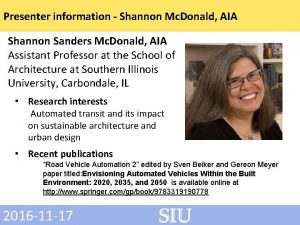
ED SlitLamp Examination Andrew Shannon MD MPH Department

- Slides: 23
ED Slit-Lamp Examination Andrew Shannon, MD MPH Department of Emergency Medicine Jacobi Medical Center
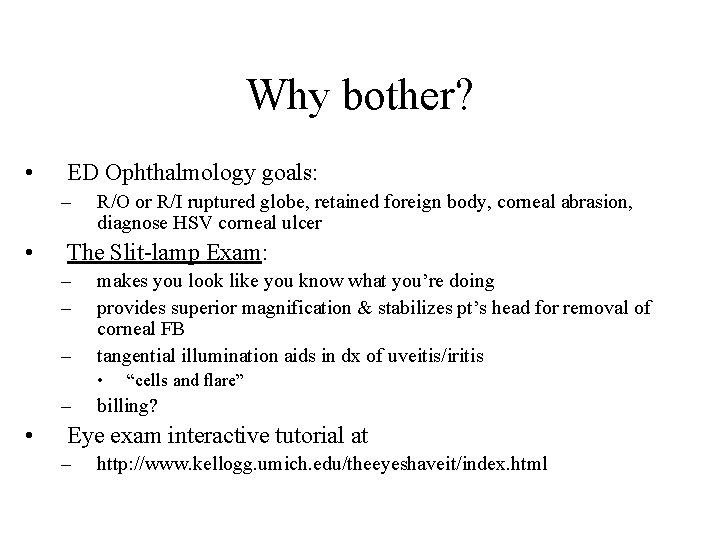
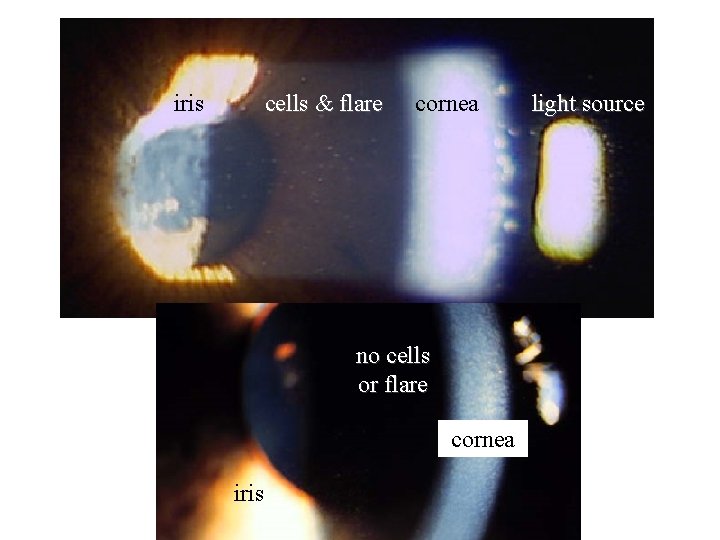
Why bother? • ED Ophthalmology goals: – • R/O or R/I ruptured globe, retained foreign body, corneal abrasion, diagnose HSV corneal ulcer The Slit-lamp Exam: – – – makes you look like you know what you’re doing provides superior magnification & stabilizes pt’s head for removal of corneal FB tangential illumination aids in dx of uveitis/iritis • – • “cells and flare” billing? Eye exam interactive tutorial at – http: //www. kellogg. umich. edu/theeyeshaveit/index. html
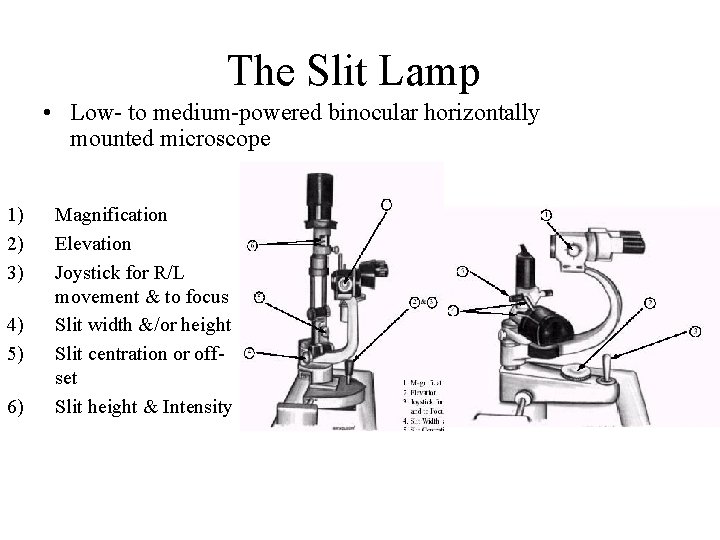
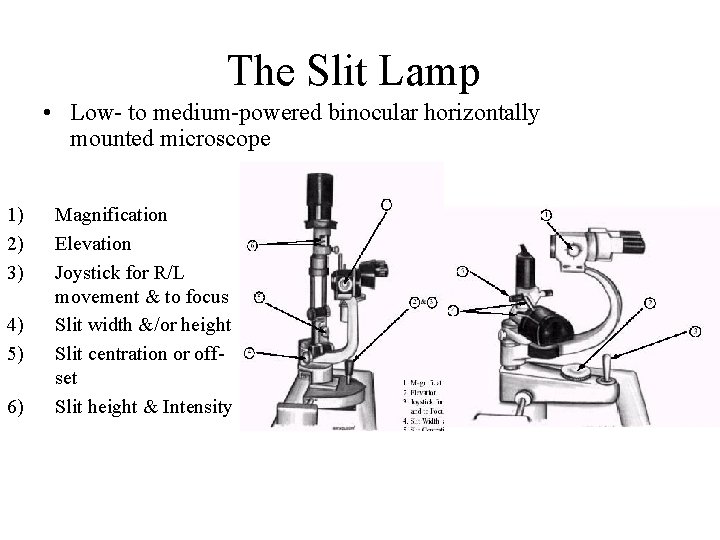
The Slit Lamp • Low- to medium-powered binocular horizontally mounted microscope 1) 2) 3) 4) 5) 6) Magnification Elevation Joystick for R/L movement & to focus Slit width &/or height Slit centration or offset Slit height & Intensity
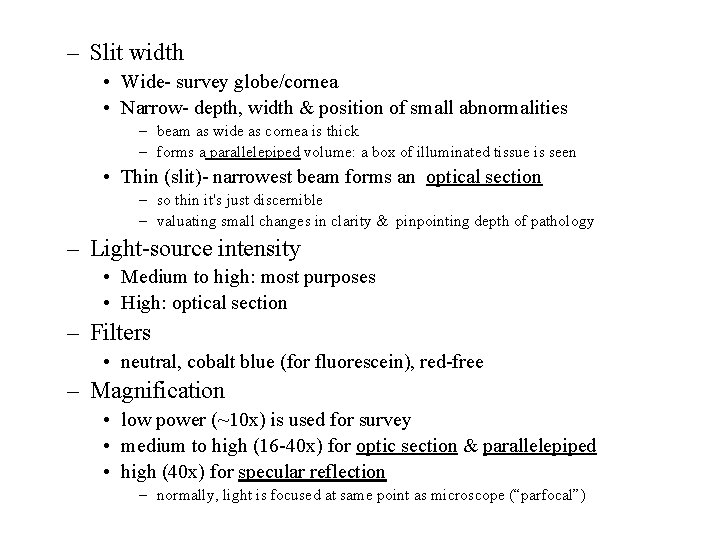
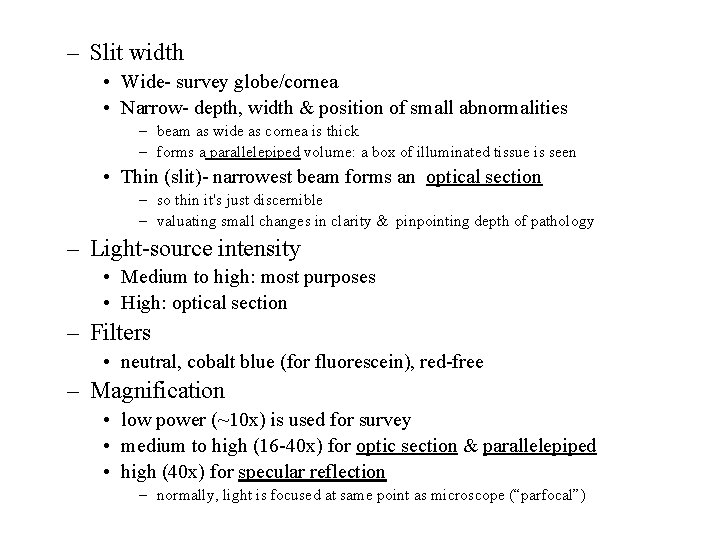
– Slit width • Wide- survey globe/cornea • Narrow- depth, width & position of small abnormalities – beam as wide as cornea is thick – forms a parallelepiped volume: a box of illuminated tissue is seen • Thin (slit)- narrowest beam forms an optical section – so