IVF pregnancy Will the risk never end Dr




- Slides: 29

IVF pregnancy: Will the risk never end? Dr Karen Paice MBBS FRANZCOG Obstetrician and Fertility Specialist High and Low risk Obstetrics Private Obstetrics - St Vincent’s Private - Epworth Freemason’s Hospital Melbourne IVF

About me Private Rooms 145 Victoria Parade Fitzroy 3065 9419 5757 Public Appointment Mercy Hospital for Women – Consultant Obstetrician The Women’s Hospital - Reproductive Services https: //www. drkarenpaice. com. au/
Take home messages Aspirin? • IVF • Third trimester growth scan
In Vitro Fertilisation (IVF) IVF- In-Vitro Fertilisation ICSI - Intracytoplasmic Sperm Injection
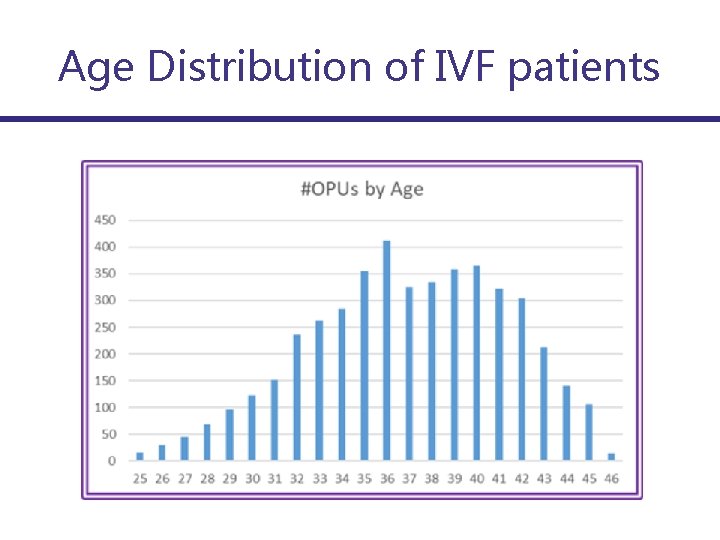
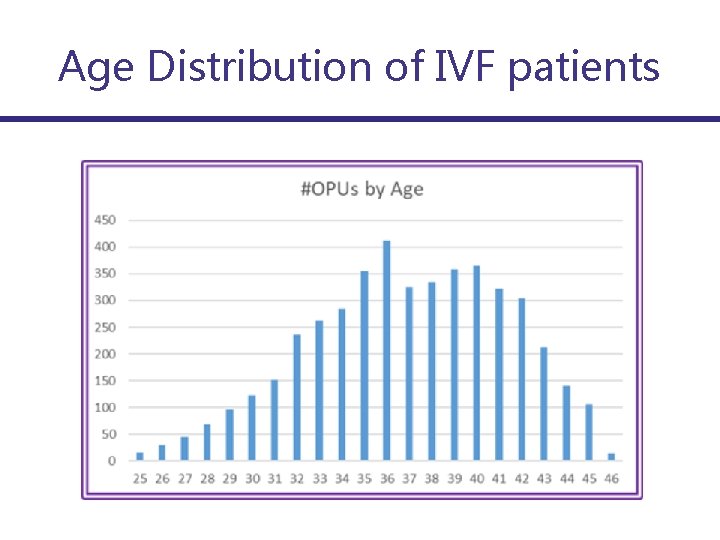
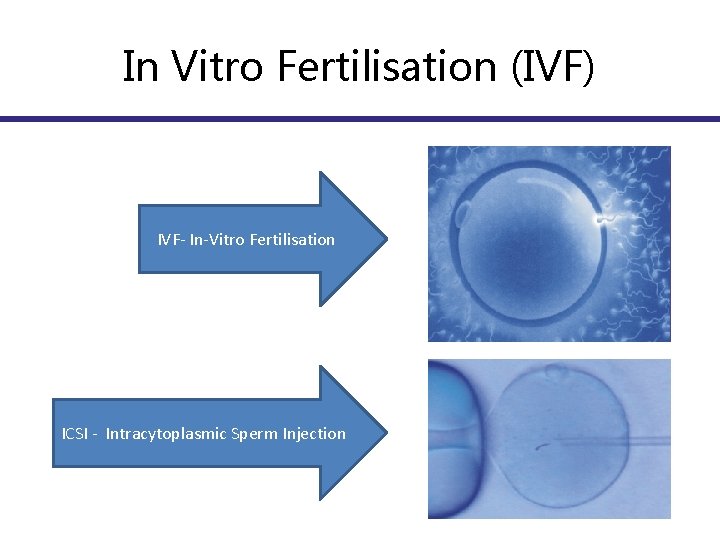
Age Distribution of IVF patients
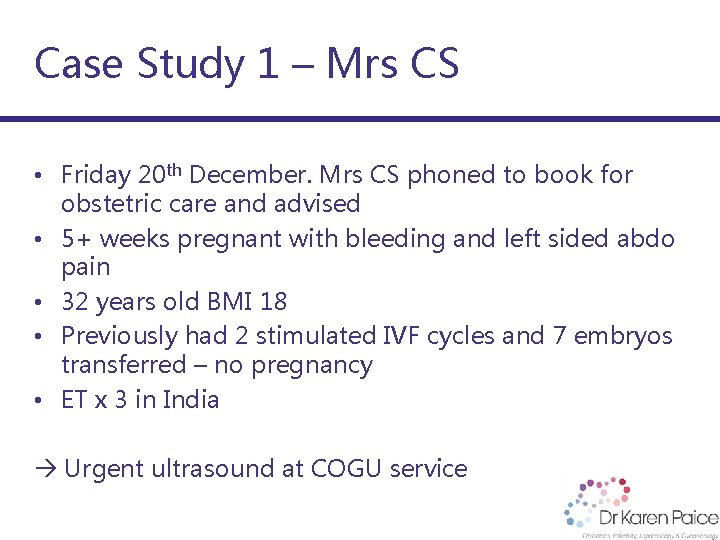
Case Study 1 – Mrs CS • Friday 20 th December. Mrs CS phoned to book for obstetric care and advised • 5+ weeks pregnant with bleeding and left sided abdo pain • 32 years old BMI 18 • Previously had 2 stimulated IVF cycles and 7 embryos transferred – no pregnancy • ET x 3 in India Urgent ultrasound at COGU service
