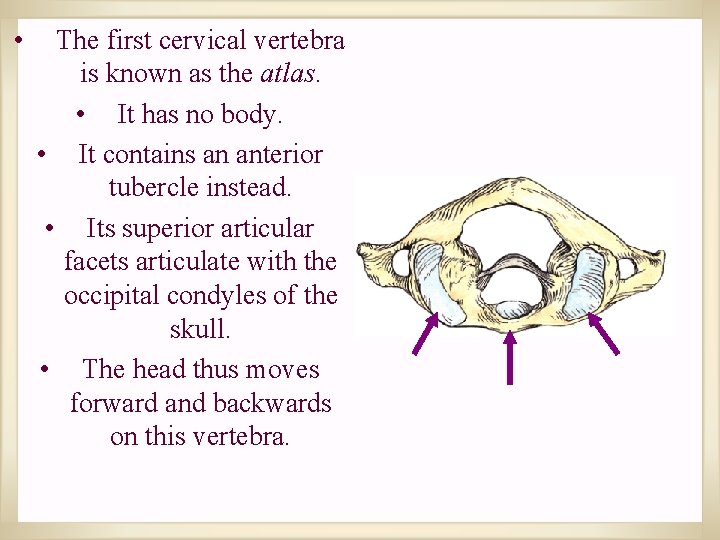
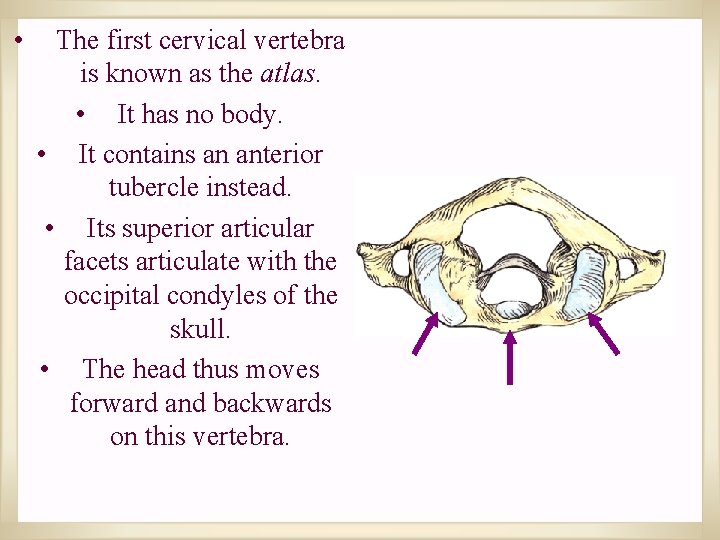
• The first cervical vertebra is known as the atlas. • It has no body. • It contains an anterior tubercle instead. • Its superior articular facets articulate with the occipital condyles of the skull. • The head thus moves forward and backwards on this vertebra.
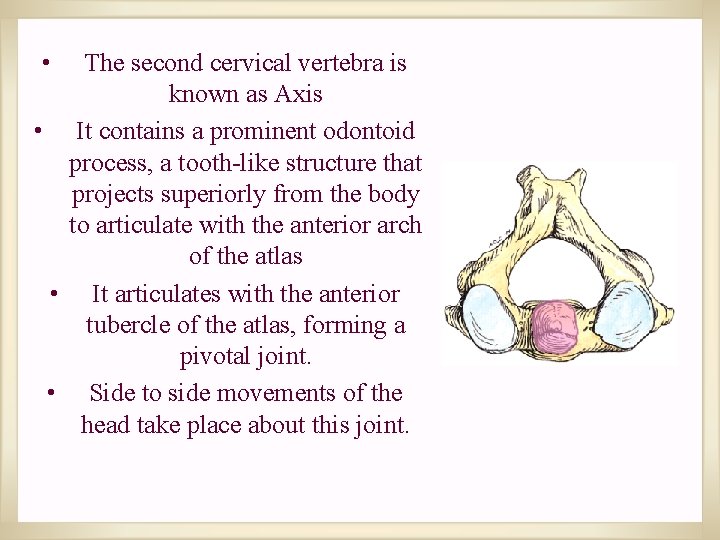
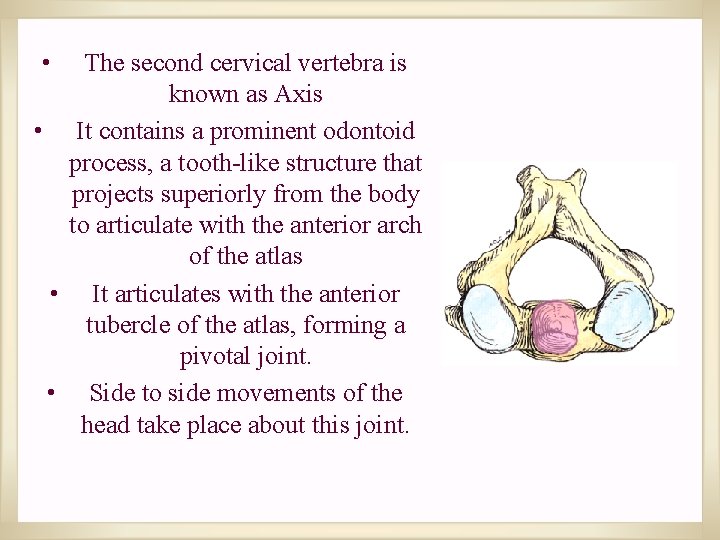
• The second cervical vertebra is known as Axis • It contains a prominent odontoid process, a tooth-like structure that projects superiorly from the body to articulate with the anterior arch of the atlas • It articulates with the anterior tubercle of the atlas, forming a pivotal joint. • Side to side movements of the head take place about this joint.
