AIRWAY ASSESSMENT MANAGEMENT DR wael Alham Mahmoud What













- Slides: 77
AIRWAY ASSESSMENT & MANAGEMENT DR. wael Alham Mahmoud
What should we know about airway management § Airway anatomy and function § Evaluation of airway § Clinical management of the airway § Maintenance and ventilation § Intubation and extubation § Difficult airway management
Airway anatomy The term “airway” refers to the upper airway consisting of § § § Nasal and oral cavities Pharynx Larynx Trachea Principle bronchi
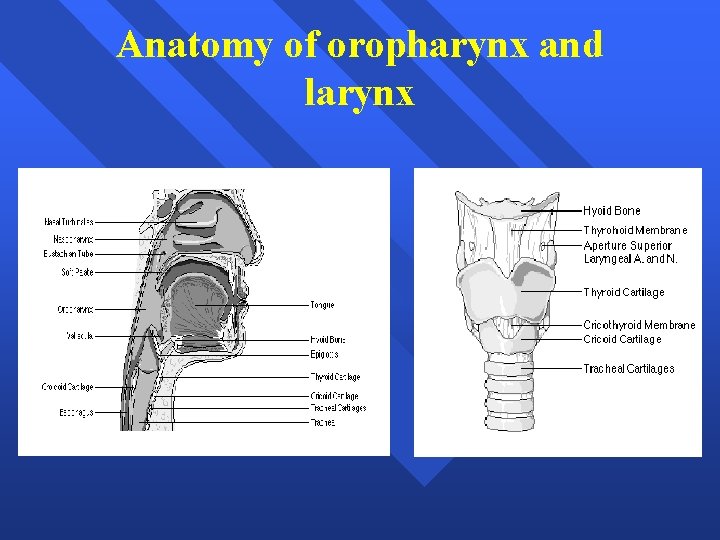
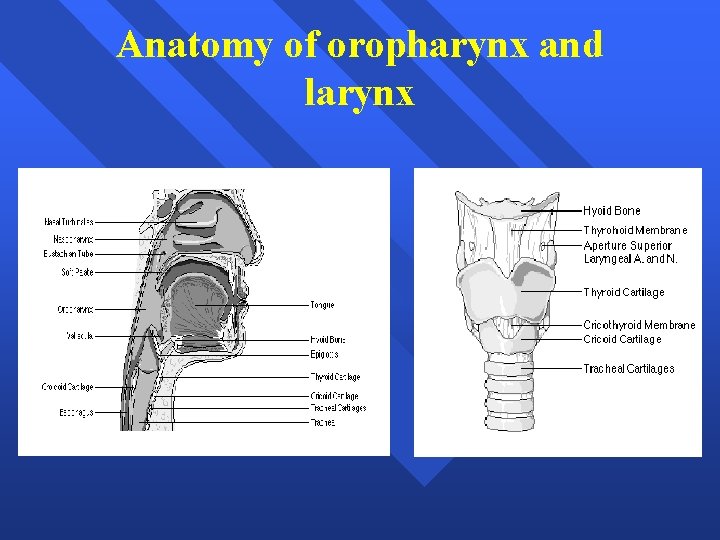
Anatomy of oropharynx and larynx
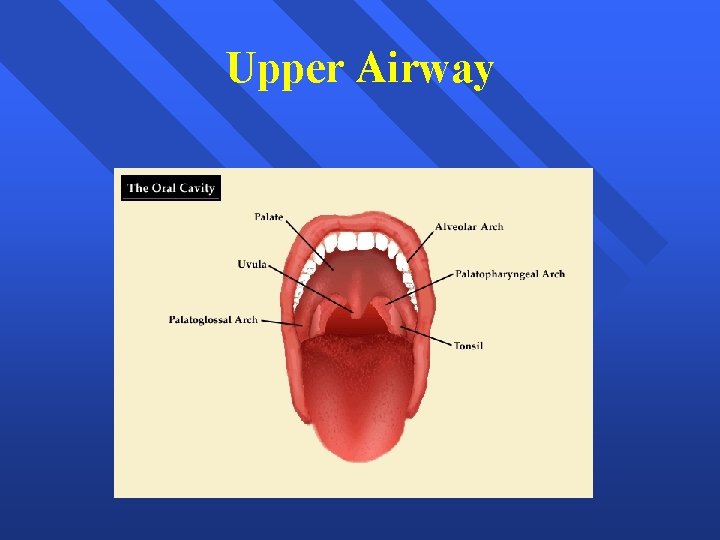
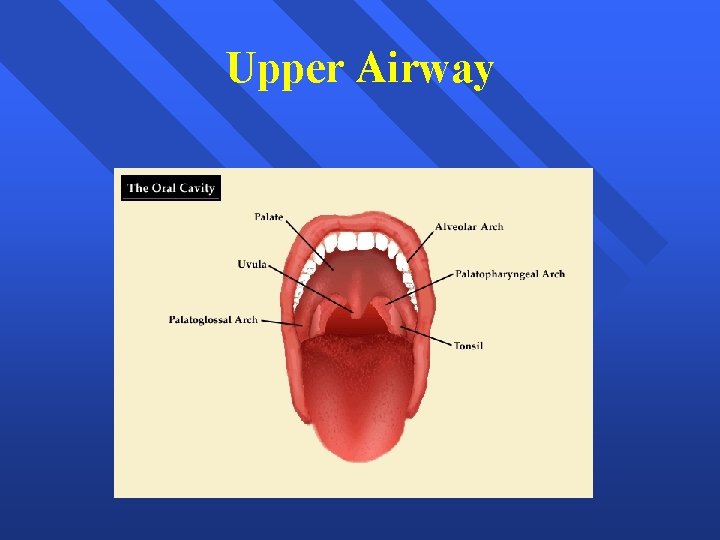
Upper Airway
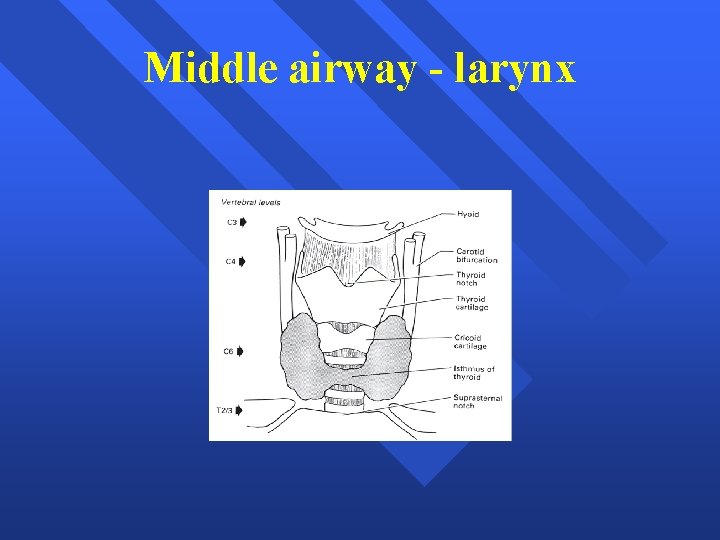
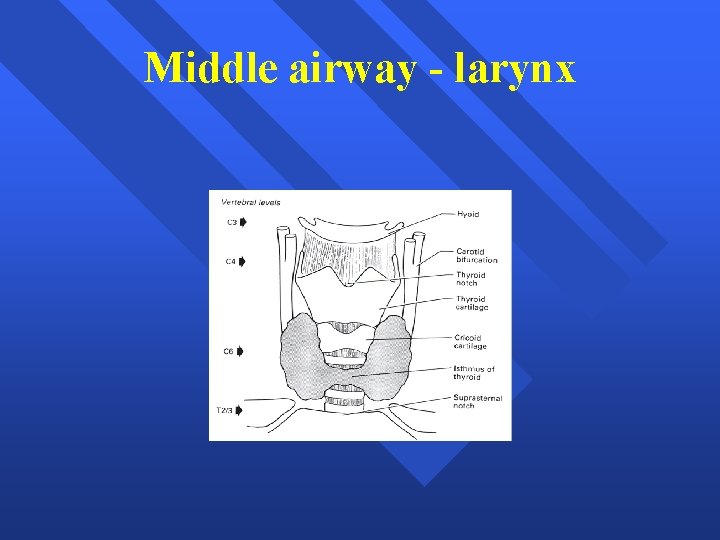
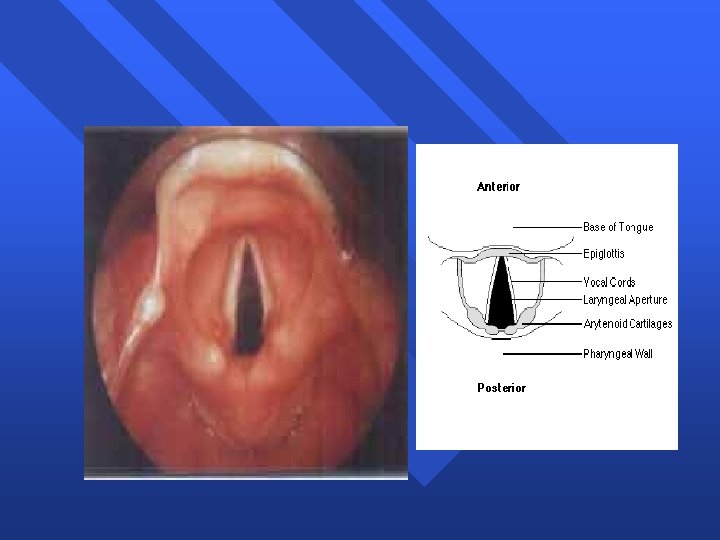
Middle airway - larynx
Larynx § Lies anterior to C 4 – C 6 § Extends from epiglottis to lower level of cricoid cartilage § 3 paired & 3 unpaired cartilages § Cricothyroid membrane bridges between cricoid and thyroid cartilage § Vocal ligament attach to angles of thyroid cartilage anteriorly and arytenoid cartilage posteriorly
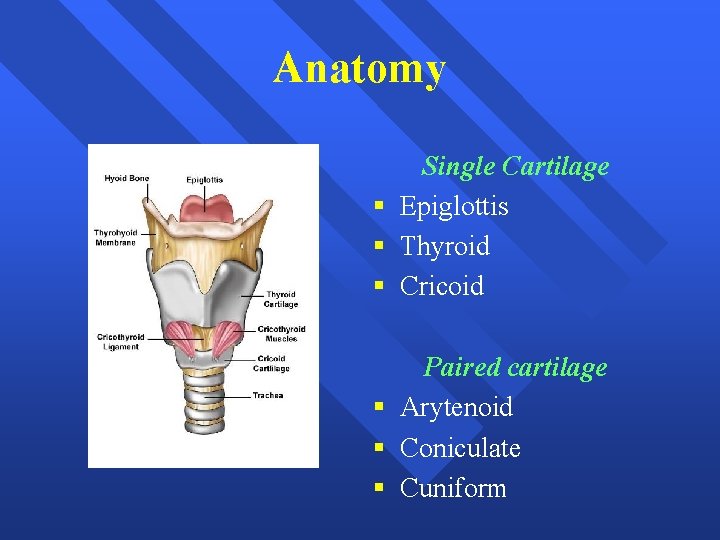
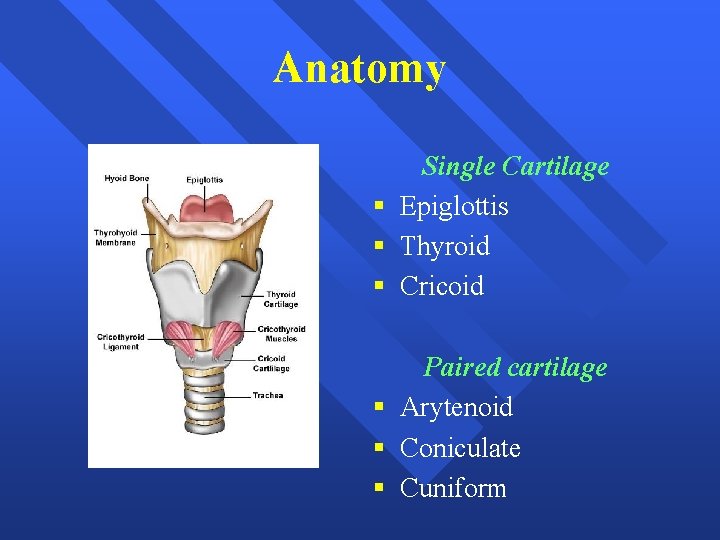
Anatomy Single Cartilage § Epiglottis § Thyroid § Cricoid Paired cartilage § Arytenoid § Coniculate § Cuniform
Nerve supply of airway Motor § All intrinsic muscles of larynx are supplied by Recurrent laryngeal nerve except Cricothyroid (SLN – External branch) Sensory § Pharynx - Glossopharyngeal § Larynx - Vagus (RLN & SLN)
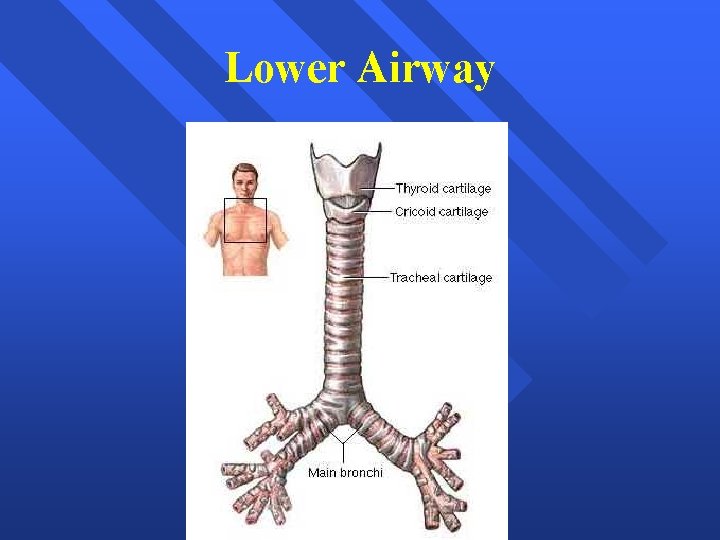
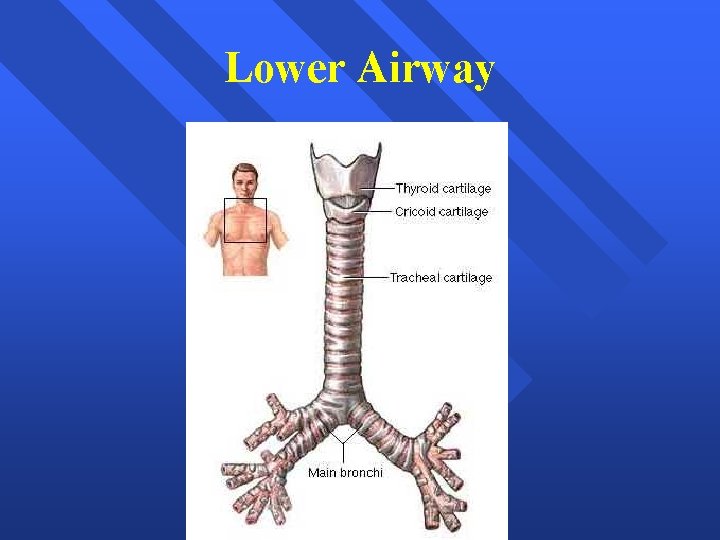
