JIA associated uveitis Uveitis morning lectures 24072019 Or








- Slides: 30
JIA associated uveitis Uveitis morning lectures 24/07/2019 Or shmueli
JIA • characterized by arthritis beginning before the age of 16 that lasts at least 6 weeks. • JIA is the most common systemic disorder associated with uveitis in the pediatric age group. • the pathophysiology is presumed to be autoimmune. With supporting evidence of serum autoantibodies. The mechanism of uveitis is immune complex mediated. Egeskjold EM, Johansen A, Permin H, et al. The significance of antinuclear antibodies in juvenile rheumatoid arthritis associated with chronic bilateral iridocyclitis. Acta Paediatr Scand 1982; 71: 615 -620.
JIA-3 subtypes • 10% -systemic (Still disease) • fever, rash, lymphadenopathy, hepatospelenomegaly. • uveitis is rare. • 40% -polyarticular • more than 4 joints involved during the first 6 months of onset. • accounts for 10 % of JIA associated uveitis. • RF+ may not develop uveitis.
JIA-3 subtypes • 50%-oligoarticular • up to four joints involved at the first 6 months of onset of arthritis and patients may have no joint symptoms. • accounts for 80 -90% of JIA-uveitis.
JIA-3 subtypes • 50%-oligoarticular • type 1 - female, less then 5 years of age, typically ANA (+). 25% of whom develop chronic anterior Uveitis. • type 2 - older males, many of whom develop seronegative spondyloarthropaties (75% are HLA B 27 positive). uveitis in these patients is typically acute and recurrent.
JIA- uveitis • Epidemiology: • average onset at 6 years of age. • generally developes within 5 -7 years of JIA diagnosis (but may be even 28 years later). • there is usually no correlation between ocular and joint inflammation.
JIA- uveitis • Risk factors for development of uveitis: • female gender • oligoarticular disease • ANA (+) • usually RF (-)
JIA- uveitis • Clinically a chronic bilateral non-granulomatous anterior uveitis. • symptoms include: • Mild or no pain. • Photophobia. • blurry vision. • some patients may be asymptomatic. • often found incidentally on routine physical exam In school.
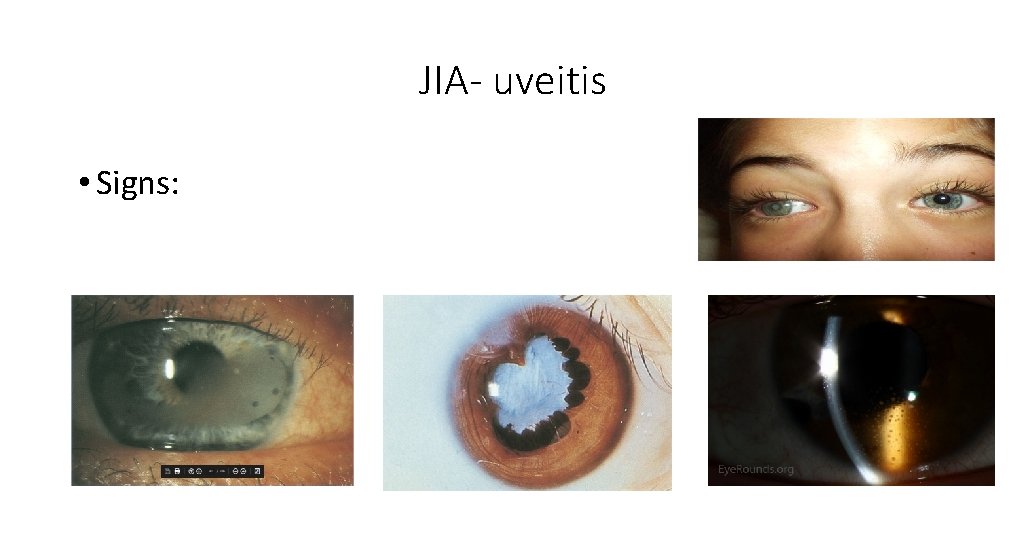
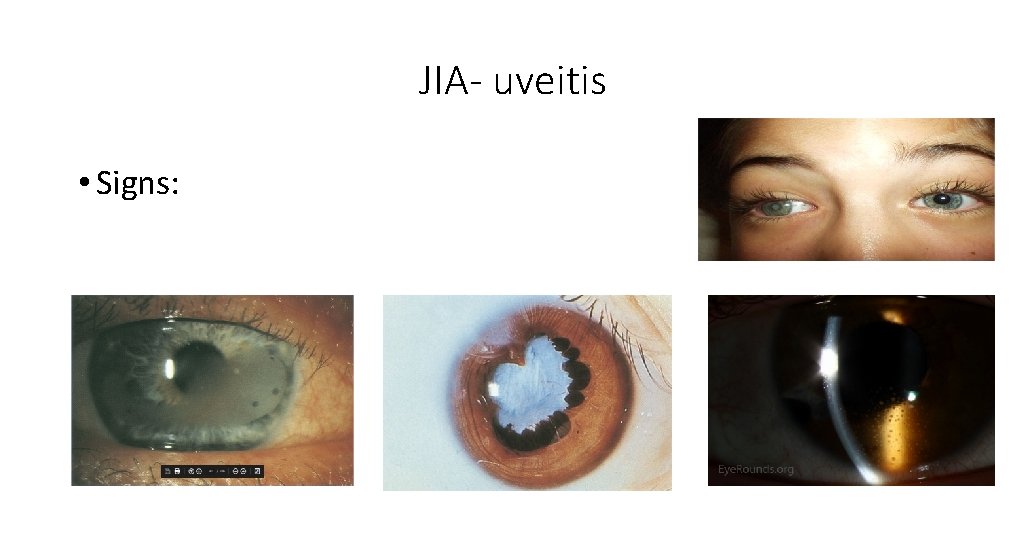
JIA- uveitis • Signs:

