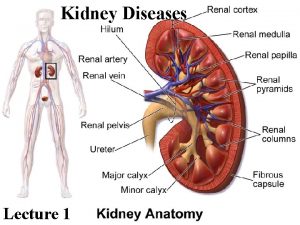
Kidney diseases Dr Manoj Radhakrishnan Addl Professor Dept
- Slides: 25
Kidney diseases Dr. Manoj Radhakrishnan Addl Professor Dept. Of Pathology
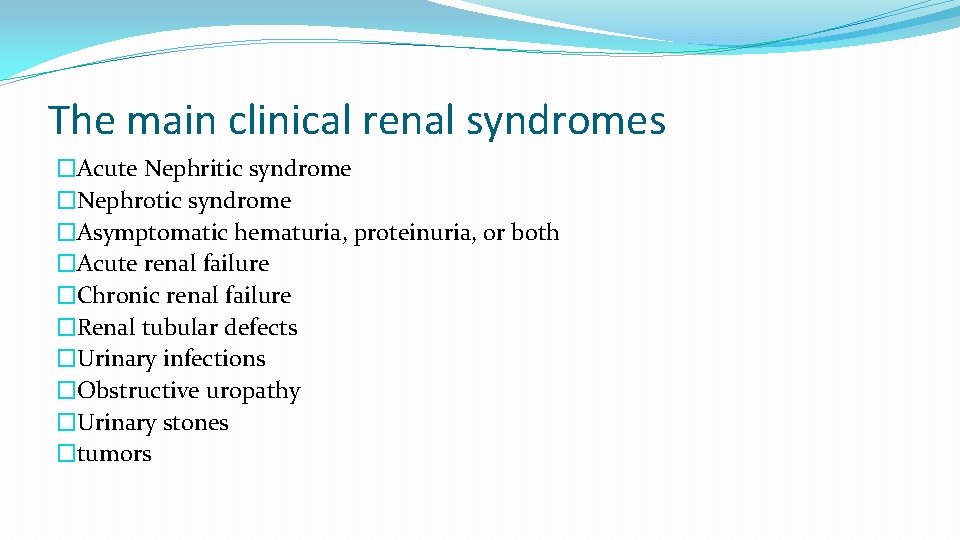
The main clinical renal syndromes �Acute Nephritic syndrome �Nephrotic syndrome �Asymptomatic hematuria, proteinuria, or both �Acute renal failure �Chronic renal failure �Renal tubular defects �Urinary infections �Obstructive uropathy �Urinary stones �tumors
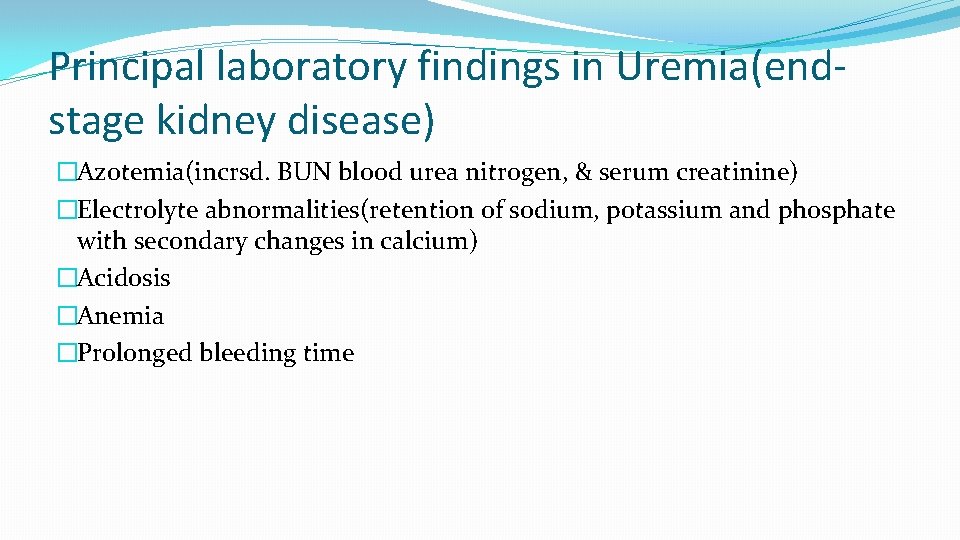
Principal laboratory findings in Uremia(endstage kidney disease) �Azotemia(incrsd. BUN blood urea nitrogen, & serum creatinine) �Electrolyte abnormalities(retention of sodium, potassium and phosphate with secondary changes in calcium) �Acidosis �Anemia �Prolonged bleeding time
Acute nephritic syndrome �Typically presents 1 -2 weeks after an upper respiratory tract infection caused by streptococci Ø Oliguria : due to reduced GFR Ø Hematuria : due to damaged GBM, brownish- red urine, RBCs in urine sediment Ø Protienuria : increased permeability of GBM, maybe mild or severe Ø Generalized edema: “ puffy eyes” due to hypo albuminemia Ø Hypertension : reduced GFR leads to secretion of renin Ø Low complement levels in blood: immune complexes bind the complement Ø Azotemia : high bld urea & serum creatinine
