Joint Trauma System Prolonged Field Care Clinical Practice




- Slides: 26
Joint Trauma System Prolonged Field Care Clinical Practice Guideline Burn wound management in prolonged field care Joint Trauma System, U. S. Army Institute of Surgical Research 3698 Chambers Pass, Bldg 3611, Fort Sam Houston, TX 78234
Burns > 20% TBSA, or those with smoke inhalation injury (and airway or breathing problems), are potentially life threatening. Also, burns that affect vision, decrease hand function, or cause severe pain can take the warfighter out of action. 05 November 2020 2
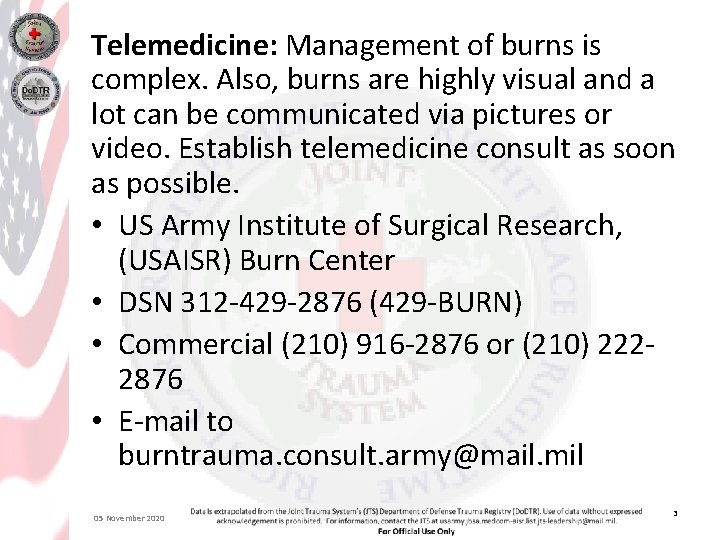
Telemedicine: Management of burns is complex. Also, burns are highly visual and a lot can be communicated via pictures or video. Establish telemedicine consult as soon as possible. • US Army Institute of Surgical Research, (USAISR) Burn Center • DSN 312 -429 -2876 (429 -BURN) • Commercial (210) 916 -2876 or (210) 2222876 • E-mail to burntrauma. consult. army@mail. mil 05 November 2020 3
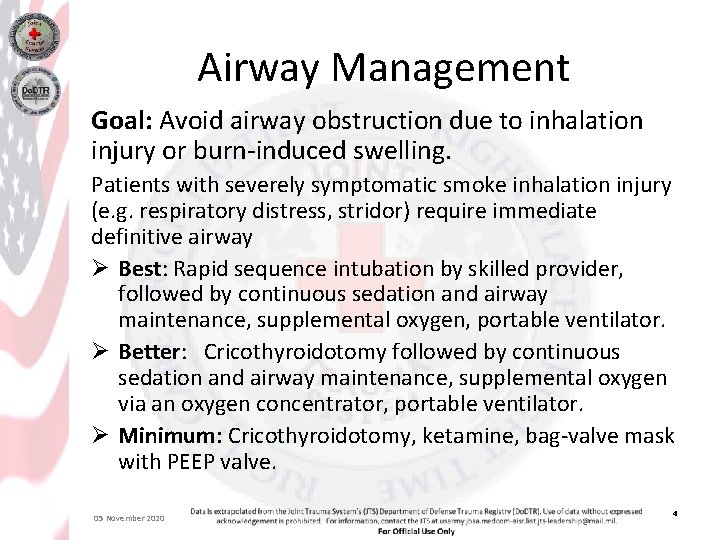
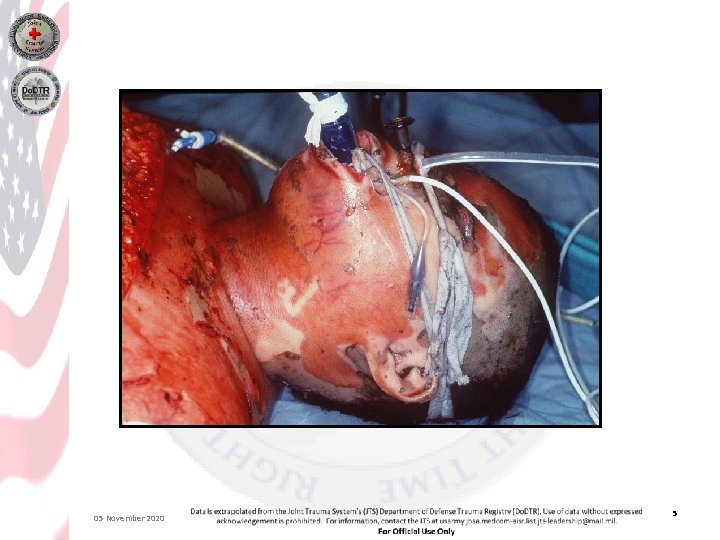