Case Study 1 – Mrs CS Date of examination: 20/12/2013 Indication: Early pregnancy: IVF pregnancy - India 3 x ET. Left pain and bleeding. EDD by conception date: 17 August 2014. Gestational age: 5 weeks + 5 days. Early Pregnancy Assessment: Gestational Sac: present. Embryo present. Fetal heart action present. Gestational Sac (Mean) 6. 4 mm Yolk Sac (Mean) 3. 8 mm Diagnosis based on ultrasound findings: intrauterine sac seen but too early to see a fetus. There is also a small ectopic pregnancy central and posterior - probably on the left It has a small 4 mm sac and yolk sac seen within a small mass measuring 31 x 18 x 28 mm in size Diagnosis: Heterotopic pregnancy - normal intrauterine and left ectopic pregnancy.
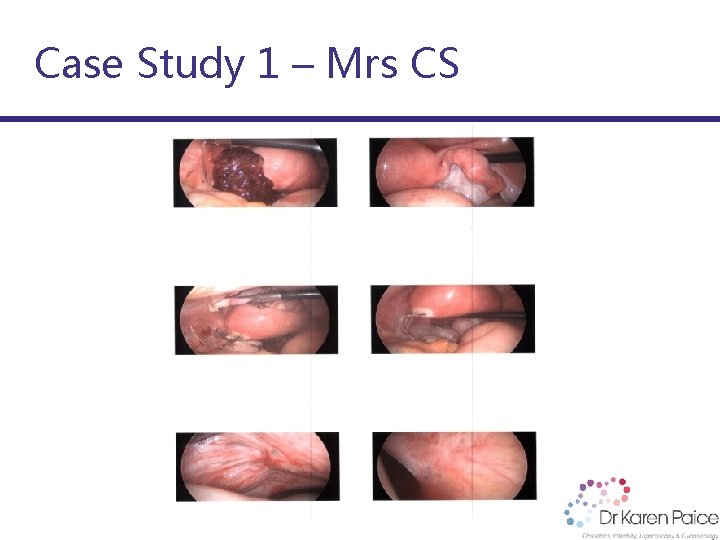
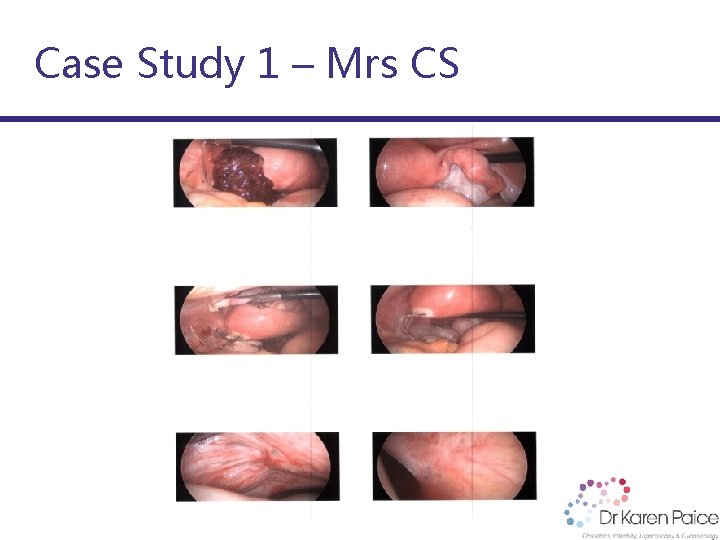
Case Study 1 – Mrs CS
Case study 1 Mrs CS Antenatally well Low risk combined screening Normal 20 week ultrasound Fundus equalled dates throughout 34 week growth scan EFW 35 th centile Mrs CS requested a planned Caesarean section • 39+2 Myra 2750 gm • • •
Case Study 1 – Mrs CS
Case Study 2 – Stephanie • 34 year old presented with 12 months of Unexplained Infertility BMI 20 • Declined a laparoscopy Declined IUI requested to proceed directly to IVF • Conceived with second embryo transfer PMHx Ø Migraines Ø Hayfever • Uncomplicated antenatal course. Fundus equalled dates • 34 week growth ultrasound
