IntravenousNon volatile aesthetics Dr Wael Alham Yasin Lecturer




- Slides: 24

Intravenous"Non volatile" aesthetics Dr/ Wael Alham Yasin Lecturer of anaesthesia&ICU Sohag Faculty of medicine Sohag university
These are drugs that, when given intravenously in an appropriate dose, cause a rapid loss of consciousness. They are used: � - To induce anaesthesia prior to other drugs being given to maintain anaesthesia. � - As a sole drug for short procedures. � -To maintain anaesthesia for longer procedures by intravenous infusion. � -To provide sedation.
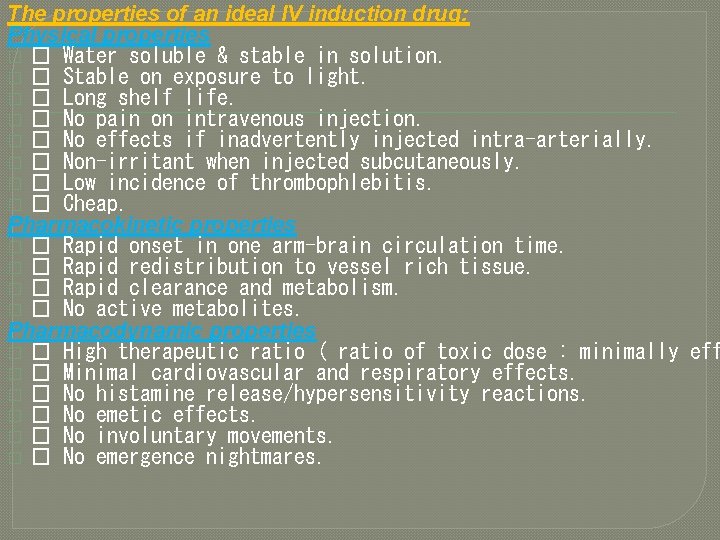
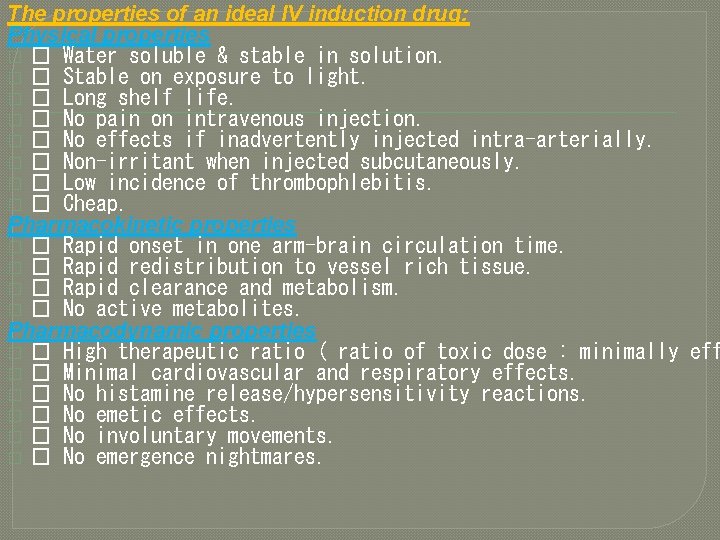
The properties of an ideal IV induction drug: Physical properties � � Water soluble & stable in solution. � � Stable on exposure to light. � � Long shelf life. � � No pain on intravenous injection. � � No effects if inadvertently injected intra-arterially. � � Non-irritant when injected subcutaneously. � � Low incidence of thrombophlebitis. � � Cheap. Pharmacokinetic properties � � Rapid onset in one arm-brain circulation time. � � Rapid redistribution to vessel rich tissue. � � Rapid clearance and metabolism. � � No active metabolites. Pharmacodynamic properties � � High therapeutic ratio ( ratio of toxic dose : minimally eff � � Minimal cardiovascular and respiratory effects. � � No histamine release/hypersensitivity reactions. � � No emetic effects. � � No involuntary movements. � � No emergence nightmares.