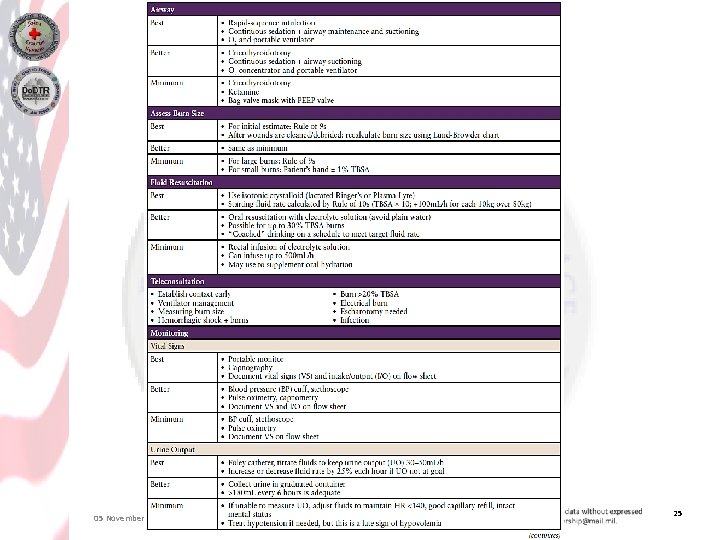
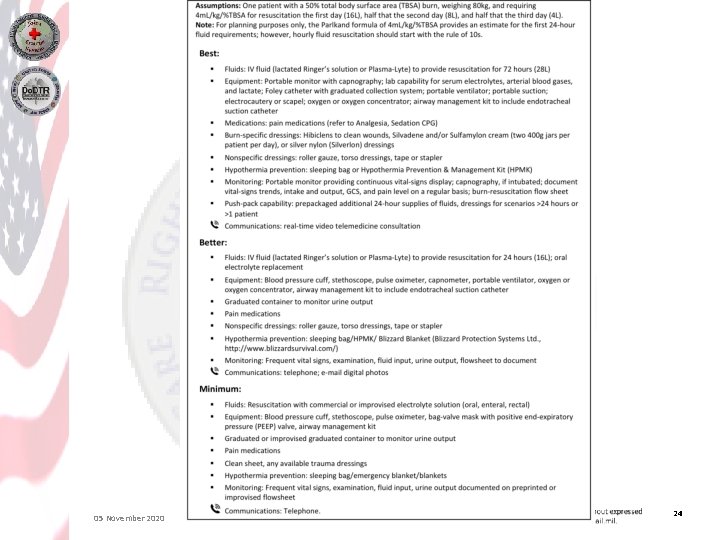
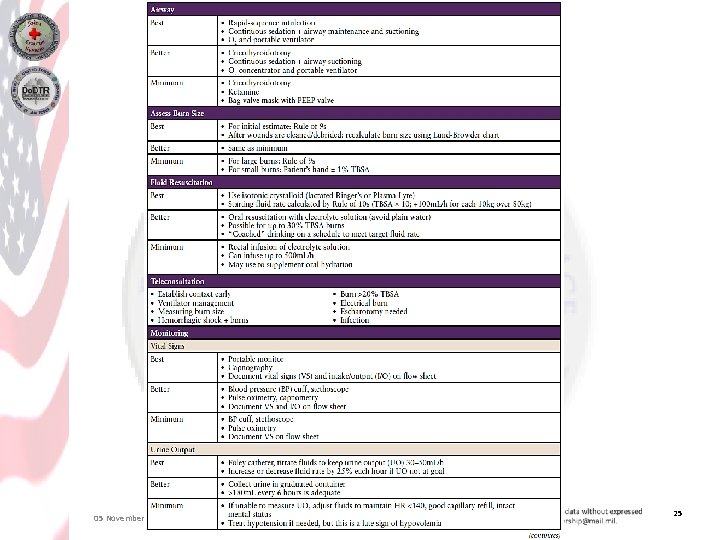
Airway Management Goal: Avoid airway obstruction due to inhalation injury or burn-induced swelling. Patients with severely symptomatic smoke inhalation injury (e. g. respiratory distress, stridor) require immediate definitive airway Ø Best: Rapid sequence intubation by skilled provider, followed by continuous sedation and airway maintenance, supplemental oxygen, portable ventilator. Ø Better: Cricothyroidotomy followed by continuous sedation and airway maintenance, supplemental oxygen via an oxygen concentrator, portable ventilator. Ø Minimum: Cricothyroidotomy, ketamine, bag-valve mask with PEEP valve. 05 November 2020 4
05 November 2020 5
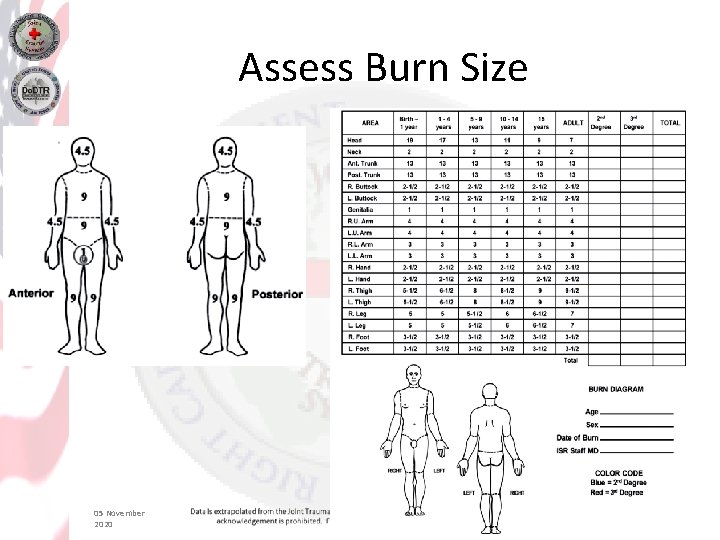
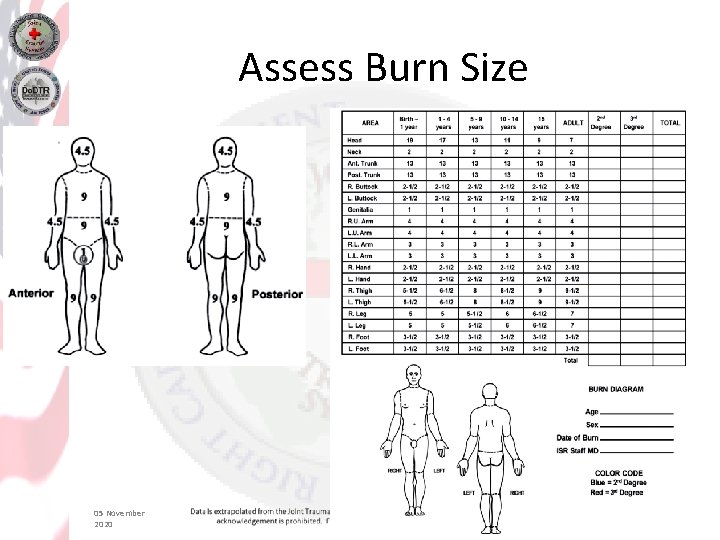
Assess Burn Size 05 November 2020 6

05 November 2020 7

05 November 2020 8

05 November 2020 9

05 November 2020 10
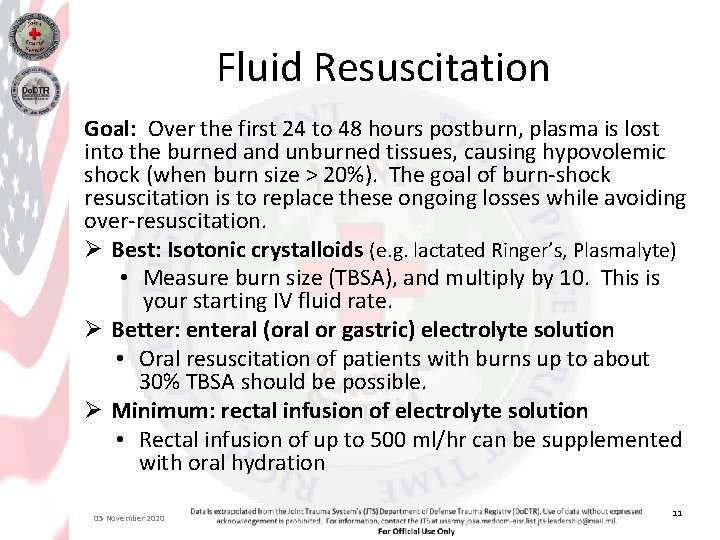