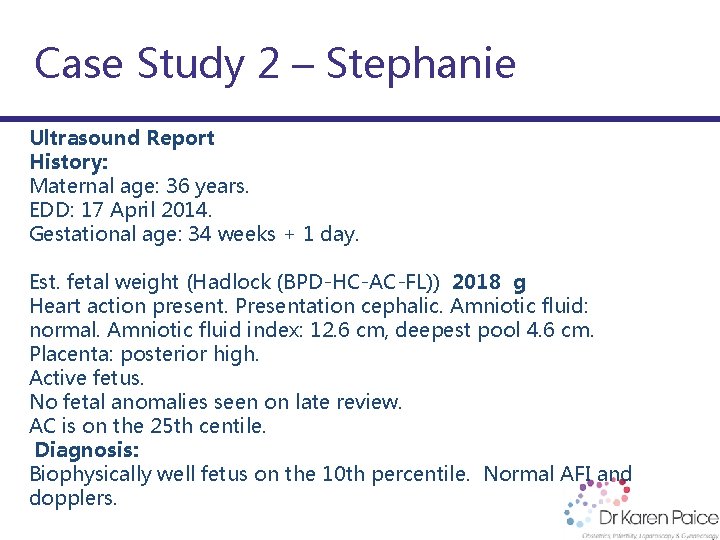
Case Study 2 – Stephanie Ultrasound Report History: Maternal age: 36 years. EDD: 17 April 2014. Gestational age: 34 weeks + 1 day. Est. fetal weight (Hadlock (BPD-HC-AC-FL)) 2018 g Heart action present. Presentation cephalic. Amniotic fluid: normal. Amniotic fluid index: 12. 6 cm, deepest pool 4. 6 cm. Placenta: posterior high. Active fetus. No fetal anomalies seen on late review. AC is on the 25 th centile. Diagnosis: Biophysically well fetus on the 10 th percentile. Normal AFI and dopplers.
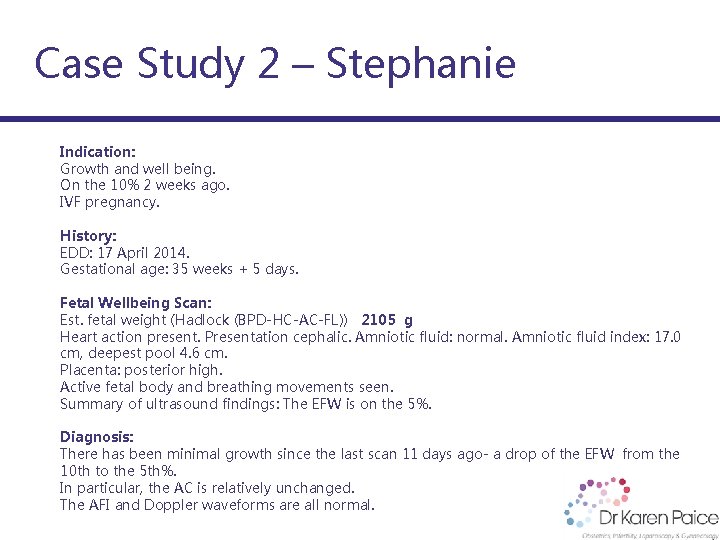
Case Study 2 – Stephanie Indication: Growth and well being. On the 10% 2 weeks ago. IVF pregnancy. History: EDD: 17 April 2014. Gestational age: 35 weeks + 5 days. Fetal Wellbeing Scan: Est. fetal weight (Hadlock (BPD-HC-AC-FL)) 2105 g Heart action present. Presentation cephalic. Amniotic fluid: normal. Amniotic fluid index: 17. 0 cm, deepest pool 4. 6 cm. Placenta: posterior high. Active fetal body and breathing movements seen. Summary of ultrasound findings: The EFW is on the 5%. Diagnosis: There has been minimal growth since the last scan 11 days ago- a drop of the EFW from the 10 th to the 5 th%. In particular, the AC is relatively unchanged. The AFI and Doppler waveforms are all normal.