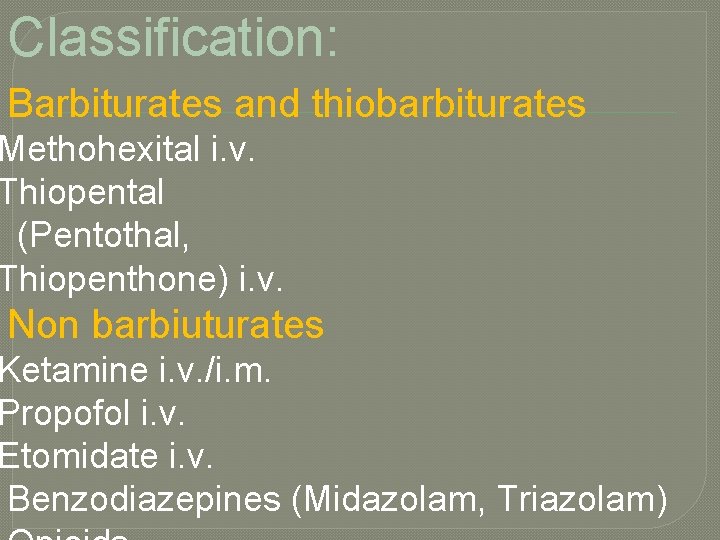
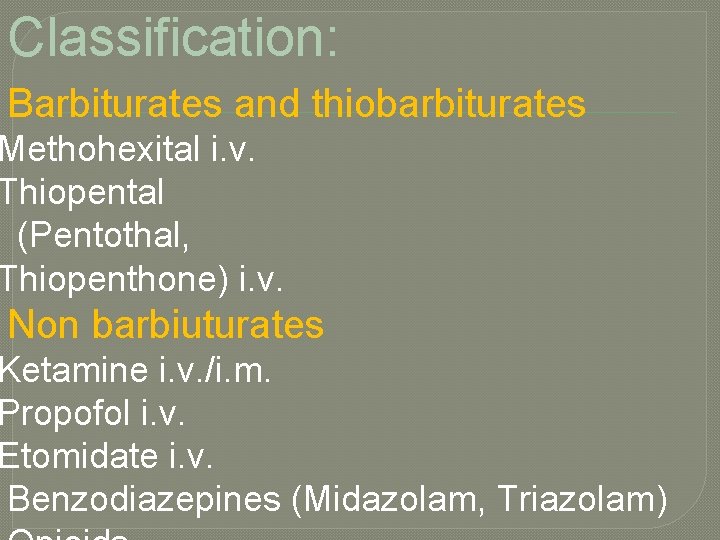
Classification: Barbiturates and thiobarbiturates Methohexital i. v. Thiopental (Pentothal, Thiopenthone) i. v. Non barbiuturates Ketamine i. v. /i. m. Propofol i. v. Etomidate i. v. Benzodiazepines (Midazolam, Triazolam)
General pharmacokinetics: � On entering the blood stream, a percentage of the drug binds to the plasma proteins, with the rest remaining unbound or “free”. � The majority of the cardiac output (70%) passes to the brain, liver and kidney (often referred to as “vessel rich organs”); thus a high proportion of the initial bolus is delivered to the cerebral circulation. The rate of this transfer is dependent on a number of factors: � � the arterial concentration of the unbound drug. f � � the lipid solubility drug. of the � � the degree of ionization.
� Unbound, lipid soluble, unionized molecules cross the blood brain barrier the quickest. Once the drug has penetrated the CNS tissue, it exerts its effects. Like most anaesthetic drugs, the exact mode of action of the intravenous drugs is unknown. It is thought that each drug acts at a specific receptor – GABA-A, NMDA. � Following the initial flooding of the CNS and other vessel rich tissues with non-ionized molecules, the drug starts to diffuse in to other tissues that do not have such a rich blood supply. This secondary tissue uptake "redistribution", predominantly by skeletal muscle, causes the plasma concentration to fall, allowing drug to diffuse out of the CNS down the resulting reverse concentration gradient.