Fluid Resuscitation Goal: Over the first 24 to 48 hours postburn, plasma is lost into the burned and unburned tissues, causing hypovolemic shock (when burn size > 20%). The goal of burn-shock resuscitation is to replace these ongoing losses while avoiding over-resuscitation. Ø Best: Isotonic crystalloids (e. g. lactated Ringer’s, Plasmalyte) • Measure burn size (TBSA), and multiply by 10. This is your starting IV fluid rate. Ø Better: enteral (oral or gastric) electrolyte solution • Oral resuscitation of patients with burns up to about 30% TBSA should be possible. Ø Minimum: rectal infusion of electrolyte solution • Rectal infusion of up to 500 ml/hr can be supplemented with oral hydration 05 November 2020 11
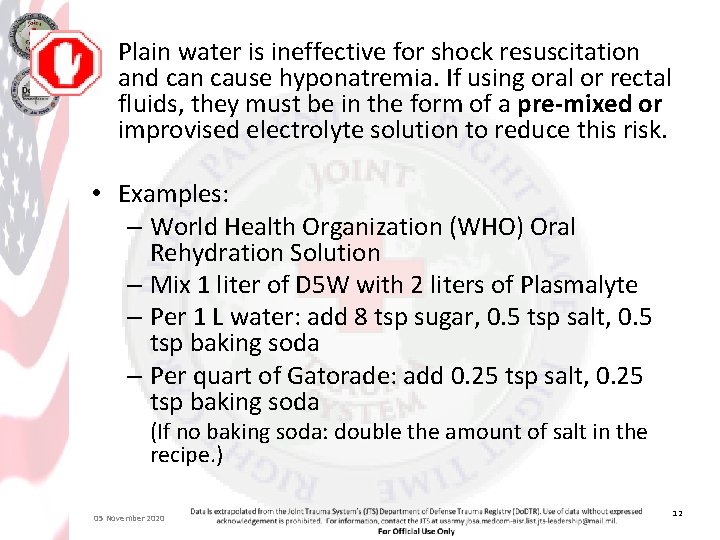
Plain water is ineffective for shock resuscitation and can cause hyponatremia. If using oral or rectal fluids, they must be in the form of a pre-mixed or improvised electrolyte solution to reduce this risk. • Examples: – World Health Organization (WHO) Oral Rehydration Solution – Mix 1 liter of D 5 W with 2 liters of Plasmalyte – Per 1 L water: add 8 tsp sugar, 0. 5 tsp salt, 0. 5 tsp baking soda – Per quart of Gatorade: add 0. 25 tsp salt, 0. 25 tsp baking soda (If no baking soda: double the amount of salt in the recipe. ) 05 November 2020 12