thin it's just discernible – valuating small changes in clarity & pinpointing depth of pathology – Light-source intensity • Medium to high: most purposes • High: optical section – Filters • neutral, cobalt blue (for fluorescein), red-free – Magnification • low power (~10 x) is used for survey • medium to high (16 -40 x) for optic section & parallelepiped • high (40 x) for specular reflection – normally, light is focused at same point as microscope (“parfocal”)
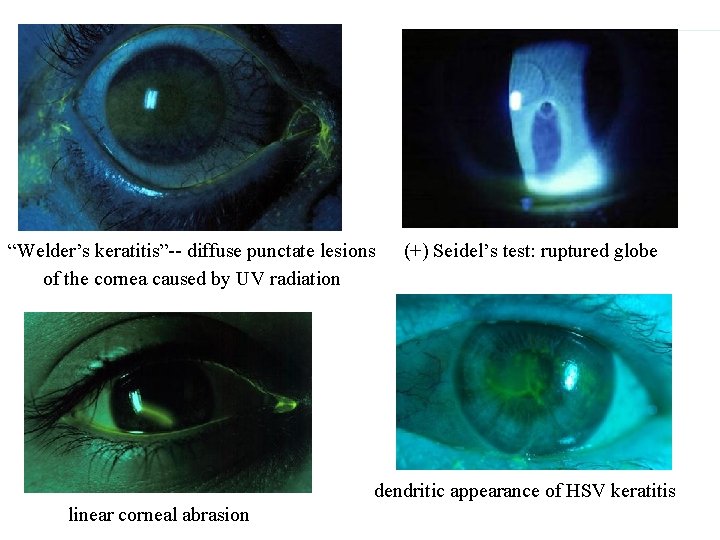
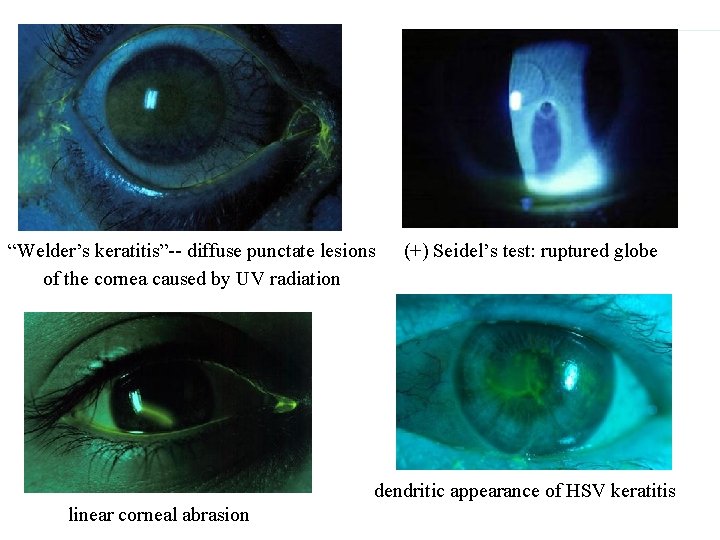
“Welder’s keratitis”-- diffuse punctate lesions of the cornea caused by UV radiation (+) Seidel’s test: ruptured globe dendritic appearance of HSV keratitis linear corneal abrasion

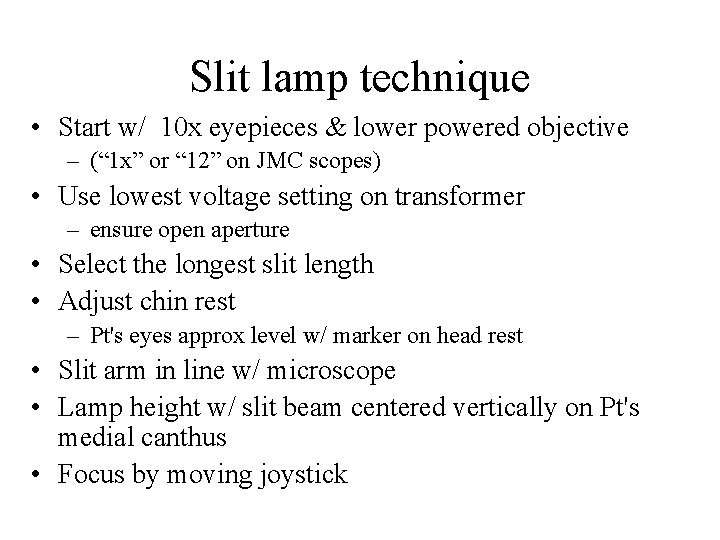
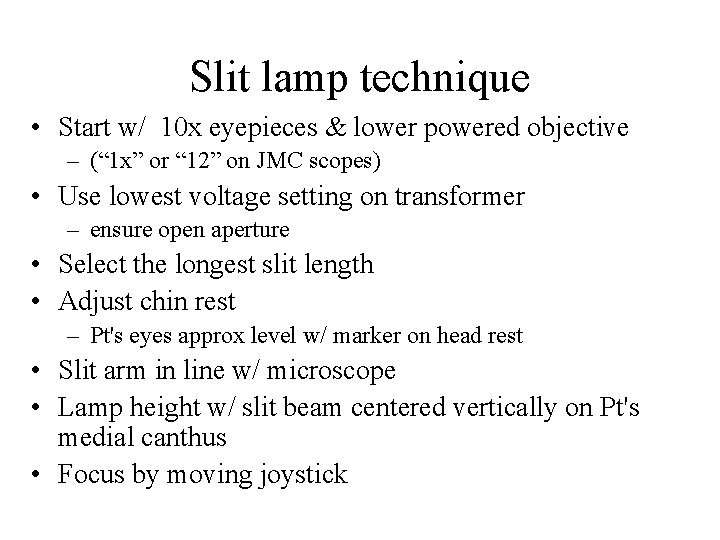
Slit lamp technique • Start w/ 10 x eyepieces & lower powered objective – (“ 1 x” or “ 12” on JMC scopes) • Use lowest voltage setting on transformer – ensure open aperture • Select the longest slit length • Adjust chin rest – Pt's eyes approx level w/ marker on head rest • Slit arm in line w/ microscope • Lamp height w/ slit beam centered vertically on Pt's medial canthus • Focus by moving joystick
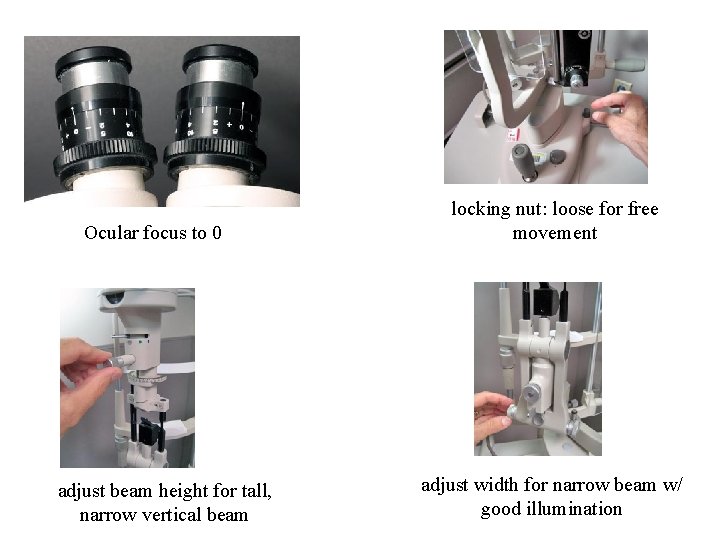
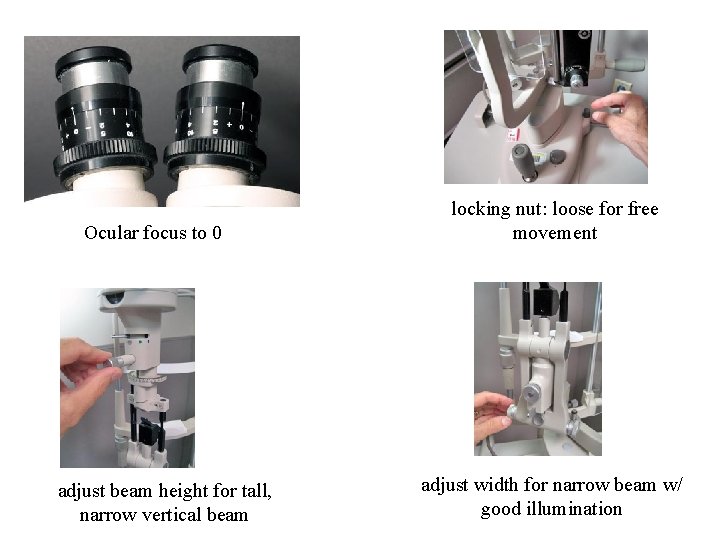
Ocular focus to 0 adjust beam height for tall, narrow vertical beam locking nut: loose for free movement adjust width for narrow beam w/ good illumination