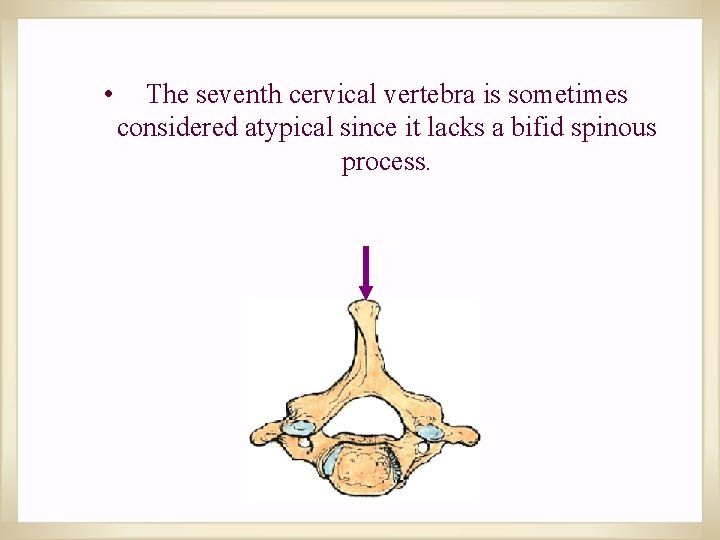
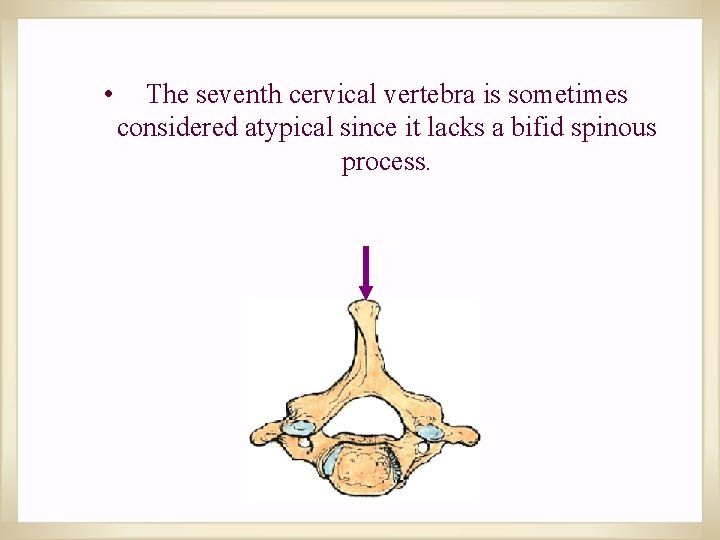
• The seventh cervical vertebra is sometimes considered atypical since it lacks a bifid spinous process.
VERTEBRAL PROCESSES 7 IN NUMBER ON TYPICAL VERTEBRAE
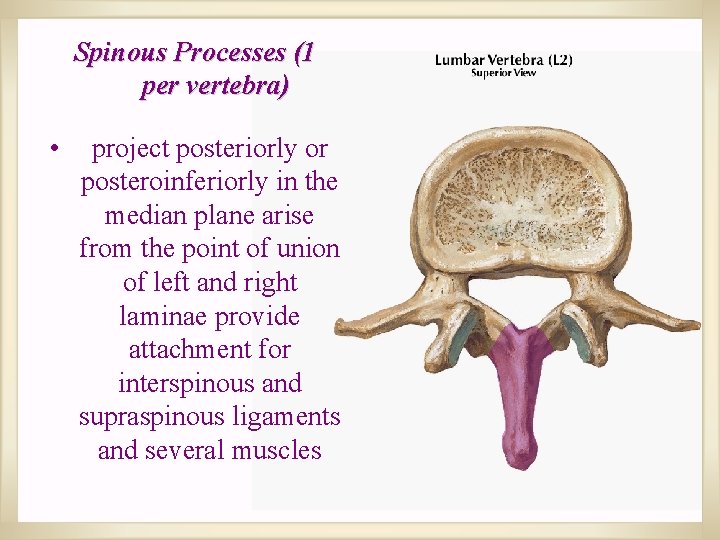
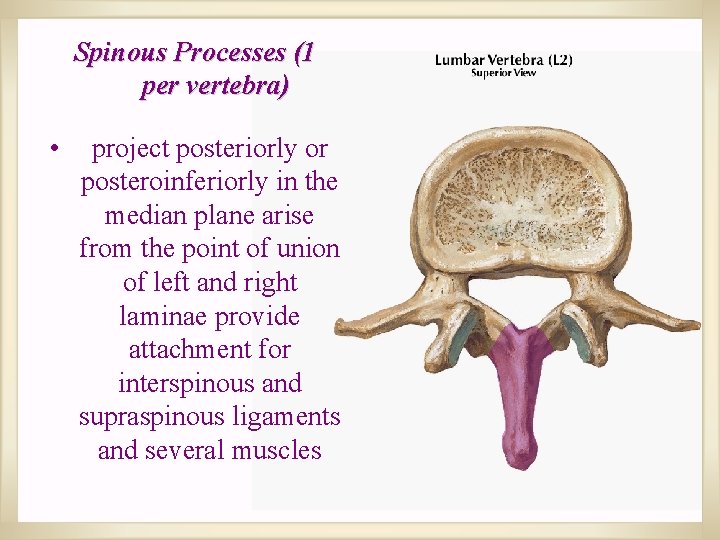
Spinous Processes (1 per vertebra) • project posteriorly or posteroinferiorly in the median plane arise from the point of union of left and right laminae provide attachment for interspinous and supraspinous ligaments and several muscles
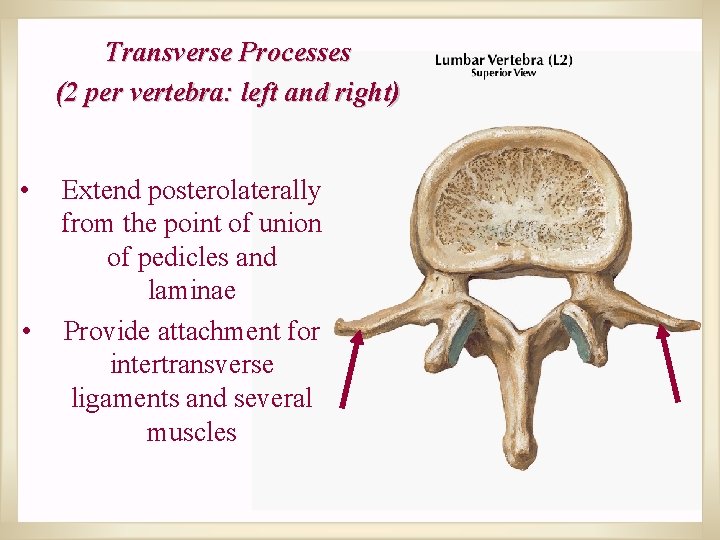