Monitoring Goal: maintain adequate oxygenation and ventilation, avoid hypotension, trend response to resuscitation. Vital signs Ø Best: Portable monitor providing continuous vital-sign display; capnography if intubated; document vital sign trends frequently (every 15 minutes initially, then every 30 -60 minutes once stable for more than 2 hours). Ø Better: Capnometry in addition to minimum requirements (if intubated). Ø Minimum: blood pressure cuff, stethoscope, pulse oximetry, document vital sign trends frequently. 05 November 2020 13
Monitoring Urine Output is the main indicator of resuscitation adequacy in burn shock. Goal: adjust IV (or oral/rectal intake) rate to urine output (UO) goal of 30 -50 ml/hr. Ø Best: place Foley catheter Ø Better: capture urine in pre-made or improvised graduated cylinder • Collect all spontaneously voided urine hourly and carefully measure; > 180 ml every 6 hours is adequate. Ø Minimum: use other measures • 05 November 2020 If unable to measure urine output, adjust IV rate to maintain heart rate (HR) < 140, palpable peripheral pulses, good capillary refill, intact mental status. 14
Note: Electric injury – Patients with high-voltage electric injury causing muscle damage and gross pigment in the urine (and similar patients, such as rhabdomyolysis or crush) have a higher target urine output of 70 -100 m. L/hr in adults. See PFC Crush CPG. – If this does not cause gradual clearing of the pigment (urine turns lighter on 3 or 4 hourly checks), the patient likely needs urgent surgery for decompression/debridement. 05 November 2020 15
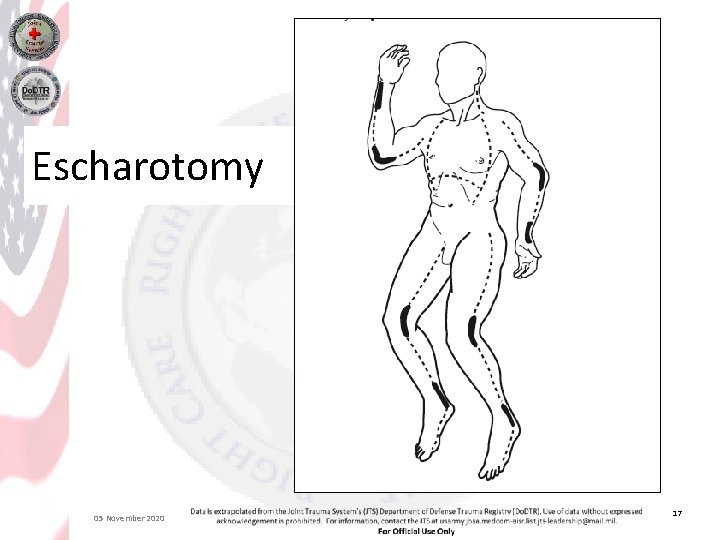
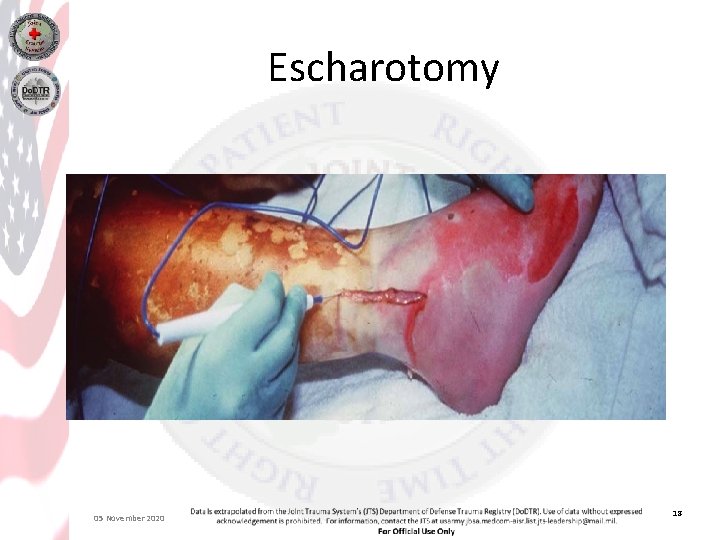
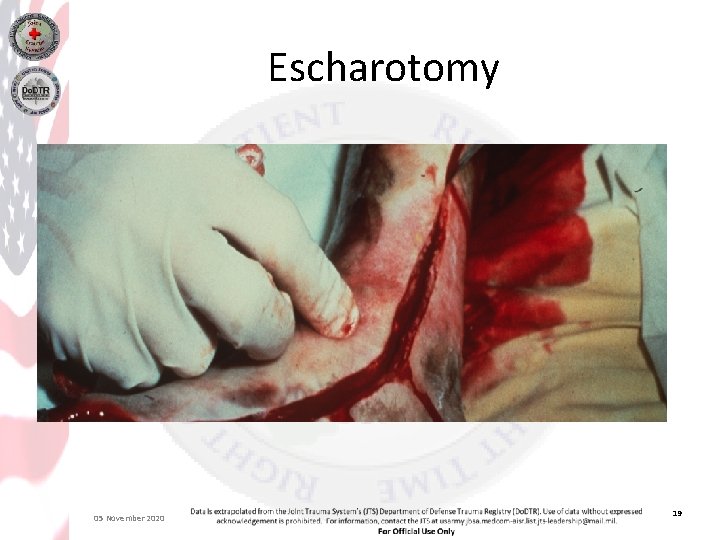
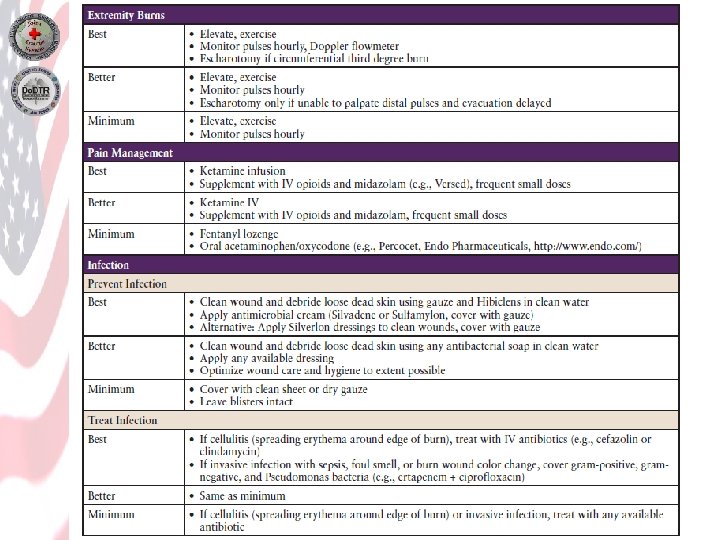
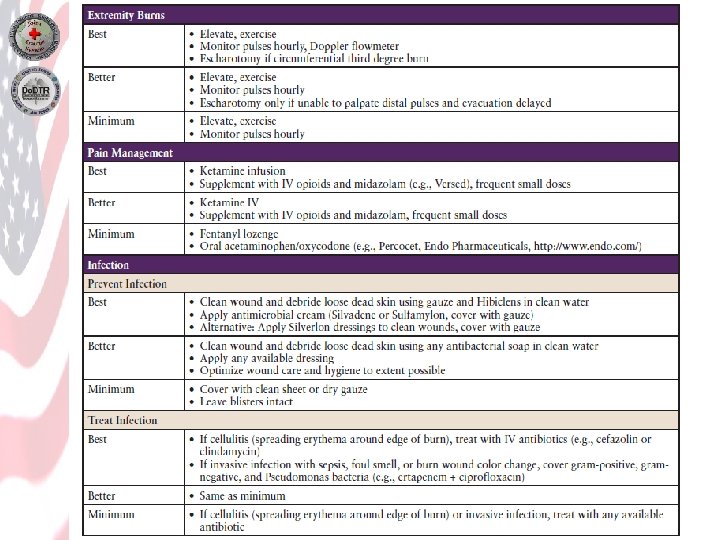
Extremity Burns Burned extremities are vulnerable to injury from postburn swelling. Goal: Prevent and manage swelling of burned extremities, to prevent long-term damage. Ø Best: Elevate above heart level. Encourage