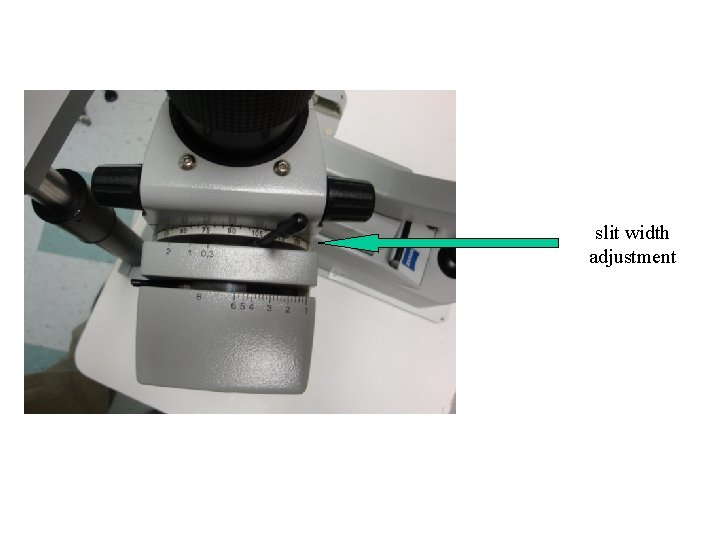
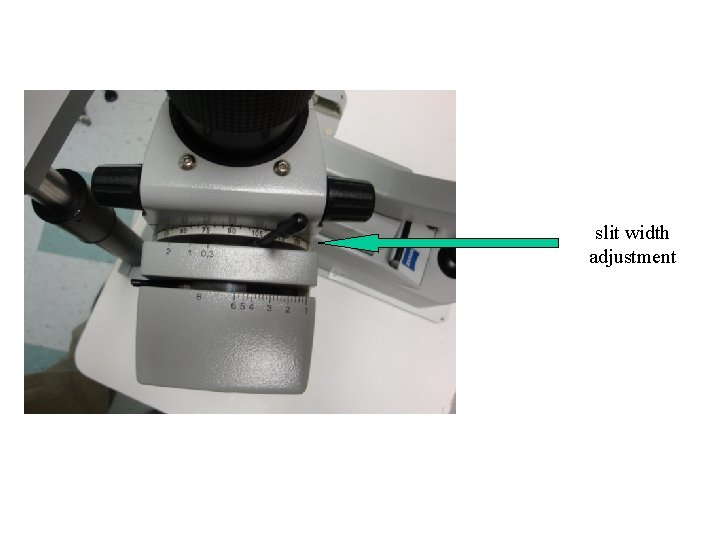
slit width adjustment
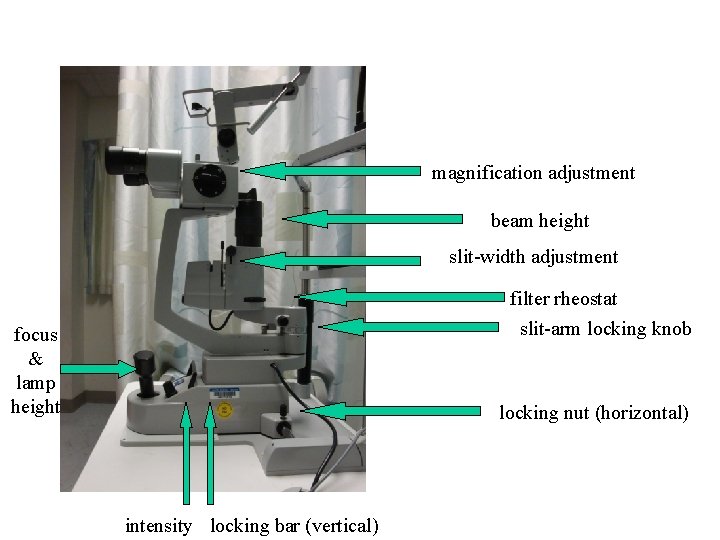
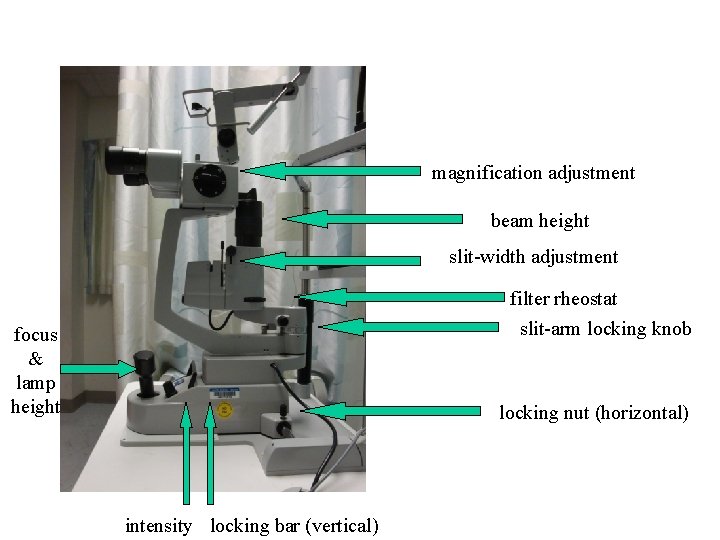
magnification adjustment beam height slit-width adjustment filter rheostat slit-arm locking knob focus & lamp height locking nut (horizontal) intensity locking bar (vertical)
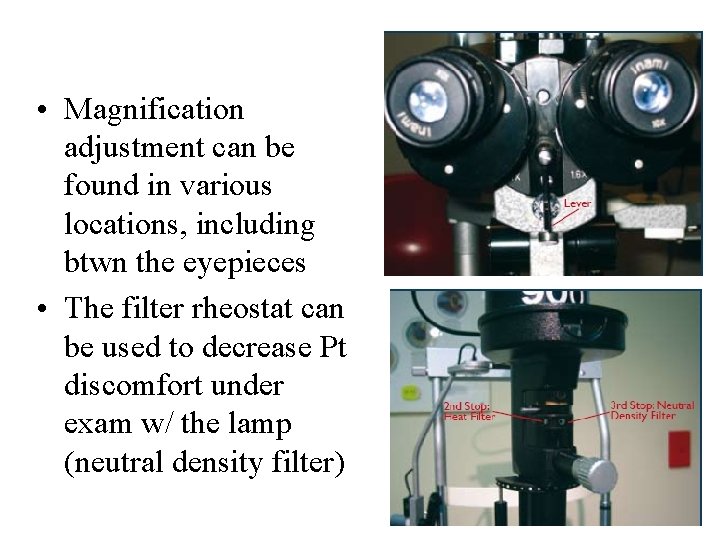
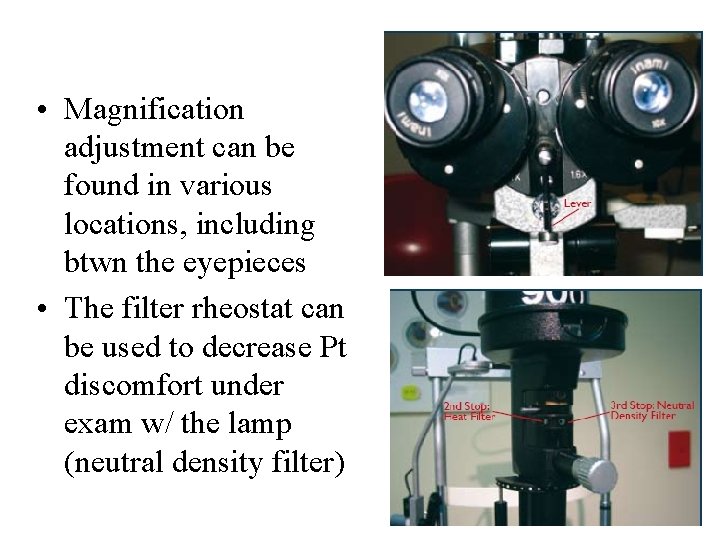
• Magnification adjustment can be found in various locations, including btwn the eyepieces • The filter rheostat can be used to decrease Pt discomfort under exam w/ the lamp (neutral density filter)
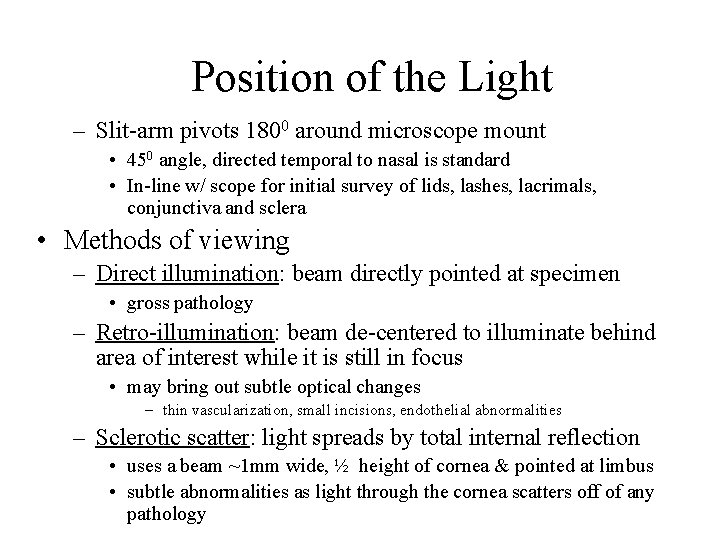
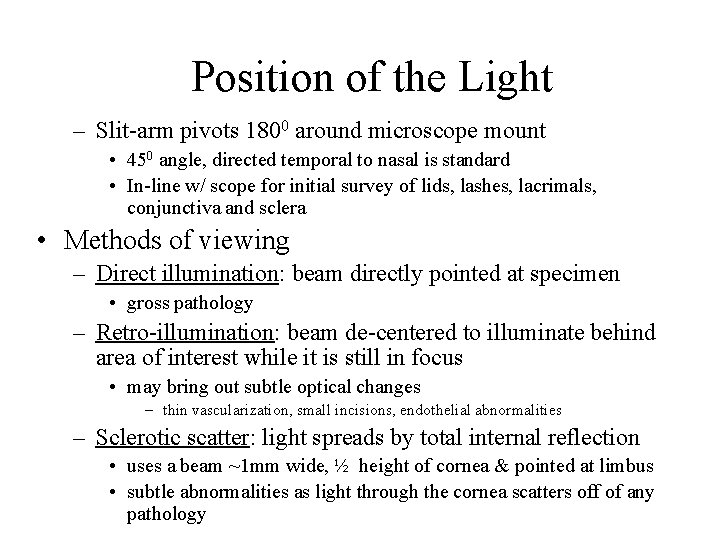
Position of the Light – Slit-arm pivots 1800 around microscope mount • 450 angle, directed temporal to nasal is standard • In-line w/ scope for initial survey of lids, lashes, lacrimals, conjunctiva and sclera • Methods of viewing – Direct illumination: beam directly pointed at specimen • gross pathology – Retro-illumination: beam de-centered to illuminate behind area of interest while it is still in focus • may bring out subtle optical changes – thin vascularization, small incisions, endothelial abnormalities – Sclerotic scatter: light spreads by total internal reflection • uses a beam ~1 mm wide, ½ height of cornea & pointed at limbus • subtle abnormalities as light through the cornea scatters off of any pathology