JIA- uveitis • Signs- chronic bilateral non-granulomatous anterior uveitis: • Typically White eye with no redness. • Fine KPs. • band keratopathy. • Flare and cells. • Posterior synechiae. • Cataract.
JIA- uveitis • Patients in whom JIA-uveitis is suspected should be referred to a pediatric rheumatologist and tested for ANA because the arthritis may be very mild at the time of uveitis diagnosis.
JIA- uveitis • Differential diagnosis? • TINU • Fuchs heterochromic uveitis • Sarcoidosis • Behcet disease • Seronegative spondiloarthropaties • Herpetic uveitis • Lyme disease
JIA- uveitis • Complications are frequent and severe, often at diagnosis: • band keratopathy. • posterior synechiae. • cataract. • glaucoma (angle closure due to ant. And post. synchiae, open angle due to presumed trabeculitis or d/t steroids). • cystoid macular edema. • cyclitic membranes with TRD, chronic hypotony and phtisis.
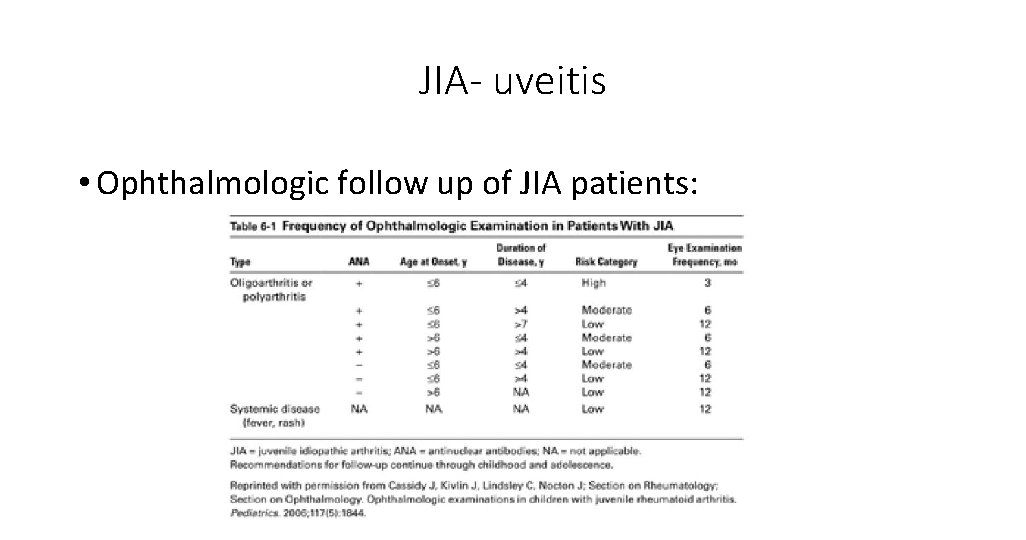
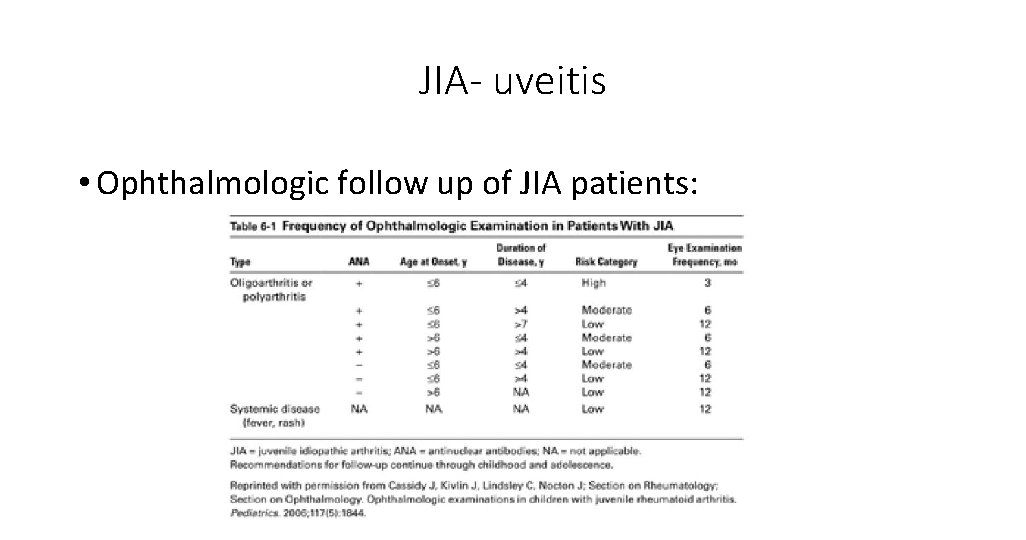
JIA- uveitis • Ophthalmologic follow up of JIA patients:
JIA- uveitis • Treatment: • topical steroids and cycloplegics. • more severe cases require systemic steroids. • prolonged use of steroids can cause growth retardation, cataract and glaucoma. • on the other hand, chronic low grade inflammation is associated with severe ocular morbidity.
JIA- uveitis • Treatment: • systemic IMT should be considered for chronic active uveitis. • weekly low-dose MTX is effective and well tolerated. • recent studies support the use of Adalimumab and biologic agents in addition to MTX for severe disease. Health Technol Assess. 2019 Apr; 23(15): 1 -140. doi: 10. 3310/hta 23150. Adalimumab in combination with methotrexate for refractory uveitis associated with juvenile idiopathic arthritis: a RCT. Ramanan AV et al.
JIA- uveitis • Treatment of cataract: • challenging; lensectomy and vitrectomy via pars plana is advocated. • IOL implantation is controversial (inflammatory complications VS aphakia and amblyopia).
JIA- uveitis • Guidelines for selecting JIA uveitis patients for cataract surgery with IOL implantation: • IMT should be used pre and post operatively with Uveitis well controlled for at least 3 months without using steroids. • acrylic IOL. • close post operative follow up • low threshold for IOL removal if there is persistent post operative inflammation.
JIA- uveitis • Treatment of band keratopathy: • chelation with EDTA. • healing should be allowed before cataract surgery is attempted.
JIA- uveitis • Treatment of glaucoma: • medical therapy is often unsucceful and surgery is often warranted. • standard filtering procedures often fail and the use of antifibrotic drugs or aqueous drainage devices is usually required.