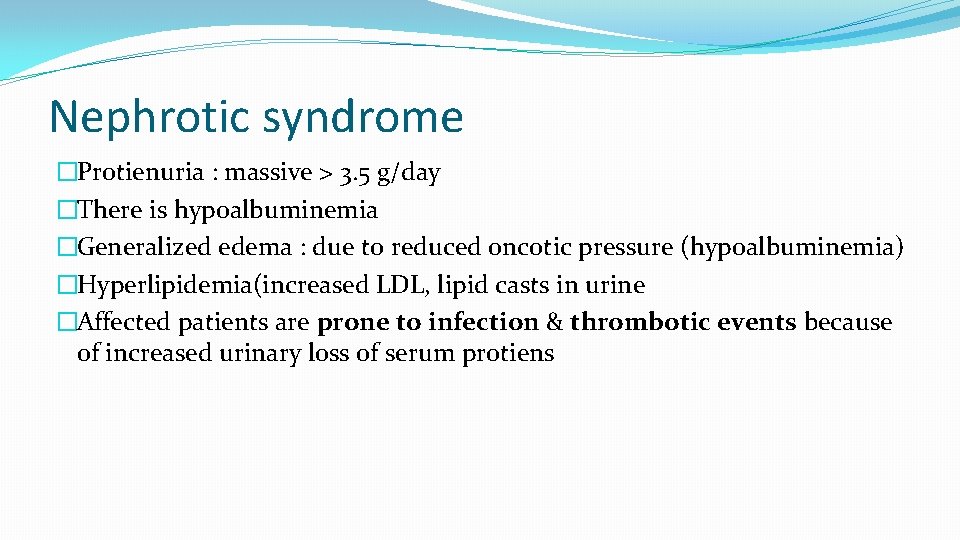
Nephrotic syndrome �Protienuria : massive > 3. 5 g/day �There is hypoalbuminemia �Generalized edema : due to reduced oncotic pressure (hypoalbuminemia) �Hyperlipidemia(increased LDL, lipid casts in urine �Affected patients are prone to infection & thrombotic events because of increased urinary loss of serum protiens
Derangements of urine volume �Anuria : reduced urine output (< 100 ml urine per day ) reflecting renal injury �Oliguria : reduced urine output below 400 ml / day sign of renal failure �Polyuria: increased volume of urine ( > 3 L of urine per day) may result from excessive fluid intake, osmotic diuresis( eg Diabetes insipidus) or impaired tubular concentration (eg tubular necrosis)
Features of Acute renal failure �Is characterised most often b reversible detrioration of renal function Ø Oliguria Ø Azotemia ( increased Blood Urea, Serum Creatinine) Ø Electrolyte disturbances �Most patients recover without dialysis
Chronic renal failure �Develops insidiously in stages Ø Diminished renal reserve : develop high urea, creatinine levels during inter-current illness Ø Renal insufficiency : GFR ( 20% - 50% of normal)azotemia anemia, polyuria Ø Renal failure : (<20% of normal GFR) & edema metabolic acidosis hypocalcemia, and multi-sstem signs of uremia Ø End-stage renal failure : <5% GFR , clinical signs of uremia