Lower Airway
Airway assessment
Why assessment? § Optimal patient preparation § Proper selection of equipment and technique § Participation of personnel experienced in difficult airway management
First step of success – Pre operative Evaluation § History § Global assessment § Regional assessment
History § Previous surgery – Anaesthetic exposure § Previous difficulty in intubation – documentation § Site of Surgery – neck § Trauma § Tumor in and around oral cavity § Burns § Tracheostomy

History § Hoarseness of voice § Stridor § Snoring § Limited neck movements – cervical spine § Limited mouth opening § Dysphagia
Global assessment § Body stature § Head and Neck examination § Congenital anomalies § Disfigurement of face § Injuries around neck § Pathological & Physiological conditions
Congenital Problems § Pierre Robin syndrome § Treacher Collin syndrome § Goldenhar’s syndrome § Down’s syndrome § Klippel Fiel syndrome
Acquired problems § Infections – Ludwig’s angina, Retropharyngeal abscess § Arthritis – Rheumatoid arthritis, Ankylosing spondylitis § Tumors – Goiter, Cystic hygroma, oral ca. § Trauma – Facio maxillary § Miscellaneous – Diabetes, Obesity, Pregnancy, Burns
Airway assessment § Individual indices § Group indices

For difficult mask ventilation… Individual indices § § § § Presence of beard Obesity Abnormal teeth Elderly Snorers Hairbun Jewelry and facial piercing
For difficult mask ventilation… Group indices - BONES § Beard § Obesity - BMI>26 kg/sq. m § No teeth § Elderly § Snorer

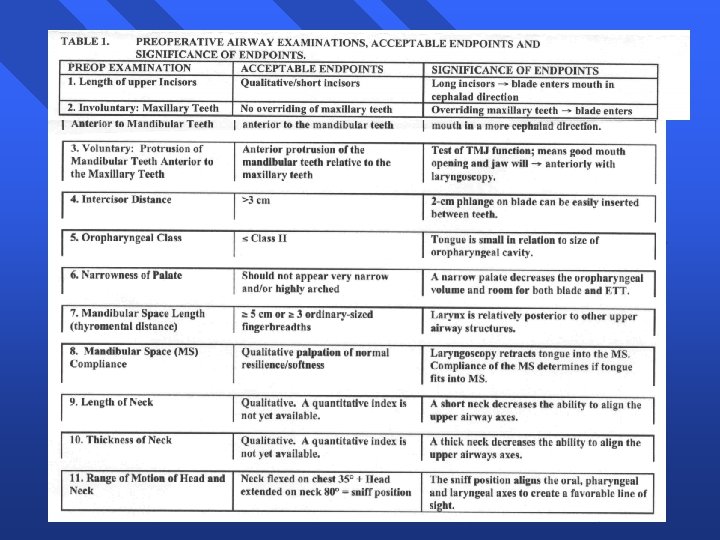
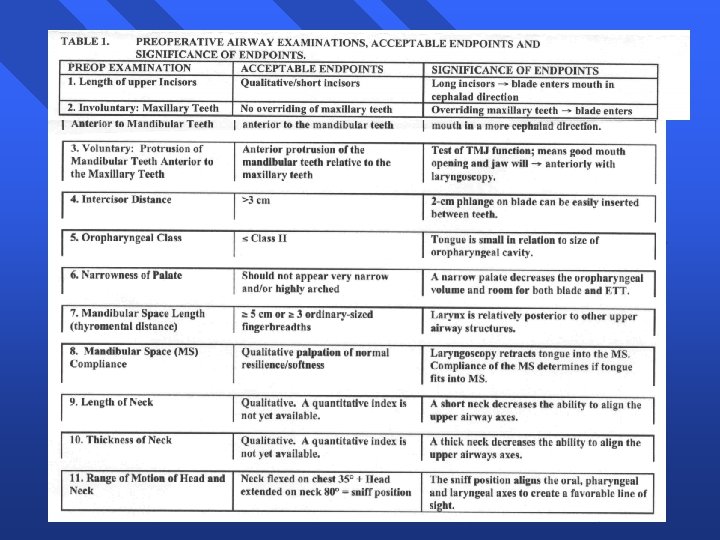