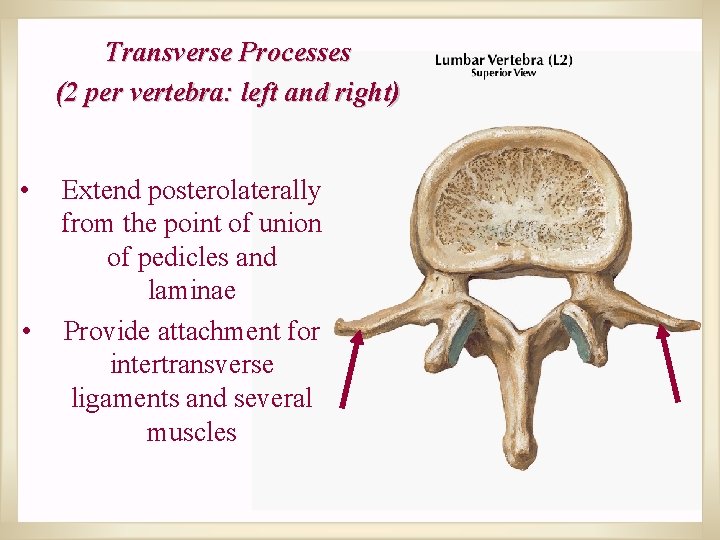
Transverse Processes (2 per vertebra: left and right) • • Extend posterolaterally from the point of union of pedicles and laminae Provide attachment for intertransverse ligaments and several muscles
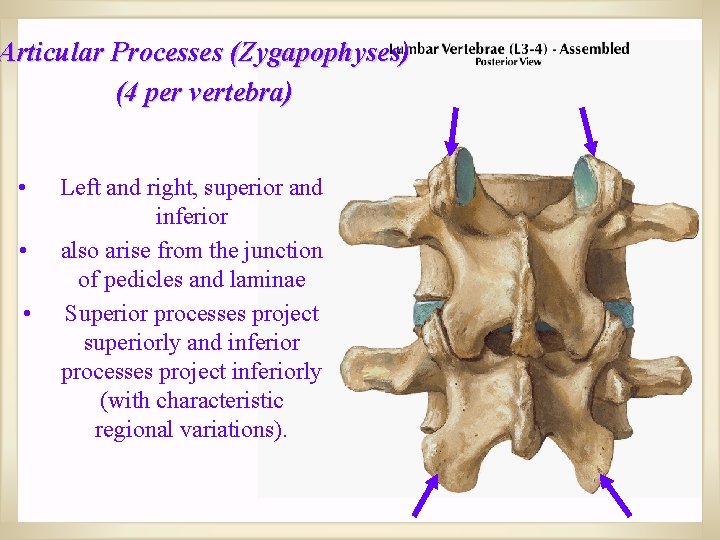
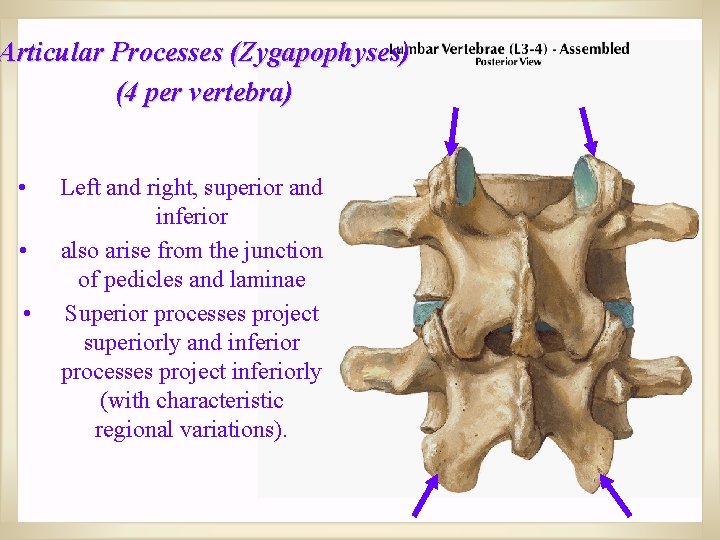
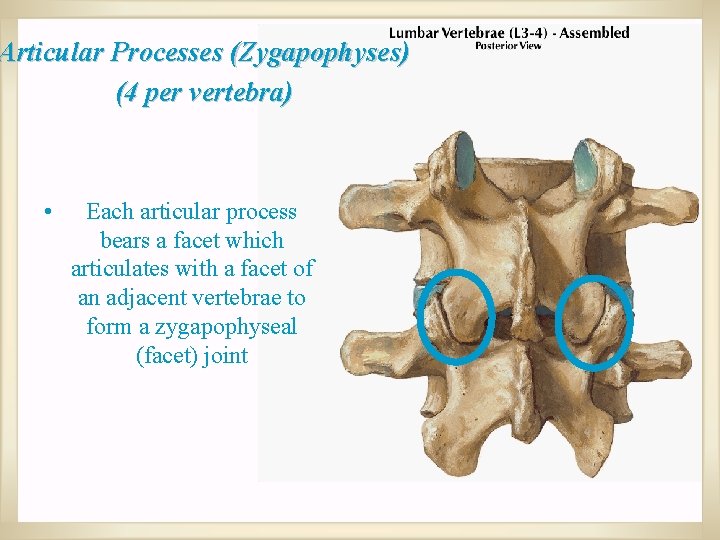
Articular Processes (Zygapophyses) (4 per vertebra) • • • Left and right, superior and inferior also arise from the junction of pedicles and laminae Superior processes project superiorly and inferior processes project inferiorly (with characteristic regional variations).