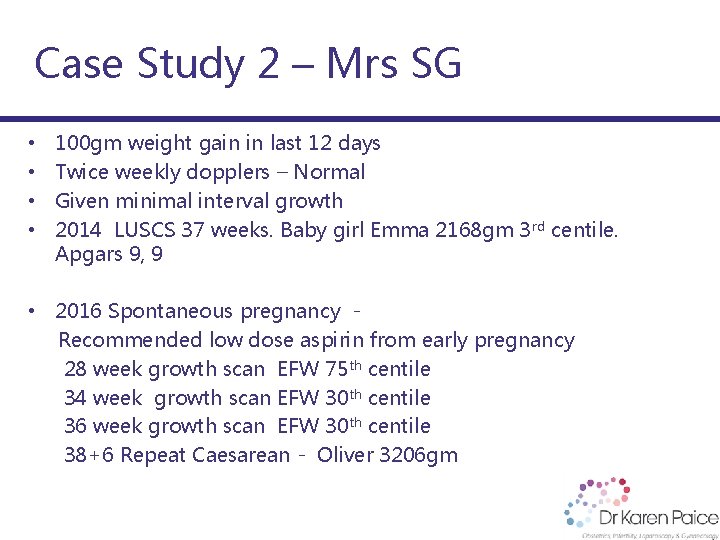
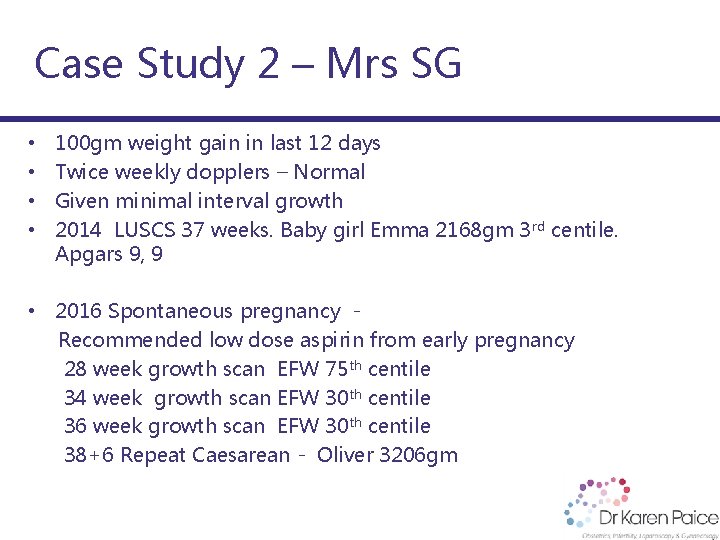
Case Study 2 – Mrs SG • • 100 gm weight gain in last 12 days Twice weekly dopplers – Normal Given minimal interval growth 2014 LUSCS 37 weeks. Baby girl Emma 2168 gm 3 rd centile. Apgars 9, 9 • 2016 Spontaneous pregnancy Recommended low dose aspirin from early pregnancy 28 week growth scan EFW 75 th centile 34 week growth scan EFW 30 th centile 36 week growth scan EFW 30 th centile 38+6 Repeat Caesarean - Oliver 3206 gm
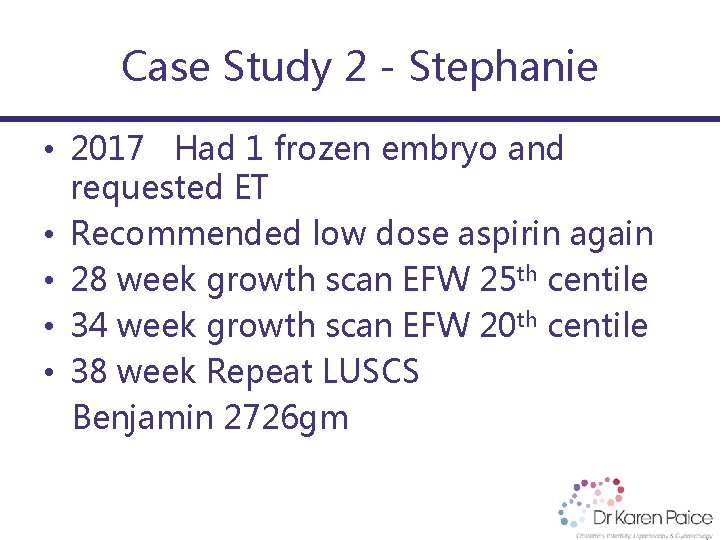
Case Study 2 - Stephanie • 2017 Had 1 frozen embryo and requested ET • Recommended low dose aspirin again • 28 week growth scan EFW 25 th centile • 34 week growth scan EFW 20 th centile • 38 week Repeat LUSCS Benjamin 2726 gm
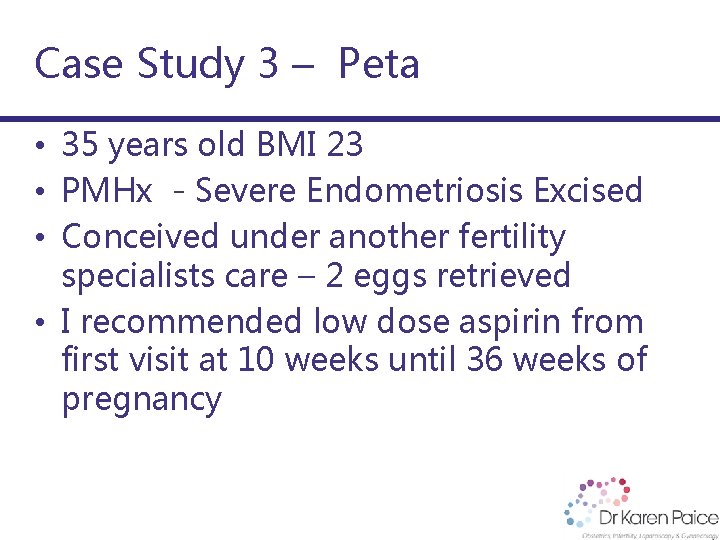
Case Study 3 – Peta • 35 years old BMI 23 • PMHx - Severe Endometriosis Excised • Conceived under another fertility specialists care – 2 eggs retrieved • I recommended low dose aspirin from first visit at 10 weeks until 36 weeks of pregnancy