Regional assessment Individual indices for difficult airway § Physical examination indices § Radiological indices § Advanced indices
Physical indices § Mouth opening – Inter incisor gap § Teeth § TMJ function § Mallampati classification and its modification by Samsoon and Young

Physical indices § Patil’s Thyromental distance § Hyo mental distance § Neck movement range § Sternomental distance § Rapid 1 -2 - 3
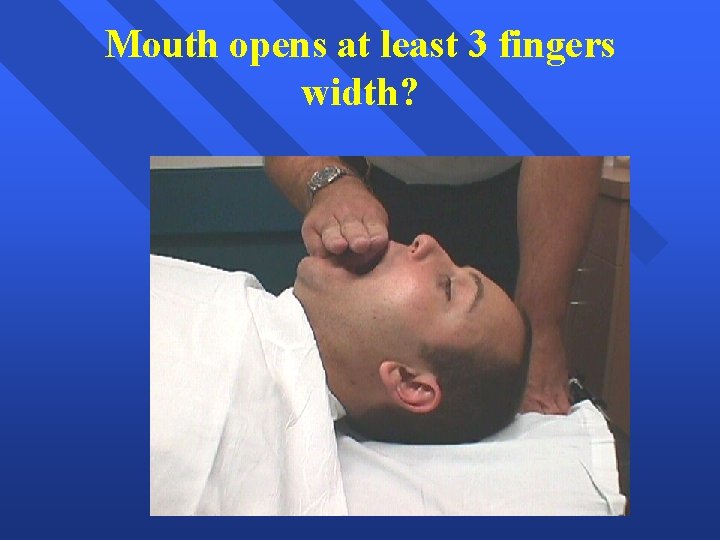
Mouth Opening – Inter incisor gap § < 3 cm - impossible to pass laryngoscope § < 2 cm – impossible to insert LMA
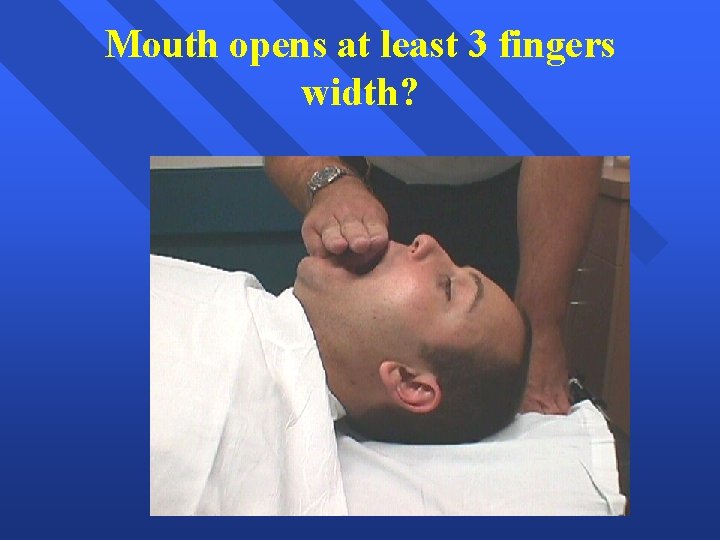
Mouth opens at least 3 fingers width?
Teeth Look for § § Loose teeth Dentures, missing teeth – document Mal alignment Buck teeth Dental injury is GRIEVIOUS so avoid it during laryngoscopy

TMJ function assessment TMJ functions are § Rotation of the condyle in the synovial cavity – Initial mouth opening § Forward displacement of condyle
TMJ function assessment 1. Adequate mouth opening & Interincisor gap > 5 cm 2. Place index finger infront of tragus, thumb in front of lower part of mastoid process behind the ear § Ask the patient to wide open the mouth § Index finger can be indented in space of condyle (sliding) § Thumb can feel sliding movement
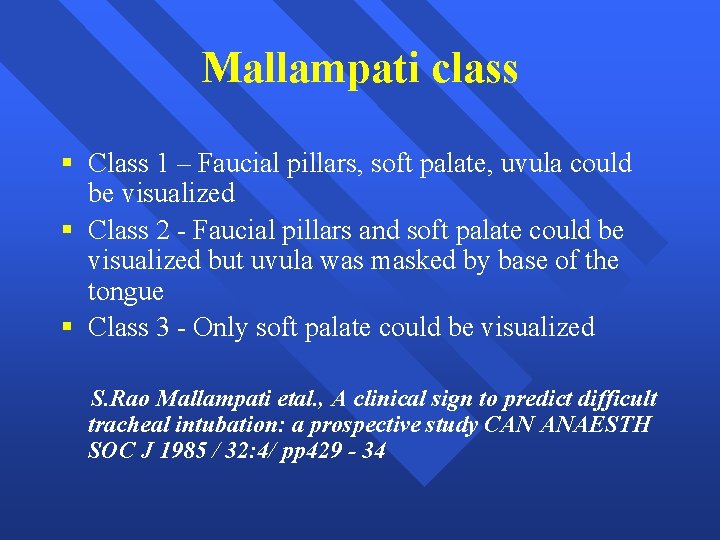
Mallampati classification § Indirect means of assessing the size of the base of the tongue § Predicts the size of the tongue relative to capacity of oropharyngeal cavity