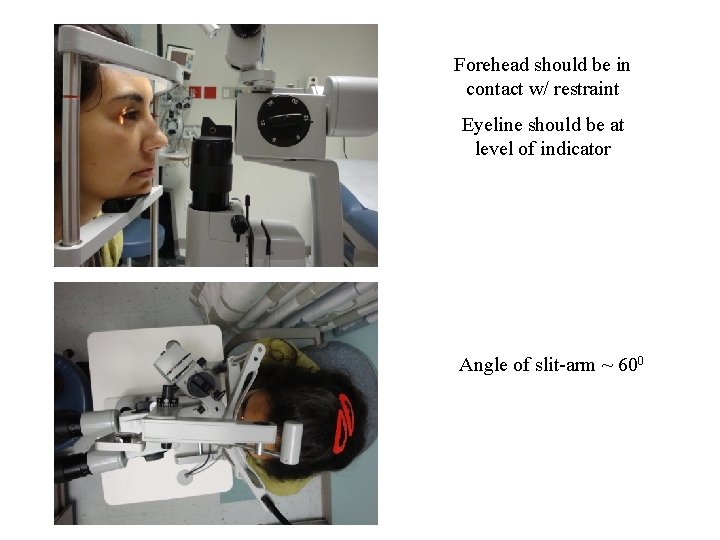
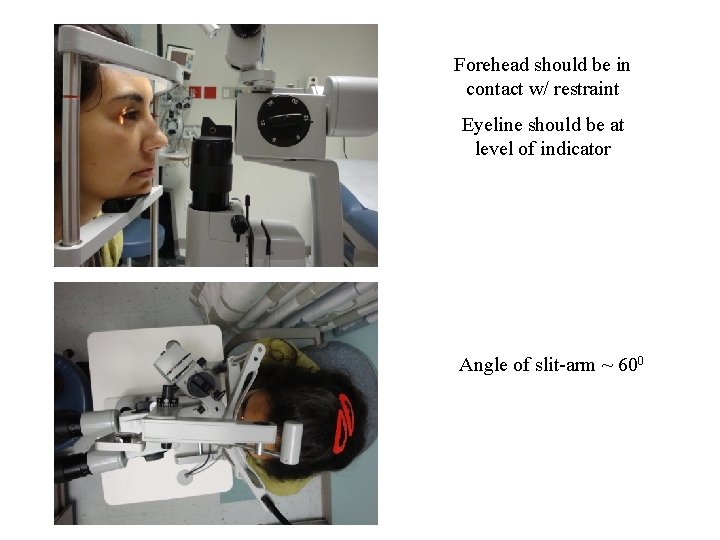
Forehead should be in contact w/ restraint Eyeline should be at level of indicator Angle of slit-arm ~ 600
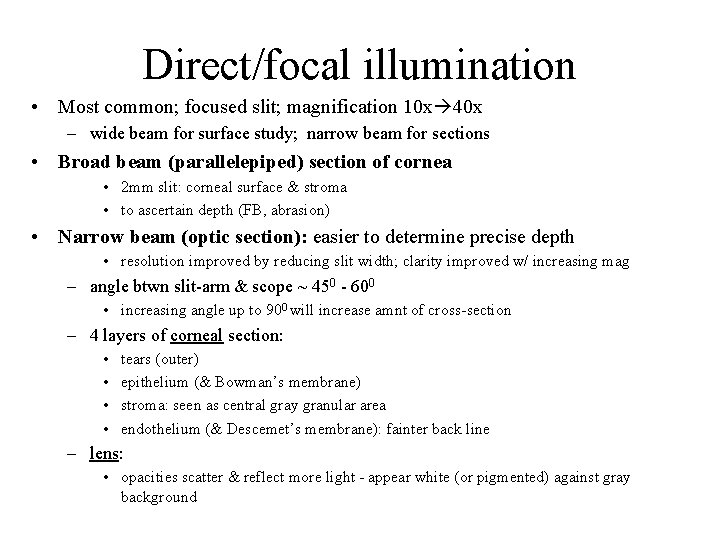
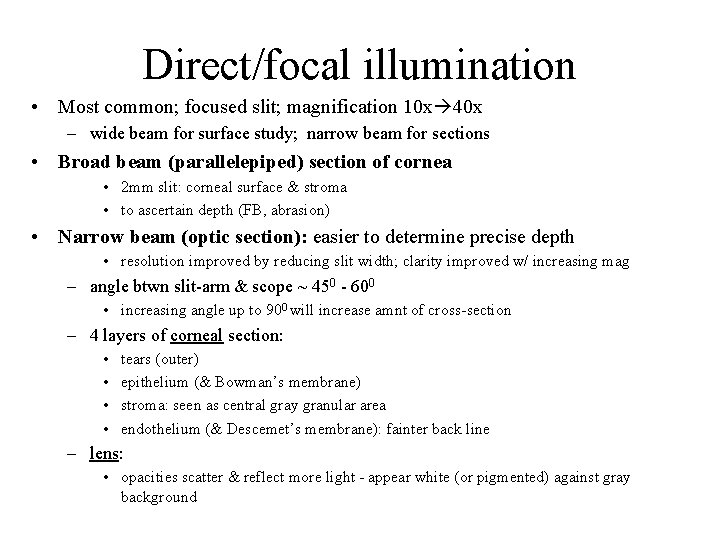
Direct/focal illumination • Most common; focused slit; magnification 10 x 40 x – wide beam for surface study; narrow beam for sections • Broad beam (parallelepiped) section of cornea • 2 mm slit: corneal surface & stroma • to ascertain depth (FB, abrasion) • Narrow beam (optic section): easier to determine precise depth • resolution improved by reducing slit width; clarity improved w/ increasing mag – angle btwn slit-arm & scope ~ 450 - 600 • increasing angle up to 900 will increase amnt of cross-section – 4 layers of corneal section: • • tears (outer) epithelium (& Bowman’s membrane) stroma: seen as central gray granular area endothelium (& Descemet’s membrane): fainter back line – lens: • opacities scatter & reflect more light - appear white (or pigmented) against gray background
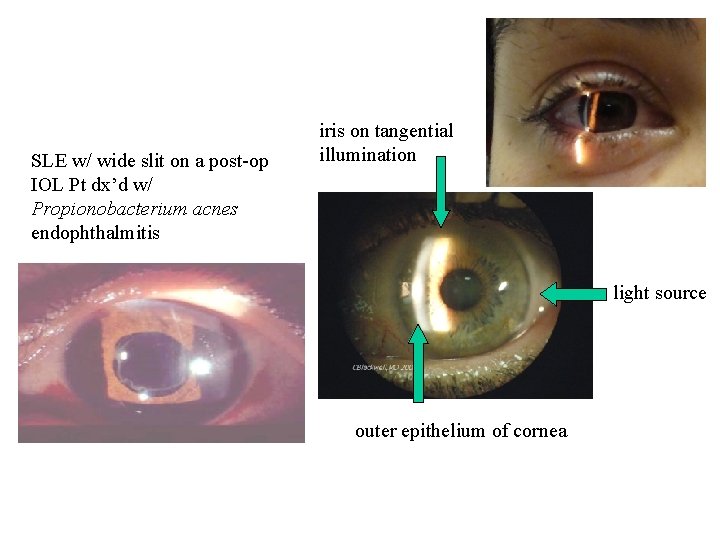
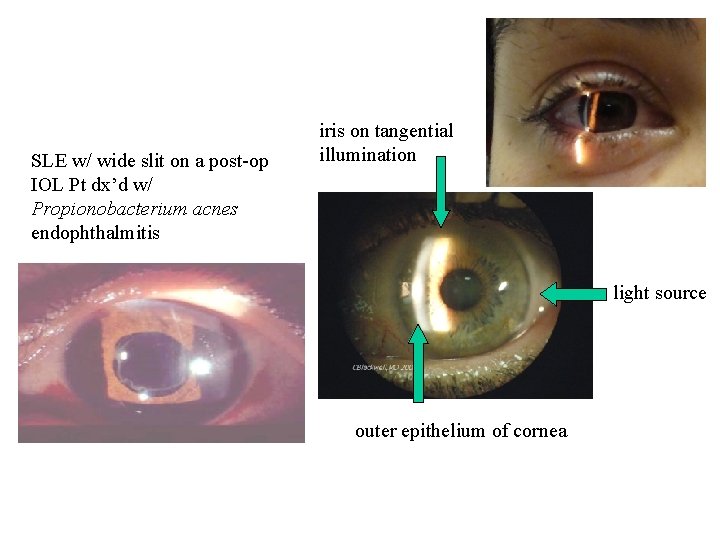
SLE w/ wide slit on a post-op IOL Pt dx’d w/ Propionobacterium acnes endophthalmitis iris on tangential illumination light source outer epithelium of cornea
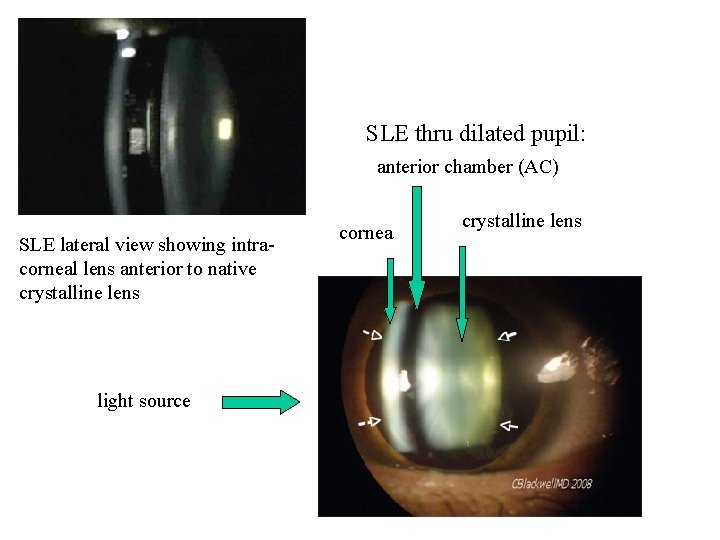
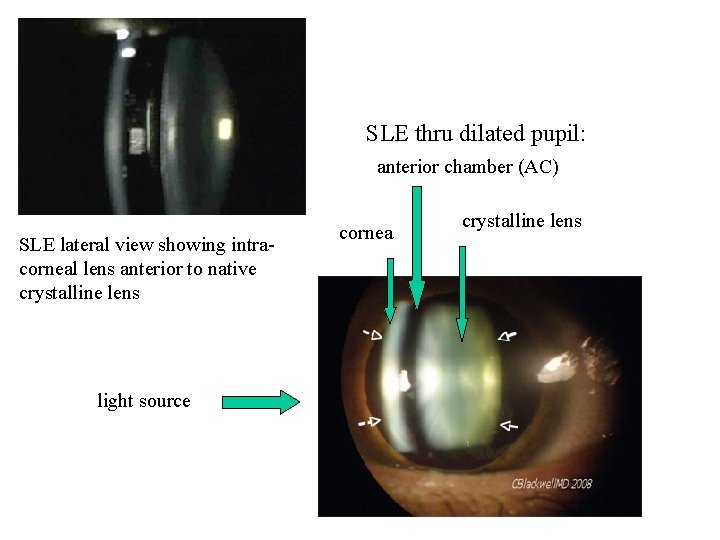