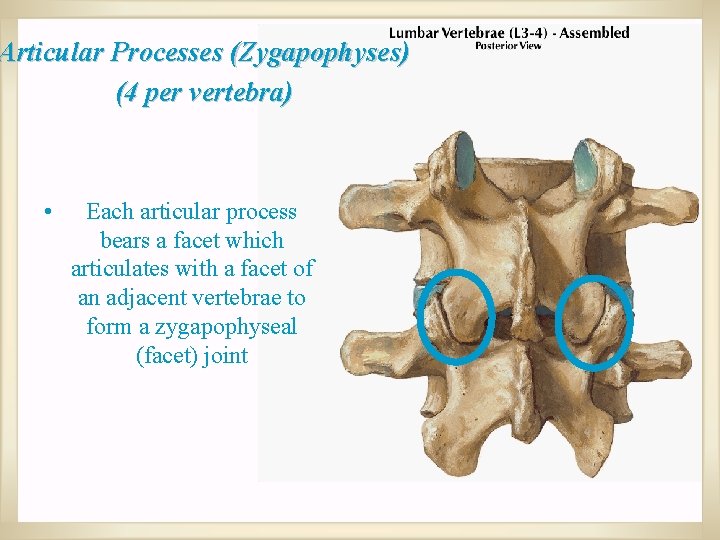
Articular Processes (Zygapophyses) (4 per vertebra) • Each articular process bears a facet which articulates with a facet of an adjacent vertebrae to form a zygapophyseal (facet) joint
JOINTS
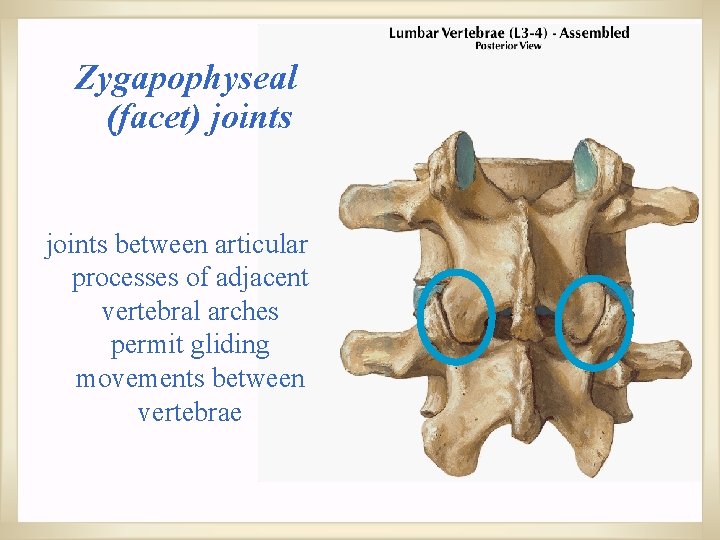
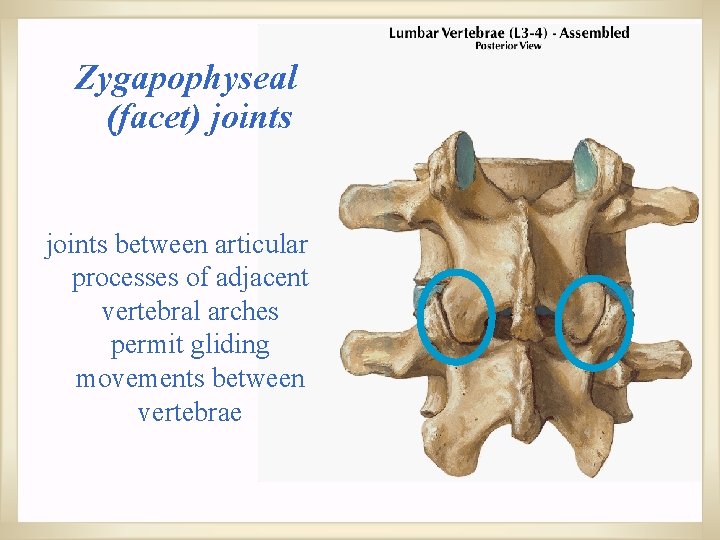
Zygapophyseal (facet) joints between articular processes of adjacent vertebral arches permit gliding movements between vertebrae
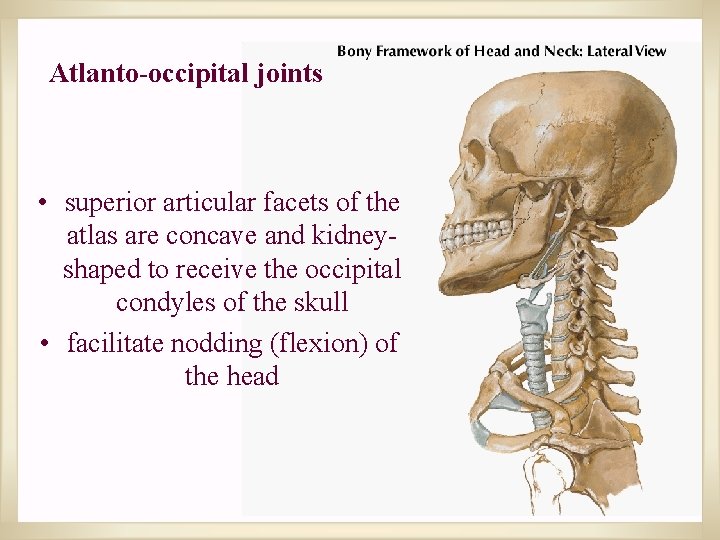
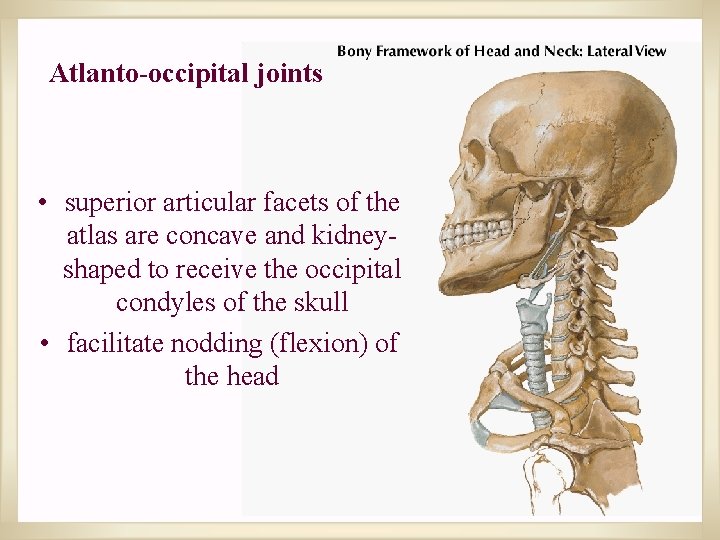
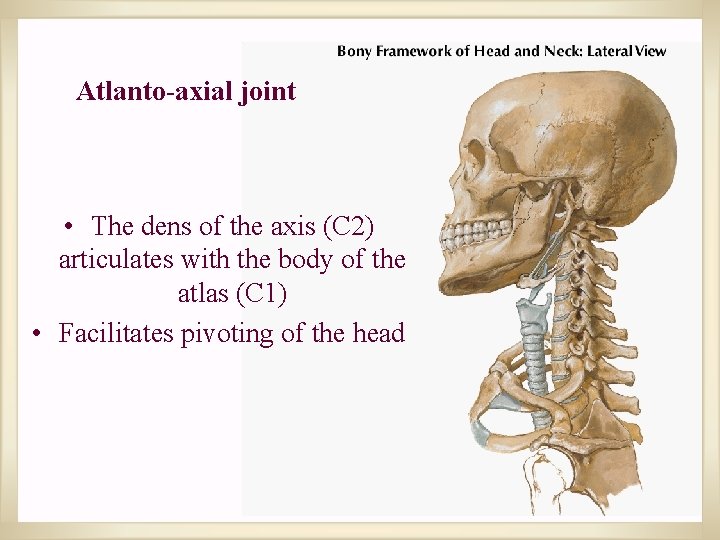