Features of urinary tract Infection �Charcterised by bacteriuria & pyuria �>100, 000 bacteria/ml of cultured urine �> 10 wbcs /HPF in urine sample �Leucocytes are counted in urinary sediment �Signs of urinary irritation- urgency, pain
Antibody associated glomerular Injury �Antibodies to endogenous antigens of the GBM : This mechanism accounts for the renal inury in Goodpasture syndrome a disease caused by antibodies to collagen type IV �Antibodies to non-glomerular antigens : Antigen-antibody complexes found in glomeruli may result from two pathogenetic mechanisms. Ø In situ immune complex formation results from the binding of circulating antibodies– seen in PSGN ( post streptococcal GN) where streptococcal antigens are implantedin the GBM during the infection Ø Circulating immune complexes formed from soluble antigens and corresponding Ab – eg seen in SLE
PSGN �Group A beta- hemolytic streptococci ( streptococcus pyogenes) account for 90% of all GN cases �Typically occurs 1 -4 weeks after a strep throat infection or skin Infection(Impetigo) �Occasionally same clinical-pathological findings may follow staphlococcal infection or even some viral diseases –HBV, HCV or HIV Infection �.
PSGN �The increase in cellularity is due to increasi in epithelial endothelial and mesangial cells �As well as neutrophils in and around capillary loops.
PSGN �Showing increased number of neutrophils , in post-infectious GN
sub-epithelial humps in acute PSGN �Represent epimembranous deposits of immune complexes on the GBM, seen under Electron microscope. �Immunofluorescence shows many other immune complexes not dense enough to be seen by EM �Smaller immune complexes in mesangium
Clinical features of acute PSGN(nephritic syndrome) �Childhood disease �Presents with fever, nausea, oliguria, hematuria, RBC casts in urine, mild protienuria(usually less than < 1 g/ day) peri-orbital edema and mild to moderate HT �As immune complex deposition is assoc. with complement activation C 3 is the complement consumed in both classical and alternate complement pathway. Hence there will be hypo-complementemia
Outcome & long term consequences of acute PSGN �CHILDREN Ø 90% recover within 2 -3 months with conservative therapy aimed at maintaining sodium & water balance. Ø 5 -8% have persistent GN, in much milder form with abnormal urinary findings for 6 -8 months. Ø <1% cases develop Rapidly progressive GN (RPGN) �ADULTS Ø 60% recover promptly Ø 3 -5% develop RPGN
