It s not too viral always Diagnostic dilemma





- Slides: 24
It ‘s not too viral always: Diagnostic dilemma of Jaundice Case presentation by Dr. A. Akhila, PGT, CNMCH
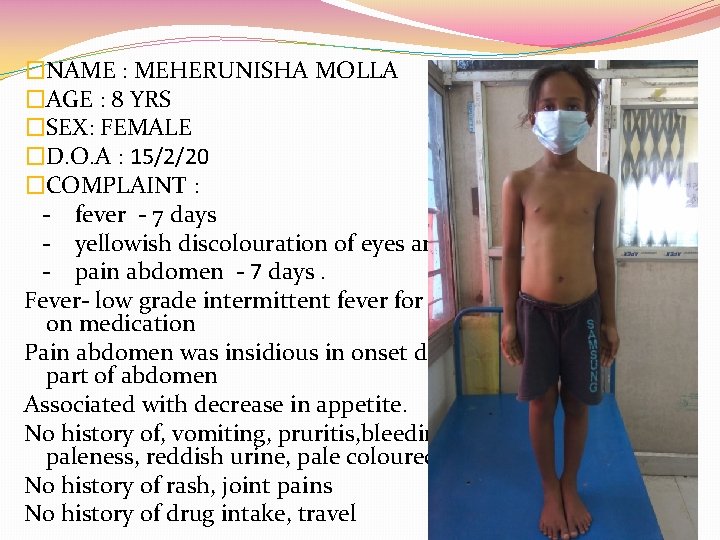
�NAME : MEHERUNISHA MOLLA �AGE : 8 YRS �SEX: FEMALE �D. O. A : 15/2/20 �COMPLAINT : - fever - 7 days - yellowish discolouration of eyes and urine – 6 days - pain abdomen - 7 days. Fever- low grade intermittent fever for last 7 days which relieved on medication Pain abdomen was insidious in onset dull aching, on right upper part of abdomen Associated with decrease in appetite. No history of, vomiting, pruritis, bleeding episodes, increased paleness, reddish urine, pale coloured stool. No history of rash, joint pains No history of drug intake, travel
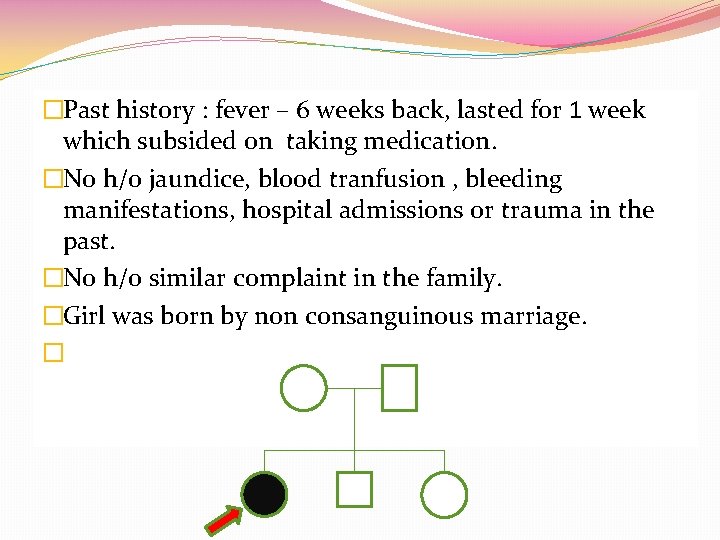
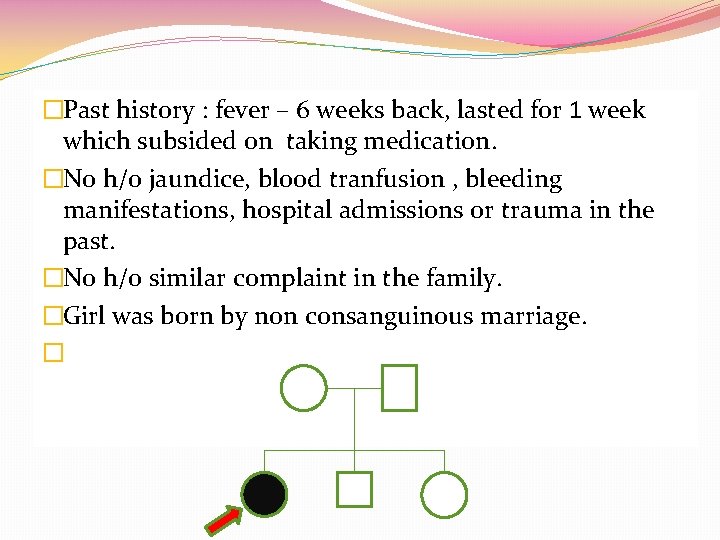