Atlanto-occipital joints • superior articular facets of the atlas are concave and kidneyshaped to receive the occipital condyles of the skull • facilitate nodding (flexion) of the head
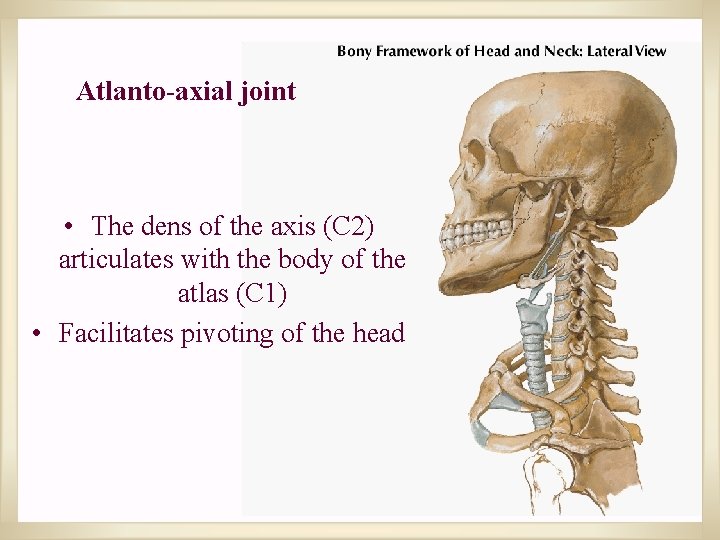
Atlanto-axial joint • The dens of the axis (C 2) articulates with the body of the atlas (C 1) • Facilitates pivoting of the head

INTER-VERTEBRAL DISC
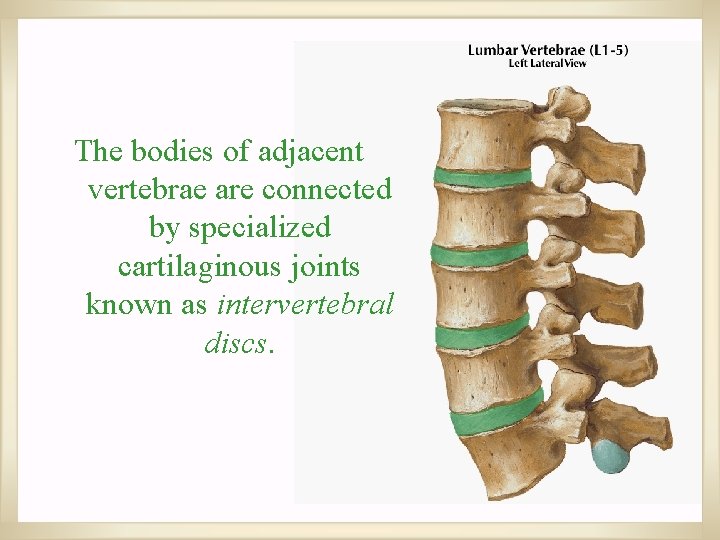
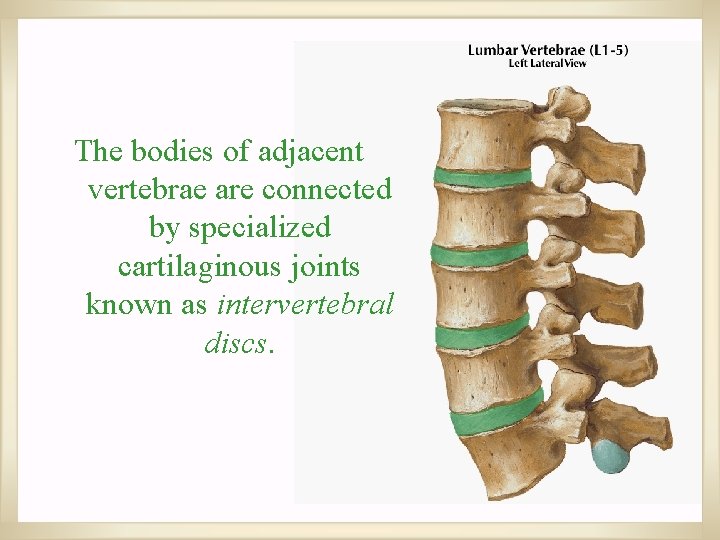
The bodies of adjacent vertebrae are connected by specialized cartilaginous joints known as intervertebral discs.