Rapidly progressive glomerulonephritis is reflective of advaned renal pathology �Mostly caused by immunologic mechanisms �Is assoc. with 25% mortality & 40 % progression to chronic end- stage kidney disease � 3 groups Ø A. N. C. A + Cases(Anti-neutrophil cytoplasmic Ab) , most Adult cases , Wegener’s granulomatosis, P. A. N Ø Immune complex mediated – most common form seen in children & young adults < 20 years – seen in post-infectious GN(PSGN) , SLE Ø Anti-GBM Ab – Good Pasteur's syndrome
RPGN or crescentic GN �Crescents are found in more than 50 % of glomeruli represent a sin of severe glomerular injury �Usually starts as focal and segmental necrosis – resulting inrupture of the GBM which allows the entry of inlammatory cells and fibrinogen into theurinary space
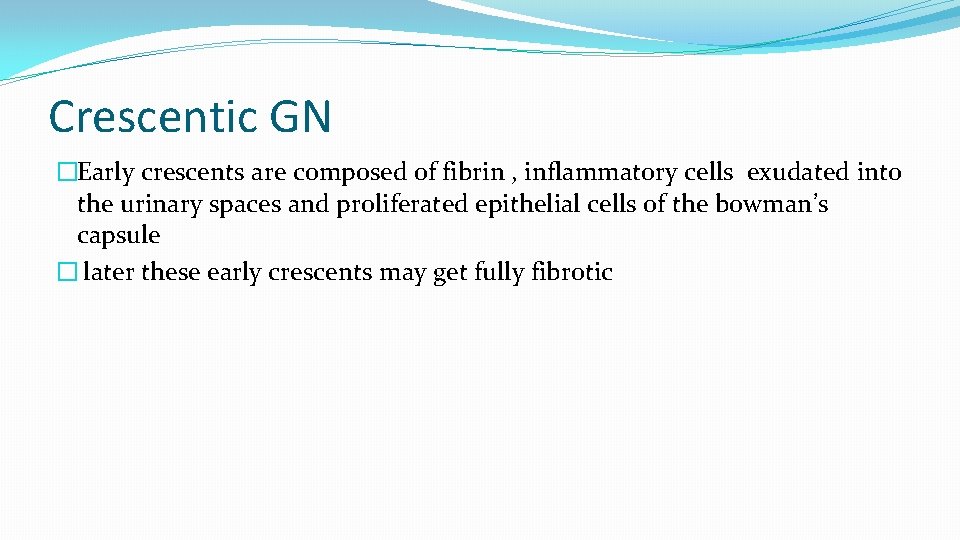
Crescentic GN �Early crescents are composed of fibrin , inflammatory cells exudated into the urinary spaces and proliferated epithelial cells of the bowman’s capsule � later these early crescents may get fully fibrotic
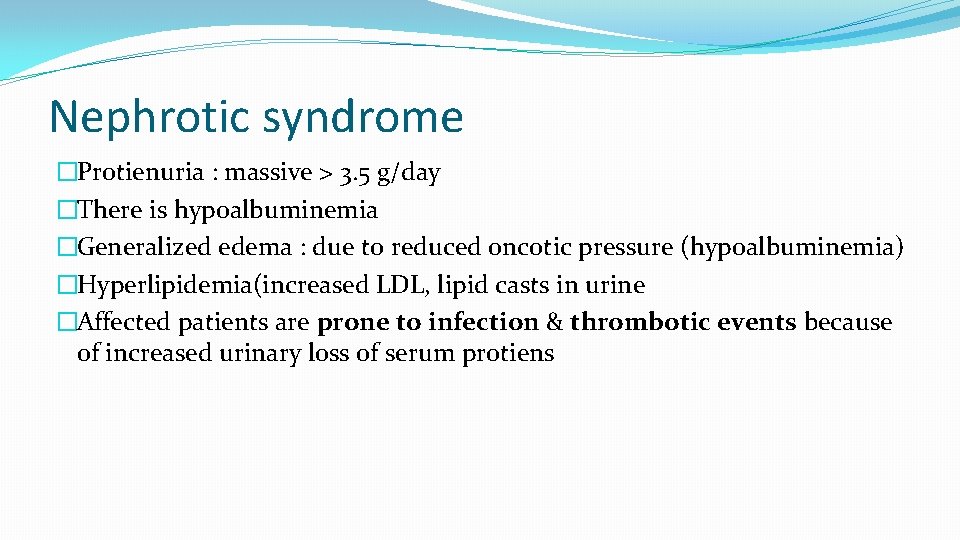