�Past history : fever – 6 weeks back, lasted for 1 week which subsided on taking medication. �No h/o jaundice, blood tranfusion , bleeding manifestations, hospital admissions or trauma in the past. �No h/o similar complaint in the family. �Girl was born by non consanguinous marriage. �
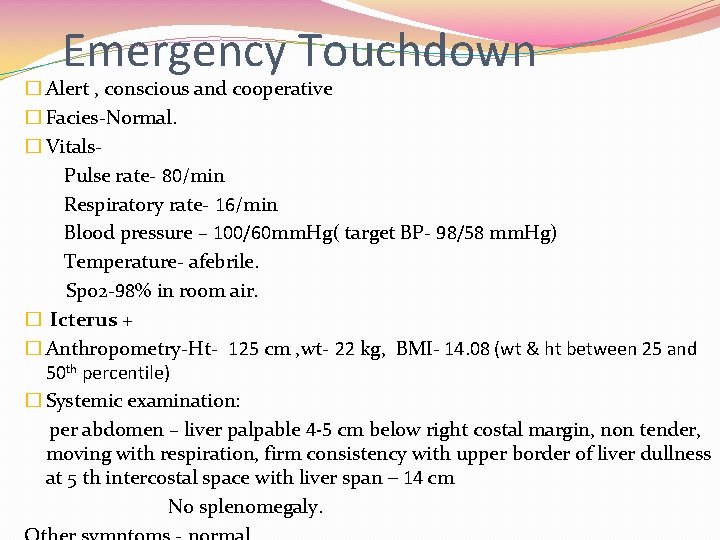
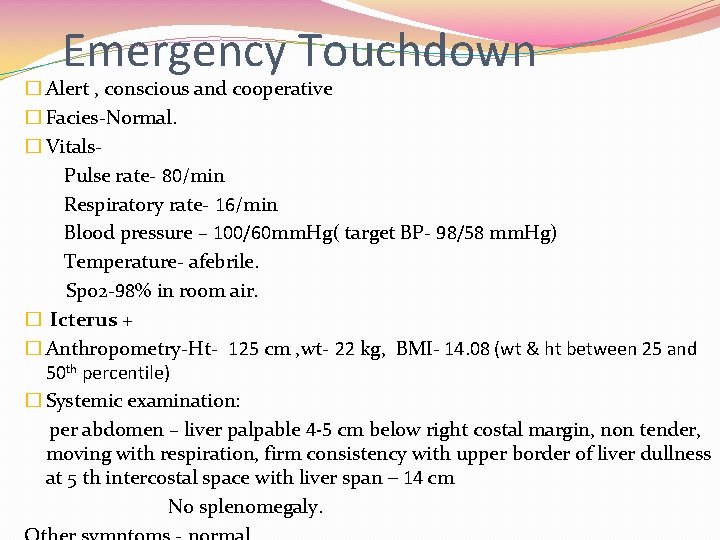
Emergency Touchdown � Alert , conscious and cooperative � Facies-Normal. � Vitals. Pulse rate- 80/min Respiratory rate- 16/min Blood pressure – 100/60 mm. Hg( target BP- 98/58 mm. Hg) Temperature- afebrile. Spo 2 -98% in room air. � Icterus + � Anthropometry-Ht- 125 cm , wt- 22 kg, BMI- 14. 08 (wt & ht between 25 and 50 th percentile) � Systemic examination: per abdomen – liver palpable 4 -5 cm below right costal margin, non tender, moving with respiration, firm consistency with upper border of liver dullness at 5 th intercostal space with liver span – 14 cm No splenomegaly.