Mallampati class § Class 1 – Faucial pillars, soft palate, uvula could be visualized § Class 2 - Faucial pillars and soft palate could be visualized but uvula was masked by base of the tongue § Class 3 - Only soft palate could be visualized S. Rao Mallampati etal. , A clinical sign to predict difficult tracheal intubation: a prospective study CAN ANAESTH SOC J 1985 / 32: 4/ pp 429 - 34
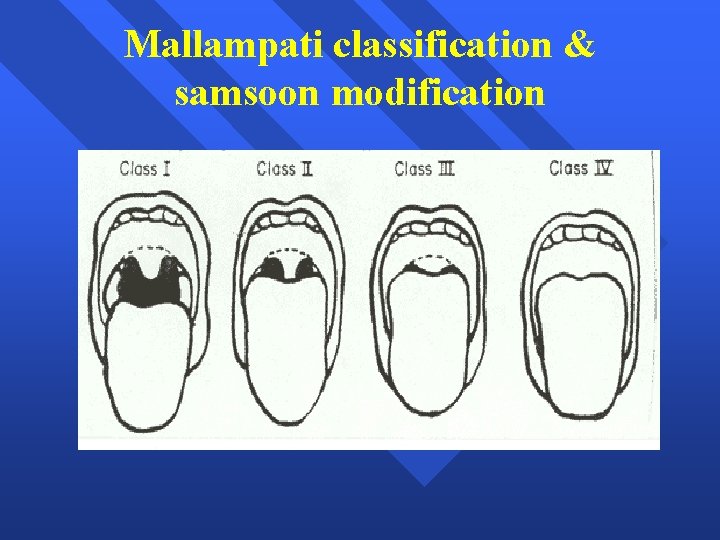
Mallampati classification § Modified by Samson & Young Class 4 – Only hard palate seen § Test has to be repeated twice – to avoid errors § Correlates with Cormack and Lehane grading of glottic view
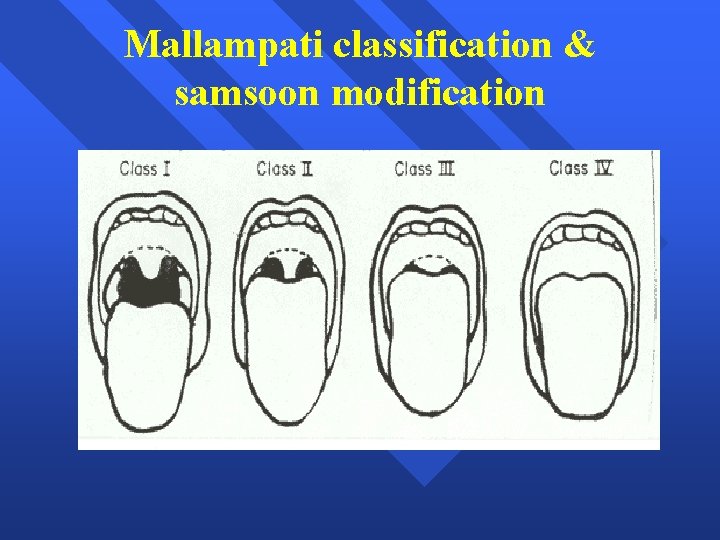
Mallampati classification & samsoon modification
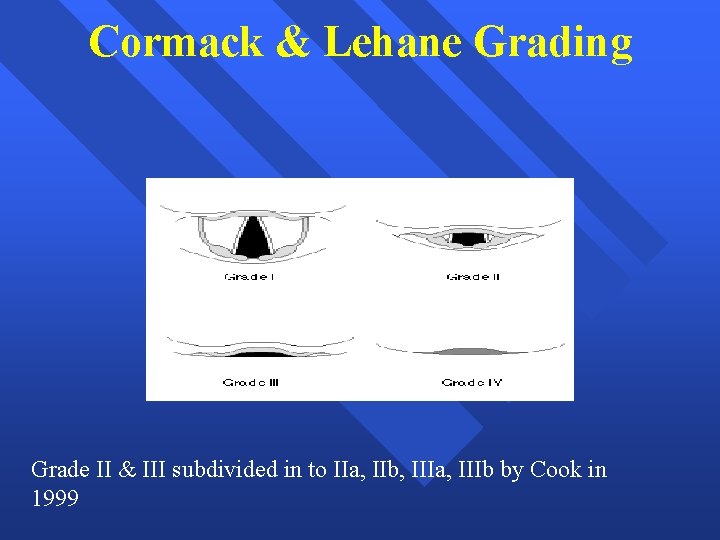
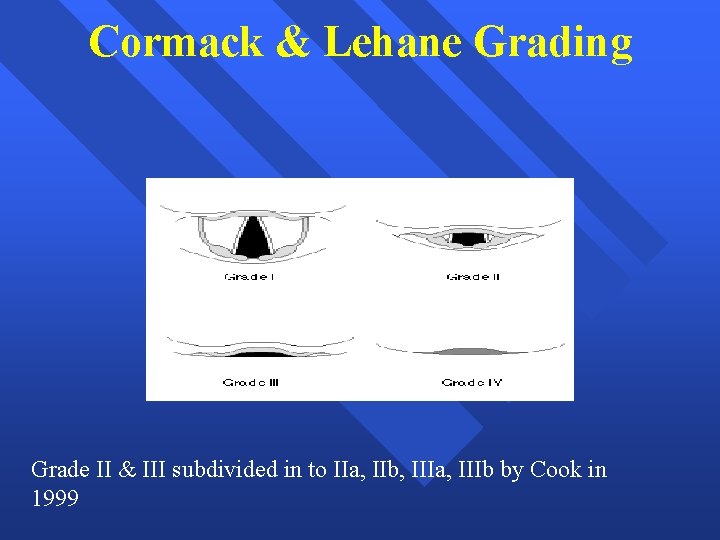
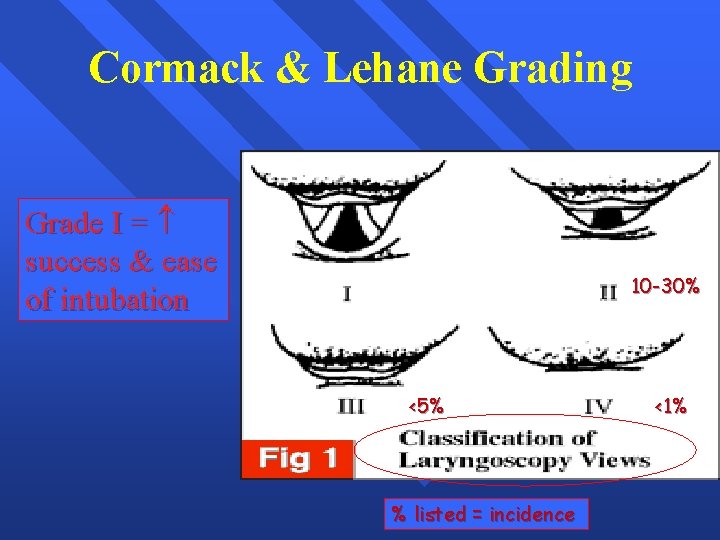
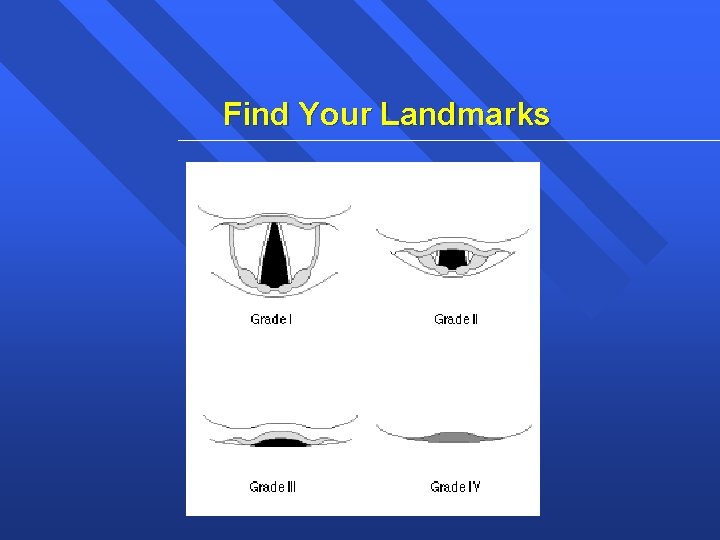
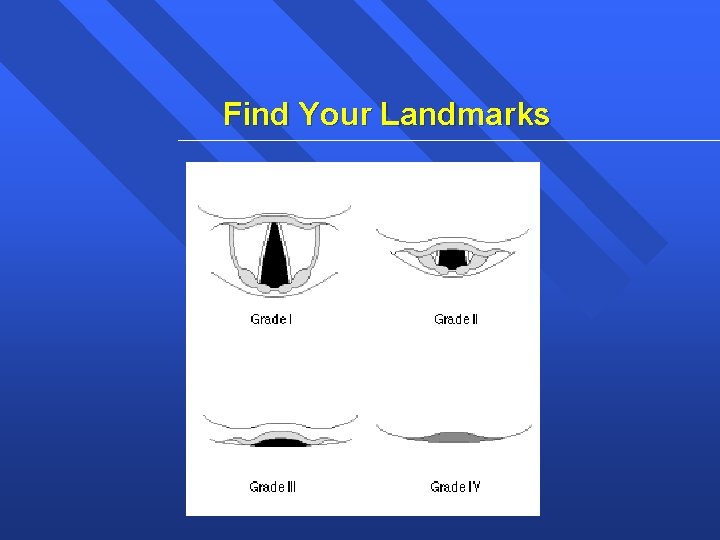
Cormack & Lehane Grading Grade II & III subdivided in to IIa, IIb, IIIa, IIIb by Cook in 1999
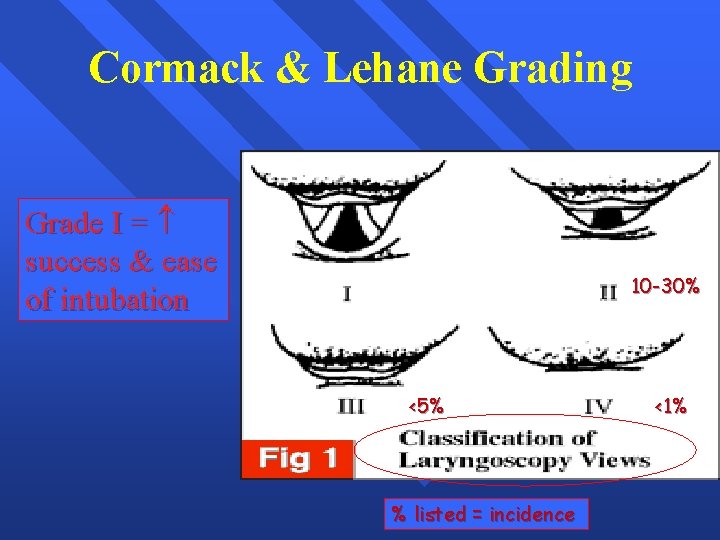
Cormack & Lehane Grading Grade I = success & ease of intubation 10 -30% <5% % listed = incidence <1%
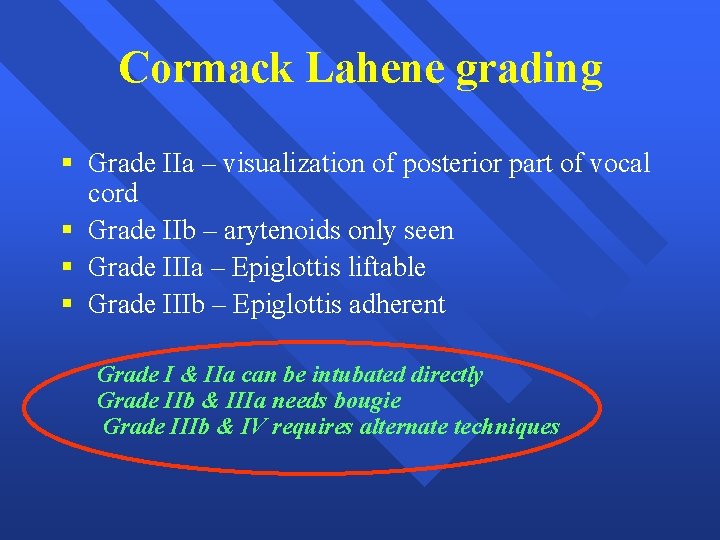
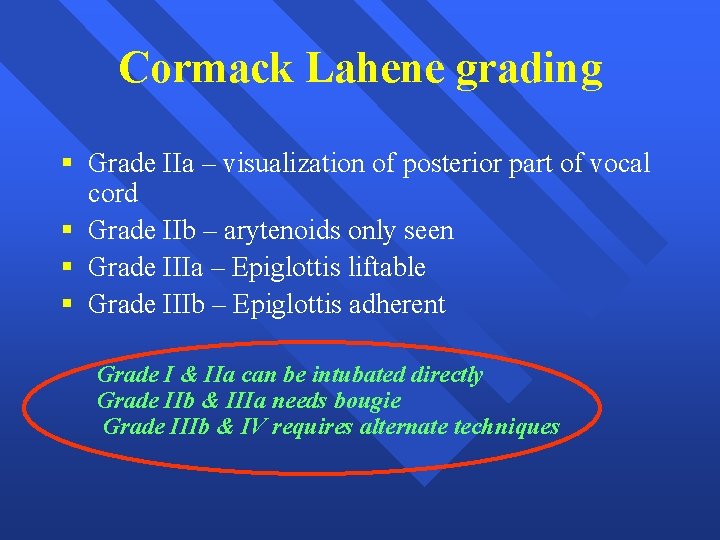
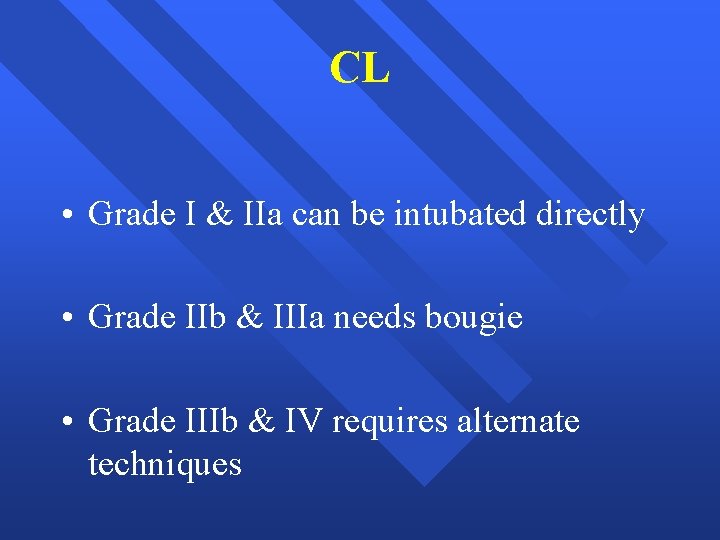
Cormack Lahene grading § Grade IIa – visualization of posterior part of vocal cord § Grade IIb – arytenoids only seen § Grade IIIa – Epiglottis liftable § Grade IIIb – Epiglottis adherent Grade I & IIa can be intubated directly Grade IIb & IIIa needs bougie Grade IIIb & IV requires alternate techniques
Neck movement range assessment – In direct assessment § “Prayer sign” § “Palm print sign”

Dr. Binnions Lemon Law: An easy way to remember multiple tests… § § § Look externally. Evaluate the 3 -3 -2 rule. Mallampati. Obstruction? Neck mobility.