SLE thru dilated pupil: anterior chamber (AC) SLE lateral view showing intracorneal lens anterior to native crystalline lens light source cornea crystalline lens
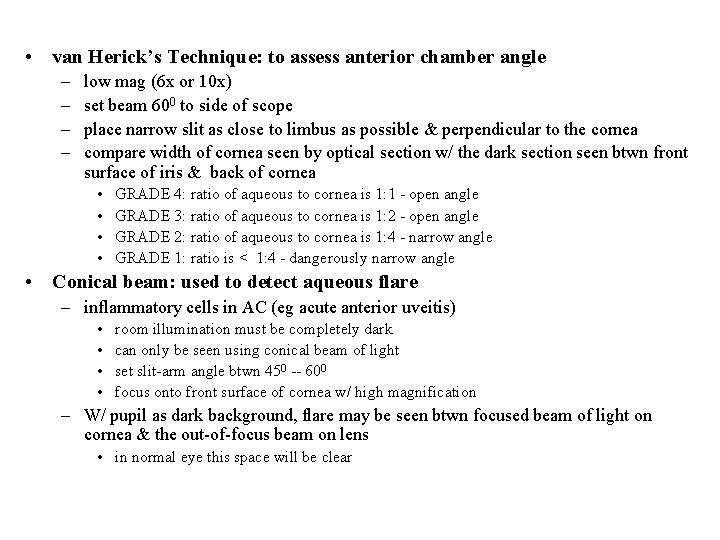
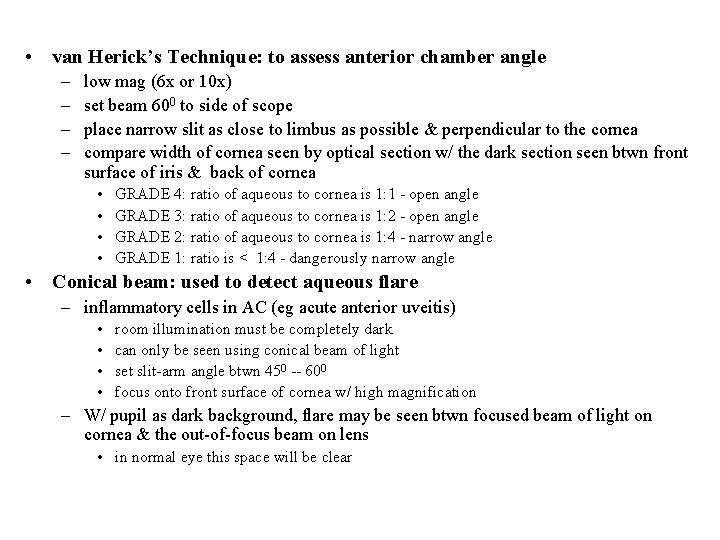
• van Herick’s Technique: to assess anterior chamber angle – – low mag (6 x or 10 x) set beam 600 to side of scope place narrow slit as close to limbus as possible & perpendicular to the cornea compare width of cornea seen by optical section w/ the dark section seen btwn front surface of iris & back of cornea • • GRADE 4: ratio of aqueous to cornea is 1: 1 - open angle GRADE 3: ratio of aqueous to cornea is 1: 2 - open angle GRADE 2: ratio of aqueous to cornea is 1: 4 - narrow angle GRADE 1: ratio is < 1: 4 - dangerously narrow angle • Conical beam: used to detect aqueous flare – inflammatory cells in AC (eg acute anterior uveitis) • • room illumination must be completely dark can only be seen using conical beam of light set slit-arm angle btwn 450 -- 600 focus onto front surface of cornea w/ high magnification – W/ pupil as dark background, flare may be seen btwn focused beam of light on cornea & the out-of-focus beam on lens • in normal eye this space will be clear
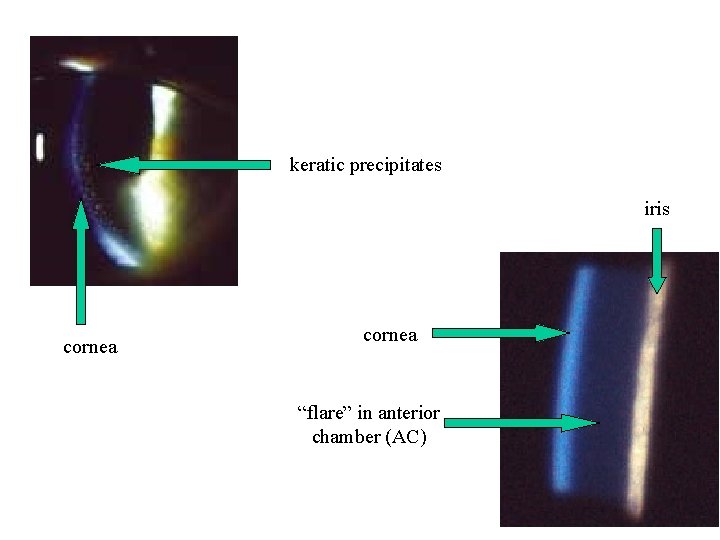
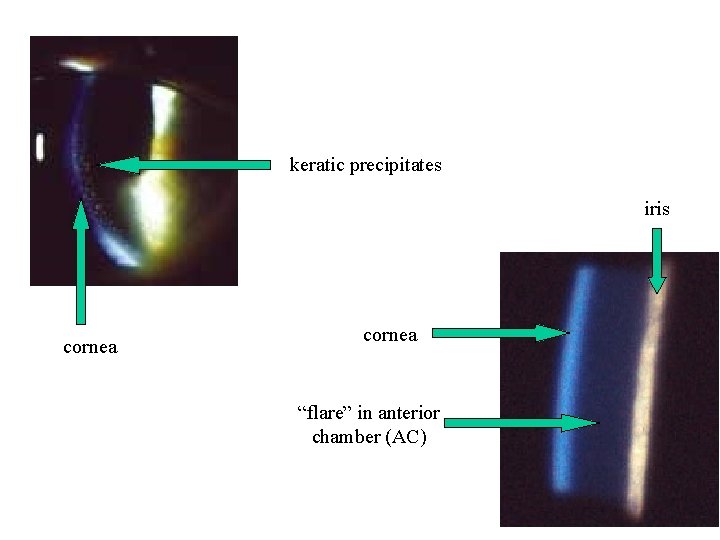
keratic precipitates iris cornea “flare” in anterior chamber (AC)
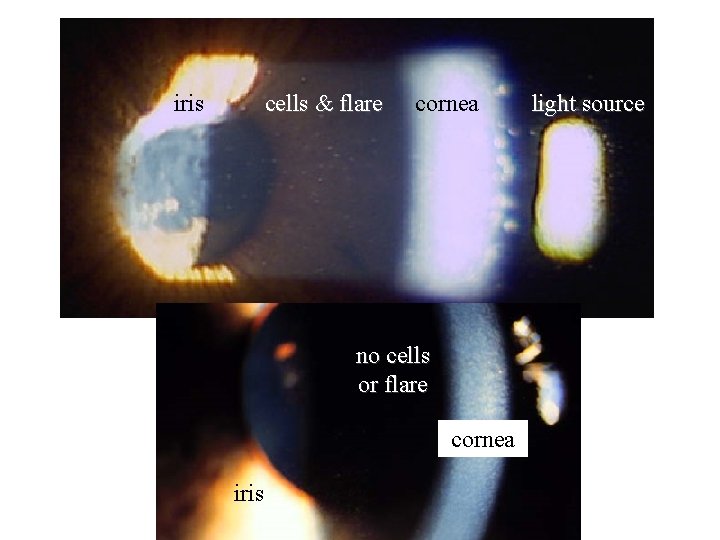