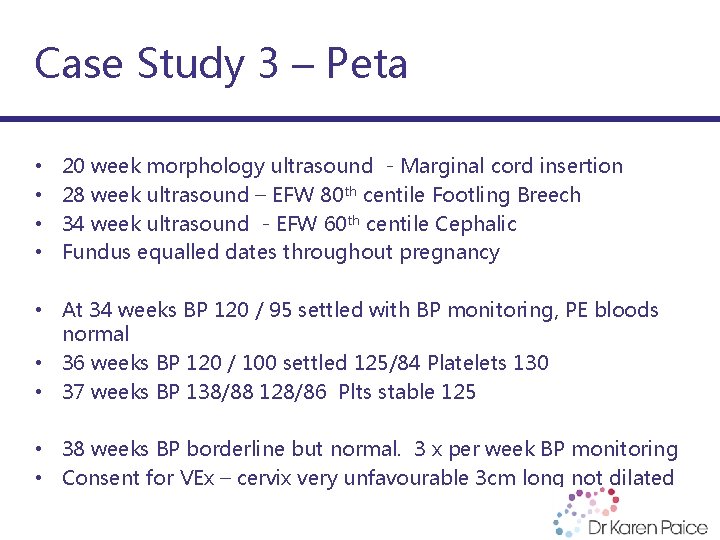
Case Study 3 – Peta • • 20 week morphology ultrasound - Marginal cord insertion 28 week ultrasound – EFW 80 th centile Footling Breech 34 week ultrasound - EFW 60 th centile Cephalic Fundus equalled dates throughout pregnancy • At 34 weeks BP 120 / 95 settled with BP monitoring, PE bloods normal • 36 weeks BP 120 / 100 settled 125/84 Platelets 130 • 37 weeks BP 138/88 128/86 Plts stable 125 • 38 weeks BP borderline but normal. 3 x per week BP monitoring • Consent for VEx – cervix very unfavourable 3 cm long not dilated
Case Study 3 – Peta • • 38+6 admitted for IOL with balloon catheter On admission BP 150/105 Improved with 100 mg labetolol Platelets stable 115 Cr 88 UA 0. 42 spot urine 21 (protein previously undetectable) Offered LUSCS. Declined Balloon inserted removed next morning - 3 cm dilated 2 cm long ARM 2 pm not yet in established labour - recurrent moderate deep variables recommended LUSCS Lucien born in good condition 2990 gm – 10 th centile