exercise. Monitor peripheral pulses hourly—use Doppler if available. Perform escharotomies of circumferential burns to restore blood flow. Anticipate blood loss and prepare for blood transfusion. Obtain teleconsultation. Ø Better: Consider escharotomies for circumferential full thickness burns of an extremity if extremity is edematous, you are unable to palpate distal pulses, and evacuation will be delayed. Anticipate blood loss and prepare for blood transfusion. Obtain teleconsultation. Ø Minimum: Triage patient to more rapid evacuation if extremity is edematous and you are unable to palpate distal pulses. Elevate burned extremities above heart level and have patient exercise or provide passive range of motion (PROM) to burned extremities to mobilize edema. Provide pain control to enable PROM. 05 November 2020 16
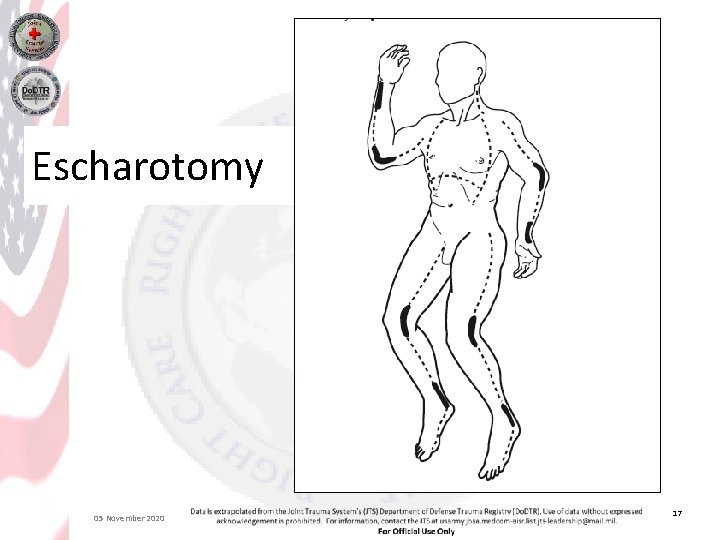
Escharotomy 05 November 2020 17
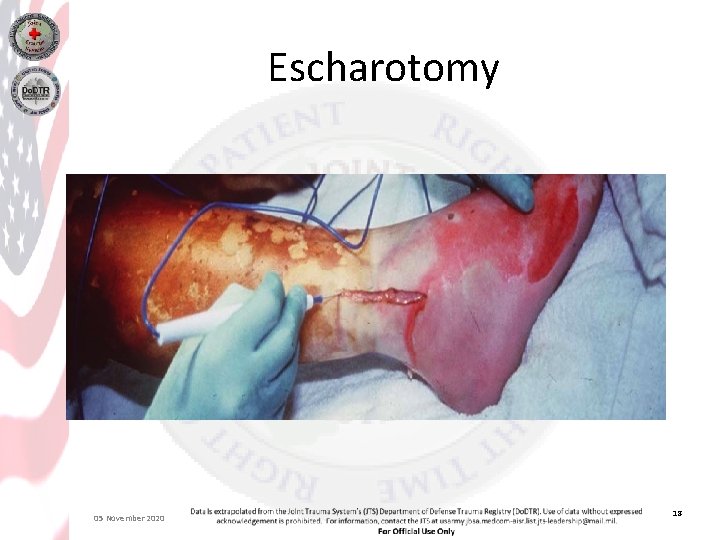
Escharotomy 05 November 2020 18
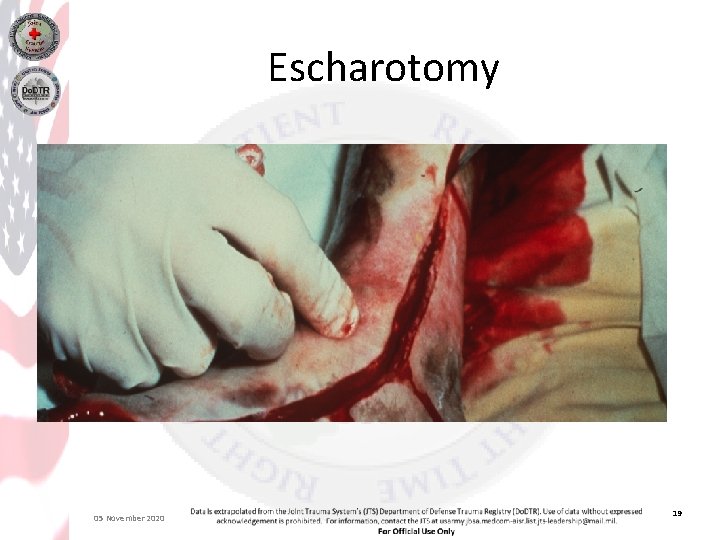
Escharotomy 05 November 2020 19
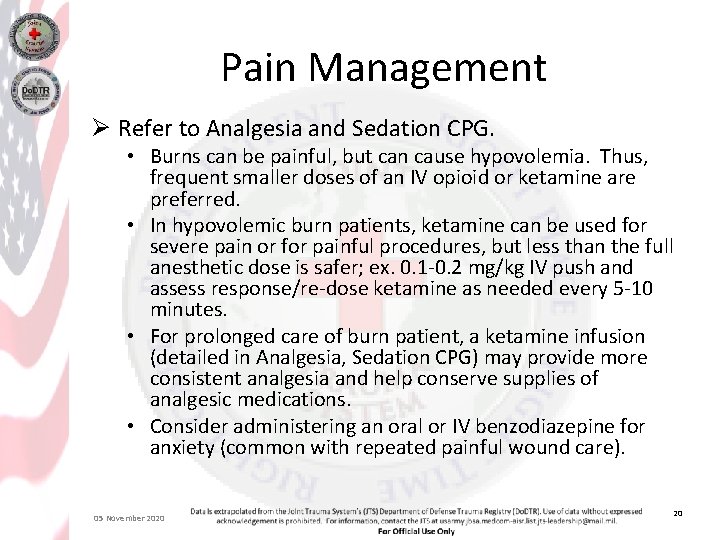