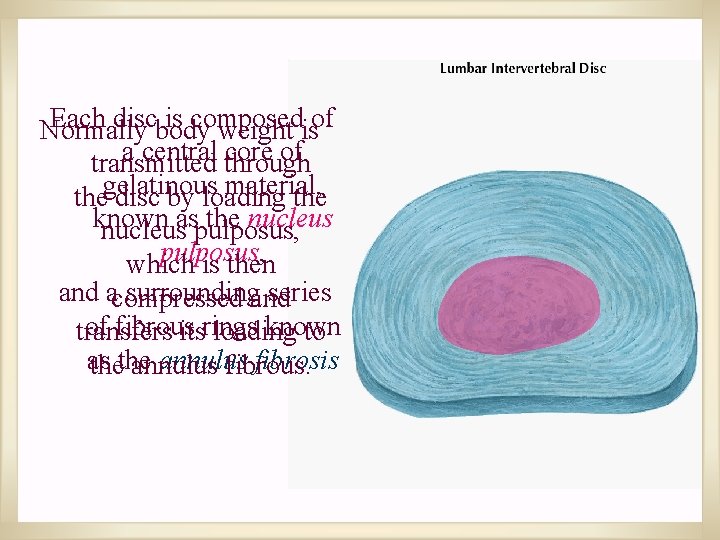
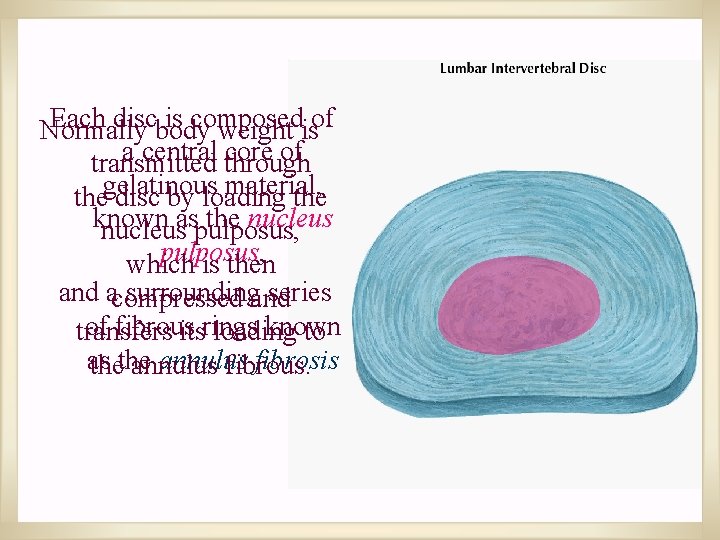
Each discbody is composed Normally weight isof a central through core of transmitted material, thegelatinous disc by loading the known the nucleusaspulposus, which is then and acompressed surroundingand series of fibrous known transfers itsrings loading to as annulus fibrosis thethe annulus fibrous.
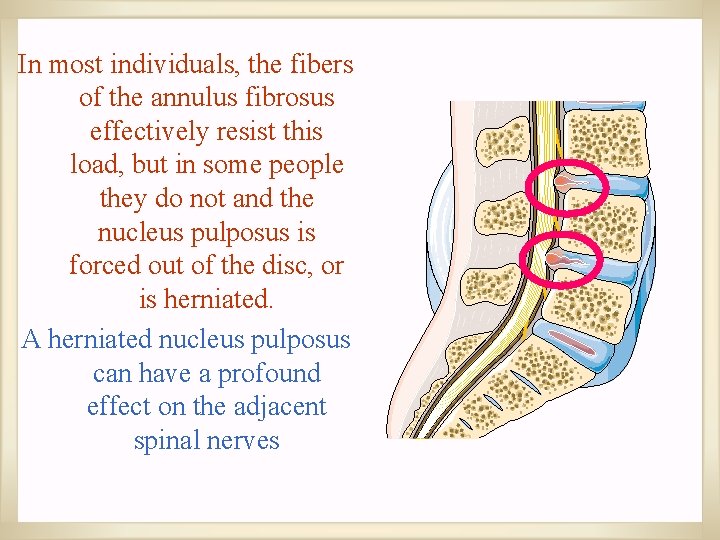
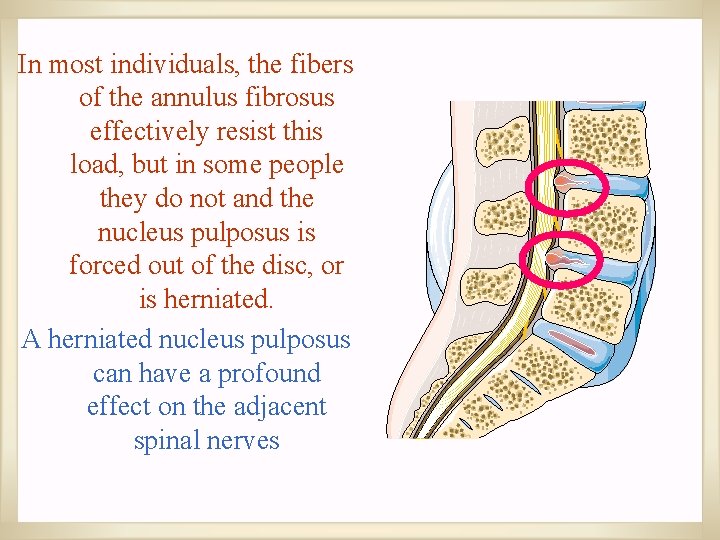
In most individuals, the fibers of the annulus fibrosus effectively resist this load, but in some people they do not and the nucleus pulposus is forced out of the disc, or is herniated. A herniated nucleus pulposus can have a profound effect on the adjacent spinal nerves
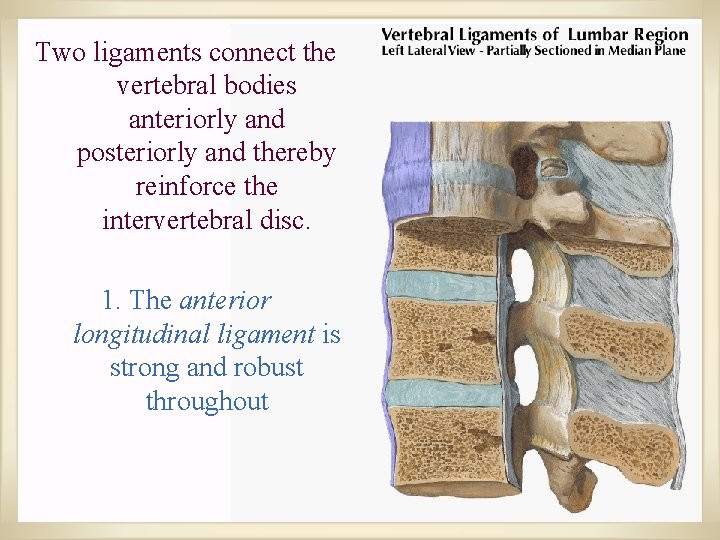
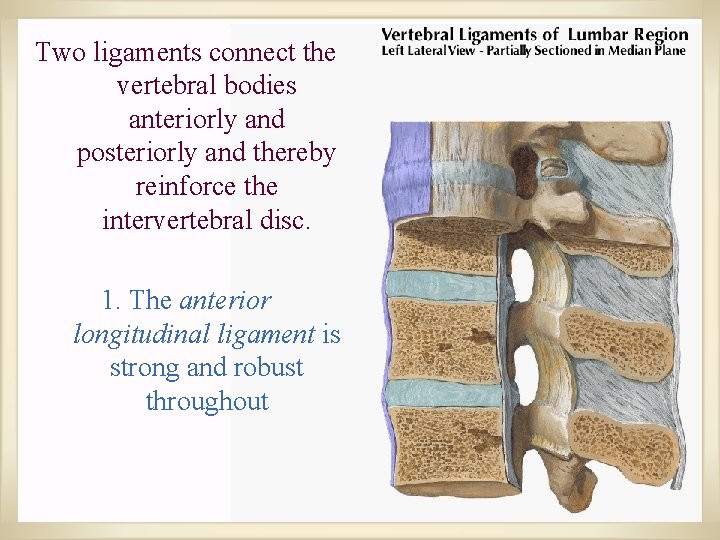
Two ligaments connect the vertebral bodies anteriorly and posteriorly and thereby reinforce the intervertebral disc. 1. The anterior longitudinal ligament is strong and robust throughout
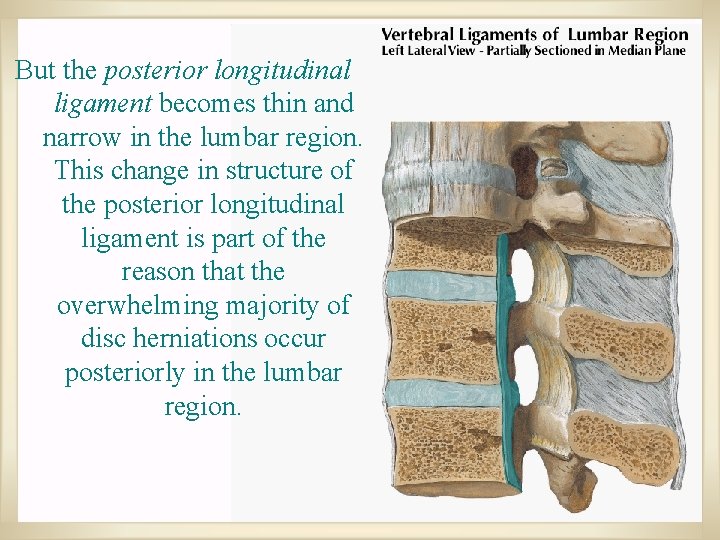
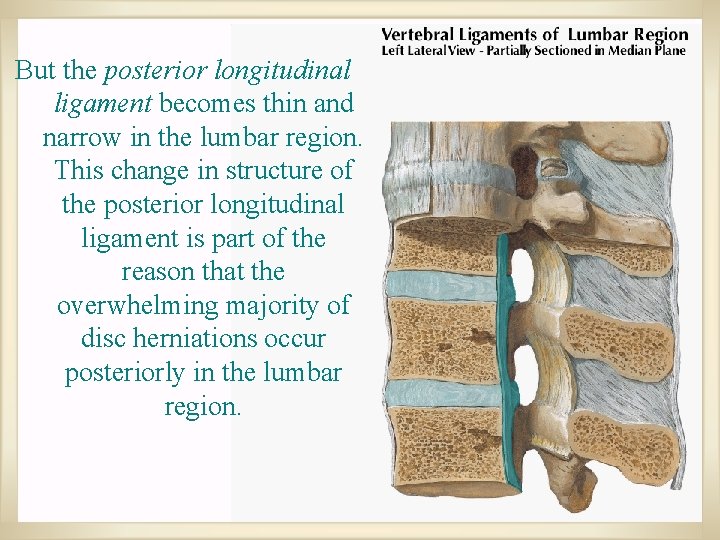
But the posterior longitudinal ligament becomes thin and narrow in the lumbar region. This change in structure of the posterior longitudinal ligament is part of the reason that the overwhelming majority of disc herniations occur posteriorly in the lumbar region.
INJURIES AND DEFORMITIES OF THE VERTEBRAL COLUMN
SPONDYLYSIS; SPONDYLOSIS Chronic degenerative disease of intervertebral discs and/or vertebral bodies. May compress spinal cord, nerves, or roots. If symptoms present, most often present as radiculopathies
SPINAL CORD TRANSECTION • • Results in loss of all sensation and voluntary movement inferior to the lesion Paraplegia: Paralysis of lower body including both lower extremities Results from spinal cord transection between cervical and lumbosacral enlargements Quadriplegia: Paralysis of all four limbs. Results from spinal cord transection superior to C 3