Case Study 3 – Peta
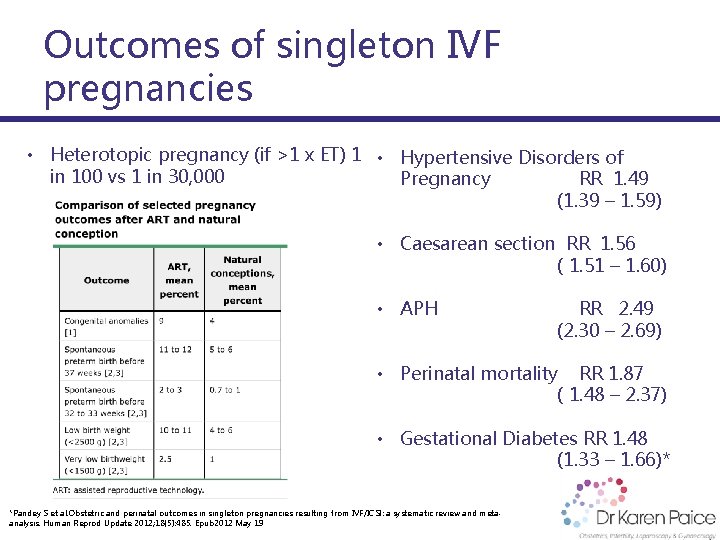
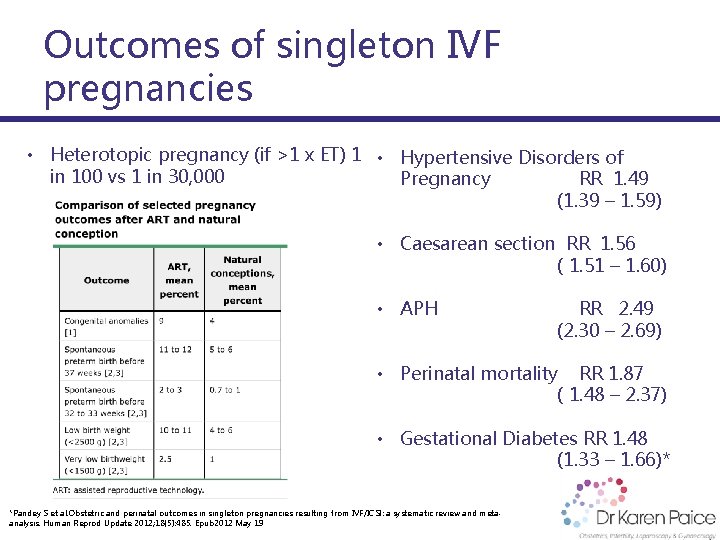
Outcomes of singleton IVF pregnancies • Heterotopic pregnancy (if >1 x ET) 1 • Hypertensive Disorders of in 100 vs 1 in 30, 000 Pregnancy RR 1. 49 (1. 39 – 1. 59) • Caesarean section RR 1. 56 ( 1. 51 – 1. 60) • APH RR 2. 49 (2. 30 – 2. 69) • Perinatal mortality RR 1. 87 ( 1. 48 – 2. 37) • Gestational Diabetes RR 1. 48 (1. 33 – 1. 66)* *Pandey S et al. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and metaanalysis. Human Reprod Update 2012; 18(5): 485. Epub 2012 May 19
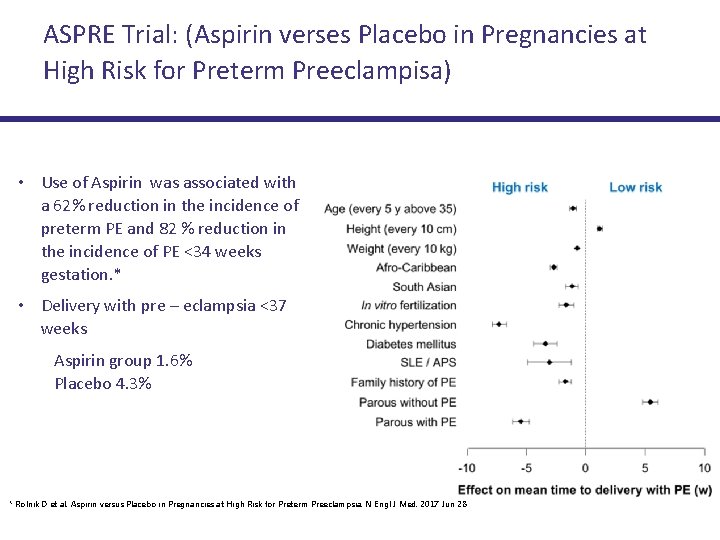
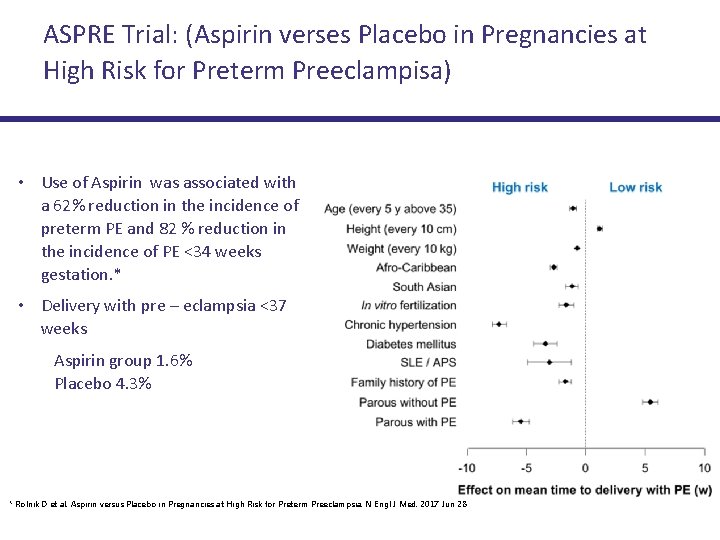
ASPRE Trial: (Aspirin verses Placebo in Pregnancies at High Risk for Preterm Preeclampisa) • Use of Aspirin was associated with a 62% reduction in the incidence of preterm PE and 82 % reduction in the incidence of PE <34 weeks gestation. * • Delivery with pre – eclampsia <37 weeks Aspirin group 1. 