�It is this initial redistribution of drug into other tissues that leads to the rapid wake up seen after a single dose of an induction drug. �Metabolism and plasma clearance have a much less important role following a single bolus, but are more important following infusions and repeat doses of a drug.
Mechanism of action of IV anaesthetics: �Facilitatation of the inhibitory effect of GABA at its receptors e. g Benzodiazepines, Barbiturates, and Propofol. �Inhibition of excitatory effect of glutamate at NMDA receptors e. g ketamine � Opiods activate opioid receptors "mu, kappa, and delta" directly or through release of endogenous opiopeptides endorphine &enceplalines lead to neuronal inhibition

Properties of specific IV induction drugs A) Barbiturates "Sodium Thiopental"
Physical characters: Thiopental (also referred to as thiopentone and Pentothal) is a barbiturate pale yellow powder. Ampoules commonly contain 500 mg of sodium thiopental with 6% sodium carbonate in an inert atmosphere of nitrogen. The alkaline solution is bacteriostatic and safe to keep for 48 hours. Short duration of action due to redistribution from the brain to other tissues (adipose tissue, &skeletal muscles) Slowly metabolized in the liver and liable to accumulate in body fat , therefore may cause prolonged effect if given repeatedly …. water soluble metabolites excreted via the kidney.
Uses: • Induction of GA • Anaethesia for shor procedures e. g D&C. • ttt of status epilepticus. • Brain protection& ↓ ICP in neurosurgeries. Dose: 3 -6 mg/ kg. Clinical. Effects: *CNS: Amnesia after 30 sec. unconciouseness after 5 -10 min. Progressive CNS depression, including spinal cord reflexes. ↓CMR ……↓CBF…. ↓ICP………. + Potent anticonvulsant. At subanesthetic dose…. →antianalgesic as it ↓pain threshold. *CVS: ↓myocardial contractility, Peripheral VD. . So ↓BP especially in hypovolaemic or cardiac patients.
*Skeletal muscles: � High concentrations…. . ↓skeletal muscle tone due to suppression of spinal cord reflexes , however it has a poor muscle relaxation. *Respiratory : � Apnea following induction, ↓ RR, and ↓ TV. � ↓FRC ……→ ↓ response to hypercapnea and hypoxia. � Bronchospasm, & laryngospasm as it doesn’t completely depress airway reflexes. *Hepatorenal: � Transient impairment of liver & renal functions. � Induction of liver microsomal enzymes → ↑ metabolism &elimination of other drugs e. g. digitoxin. *Uterus &Placenta: � ↓uterine contractions at high doses…. . Also it crosses the placenta.
Adverse reactions: � Hypotension � Respiratory depression. � Subcutaneous injection : Local tissue necrosis. � Intra-arterial ingection : profound VC may cause iscaemia &gangrene of hanf and fingers. � Thrombophlebitis : Uncommon. � Allergic reactions : from rash to fatal anaphylactic reactions & cardiovascular collapse. Contraindications: * Airway obstruction: e. g epiglottitis , oral or pharyngeal tumours d. t ↓ airway reflexes& hypoventilation. *Porphyria: Precipitate LMNL & severe CV collapse in those patients *Previous hypersensitivity reactions to barbiturates.

B) Non barbiturates 1 - Propofol (2, 6 di-isopropylphenol)
Physical characters: � Propofol is usually presented as a 1 or 2% aqueous emulsion (tiny fat droplets in suspension, hence the white colour) containing soya oil, egg phosphatide and glycerol. It is isotonic to plasma and has a p. H of 7. 0 - 8. 5. Uses: � Induction of GA � Main anaesthesia with opioids in TIVA. � Sedation in ICU …. . → through infusion � Adjunct to anti-emetics as it ↓ PONV. pumps. Dose: 1. 5 -2. 5 mg/kg. Pharmacokinetics: � Absorption: iv � Distribution: fast onset to high lipid solubility. � Metabolism: Redistribution mainly …. also conjugation in liver to inactive metabolites that are eliminated by the kidney, Extrahepatic”lung” 30%.