Differential Diagnosis �Hepatitis �Autoimmune liver disease �Metabolic - wilson
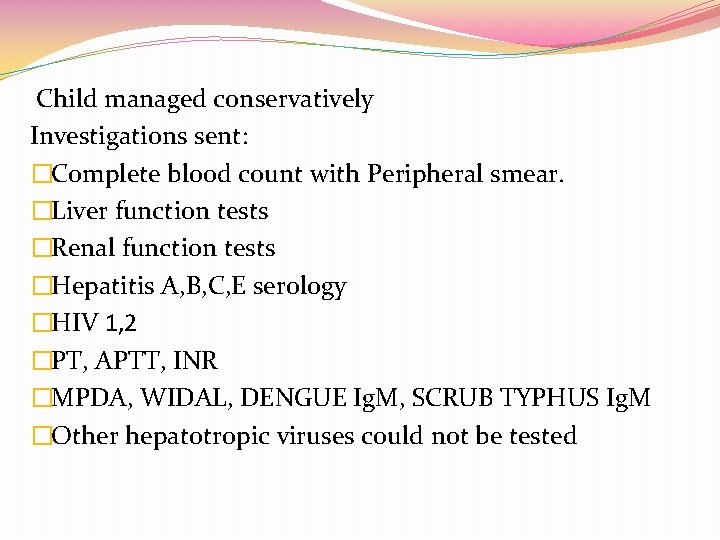
Child managed conservatively Investigations sent: �Complete blood count with Peripheral smear. �Liver function tests �Renal function tests �Hepatitis A, B, C, E serology �HIV 1, 2 �PT, APTT, INR �MPDA, WIDAL, DENGUE Ig. M, SCRUB TYPHUS Ig. M �Other hepatotropic viruses could not be tested
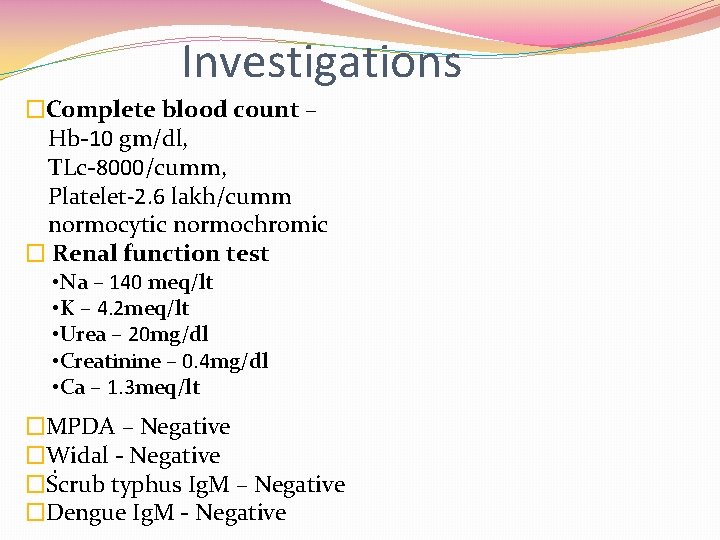
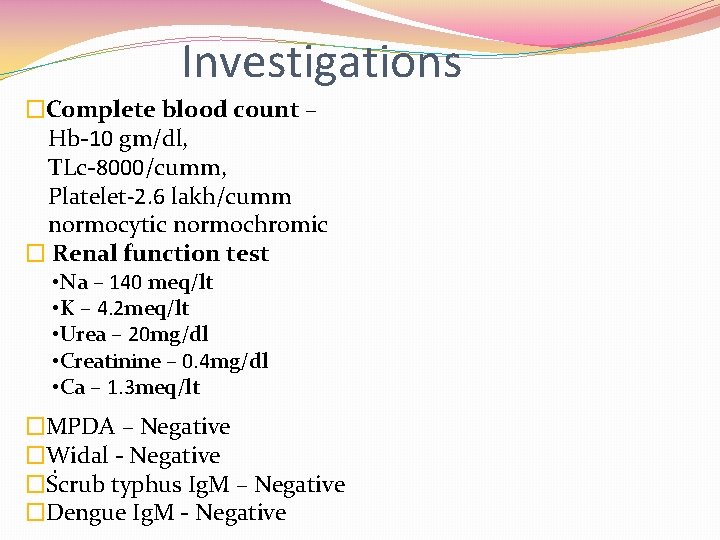
Investigations �Complete blood count – Hb-10 gm/dl, TLc-8000/cumm, Platelet-2. 6 lakh/cumm normocytic normochromic � Renal function test • Na – 140 meq/lt • K – 4. 2 meq/lt • Urea – 20 mg/dl • Creatinine – 0. 4 mg/dl • Ca – 1. 3 meq/lt �MPDA – Negative �Widal - Negative. �Scrub typhus Ig. M – Negative �Dengue Ig. M - Negative
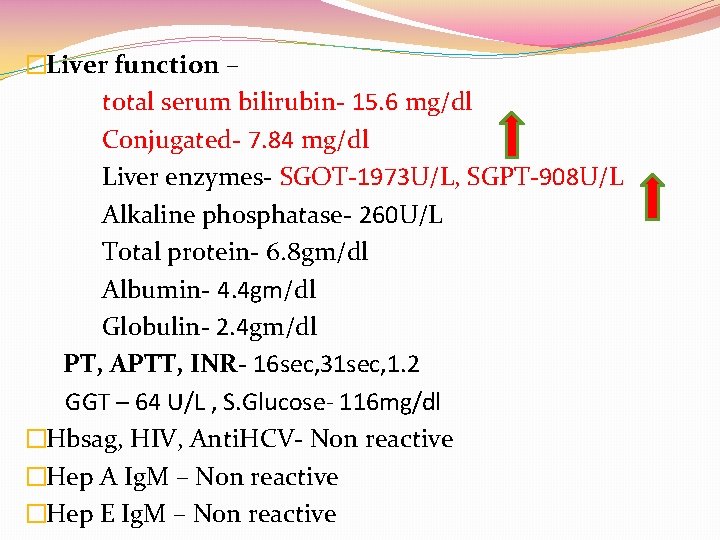