L: Look Externally § § § § § Obesity or very small. Short Muscular neck Large breasts Prominent Upper Incisors (Buck Teeth) Receding Jaw (Dentures) Burns Facial Trauma S/S of Anaphylaxis Stridor FBAO

Keep it open
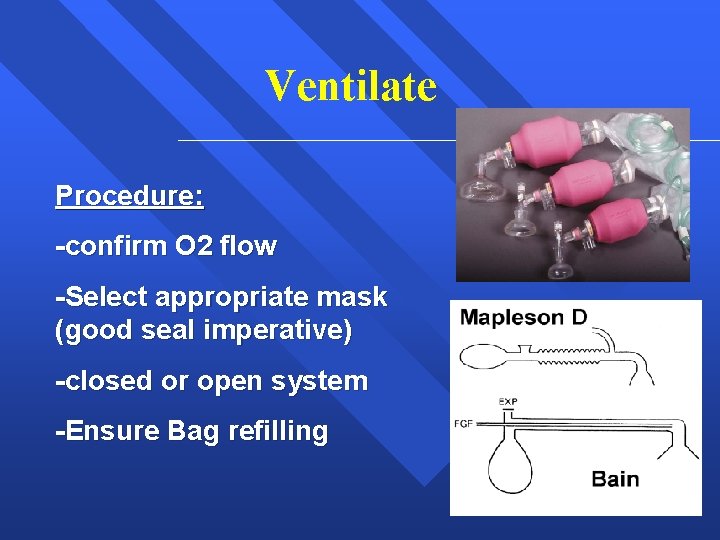
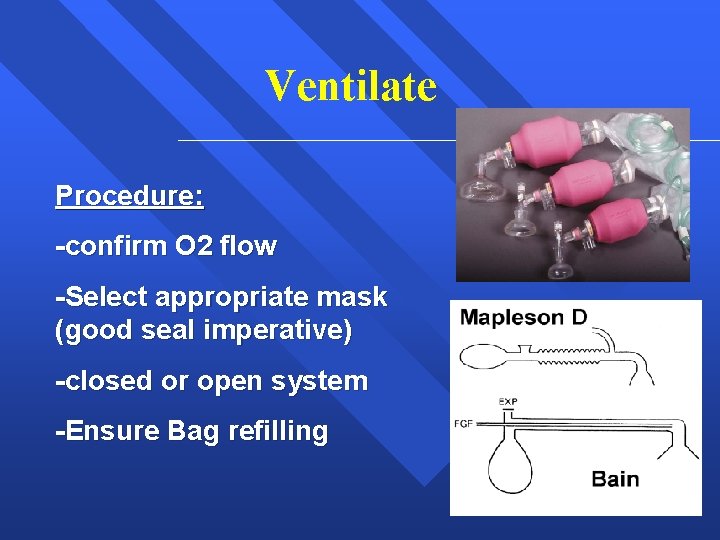
Ventilate Procedure: -confirm O 2 flow -Select appropriate mask (good seal imperative) -closed or open system -Ensure Bag refilling
Adequate Ventilation Approximate normal ventilation rates: § 10 bpm Adult § 20 bpm Child § 25 bpm Infant


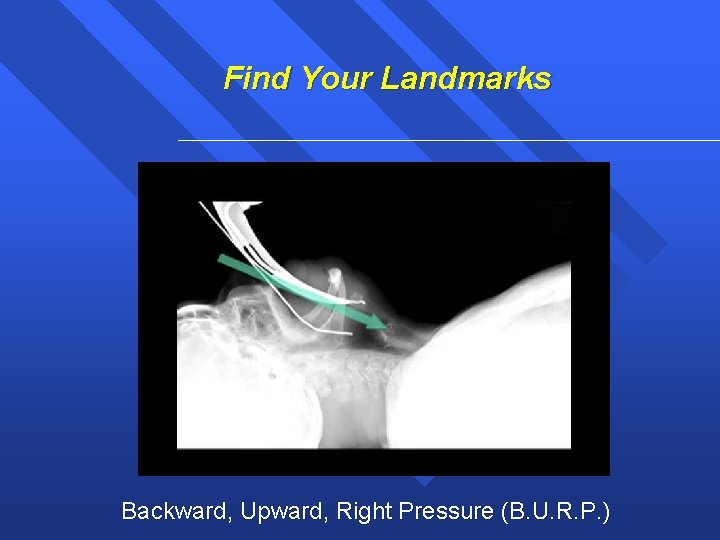
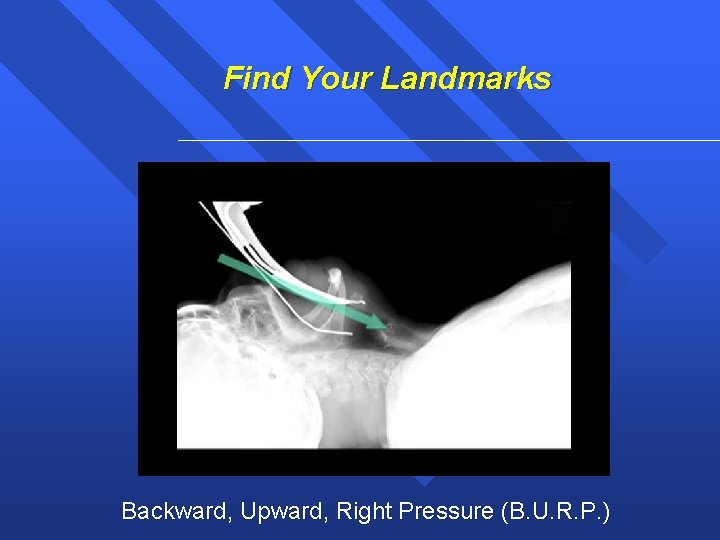
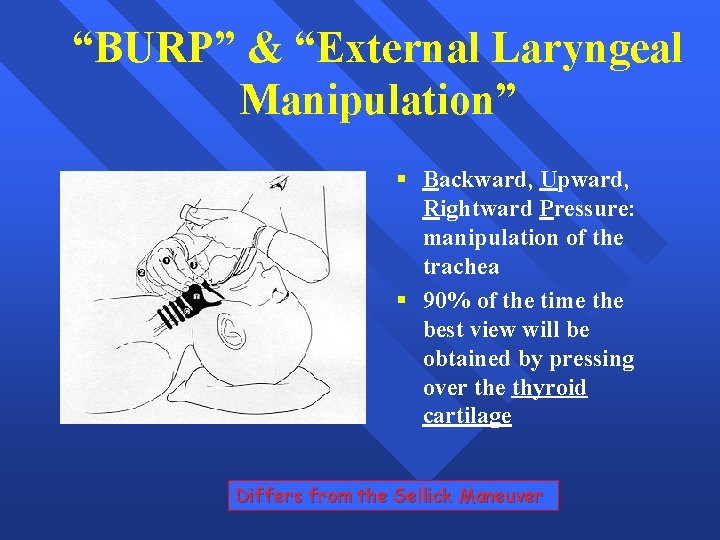
Find Your Landmarks Backward, Upward, Right Pressure (B. U. R. P. )
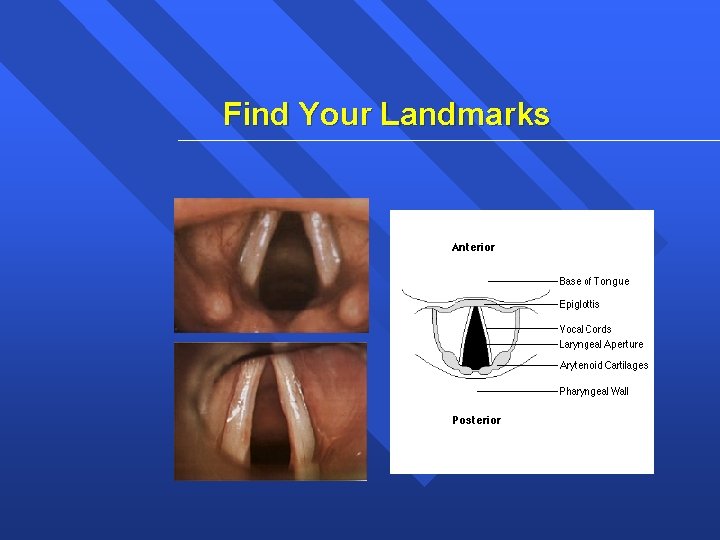
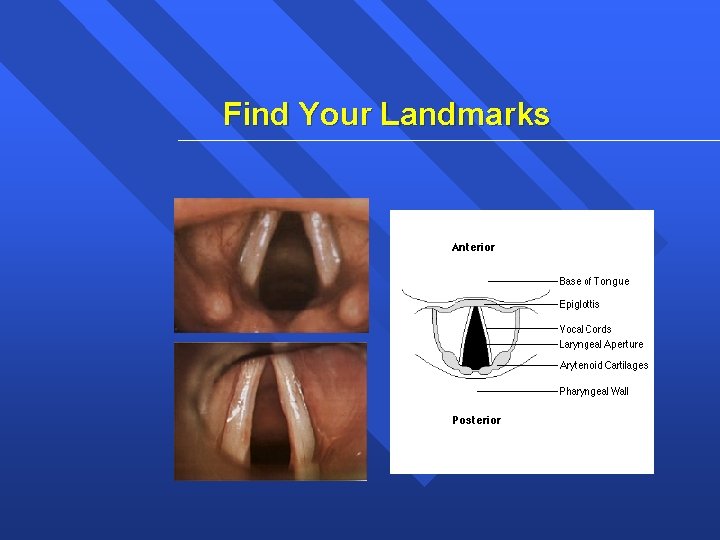
Find Your Landmarks

Find Your Landmarks It may not be perfect!