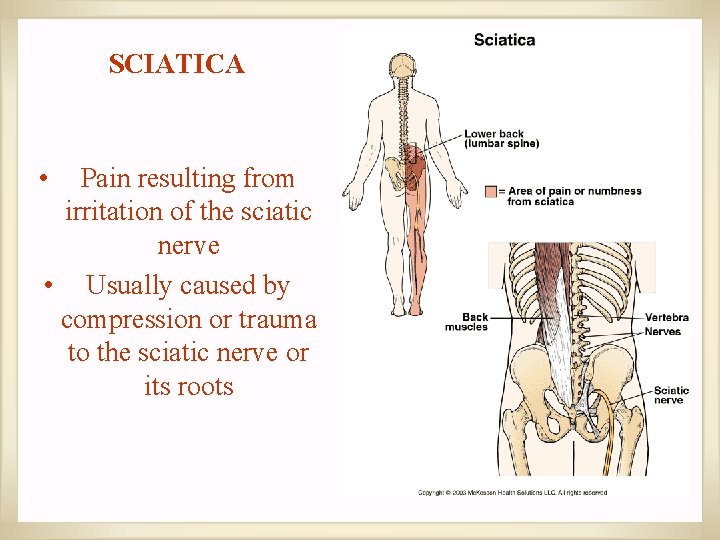
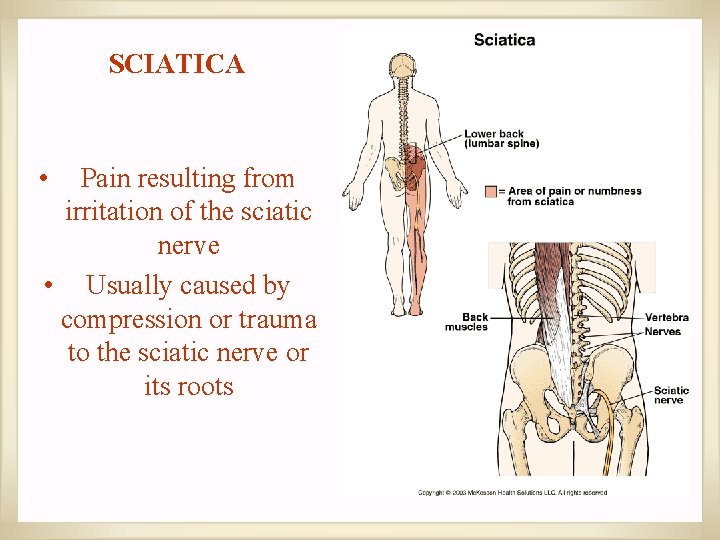
SCIATICA • Pain resulting from irritation of the sciatic nerve • Usually caused by compression or trauma to the sciatic nerve or its roots
RADICULOPATHIES • • Shooting pain that radiates down one or both legs in a dermatomal distribution, often with associated sensory and motor impairment Usually caused by compression or stretching of spinal nerves or roots
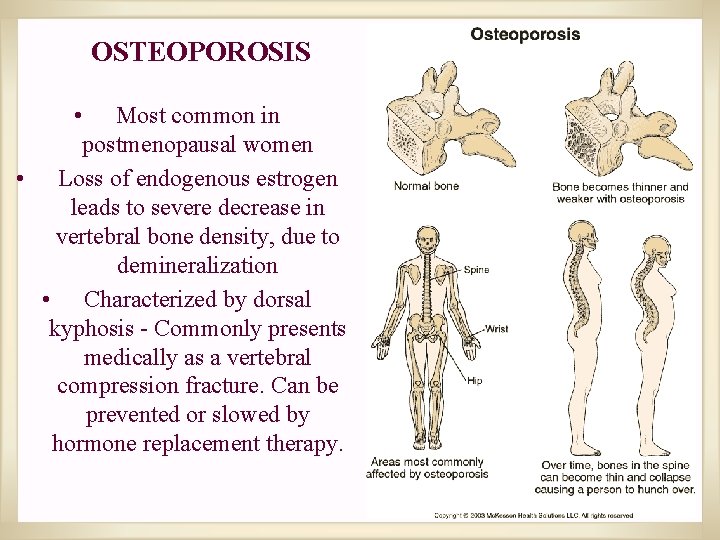
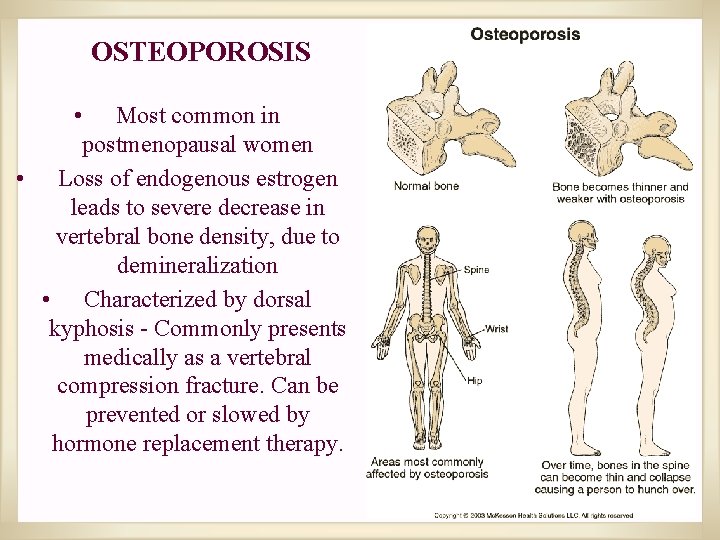
OSTEOPOROSIS • Most common in postmenopausal women • Loss of endogenous estrogen leads to severe decrease in vertebral bone density, due to demineralization • Characterized by dorsal kyphosis - Commonly presents medically as a vertebral compression fracture. Can be prevented or slowed by hormone replacement therapy.
 Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Solid thyroid nodule
Solid thyroid nodule King abdulaziz university faculty of medicine
King abdulaziz university faculty of medicine Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Faculty of veterinary medicine cairo university logo
Faculty of veterinary medicine cairo university logo Hacettepe university faculty of medicine
Hacettepe university faculty of medicine دانشگاه دامپزشکی تهران
دانشگاه دامپزشکی تهران Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Faculty of veterinary medicine cairo university
Faculty of veterinary medicine cairo university Cairo university faculty of veterinary medicine
Cairo university faculty of veterinary medicine Kuwait fire department online
Kuwait fire department online Kuwait university subsidiaries
Kuwait university subsidiaries Faculty of medicine nursing and health sciences
Faculty of medicine nursing and health sciences Mcgill medicine supporting documents
Mcgill medicine supporting documents Pubh4401
Pubh4401 Coumadin clinic emory
Coumadin clinic emory Nit calicut chemistry
Nit calicut chemistry University of split faculty of maritime studies