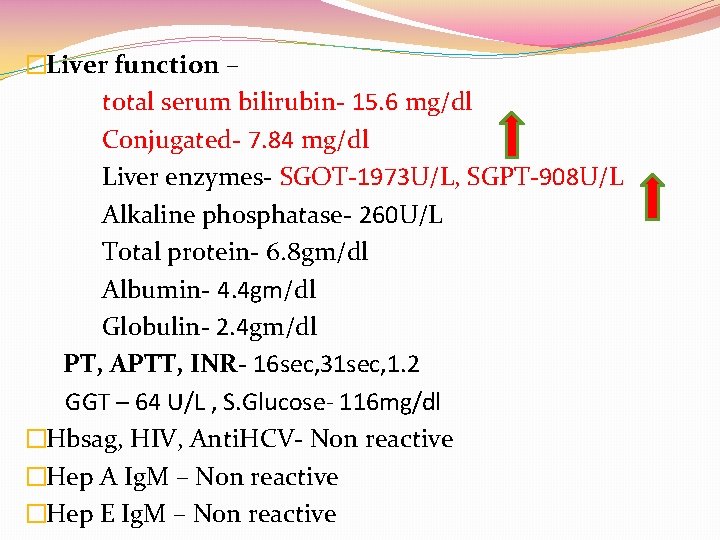
�Liver function – total serum bilirubin- 15. 6 mg/dl Conjugated- 7. 84 mg/dl Liver enzymes- SGOT-1973 U/L, SGPT-908 U/L Alkaline phosphatase- 260 U/L Total protein- 6. 8 gm/dl Albumin- 4. 4 gm/dl Globulin- 2. 4 gm/dl PT, APTT, INR- 16 sec, 31 sec, 1. 2 GGT – 64 U/L , S. Glucose- 116 mg/dl �Hbsag, HIV, Anti. HCV- Non reactive �Hep A Ig. M – Non reactive �Hep E Ig. M – Non reactive
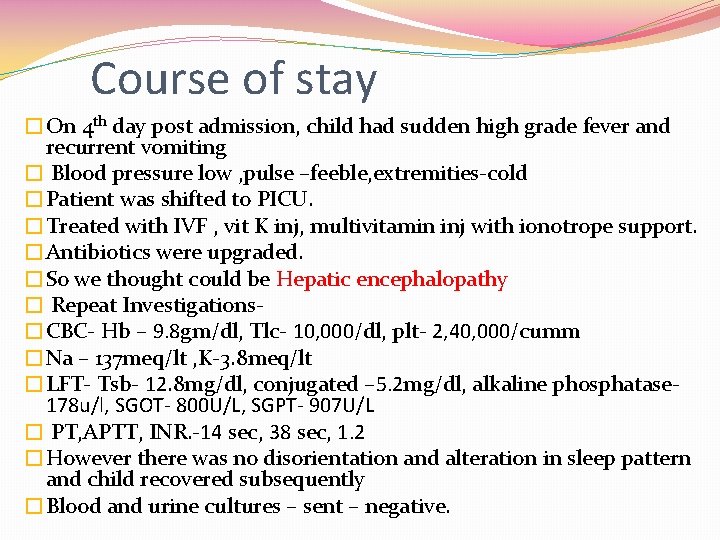
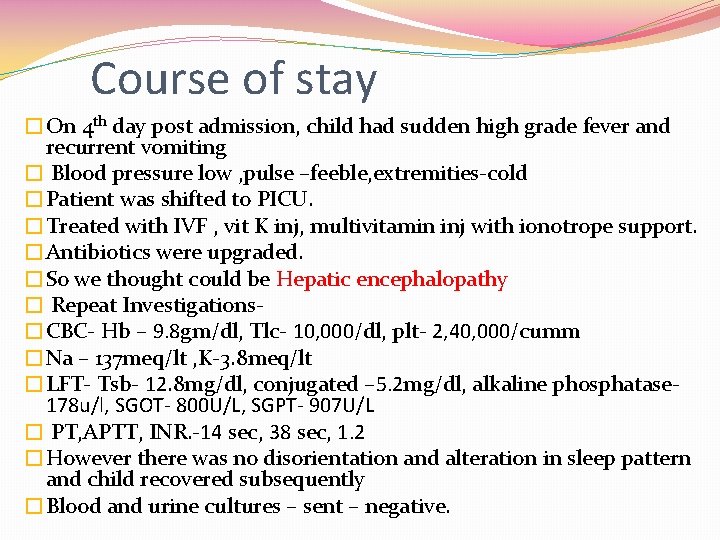
Course of stay �On 4 th day post admission, child had sudden high grade fever and recurrent vomiting � Blood pressure low , pulse –feeble, extremities-cold �Patient was shifted to PICU. �Treated with IVF , vit K inj, multivitamin inj with ionotrope support. �Antibiotics were upgraded. �So we thought could be Hepatic encephalopathy � Repeat Investigations�CBC- Hb – 9. 