iris cells & flare cornea no cells or flare cornea iris light source
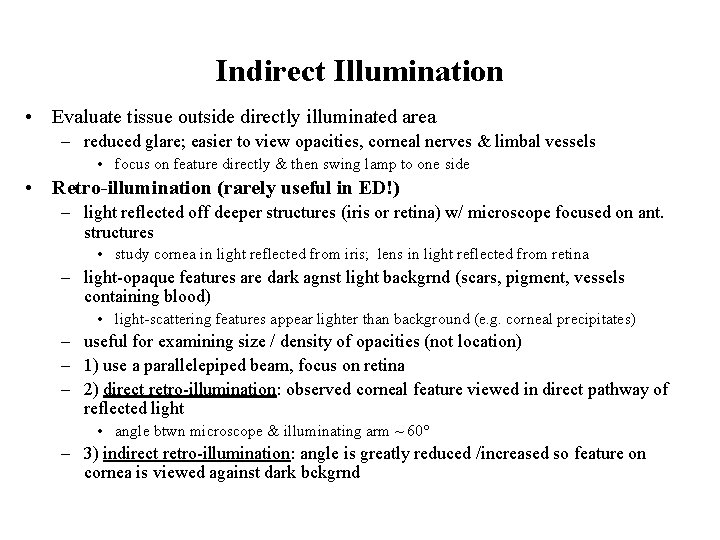
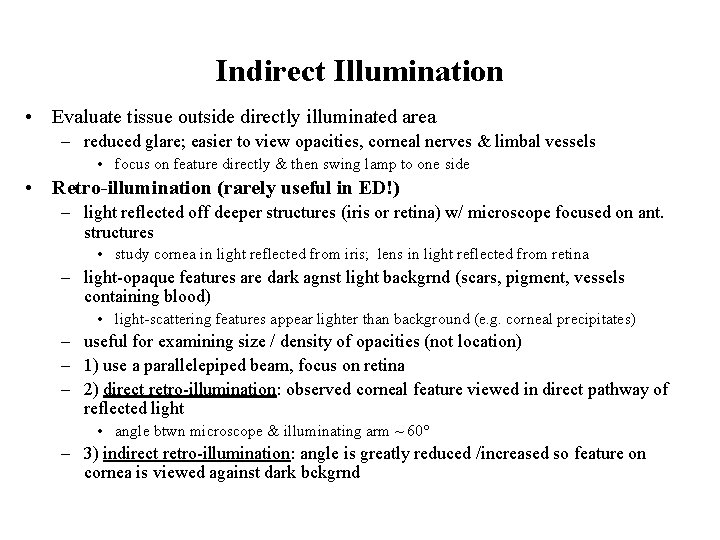
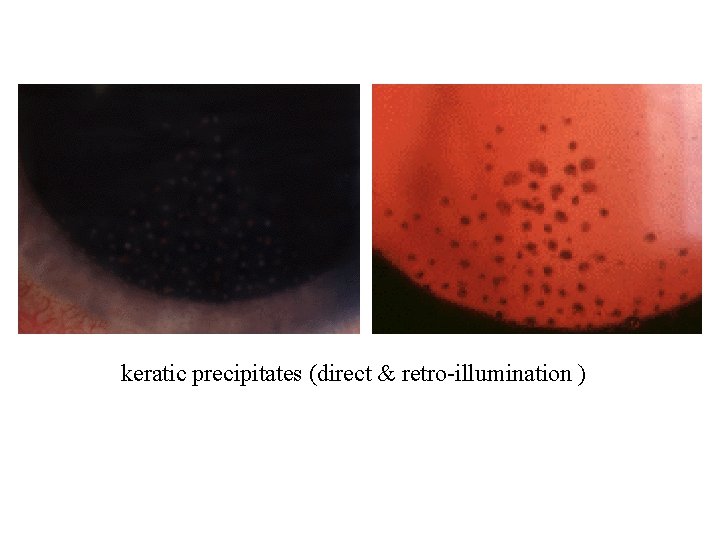
Indirect Illumination • Evaluate tissue outside directly illuminated area – reduced glare; easier to view opacities, corneal nerves & limbal vessels • focus on feature directly & then swing lamp to one side • Retro-illumination (rarely useful in ED!) – light reflected off deeper structures (iris or retina) w/ microscope focused on ant. structures • study cornea in light reflected from iris; lens in light reflected from retina – light-opaque features are dark agnst light backgrnd (scars, pigment, vessels containing blood) • light-scattering features appear lighter than background (e. g. corneal precipitates) – useful for examining size / density of opacities (not location) – 1) use a parallelepiped beam, focus on retina – 2) direct retro-illumination: observed corneal feature viewed in direct pathway of reflected light • angle btwn microscope & illuminating arm ~ 60° – 3) indirect retro-illumination: angle is greatly reduced /increased so feature on cornea is viewed against dark bckgrnd
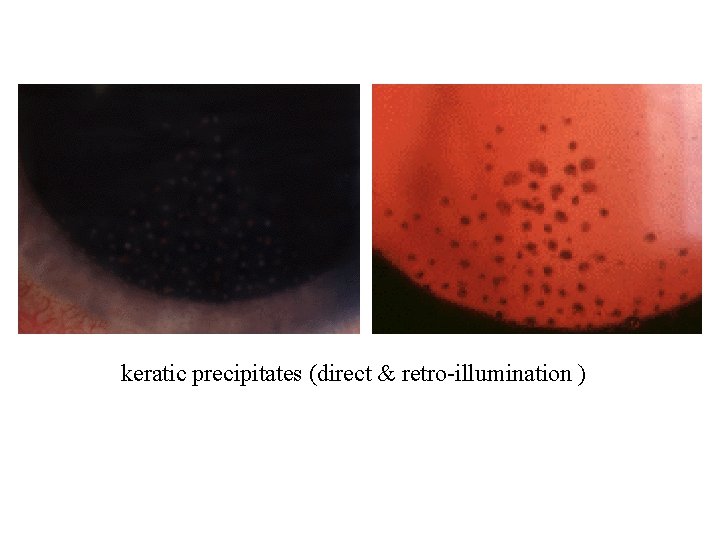
keratic precipitates (direct & retro-illumination )
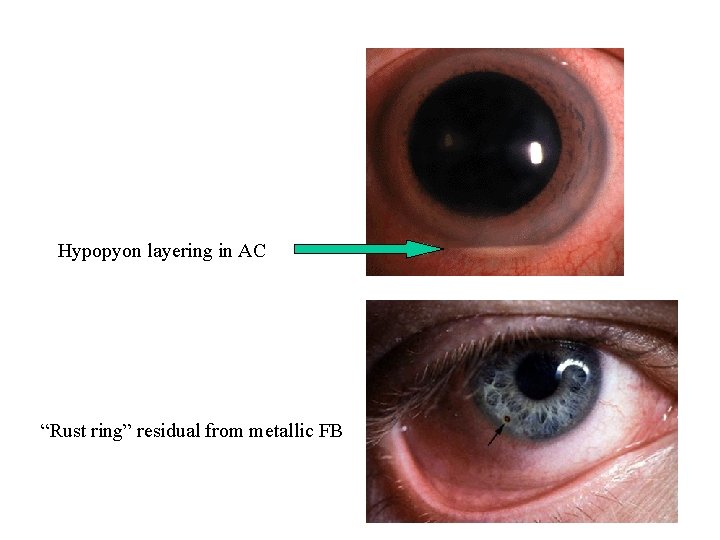
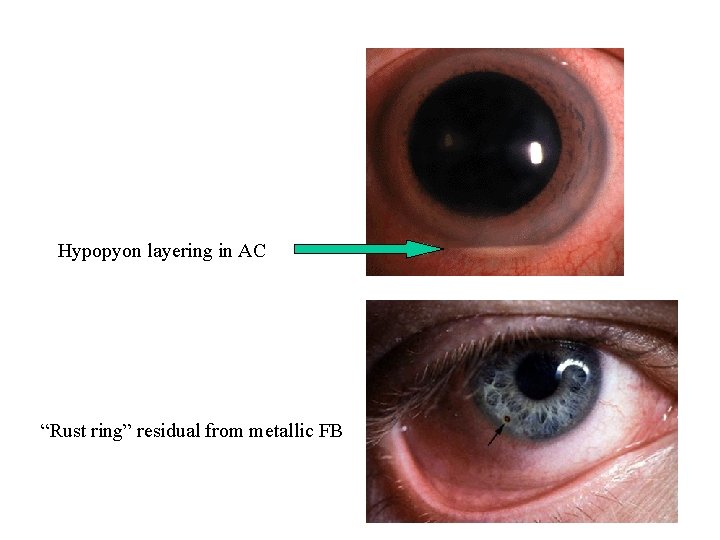
Hypopyon layering in AC “Rust ring” residual from metallic FB