• Objective- to develop recommendations for the screening, monitoring and treatment of JIA associated uveitis.
• Methods • a panel of patients and experts generated key clinical questions to be addressed. • This was followed by a systematic literature review and rating available evidence according to the GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology. • A group consensus process was used to compose the final recommendations and grade their strength as conditional or strong.





• Conclusion- This guideline provides direction for clinicians and patients/parents making decisions on the screening, monitoring, and management of children with JIA and uveitis.

Thank you!
 Hello responses
Hello responses Good afternoon teachers
Good afternoon teachers Tardes buenas tardes
Tardes buenas tardes Morning i see you in the sunrise every morning
Morning i see you in the sunrise every morning Good morning welcome back
Good morning welcome back Good morning class
Good morning class Good night i am glad to see you
Good night i am glad to see you Are you sleeping brother john drawing
Are you sleeping brother john drawing Toxocara
Toxocara Candida uveitis
Candida uveitis Posterior uveitis images
Posterior uveitis images Uveitis
Uveitis Pathophysiology of visual impairment
Pathophysiology of visual impairment Lithimnubólga
Lithimnubólga Ischihara
Ischihara Andrew shannon
Andrew shannon Aqueous flare definition
Aqueous flare definition Uveitis
Uveitis Membreo
Membreo Juvenile rheumatoid arthritis symptoms
Juvenile rheumatoid arthritis symptoms Uvea iris
Uvea iris Hypertensive uveitis
Hypertensive uveitis Eyeritis disease
Eyeritis disease Purulent uveitis
Purulent uveitis Iris ciliary body and choroid
Iris ciliary body and choroid Seclusio pupillae diagram
Seclusio pupillae diagram Uveitis
Uveitis Sinequias uveitis
Sinequias uveitis Boon lay garden primary school logo
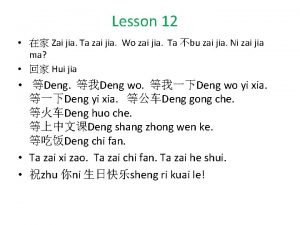
Boon lay garden primary school logo Ni jia you ji ge ren in english
Ni jia you ji ge ren in english Ye qiu
Ye qiu