8 gm/dl, Tlc- 10, 000/dl, plt- 2, 40, 000/cumm �Na – 137 meq/lt , K-3. 8 meq/lt �LFT- Tsb- 12. 8 mg/dl, conjugated – 5. 2 mg/dl, alkaline phosphatase 178 u/l, SGOT- 800 U/L, SGPT- 907 U/L � PT, APTT, INR. -14 sec, 38 sec, 1. 2 �However there was no disorientation and alteration in sleep pattern and child recovered subsequently �Blood and urine cultures – sent – negative.


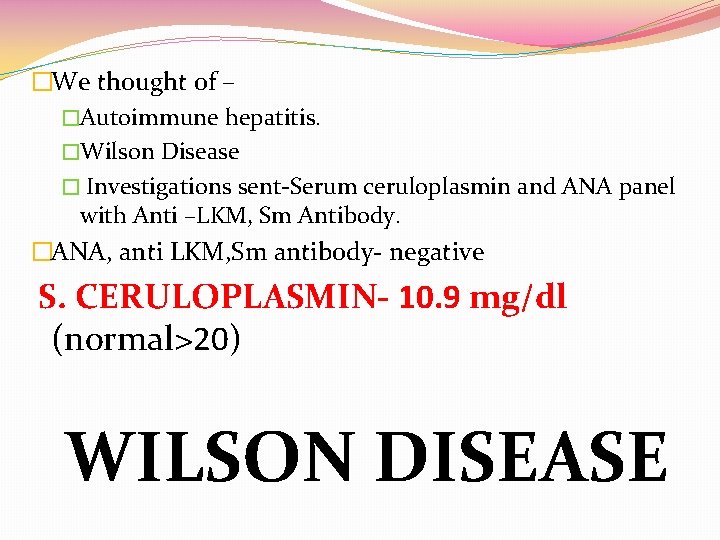
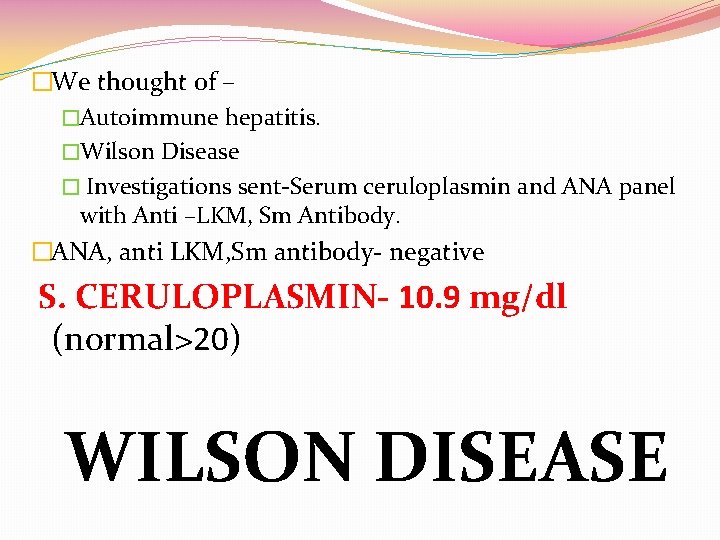
�We thought of – �Autoimmune hepatitis. �Wilson Disease � Investigations sent-Serum ceruloplasmin and ANA panel with Anti –LKM, Sm Antibody. �ANA, anti LKM, Sm antibody- negative S. CERULOPLASMIN- 10. 9 mg/dl (normal>20) WILSON DISEASE
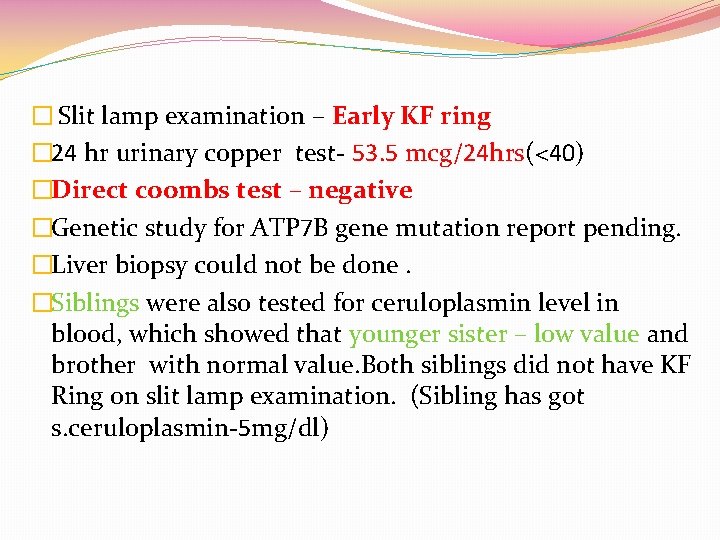
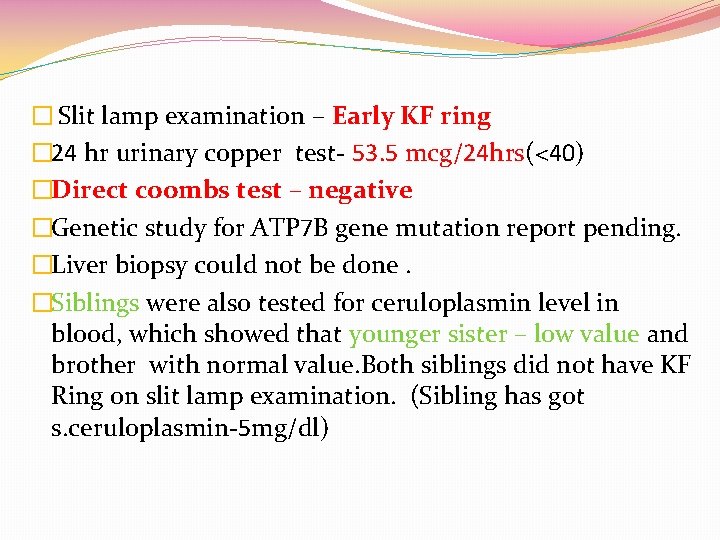