References: • • • My Hanh Nguyen. Ophthalmology Grand Rounds. Tufts Unviersity. http: //ocw. tufts. edu/Content/37/topics/487903/488024. Content accessed 9/23/08. Introduction to Slit Lamp Technique. CYBER-SIGHT: Copyright © 2003 Project ORBIS International Inc. http: //www. cybersight. org/bins/content_page. asp? cid=1 -1581 -1604. Content accessed 9/23/08. G Papaliodis. Propionibacterium acnes Endophthalmitis. Ocular Immunology and Uveitis Foundation. Massachusetts Eeye Research and Surgery Institution. Copyright © 1996 -2008 C. Stephen Foster M. D. http: //www. uveitis. org/medical/articles/case/P_acnes. html. Content accessed 9/23/08. Vance Thompson. Postoperative Care for Phakic Intraocular Lens Implants. In: Phakic Intraocular Lenses: Principles and Practice by Hardten, Lindstrom, and Davis. Slack, Inc. www. slackbooks. com/excerpts/66402. asp. Content accessed 9/23/08. Jared Schultz. One intracorneal segment treats keratoconus better than two. Copyright 2008 SLACK Inc. , www. osnsupersite. com/view. asp? r. ID=23456. Content accessed 9/23/08. Craig Blackwell. Narrated Eye Exam: Copyright 2008. www. blackwelleyesight. com/narrated-eye-exam/. Content accessed 9/23/08. Patient Glossary. Ocular Immunology and Uveitis Foundation. Massachusetts Eeye Research and Surgery Institution. Copyright © 1996 -2008 C. Stephen Foster M. D. http: //www. uveitis. org/patient/glossary/a_f. html. Content