Nephrotic syndrome �Protienuria : massive > 3. 5 g/day �There is hypoalbuminemia �Generalized edema : due to reduced oncotic pressure (hypoalbuminemia) �Hyperlipidemia(increased LDL, lipid casts in urine �Affected patients are prone to infection & thrombotic events because of increased urinary loss of serum protiens
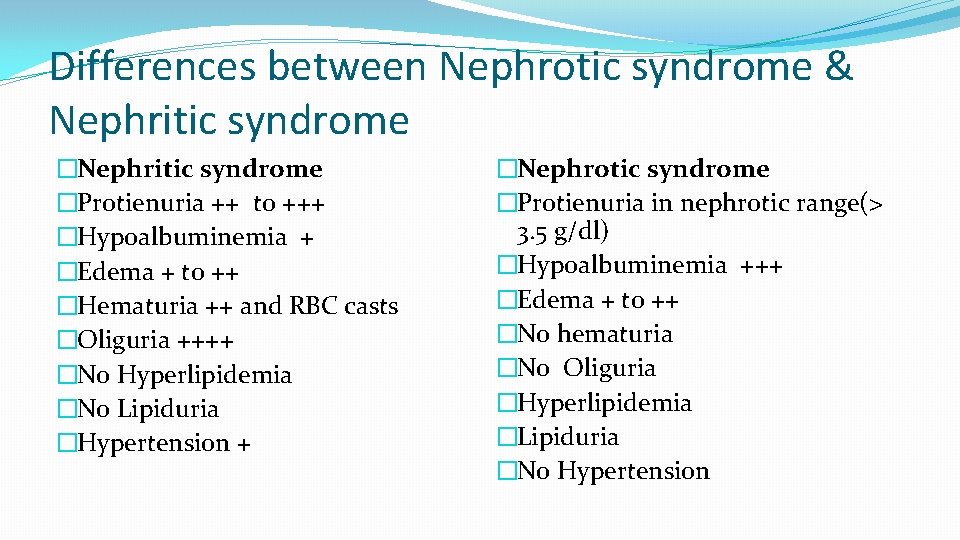
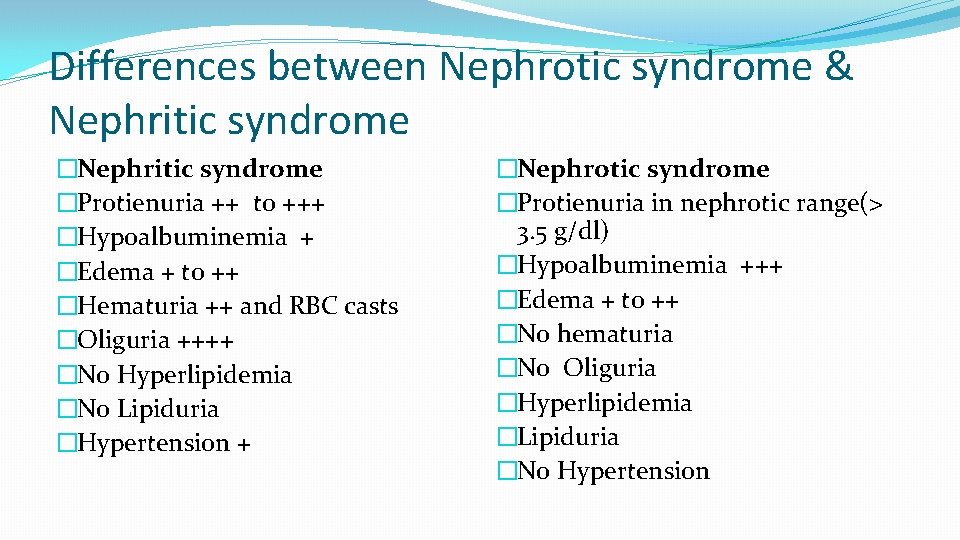
Differences between Nephrotic syndrome & Nephritic syndrome �Protienuria ++ to +++ �Hypoalbuminemia + �Edema + to ++ �Hematuria ++ and RBC casts �Oliguria ++++ �No Hyperlipidemia �No Lipiduria �Hypertension + �Nephrotic syndrome �Protienuria in nephrotic range(> 3. 5 g/dl) �Hypoalbuminemia +++ �Edema + to ++ �No hematuria �No Oliguria �Hyperlipidemia �Lipiduria �No Hypertension
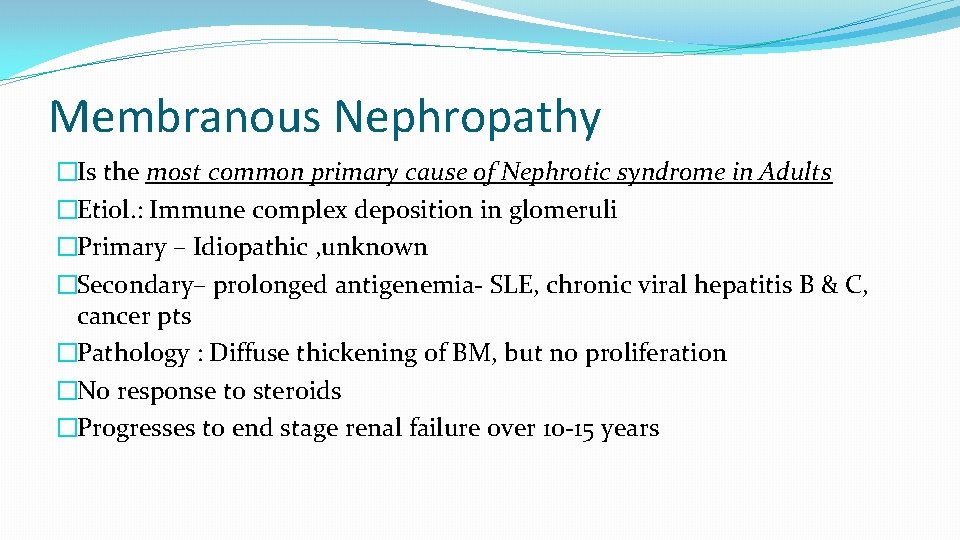
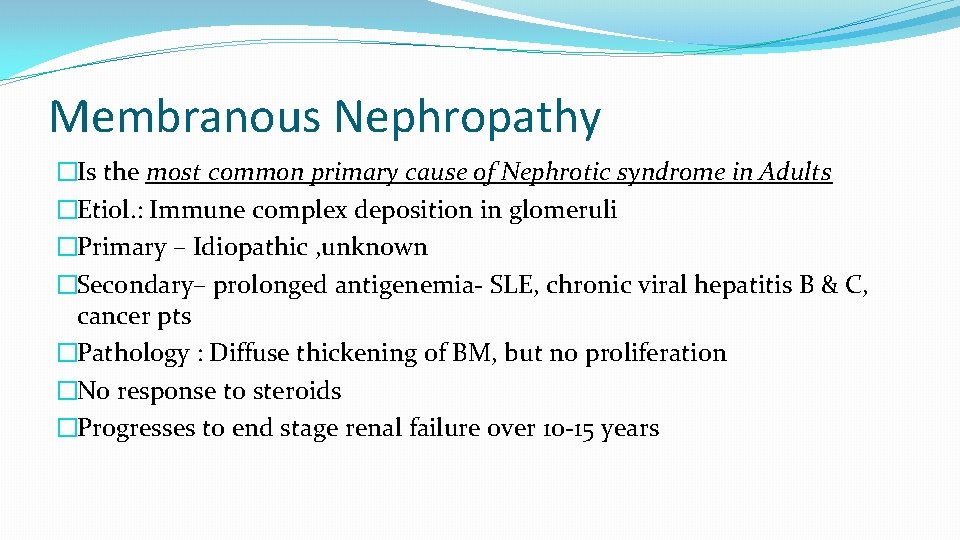
Membranous Nephropathy �Is the most common primary cause of Nephrotic syndrome in Adults �Etiol. : Immune complex deposition in glomeruli �Primary – Idiopathic , unknown �Secondary– prolonged antigenemia- SLE, chronic viral hepatitis B & C, cancer pts �Pathology : Diffuse thickening of BM, but no proliferation �No response to steroids �Progresses to end stage renal failure over 10 -15 years
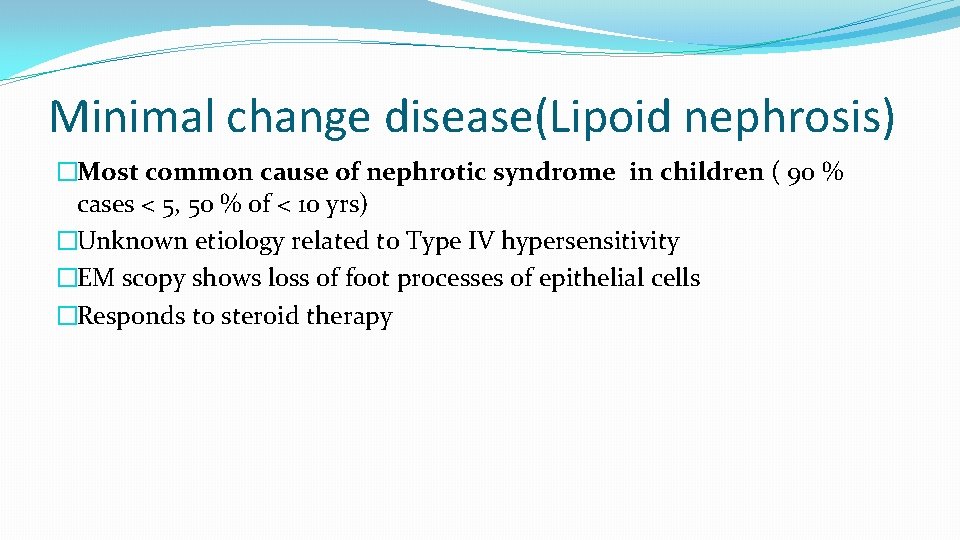
