Innovating Healthcare Delivery Dr Nicolaus Henke HFMA 17
































- Slides: 32

Innovating Healthcare Delivery Dr. Nicolaus Henke HFMA 17 November 2015

What I will talk about today Last Modified 17/11/2015 12: 10 GMT Standard Time Challenges Printed 21/01/2015 15: 19 GMT Standard Time Plan A Plan B | 1 Mc. Kinsey & Company

Healthcare has been a great success story of the past century …… Life expectancy in EU-5 and U. S. Years Last Modified 17/11/2015 12: 10 GMT Standard Time Printed 21/01/2015 15: 19 GMT Standard Time Source: OECD. Mc. Kinsey & Company | 2

… But there a whole set of challenges facing healthcare systems globally People globally with diabetes People globally who suffer a complication as a result of surgery 0. 6% Average annual reduction in US healthcare productivity since 1990 compared to 2. 9% average annual growth in the workforce Printed 21/01/2015 15: 19 GMT Standard Time 7 m Last Modified 17/11/2015 12: 10 GMT Standard Time 347 m 1/3 Of people with a long-term condition don’t know how to manage it Mc. Kinsey & Company | 3

Not to mention the money! < 10 10 -20 > 20 Share of health care costs as percentage of GDP 2015 2030 2050 Last Modified 17/11/2015 12: 10 GMT Standard Time 2008 2080 5. 9 6. 7 8. 9 14. 4 25. 7 Spain 7. 8 8. 9 11. 7 19. 6 35. 2 UK 9. 3 10. 6 14. 0 19. 9 35. 6 Italy 8. 8 10. 0 13. 2 21. 3 38. 2 Australia 10. 5 15. 8 22. 8 40. 8 Canada 10. 8 12. 3 16. 2 23. 5 42. 0 Germany 10. 8 12. 3 16. 2 25. 6 45. 9 France 11. 2 12. 7 16. 8 26. 6 47. 6 USA 16. 1 18. 3 24. 2 36. 7 65. 6 Printed 21/01/2015 15: 19 GMT Standard Time Korea 1 Assumptions: GDP growth of 2% (OECD-Prognosis 2000 - 50). Health care spending grows 1. 9 basis points faster (OECD historical rate) SOURCE: OECD Policy Implications of the New Economy 2000 - 50 (2001); Global Insight WMM 2000 - 37; Espicom: World Pharmaceutical Fact Book 2008; International Monetary Fund. World Economic Outlook Database. October 2009; Espicom: World Pharmaceutical Fact Book 2008; Mc. Kinsey & Company | 4

What I will talk about today Last Modified 17/11/2015 12: 10 GMT Standard Time Challenges Printed 21/01/2015 15: 19 GMT Standard Time Plan A Plan B | 5 Mc. Kinsey & Company

Focus on cost and driving value Last Modified 17/11/2015 12: 10 GMT Standard Time Macroeconomics (reduced individual spend) Squeeze spend Reduced funding/ flat spending growth Pay freezes Printed 21/01/2015 15: 19 GMT Standard Time Provider efficiencies Reduced drug costs Redesign the system Health checks & proactive LTC management Strengthened gate keeping Mc. Kinsey & Company | 6