� Slit lamp examination – Early KF ring � 24 hr urinary copper test- 53. 5 mcg/24 hrs(<40) �Direct coombs test – negative �Genetic study for ATP 7 B gene mutation report pending. �Liver biopsy could not be done. �Siblings were also tested for ceruloplasmin level in blood, which showed that younger sister – low value and brother with normal value. Both siblings did not have KF Ring on slit lamp examination. (Sibling has got s. ceruloplasmin-5 mg/dl)

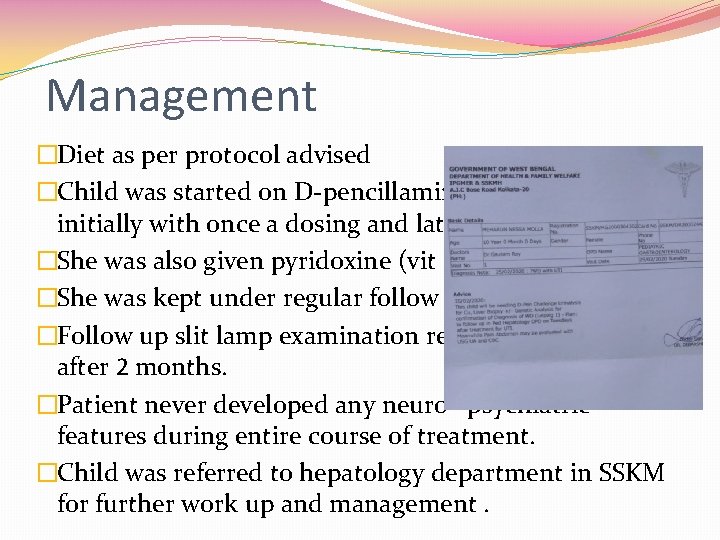
Management �Diet as per protocol advised �Child was started on D-pencillamine therapy 250 mg initially with once a dosing and later to twice daily. �She was also given pyridoxine (vit B 6) �She was kept under regular follow up. �Follow up slit lamp examination revealed no KF ring after 2 months. �Patient never developed any neuro –psychiatric features during entire course of treatment. �Child was referred to hepatology department in SSKM for further work up and management.