Minimal change disease(Lipoid nephrosis) �Most common cause of nephrotic syndrome in children ( 90 % cases < 5, 50 % of < 10 yrs) �Unknown etiology related to Type IV hypersensitivity �EM scopy shows loss of foot processes of epithelial cells �Responds to steroid therapy
How does SLE affect the kidneys? �Signs of renal disease are found in 50 % of patients at the time of diagnosis � 80% will develop some signs of renal disease at some time during the life span. �SLE is an immune complex mediated disease, immune complexes are deposited in Ø Glomeruli : most frequently affected part, Immune complexes maybe trapped on the sub-endothelial side, inside the GBM, or on the sub epithelial side & mesangium basement membranes lined with sub-endothelial deposits appear thickened , called wireloops Ø Blood vessels Ø Tubules & interstitial spaces
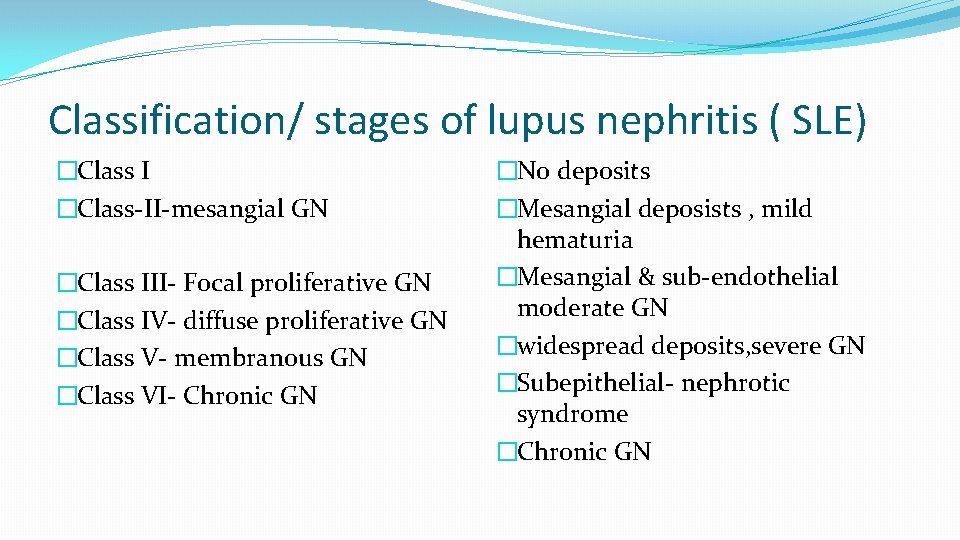
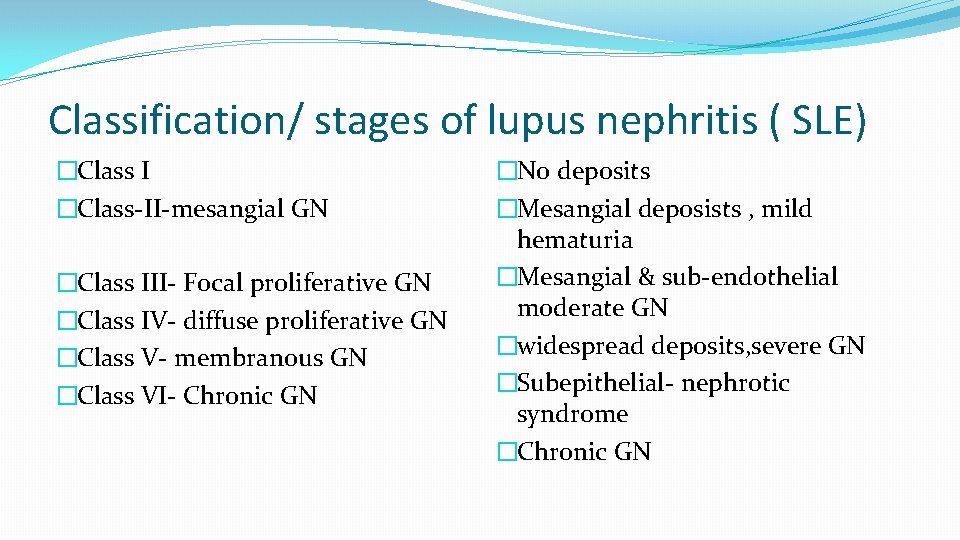
Classification/ stages of lupus nephritis ( SLE) �Class I �Class-II-mesangial GN �Class III- Focal proliferative GN �Class IV- diffuse proliferative GN �Class V- membranous GN �Class VI- Chronic GN �No deposits �Mesangial deposists , mild hematuria �Mesangial & sub-endothelial moderate GN �widespread deposits, severe GN �Subepithelial- nephrotic syndrome �Chronic GN
 Manoj radhakrishnan
Manoj radhakrishnan Sarvepalli radhakrishnan
Sarvepalli radhakrishnan Jai radhakrishnan
Jai radhakrishnan Veena radhakrishnan
Veena radhakrishnan Promotion from associate professor to professor
Promotion from associate professor to professor Measurement and scaling
Measurement and scaling Manoj abichandani
Manoj abichandani Given signs signify something and on that basis
Given signs signify something and on that basis Manoj toshniwal dubai
Manoj toshniwal dubai Panama real estate law
Panama real estate law Manoj magician
Manoj magician Dr manoj das products
Dr manoj das products Manoj mehta ficci
Manoj mehta ficci Department of finance and administration
Department of finance and administration Nys dept of homeland security
Nys dept of homeland security Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Vaginal dept
Vaginal dept Worcester ma building department
Worcester ma building department Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Nebraska dept of agriculture
Nebraska dept of agriculture Albany county dept of social services
Albany county dept of social services Dept of education
Dept of education Gome dept
Gome dept Oviposition
Oviposition Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) La dept of revenue
La dept of revenue