Productivity is (almost) everything Historical Funding pressures on the NHS in England (~4%)1 Real terms freeze Funding £b £ 9 bn gap in 2013/14 closed by: ▪ Pay freeze ▪ Lower investment ▪ Productivity quick wins 2015/16 position additionally challenged by £ 1. 9 bn transfer of funds from CCGs to LAs for ITF £ 1. 5 bn procurement efficiencies expected by 2015/162 2014 PPRS to freeze spend on branded medicines 2014 -16 then 2% growth p. a. 2017 -2018. Savings potential of ~£ 5 bn to 2018 versus historic trend Last Modified 17/11/2015 12: 10 GMT Standard Time Real terms freeze through 2014/15 followed by increase with real GDP (2. 4%) £ 28 b Printed 21/01/2015 15: 19 GMT Standard Time £ 44 b £ 15 b £ 9 b 2010/11 11/12 12/13 13/14 14/15 15/16 16/17 17/18 18/19 19/20 20/21 2021/22 1 The forecast spend assumes pressures continue to rise in line with patterns observed prior to 2010/11 and that policy-makers and managers take no action to improve efficiency and reduce costs. This estimate is based on the rising pressures on the NHS from 1) Demographics (principal population projection from ONS), 2) Health care activity (Chronic demands on acute 04/05 -09/10; MH 08 -10/11; primary care 95/96 -08/09; prescribing 08/09 -11/12) and 3) Health care costs (Pay 2% a year over GDP deflator; drugs in line with GDP). Assumes NHS funding continues to grow with inflation (GDP deflator) 2 £ 1. 5 bn procurement savings, from annual £ 20. 6 bn non-pay spend, target set by Dept of Health/NHS England in August 2013 SOURCE: Nuffield Trust: The funding pressures facing the NHS from 2010/11 to 2021/22: A decade of austerity? ; Better procurement, better value better care: a procurement development programme for the NHS, DH, 2013 Mc. Kinsey & Company | 7

Follow the money X Primary prevention Demand a management Technical efficiency Bold-stretch scenario Net savings, £bn, FY 20/21 2 Primary prevention (e. g. , smoking, sexual health, . . . ) Integrated care 1 3 Self-care 0. 2 1. 8 4 0. 9 6 Screening Stop using low-value interventions, and procedures Avoid adverse effects due to drugs 0. 3 0. 5 7 Shift activity to lower cost settings 8 Acute care efficiency 1 9 Primary care efficiency 1 5 10 Community care efficiency 1. 0 2. 1 1. 5 3. 0 0. 9 3. 6 7. 3 1. 5 2. 6 1. 1 1. 4 12 Estate efficiency 0. 4 Total opportunity 7. 4 10. 1 11 Mental Health efficiency Overlap 2 1. 4 1. 5 1. 7 11. 7 0. 9 1. 0 2. 3 15. 6 24. 9 16. 7 1 Length of stay reduction included in both integrated care and acute care efficiency. Double counting removed in “overlap” 2 Overlap includes both double counting on Lo. S and adjustment for productivity savings applied to avoided demand 3 Based on applying all levers in category together. May differ from sum of levers because of internal overlap (e. g. , Lo. S compounding on the effect of activity shift). Includes overlapping between categories SOURCE: Monitor ‘Closing the Gap’, NHSE ‘Digital Enablement’, Monitor Evidence for the 2015/16 national tariff efficiency factor, Team analysis Mc. Kinsey & Company | 8 Printed 21/01/2015 15: 19 GMT Standard Time Provider b productivity Activity management Medium-stretch scenario Net savings, £bn, FY 20/21 Last Modified 17/11/2015 12: 10 GMT Standard Time Improvement levers Total by type of lever 3 PRELIMINARY WORK IN PROGRESS VALUES

Nursing productivity A Scope to improve nursing productivity by decreasing noncore B Scope to improve nursing productivity by adjusting staffing to workload 2 Workload score (high score = high workload per bed) 100 Last Modified 17/11/2015 12: 10 GMT Standard Time activities % of nurse time spent 1 Ward 12: CICU 20 Ward 3 Ward 10 Ward 11: Angio -66% Ward 8: CCU Ward 2 Ward 7 Ward 5 Ward 6 Ward 4 Ward 1 Total Motion Admin Handschedovers uled time Medicines mgt. Dis. Per. Patient Other cussion sonal flow hygiene Ward 9 Printed 21/01/2015 15: 19 GMT Standard Time Wards with different workloads have same staffing ratios Wards with similar workloads have different staffing ratios Direct care Increasing direct care time to 44% would release 10% of total nursing costs Nurses/bed Established WTE/bed Moving to average Nurse per Bed ratio for clusters of wards with similar workload per bed in all Divisions would release 5% of total nursing costs 1 Typical band 5 nurse; based on 12 -hour observation in each ward; average across 3 wards 2 Relative workload per bed estimated by Head Nurse of the Division; shows 12 wards within Renal & Cardiovascular Department at large teaching hospital SOURCE: Anonymised example Mc. Kinsey & Company | 9