Clinical effects: CNS: � � ↓CMR ……↓CBF…. ↓ICP…↓IOP……. + Potent anticonvulsant. Antiemetic …. antipruritic. � ↓ABP due to ↓Contractility of the heart, VD & ↓SVR. . Hypotension CVS: ›thiopental. Respiratory: � � Apnea following induction. . profound hypoventilation Histamine release…possible. ›thiopental. Adverse effects: Pain on injection: in 40% of patients CVS depression: ↓myocardial contractility, Peripheral VD. . So ↓BP especially in hypovolaemic or cardiac patients. � Respiratory depression: Apnea is more common & of longer duration that occurs after barbiturate administration. � Excitatory phenomenon: on induction › thiopental. � Emergence agitation: › thiopental. � �
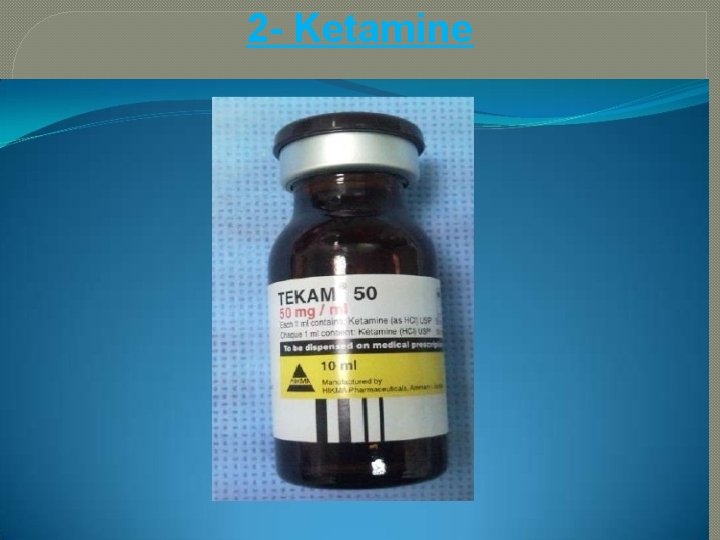
2 - Ketamine
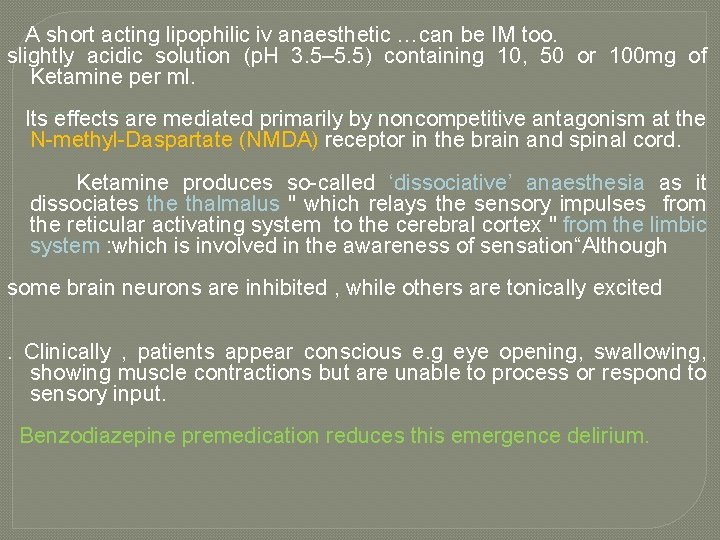
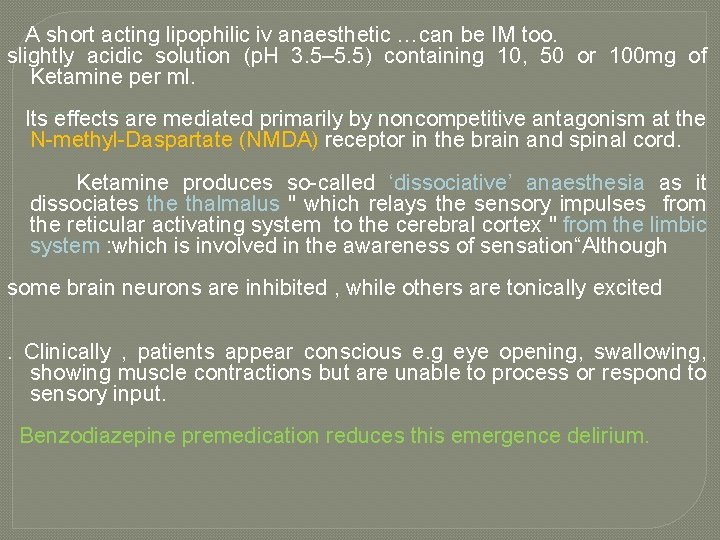
A short acting lipophilic iv anaesthetic …can be IM too. slightly acidic solution (p. H 3. 5– 5. 5) containing 10, 50 or 100 mg of Ketamine per ml. Its effects are mediated primarily by noncompetitive antagonism at the N-methyl-Daspartate (NMDA) receptor in the brain and spinal cord. Ketamine produces so-called ‘dissociative’ anaesthesia as it dissociates the thalmalus " which relays the sensory impulses from the reticular activating system to the cerebral cortex " from the limbic system : which is involved in the awareness of sensation“Although some brain neurons are inhibited , while others are tonically excited. Clinically , patients appear conscious e. g eye opening, swallowing, showing muscle contractions but are unable to process or respond to sensory input. Benzodiazepine premedication reduces this emergence delirium.
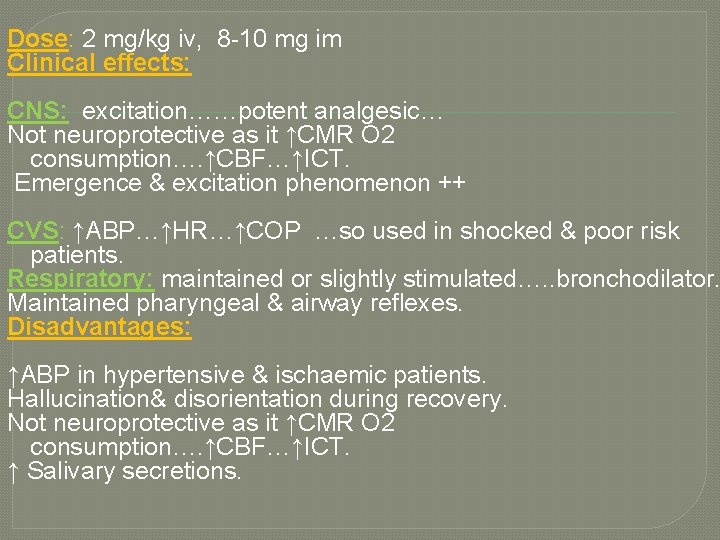
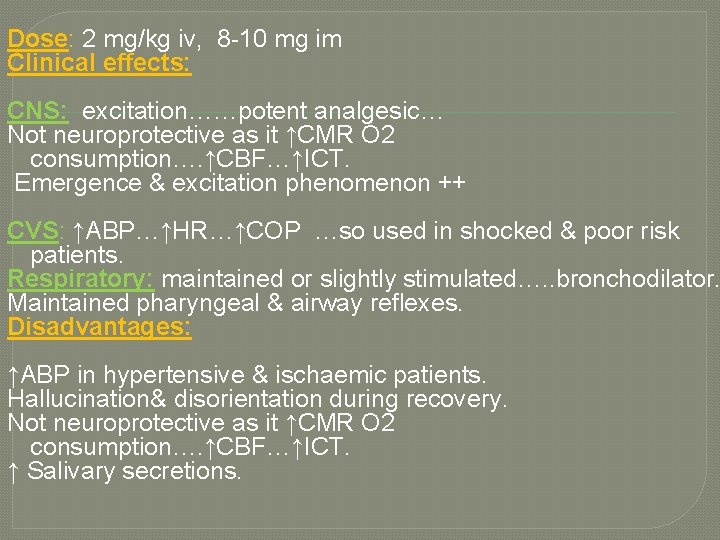
Dose: 2 mg/kg iv, 8 -10 mg im Clinical effects: CNS: excitation……potent analgesic… Not neuroprotective as it ↑CMR O 2 consumption…. ↑CBF…↑ICT. Emergence & excitation phenomenon ++ CVS: ↑ABP…↑HR…↑COP …so used in shocked & poor risk patients. Respiratory: maintained or slightly stimulated…. . bronchodilator. Maintained pharyngeal & airway reflexes. Disadvantages: ↑ABP in hypertensive & ischaemic patients. Hallucination& disorientation during recovery. Not neuroprotective as it ↑CMR O 2 consumption…. ↑CBF…↑ICT. ↑ Salivary secretions.