accessed 9/23/08. JG O'Shea, DA Infeld, RB Harvey. Uveitis- a photoessay. http: //medweb. bham. ac. uk/easdec/eyetextbook/Uveitis/uveitis. htm. Content accessed on 9/23/08. Second Year 99/00: Clinical Optometry 3. Slit lamp examination: Practical. http: //www. academy. org. uk/lectures/eperjesi 5. htm. Content accessed 9/23/08. KJ Knoop. Slit-lamp exam. Uptodate. com. Last updated: February 12, 2008. http: //www. uptodateonline. com/online/content/topic. do? topic. Key=ad_proc/2391&selected. Title=1~61&sou rce=search_result. Content accessed 9/23/08.
 Slit lamp parts
Slit lamp parts Uveitis
Uveitis 75 miles per hour to km
75 miles per hour to km Public health monash
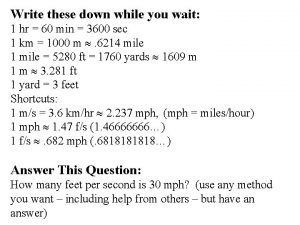
Public health monash 40 mph to ft/s
40 mph to ft/s Melody hou md mph
Melody hou md mph 75 mph to ft/s
75 mph to ft/s A&m md mph
A&m md mph Umass online mph
Umass online mph Webste
Webste Utep mph
Utep mph James fraser ucsf
James fraser ucsf Dr. meyers dorsten erfahrungen
Dr. meyers dorsten erfahrungen How fast does light travel
How fast does light travel Mph drug
Mph drug F/s to mph
F/s to mph 451 kts to mph
451 kts to mph Mudr. tomáš kampe mph
Mudr. tomáš kampe mph Drexel executive mph
Drexel executive mph Disease adalah
Disease adalah Mph rules
Mph rules Beverly loudin md mph
Beverly loudin md mph Edgar figueroa md mph
Edgar figueroa md mph University of montana mph
University of montana mph