Shifting care Exit the marke Lose volume Gain volume 832 units of elective activity move to lower cost settings 3. 6 3. 1 2. 7 ▪ 3. 2 The local health economy total cost for complex elective surgery is reduced from £ 11. 4 m to £ 10 m (-13%)4 2. 7 ▪ 0. 9 The two least efficient trusts, Trusts H and I, exit the market ▪ Printed 21/01/2015 15: 19 GMT Standard Time £k/ activity This assumes each hospital has 15% additional capacity Activity Trust A Trust B Trust C Trust D Trust E Trust G Trust I Trust F Trust H 1 Assumes quality outcome is the same in each hospital (i. e. , does not account for local unit cost being due to poor care) 2 Calculated for a sample service line and assumes activity within service lines can be readily shifted between trusts and performed at a lower cost 3 Assumes movement of activity is driven by “for market” competition, based on price, between trusts for commissioners (in contrast to patients choosing to go to higher quality, though potentially higher cost, hospitals) 4 This analysis is for a sample service line. The average savings for all elective service lines is 7%, so we estimate that between 5 – 10% of elective spend can be saved SOURCE: NHS Programme Budgets, HES 2011/12, Trust financials, Team analysis Mc. Kinsey & Company Last Modified 17/11/2015 12: 10 GMT Standard Time Acute care cost curve for a sample service line, complex elective surgery, for a sample local health economy, 2012/13 Forecast 1, 2, 3 | 10

Asset optimization If acute trusts were as efficient as the median (0. 6), £ 4. 2 b could be freed 4 and annual maintenance costs reduced by £ 0. 7 b Highest asset base/ revenue Trust with lowest asset base/ 1 Total income and tangible assets are used 2 Outliers are excludedrevenue 3 Only acute trusts are used in this analysis 4 In practice, realising these savings may be difficult due to 1) long-term PFI contracts, 2) difficulty in selling under-utilised estate, and 3) inclusion of non -estate assets SOURCE: Laing & Buisson financials 2010/11; Team analysis Mc. Kinsey & Company | 11 Printed 21/01/2015 15: 19 GMT Standard Time Ranked trusts But if all trusts were as efficient as the 25 th percentile (0. 53), £ 6. 4 b could be freed 4 and annual maintenance costs reduced by £ 1. 1 b Last Modified 17/11/2015 12: 10 GMT Standard Time Assets to revenues 1 by trust 2, 3, 2010/11

Social care 2010/11; 4 London boroughs Very high risk High risk Low risk Very low risk Total 24, 752 41, 675 142, 773 322, 609 378, 020 889, 833 54 7, 857 2, 477 575 40 13 1 Includes elective admissions, outpatient, and A&E 117. 7 327. 4 3. 68 14 185. 6 104. 1 25% 1088. 5 11, 591 2, 468 2. 48 353. 6 275 1, 223 NEL LOS, Bed days Per admission Per ‘ 000 1. 20 504 1. 17 186 0 0 1. 95 264 2 Includes community health & primary care Mc. Kinsey & Company | 12 SOURCE: Team analysis, HES 2010/11, FIMS, Q research/NHS Information centre, PSSEX; NHS Reference Costs Printed 21/01/2015 15: 19 GMT Standard Time Moderate risk 4, 757 Social care, % Total of stratum costs spend, £m Last Modified 17/11/2015 12: 10 GMT Standard Time Population Average cost per capita, £