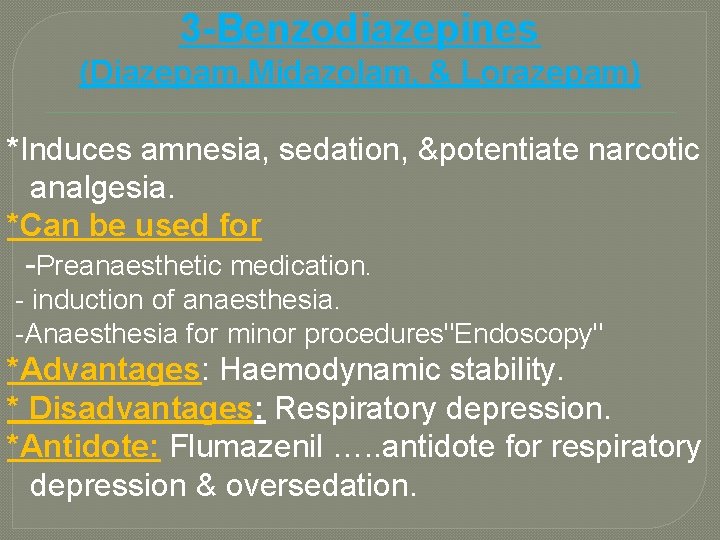
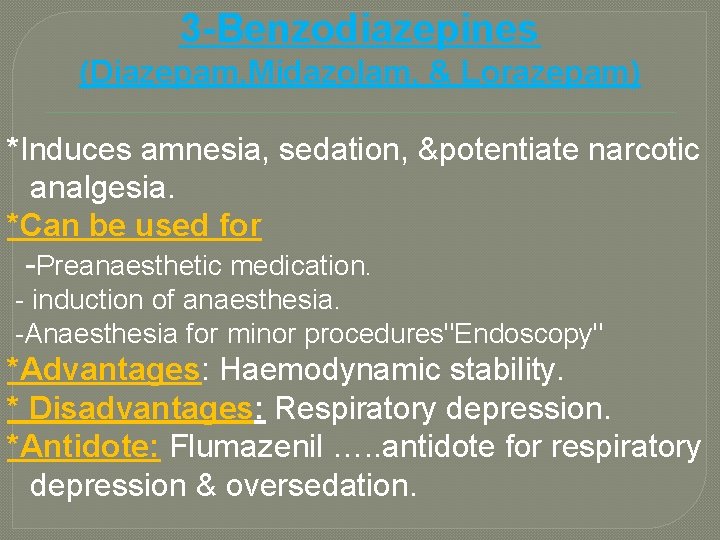
3 -Benzodiazepines (Diazepam, Midazolam, & Lorazepam) *Induces amnesia, sedation, &potentiate narcotic analgesia. *Can be used for -Preanaesthetic medication. - induction of anaesthesia. -Anaesthesia for minor procedures"Endoscopy" *Advantages: Haemodynamic stability. * Disadvantages: Respiratory depression. *Antidote: Flumazenil …. . antidote for respiratory depression & oversedation.