Find Your Landmarks

CL • Grade I & IIa can be intubated directly • Grade IIb & IIIa needs bougie • Grade IIIb & IV requires alternate techniques
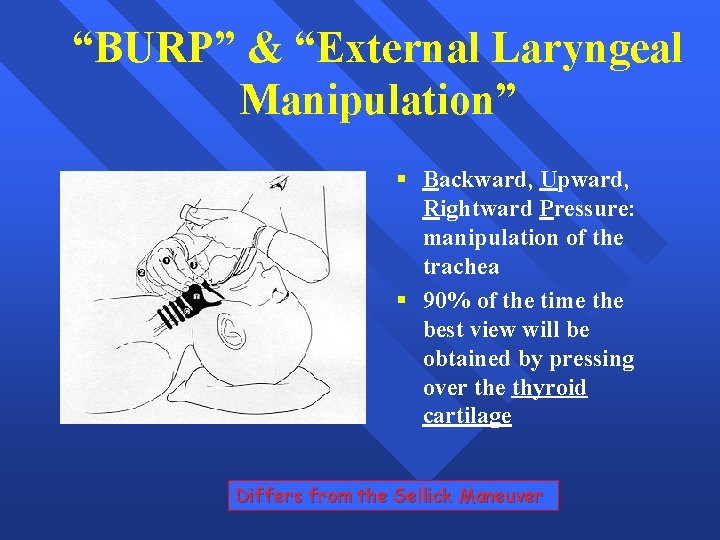
“BURP” & “External Laryngeal Manipulation” § Backward, Upward, Rightward Pressure: manipulation of the trachea § 90% of the time the best view will be obtained by pressing over the thyroid cartilage Differs from the Sellick Maneuver
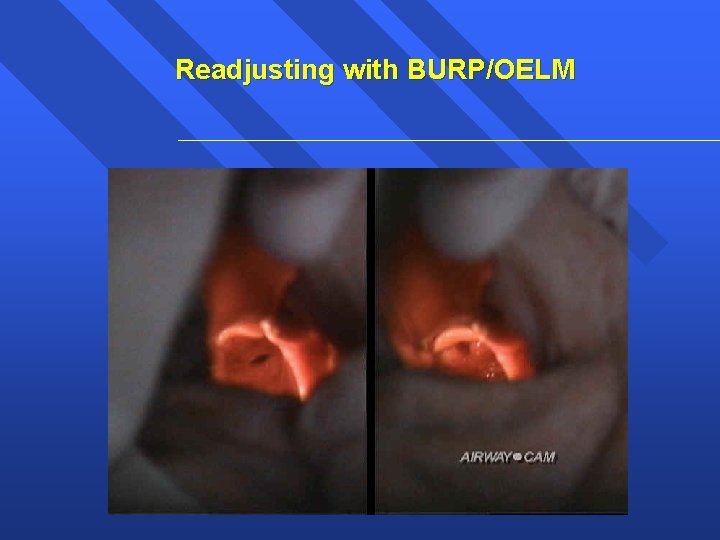
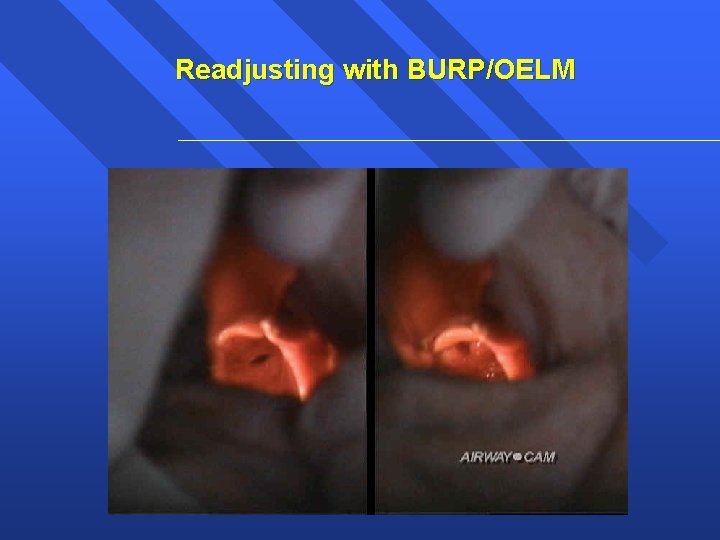
Readjusting with BURP/OELM
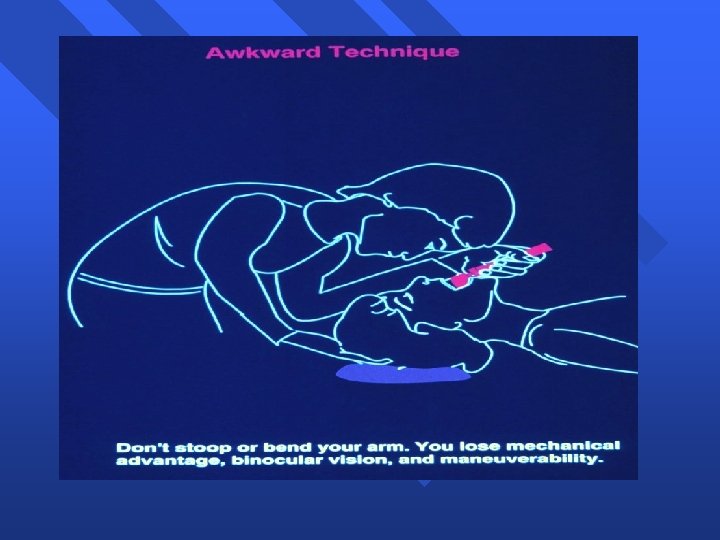
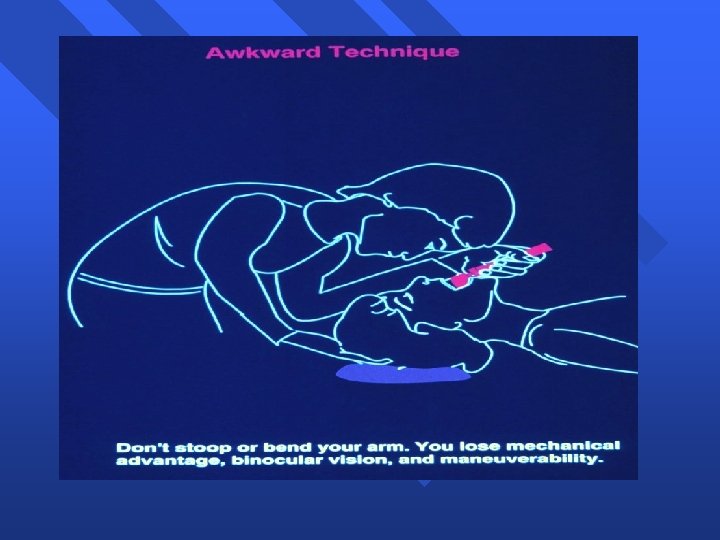
Control the airway Common Provider Mistakes Making a difficult intubation more difficult *Rushing *Poor equipment preparation *Suction (lack there of)
Control the airway What is your back-up plan today? prolonged BVM… another provider… a smaller tube… better lighting… additional suctioning…
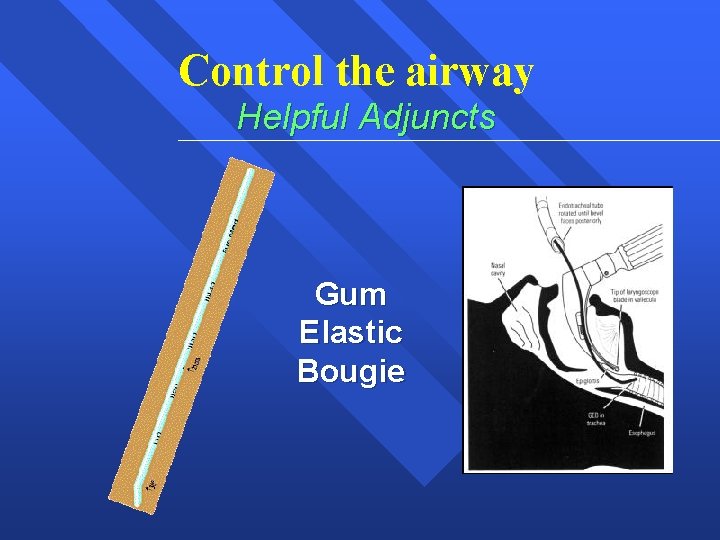
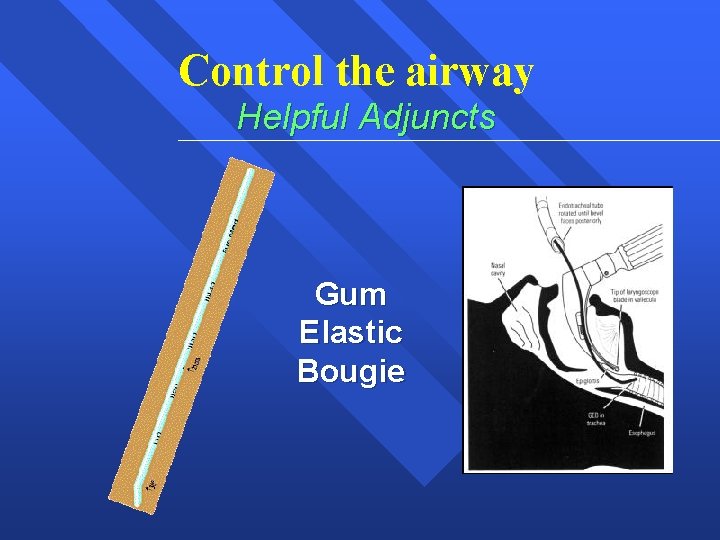
Control the airway Helpful Adjuncts Gum Elastic Bougie
Control the airway Helpful Adjuncts Lighted Stylette
Complications Of Orotracheal Intubation (During) • Dental And Oral Soft tissue Trauma • Hypertension And Tachycardia • Cardiac Dysrhythmias And Myocardial Ischemia • Aspiration • Corneal Damage
Complications Of Orotracheal Intubation (Intubated Patient) • • • Tracheal Tube Obstruction Endobronchial Intubation Barotrauma Accidental Disconnect Tracheal Mucosa Ischemia Accidental Extubation
Control the airway Nasotracheal Intubation Indications: “Patient still breathing but in respiratory failure and in whom oral intubation is impossible or difficult. ”
Nasotracheal Intubation Contraindications: -Apnea -Resistance in the nares -Blood clotting or anticoagulation problems -Basal Skull Fx (? )
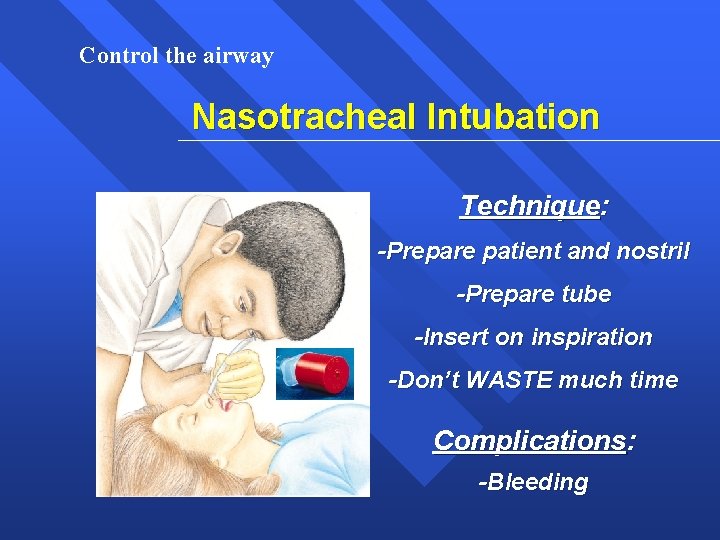
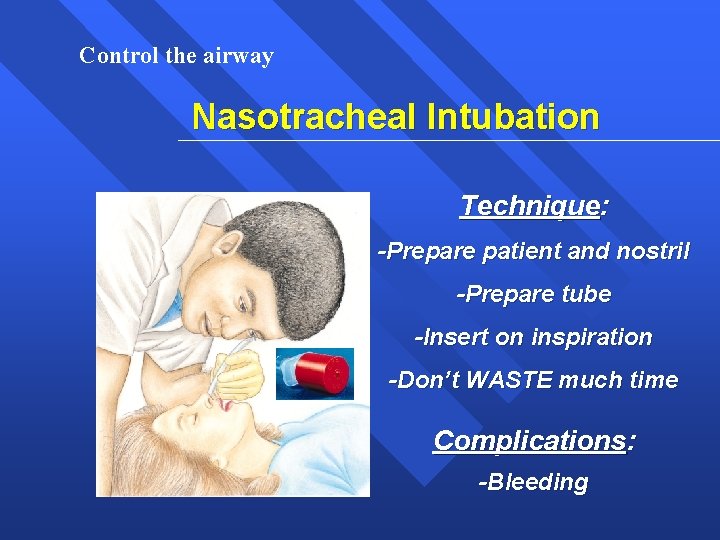
Control the airway Nasotracheal Intubation Technique: -Prepare patient and nostril -Prepare tube -Insert on inspiration -Don’t WASTE much time Complications: -Bleeding
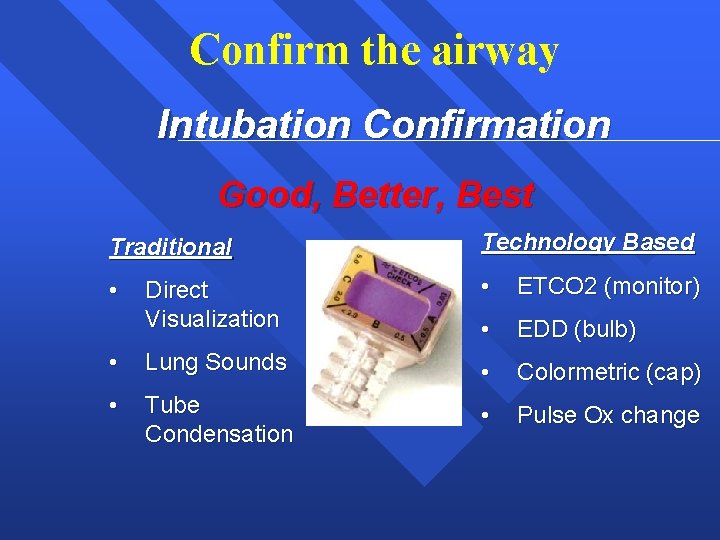
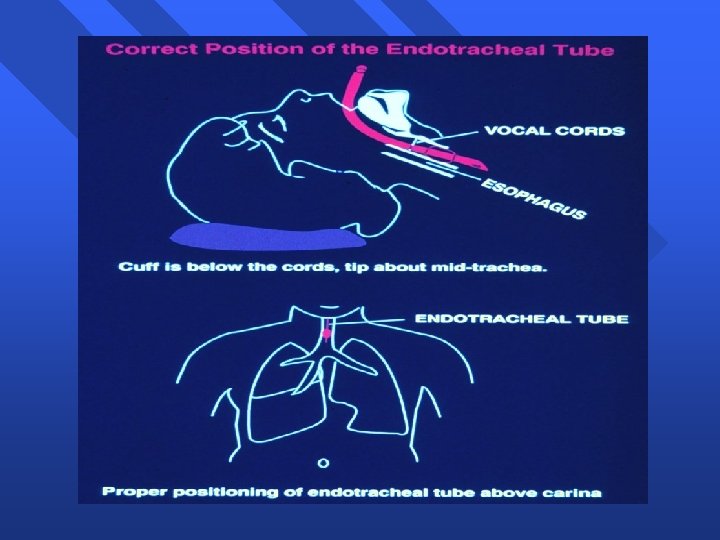
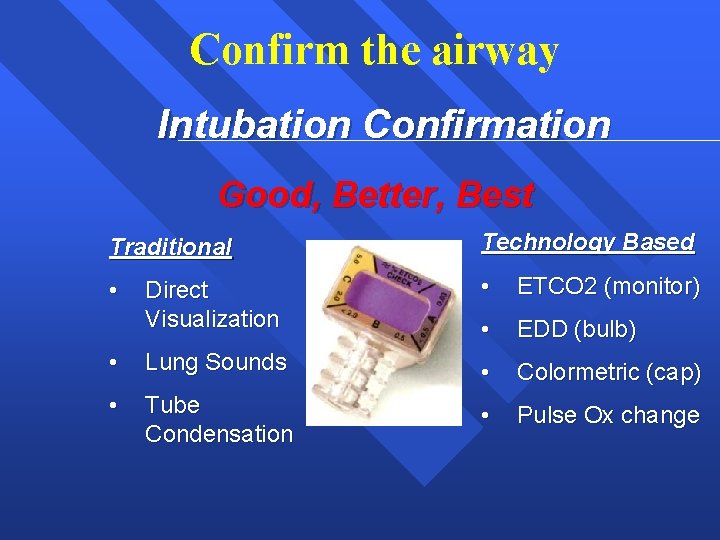
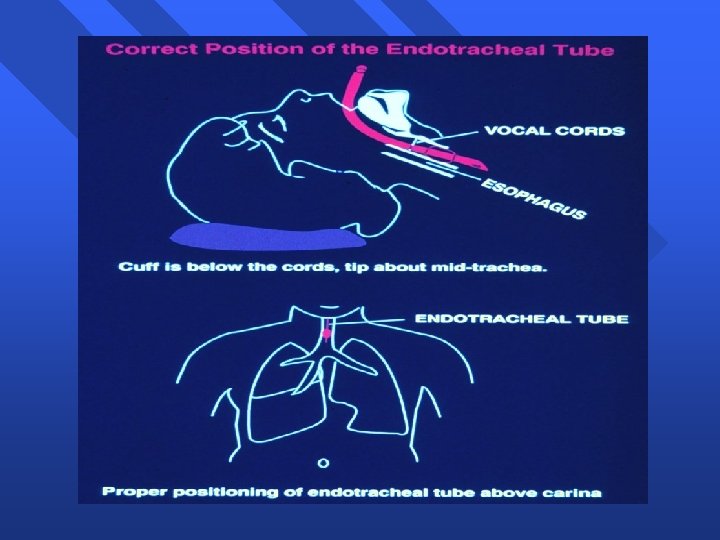
Confirm the airway Intubation Confirmation Good, Better, Best Traditional Technology Based • Direct Visualization • ETCO 2 (monitor) • EDD (bulb) • Lung Sounds • Colormetric (cap) • Tube Condensation • Pulse Ox change
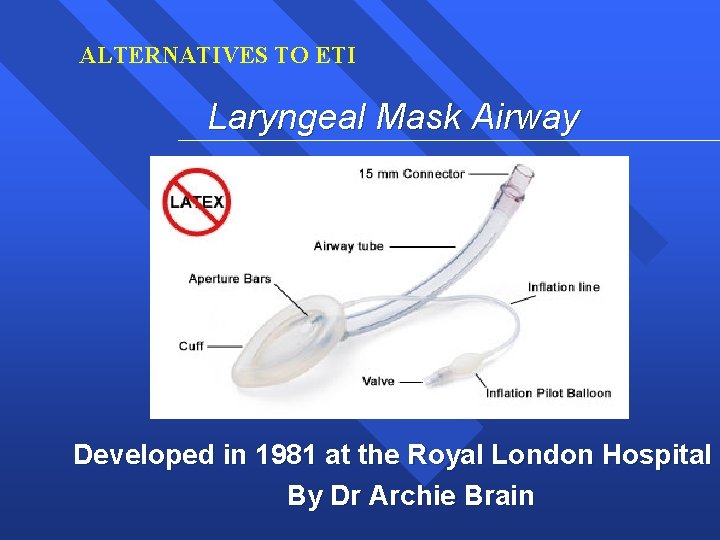
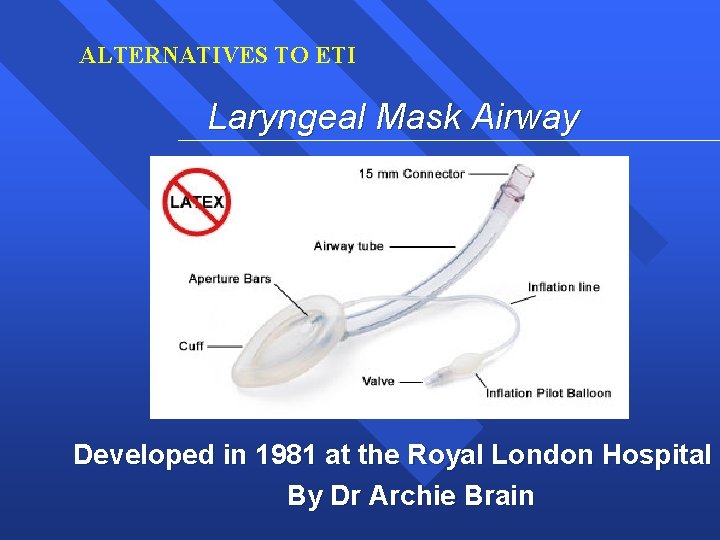
ALTERNATIVES TO ETI Laryngeal Mask Airway Developed in 1981 at the Royal London Hospital By Dr Archie Brain
ALTERNATIVES TO ETI Laryngeal Mask Airway Indications: -When definitive airway management cannot be obtained. (ETT) Not a substitute for definitive airway management