6% Placebo 4. 3% * Rolnik D et al. Aspirin versus Placebo in Pregnancies at High Risk for Preterm Preeclampsia. N Engl J Med. 2017 Jun 28
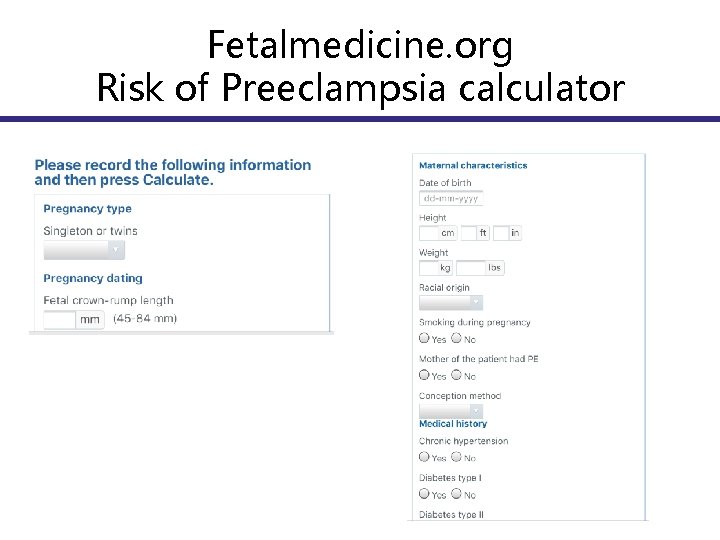
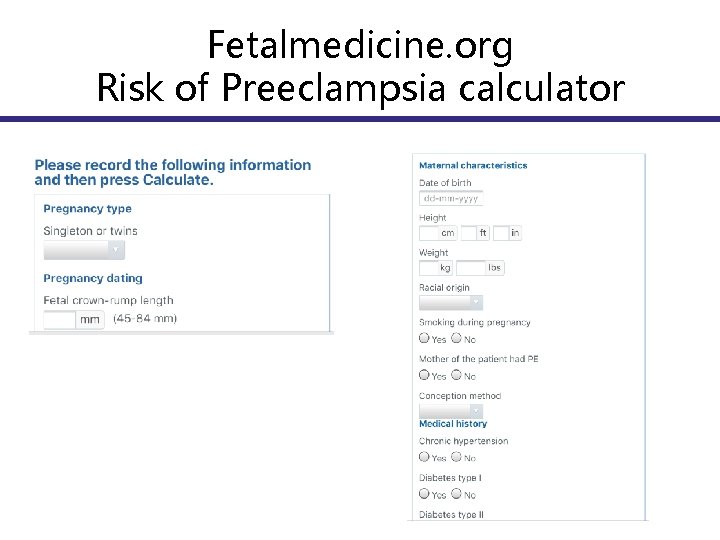
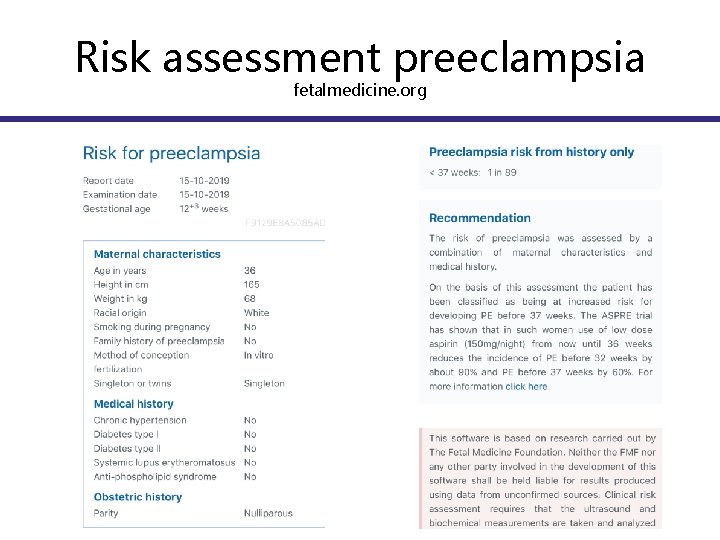
Fetalmedicine. org Risk of Preeclampsia calculator
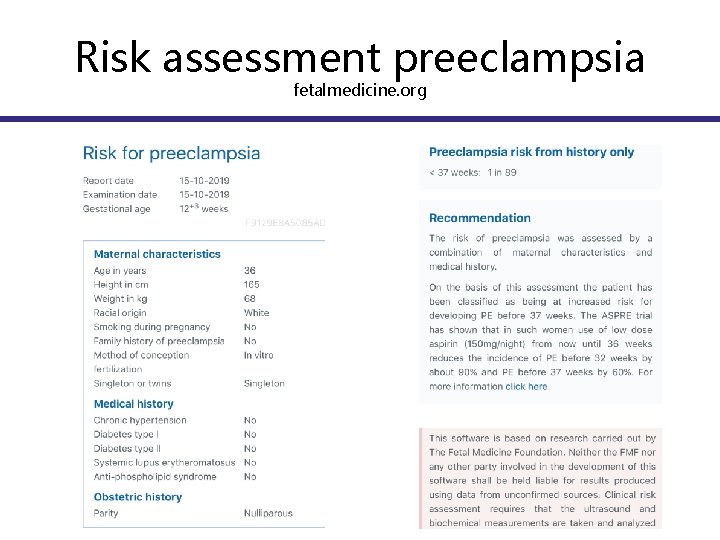
Risk assessment preeclampsia fetalmedicine. org
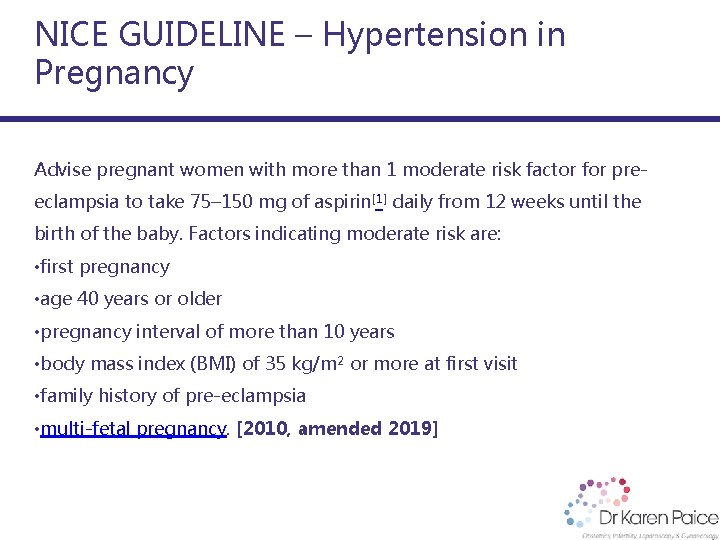
NICE GUIDELINE – Hypertension in Pregnancy Advise pregnant women with more than 1 moderate risk factor for preeclampsia to take 75– 150 mg of aspirin[1] daily from 12 weeks until the birth of the baby. Factors indicating moderate risk are: • first pregnancy • age 40 years or older • pregnancy interval of more than 10 years • body mass index (BMI) of 35 kg/m 2 or more at first visit • family history of pre-eclampsia • multi-fetal pregnancy. [2010, amended 2019]