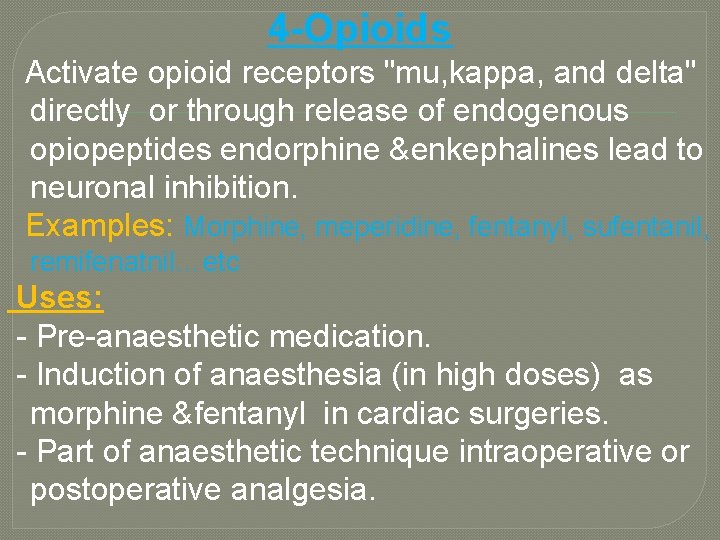
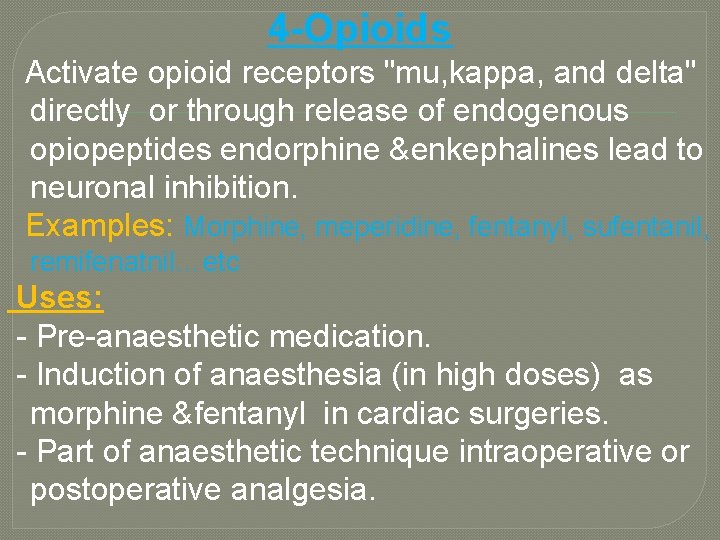
4 -Opioids Activate opioid receptors "mu, kappa, and delta" directly or through release of endogenous opiopeptides endorphine &enkephalines lead to neuronal inhibition. Examples: Morphine, meperidine, fentanyl, sufentanil, remifenatnil…etc Uses: - Pre-anaesthetic medication. - Induction of anaesthesia (in high doses) as morphine &fentanyl in cardiac surgeries. - Part of anaesthetic technique intraoperative or postoperative analgesia.

Thank You
 Lecturer's name
Lecturer's name Wael is the teacher of n students
Wael is the teacher of n students Exposition of the fly by katherine mansfield
Exposition of the fly by katherine mansfield Wael ouarda
Wael ouarda Lector vs lecturer
Lector vs lecturer Lecturer name
Lecturer name Spe distinguished lecturer
Spe distinguished lecturer Designation lecturer
Designation lecturer Lecturer in charge
Lecturer in charge Pearson lecturer resources
Pearson lecturer resources Afternoon teacher
Afternoon teacher Designation of lecturer
Designation of lecturer Cfa lecturer handbook
Cfa lecturer handbook Spe distinguished lecturer
Spe distinguished lecturer Photography lecturer
Photography lecturer Why himalayan rivers are pernnial in nature
Why himalayan rivers are pernnial in nature Jeannie watkins
Jeannie watkins Lecturer asad ali
Lecturer asad ali Lecturer in charge
Lecturer in charge Dr yasin bayram
Dr yasin bayram Ibnu yasin
Ibnu yasin Zafar yasin
Zafar yasin Tartil surat yasin
Tartil surat yasin Zaki yasin architect
Zaki yasin architect Sevtap yasin
Sevtap yasin