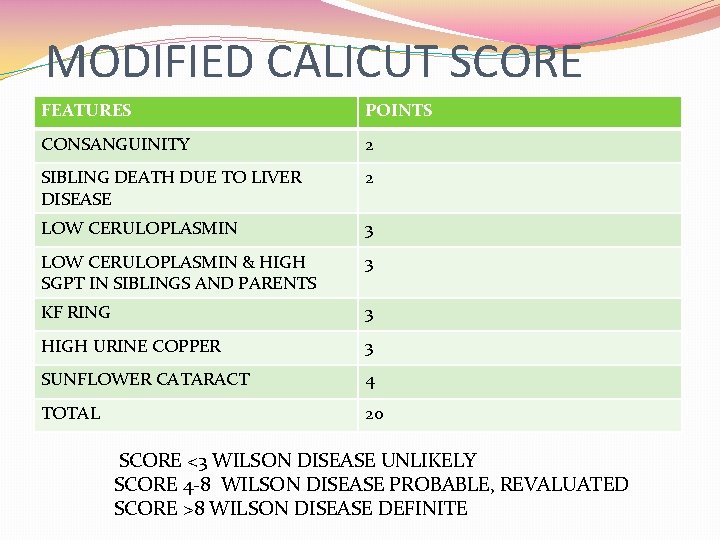
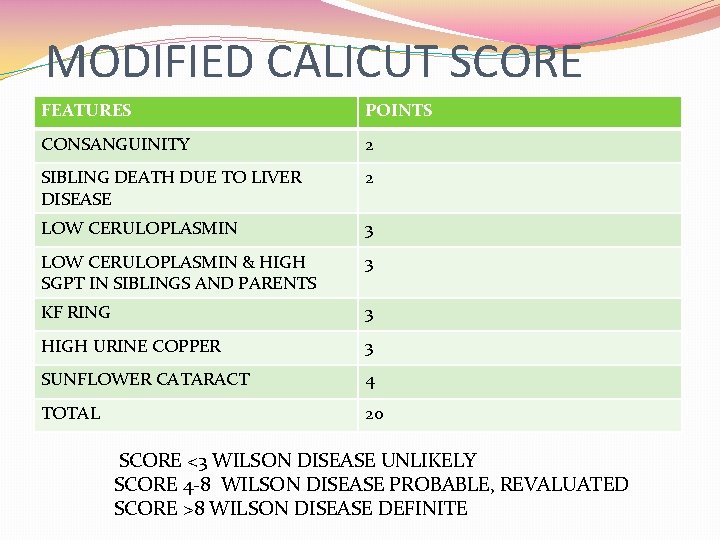
MODIFIED CALICUT SCORE FEATURES POINTS CONSANGUINITY 2 SIBLING DEATH DUE TO LIVER DISEASE 2 LOW CERULOPLASMIN 3 LOW CERULOPLASMIN & HIGH SGPT IN SIBLINGS AND PARENTS 3 KF RING 3 HIGH URINE COPPER 3 SUNFLOWER CATARACT 4 TOTAL 20 SCORE <3 WILSON DISEASE UNLIKELY SCORE 4 -8 WILSON DISEASE PROBABLE, REVALUATED SCORE >8 WILSON DISEASE DEFINITE
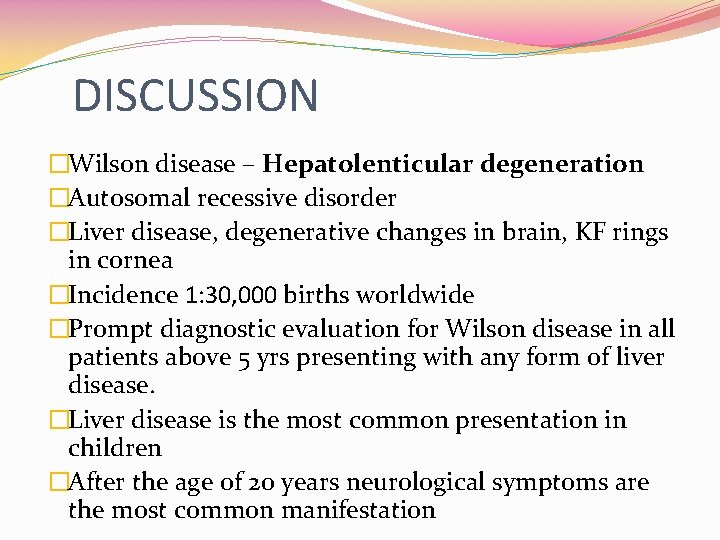
DISCUSSION �Wilson disease – Hepatolenticular degeneration �Autosomal recessive disorder �Liver disease, degenerative changes in brain, KF rings in cornea �Incidence 1: 30, 000 births worldwide �Prompt diagnostic evaluation for Wilson disease in all patients above 5 yrs presenting with any form of liver disease. �Liver disease is the most common presentation in children �After the age of 20 years neurological symptoms are the most common manifestation


When to suspect? ? ? �Unexplained acute or chronic liver disease �Neurological symptoms of unexplained etiology �Acute hemolysis �Psychiatric illness �Behavioural changes �Fanconi syndrome �Unexplained bone or muscle disease
Treatment �DIETARY - avoid copper rich foods like chocolates, nuts, liver, shellfish �PHARMACOLOGICAL- copper chelating agents like. D-pencillamine, trientene, ammonium tetrathiomolybdate and zinc Vit B 6 adjuvant to D- Pencillamine �LIVER TRANSPLANTATION – acute liver failure or decompensated cirrhosis.
PROGNOSIS �variable �Depends on time of initiation and individual response to chelation �Usually significant clinical improvement is seen within weeks of starting treatment. �Generally symptoms subside first, followed by disappearance or fading of KF ring