ALTERNATIVES TO ETI Laryngeal Mask Airway Contraindication/Limitations: -Obesity -Non-secure -Size based -Not a med route
Difficult airway
Key to success § Anticipation § Preparation § Recognition § Correct and accurate decision in an emergency situation § Mandatory to know how to tackle a failed intubation
Key to success § Understanding airway anatomy § Anticipation of difficult airway § Familiarization of various techniques Muscle relaxants had made intubation easy but also failure to intubate in to a serious problem
Difficult airway § Anticipated difficult airway § Unanticipated difficult airway § Normal airway made difficult

Difficult airway “A clinical situation in which conventionally trained anaesthesiologists experiences difficulty with mask ventilation, tracheal intubation or both”
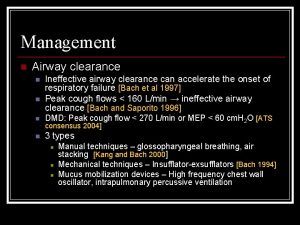
Difficult Mask Ventilation “The clinical situation where using 100% oxygen and bag/valve/mask ventilation, an unassisted anaesthesiologist is unable to maintain oxygen saturation greater than 90% in a person who was capable of doing so before intervention”
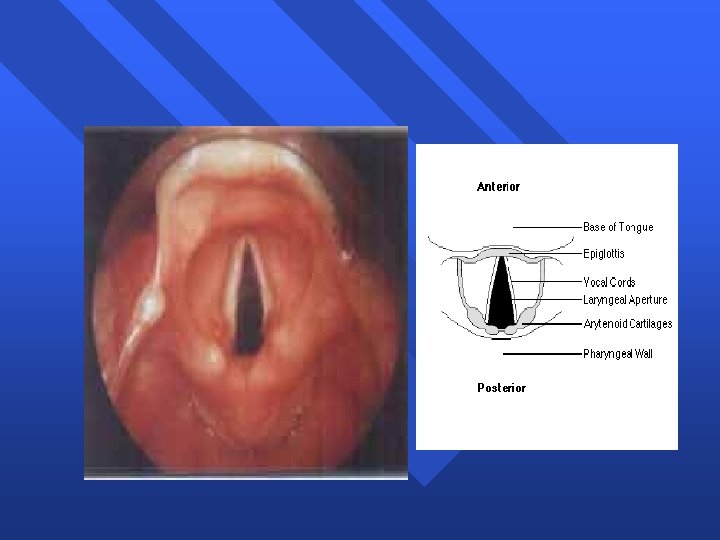
Difficult laryngoscopy “It is not possible to visualize any portion of vocal cords with conventional laryngoscope”
Difficult Endotracheal Intubation “Using conventional laryngoscopy, it requires more than three attempts or more than 10 min. for proper positioning of endotracheal tube”
 Laryngoscopy view grades
Laryngoscopy view grades Wael ouarda
Wael ouarda Wael is the teacher of n students
Wael is the teacher of n students Exposition of the fly by katherine mansfield
Exposition of the fly by katherine mansfield 332 rule intubation
332 rule intubation What is gag reflex mean
What is gag reflex mean Larangoscopy
Larangoscopy Tatalaksana acls
Tatalaksana acls Chapter 10 airway management
Chapter 10 airway management Supraglotal
Supraglotal Chapter 9 airway management
Chapter 9 airway management Airway abcde
Airway abcde Sandwich manuver adalah
Sandwich manuver adalah Stepwise approach to airway management
Stepwise approach to airway management Mahmoud abdelfattah age
Mahmoud abdelfattah age The passport poem by mahmoud darwish
The passport poem by mahmoud darwish Dr mahmoud salman
Dr mahmoud salman Mahmoud arafa
Mahmoud arafa Mahmoud boudarene
Mahmoud boudarene Mahmoud sarmini md
Mahmoud sarmini md Adp antagonist drugs
Adp antagonist drugs Mahmoud khattab md
Mahmoud khattab md Hana mahmoud
Hana mahmoud Lower respiratory structures
Lower respiratory structures Air path through the respiratory system
Air path through the respiratory system Respiratory airway secretary
Respiratory airway secretary King airway
King airway Grade view intubation