Pain Management Ø Refer to Analgesia and Sedation CPG. • Burns can be painful, but can cause hypovolemia. Thus, frequent smaller doses of an IV opioid or ketamine are preferred. • In hypovolemic burn patients, ketamine can be used for severe pain or for painful procedures, but less than the full anesthetic dose is safer; ex. 0. 1 -0. 2 mg/kg IV push and assess response/re-dose ketamine as needed every 5 -10 minutes. • For prolonged care of burn patient, a ketamine infusion (detailed in Analgesia, Sedation CPG) may provide more consistent analgesia and help conserve supplies of analgesic medications. • Consider administering an oral or IV benzodiazepine for anxiety (common with repeated painful wound care). 05 November 2020 20
Infection Goal: Prevent burn-wound infection through wound care. Note. If evacuation to higher level of care is anticipated within 24 hours, cover burns with clean gauze. Leave intact blisters in place. Avoid wet dressings due to risk of hypothermia. If not: Ø Best: Clean and debride wounds by scrubbing with Hibiclens in water; apply Silvadene or Sulfamylon cream and gauze dressing. Repeat daily. • Alternative: Use silver nylon dressing (Silverlon), followed by gauze dressing. Change Silverlon every 3 -5 days. Ø Better: Ensure wounds cleaned and dressed; optimize wound and patient hygiene to the extent possible given environment. Ø Minimum: Cover with clean sheet or dry gauze. Leave blisters in place. Avoid wet dressings. 05 November 2020 21
Infection IV or oral antibiotics are not normally used for prophylaxis in burn patients. Ø After several days, if patient develops cellulitis (spreading erythema around edges of burn), treat for gram-positive organisms. Ø If patient develops invasive burn-wound infection (sepsis/septic shock, changes in color of wound, possible foul smell of wound) consider broad-spectrum antibiotics to include gram-negative coverage. 05 November 2020 22
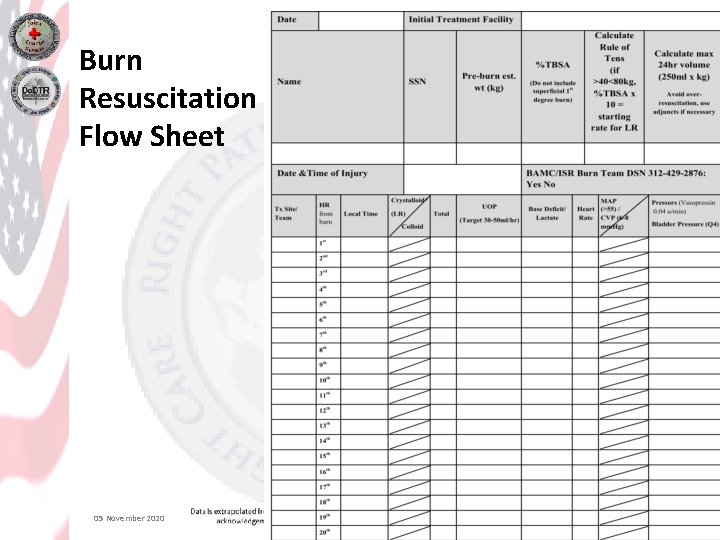
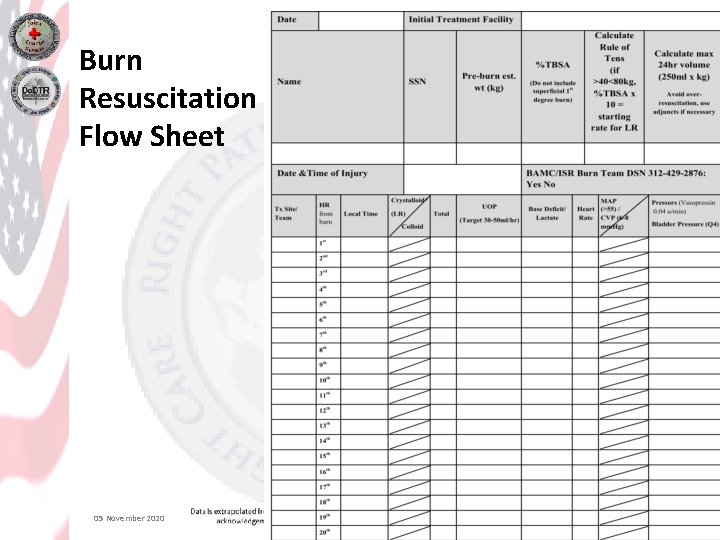
Burn Resuscitation Flow Sheet 05 November 2020 23
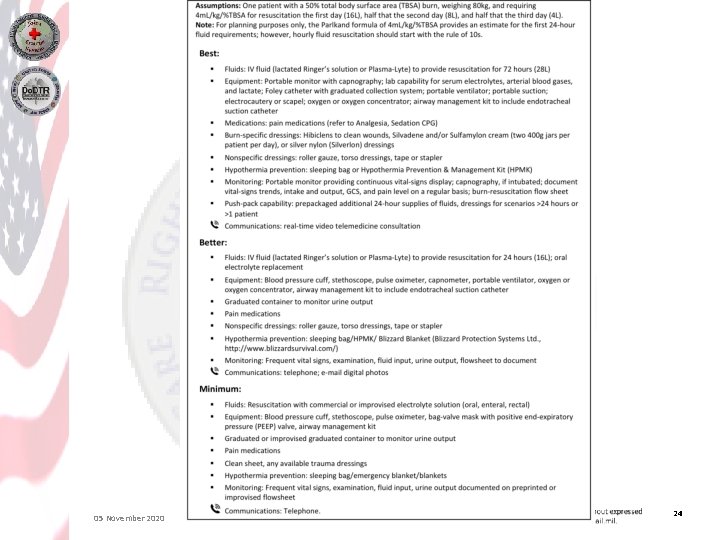
05 November 2020 24
05 November 2020 25
05 November 2020 26