Take home message �Always suspect metabolic and autoimmune liver disease when it’s presentation like viral hepatitis �Always screen family members / siblings in case of wilson disease �Counselling of parents regarding long term prognosis of disease is important to make the patient party aware of complications of toxicity of drug (as sudden stoppage of therapy leads to fulminant liver disease)
Thank you
 Too broad too narrow
Too broad too narrow Small just
Small just Too much too many and enough
Too much too many and enough Cryptinject
Cryptinject Too broad and too narrow examples
Too broad and too narrow examples Too broad and too narrow examples
Too broad and too narrow examples Too foreign for home
Too foreign for home Rational of the study
Rational of the study Too anointed to be disappointed meaning
Too anointed to be disappointed meaning Too much money is chasing too few goods
Too much money is chasing too few goods The road not taken connotation
The road not taken connotation Always low prices always
Always low prices always Sadlier unit 1 level d synonyms
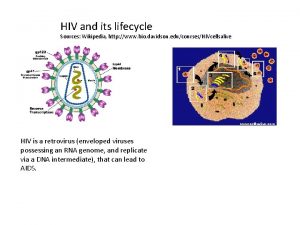
Sadlier unit 1 level d synonyms Section 24-1 viral structure and replication
Section 24-1 viral structure and replication Viral communications
Viral communications Mobilivirus
Mobilivirus Replicação viral ciclo lítico e lisogênico
Replicação viral ciclo lítico e lisogênico Viral entry
Viral entry Inmunidad
Inmunidad Virus cultivation in embryonated eggs
Virus cultivation in embryonated eggs Viral arthritis
Viral arthritis Rhinopneumonitis definition
Rhinopneumonitis definition Hemolyzed serum sample
Hemolyzed serum sample Inklüzyon cisimcikleri
Inklüzyon cisimcikleri Itil wikipedia fr
Itil wikipedia fr