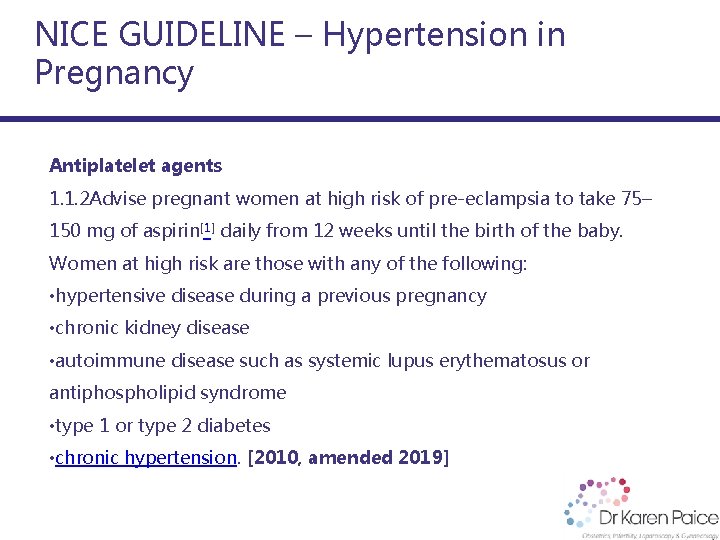
NICE GUIDELINE – Hypertension in Pregnancy Antiplatelet agents 1. 1. 2 Advise pregnant women at high risk of pre-eclampsia to take 75– 150 mg of aspirin[1] daily from 12 weeks until the birth of the baby. Women at high risk are those with any of the following: • hypertensive disease during a previous pregnancy • chronic kidney disease • autoimmune disease such as systemic lupus erythematosus or antiphospholipid syndrome • type 1 or type 2 diabetes • chronic hypertension. [2010, amended 2019]

Take Home Messages for IVF Pregnancies Aspirin? • First visit IVF …. . 150 mg Aspirin nocte ? (Fetalmedicine. org calculator) • Third trimester growth scan • Consider fortnightly visits in third trimester (BP checks)

Thank you Dr Karen Paice MBBS FRANZCOG MRMed High and Low Risk Obstetrics St Vincent’s Private - Epworth Freemason’s Hospital Melbourne IVF Contact 9419 5757 145 Victoria Parade Fitzroy https: //www. drkarenpaice. com. au