Hospital transformation (French example) Situation 23, 000 staff ▪ ▪ ▪ 5, 300 beds € 1. 6 bn annual budget Massive (~ € 950 m ) investments ▪ DRGbased payments Net profit, € millions 2006 2007 2008 2009 Management infrastructure 2010 ▪ 2011 New departmental management structure ▪ Strengthened performance dialogues/ contracts with departments ▪ Significant investment in management reporting tools and performance management processes -37 -86 -59 -22 2013 ▪ Switch to Mindsets, capabilities & behaviors ▪ Created strong burning platform Co-created plan with bottom-up input ▪ Communicated heavily on results internally and externally ▪ Established central performance team to support transformation ▪ Robust turnaround of performance… but difficulty to focus enough on longer-term levers (e. g. capability building) ▪ Head winds are stronger than ever – which levers next ? Mc. Kinsey & Company | 13 Printed 21/01/2015 15: 19 GMT Standard Time ▪ Portfolio of 140 initiatives across 14 sites and all key functions, incl. ▪ Restructuring plan : purchasing (€ 50 m) ; Realestate divestments (- € 140 m) ; 5 site closures (€ 45 m personnel cost savings) ; clinical and non-clinical growth (€ 10 -20 m)… ▪ Operational excellence (theaters, ER, …) ▪ Reconfiguration (cardiology, pathology, geriatrics…) Significant impact on the bottom line Last Modified 17/11/2015 12: 10 GMT Standard Time Operating system

Hospital transformation (NHS example) ▪ Situation ▪ § 1, 800 beds and 14, 000 staff ▪ ▪ § £ 830 m turnover § £ 100 m shortfall § Medical leadership not Significant savings achieved 40 Management infrastructure ▪ Chief Restructuring Officer added to Board ▪ Strengthened PMO for delivery tracking ▪ Executive challenge and confirm sessions ▪ Embedded implementation support running 3 waves of initiatives per year £m Printed 21/01/2015 15: 19 GMT Standard Time forecast in next 2 years Pathway/functional teams generated portfolio of 120 initiatives Clinical pathway re-design - Acute Medicine; Orthopaedics and others (£ 22 m) Clinical support (Imaging; Pharmacy) service productivity and demand management (£ 5 m) Corporate functions and non-clinical service support (£ 8 m) ▪ Estate rationalization and outsourcing Last Modified 17/11/2015 12: 10 GMT Standard Time Operating system 6, 5 engaged § Previous reliance on volume growth for financial success Mindsets, capabilities & behaviors ▪ Pathway/functional teams generated portfolio of initiatives ▪ Role modeling by CEO, visibly “leading from the shop-floor” ▪ 150 leaders engaged and trained on how to inspire and lead change ▪ Change agent training (meds, nurses…) % of cost base Mc. Kinsey & Company | 14

What I will talk about today Last Modified 17/11/2015 12: 10 GMT Standard Time Challenges Printed 21/01/2015 15: 19 GMT Standard Time Plan A Plan B | 15 Mc. Kinsey & Company

Plan B Last Modified 17/11/2015 12: 10 GMT Standard Time 1. Do as much as possible within Plan A 2. Consider: 1 2 Learning from other sectors Redesign models of care 3 Use technology Printed 21/01/2015 15: 19 GMT Standard Time Mc. Kinsey & Company | 16

1 Learn from other sectors Innovate the workforce Increase utilisation of assets Support self service/ self care Last Modified 17/11/2015 12: 10 GMT Standard Time Drive frontline productivity Improved purchasing power Printed 21/01/2015 15: 19 GMT Standard Time Compared to other industries, healthcare is still lagging behind in technical efficiency driven by standardisation and industrialisation of processes Mc. Kinsey & Company | 17

1 Aravind has significantly reduced costs of care (and delivered improved productivity) Last Modified 17/11/2015 12: 10 GMT Standard Time Unit cost of cataract surgery in 2010/11 Aravind Printed 21/01/2015 15: 19 GMT Standard Time $PPP 250 $PPP 1, 400 … at ~1/6 th the cost… UK-NHS Infection rate per 10, 000 patients 4% Aravind 6% UK-NHS … and with better outcomes SOURCE: Rockefeller Foundation; Interviews; 2010/11 National Schedule of Reference Costs; 2010/11 Aravind Eye Care System Activity Report; Global Insight; Conversation with Dr. Sathya Ravilla at Aravind; Team Analysis Mc. Kinsey & Company | 18