Grade view intubation Statics persiapan intubasi
Statics persiapan intubasi Mean airway pressure
Mean airway pressure Mean airway pressure
Mean airway pressure Krikotiroid membran
Krikotiroid membran Mallampati score intubation
Mallampati score intubation Airway
Airway Mean airway pressure formula
Mean airway pressure formula Ahi cpap
Ahi cpap Mild foreign-body airway obstruction
Mild foreign-body airway obstruction Airway numaraları
Airway numaraları Asa airway classification
Asa airway classification Aprv indications
Aprv indications Intubating lma
Intubating lma Pharyngo-tracheal lumen airway
Pharyngo-tracheal lumen airway Valeculla
Valeculla Sniffing position for intubation
Sniffing position for intubation Nursing process sequence
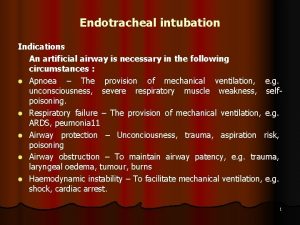
Nursing process sequence Indications for artificial airway
Indications for artificial airway 3 emergency action steps
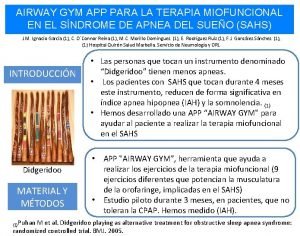
3 emergency action steps Airway gym app
Airway gym app A airway b breathing c circulation
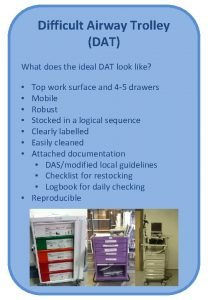
A airway b breathing c circulation Difficult airway trolley
Difficult airway trolley Norwich terrier upper airway syndrome
Norwich terrier upper airway syndrome Moans airway
Moans airway Asa airway fire algorithm
Asa airway fire algorithm Generations of supraglottic airway devices
Generations of supraglottic airway devices Thyromental distance
Thyromental distance Nasopharyngeal airway
Nasopharyngeal airway Bronchiole
Bronchiole Asa airway
Asa airway Mouth gag airway
Mouth gag airway Open a casualty's airway
Open a casualty's airway Abcde ehbo
Abcde ehbo Mellampati
Mellampati Education outside the classroom
Education outside the classroom Constricted airway
Constricted airway Penumothorax
Penumothorax Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching Static assessment vs dynamic assessment
Static assessment vs dynamic assessment Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching Scientific management
Scientific management Top management middle management first line management
Top management middle management first line management Top level management
Top level management Www.texas assessment.com
Www.texas assessment.com Framp tool
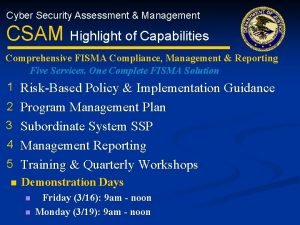
Framp tool Cyber security assessment and management
Cyber security assessment and management Chapter 4 the internal assessment (strategic management)
Chapter 4 the internal assessment (strategic management) External assessment in strategic management
External assessment in strategic management The external assessment in strategic management
The external assessment in strategic management National asset management assessment framework
National asset management assessment framework