University of split faculty of maritime studies Bridgeport engineering department
Bridgeport engineering department University of bridgeport computer engineering
University of bridgeport computer engineering Computer science fsu
Computer science fsu Faculty of business and economics mendel university in brno
Faculty of business and economics mendel university in brno Singularity executive program
Singularity executive program Ascaris lumbricoides ova
Ascaris lumbricoides ova Feup university of porto
Feup university of porto Ldap cuni
Ldap cuni Faculty of law of the university of zagreb
Faculty of law of the university of zagreb University of montenegro faculty of law
University of montenegro faculty of law University of kragujevac faculty of technical sciences
University of kragujevac faculty of technical sciences University of cologne faculty of management
University of cologne faculty of management Leading university cse faculty members
Leading university cse faculty members Brown university computer science
Brown university computer science Roumieh university
Roumieh university Myfile york university
Myfile york university Elearningunideb
Elearningunideb Clemson electrical engineering
Clemson electrical engineering Faculty of mechanical engineering thammasat university
Faculty of mechanical engineering thammasat university Faculty of business and economics mendel university in brno
Faculty of business and economics mendel university in brno Chronic meningitis
Chronic meningitis Faculty of public health mahidol university
Faculty of public health mahidol university Thick and thin malaria smear
Thick and thin malaria smear Faculty of education khon kaen university
Faculty of education khon kaen university Shawhong ser
Shawhong ser Department of medicine solna
Department of medicine solna What is textbook
What is textbook Elt supervision
Elt supervision General elt supervision
General elt supervision Eor kuwait
Eor kuwait