1 Support self care: In Jonkoping 63% of patients self-dialyse Last Modified 17/11/2015 12: 10 GMT Standard Time Printed 21/01/2015 15: 19 GMT Standard Time ▪ ▪ ▪ Patients manage entire dialysis process Encourage exercise & peer-to-peer support 50– 75% lower spend per patient 63% patients self-dialyse, target is 75% Convenience and greater sense of control Nursing staff role transformed Mc. Kinsey & Company | 19

1 Support self care – changing the paradigm Last Modified 17/11/2015 12: 10 GMT Standard Time Printed 21/01/2015 15: 19 GMT Standard Time | 20 Mc. Kinsey & Company

There are examples of innovation that suggest change is possible “The world without me” incentive Self-dialysis by patients 50% of salary activity and performance related Video-enabled pharmacy dispensers in 34 states Printed 21/01/2015 15: 19 GMT Standard Time Rapid in house trained staff make up 60% of workforce Low-cost highquality care for older people Accelerated training of youth unemployed Patient portal and accessible records … Mc. Kinsey & Company Last Modified 17/11/2015 12: 10 GMT Standard Time Advanced Pharmacy Prescribing | 21

2 Redesign models of care – emerging themes Managed primary care ▪ Adopting core principles of patient segmentation, proactive care, standardised and tailored approaches, and performance management Standardized, at scale ▪ Dramatically improve productivity, drawing on innovation from other industries Mc. Kinsey & Company Printed 21/01/2015 15: 19 GMT Standard Time Horizontal integration ▪ Create stronger networks to build scale ▪ Standardise approaches ▪ Build centres of excellence ▪ Rigorously measure and monitor quality Last Modified 17/11/2015 12: 10 GMT Standard Time Vertical Integration ▪ Hospitals expanding into primary and community care ▪ Enables providers to optimise asset base and provide patients with seamless pathways and one port of call | 22

2 Implement improved primary and community care at scale to keep people out of hospitals ▪ Improved patient health (22% lower cholesterol levels for patients on statins) Mc. Kinsey & Company Printed 21/01/2015 15: 19 GMT Standard Time 18% lower hospitalisation rates Last Modified 17/11/2015 12: 10 GMT Standard Time ▪ | 23

2 Adjust payments Fixed payment Variable payment Period of time Population Mechanism Block funding Capitation (inc. weighted) Last Modified 17/11/2015 12: 10 GMT Standard Time Basis Activity Episode / bundled DRG Fee-for-service Impact on… Increased activity Printed 21/01/2015 15: 19 GMT Standard Time Cost control Primary prevention Secondary prevention Care pathway coordination All options can be overlaid with performance incentives, e. g. Pay for Value (P 4 V) or Pay for Performance (P 4 P) SOURCE: Adapted from WHO 2000, Charlesworth 2012, Busse 2011 Mc. Kinsey & Company | 24

2 Five tests How the test was applied 2 Risk allocation Provider bears morbidity risk through prospectively defined capitation formula, with no risk adjustment mechanism; competition and choice incentivize quality care Pricing Prices within a given episode remain fee-for-service, while thresholds for risk and gain-sharing is based on historical prioryear average costs Scale Prinicipal Accountable Providers are directly responsible for full episode of care, and 50% will fall under risk or gain sharing arrangements 3 4 5 Roadmap & agreement Significant provider and user involvement throughout design and clear 3 -5 year roadmap with shadow form and phased risk transfer Extensive engagement including clinical advisory group for design, taking time to develop with wide input, and a large public consultation to ensure buy-in and support Mc. Kinsey & Company | 25 Printed 21/01/2015 15: 19 GMT Standard Time Vision Last Modified 17/11/2015 12: 10 GMT Standard Time 1 Capitation is the key vehicle for delivering their system-wide reconfiguration strategy, breaking down organisational siloes to achieve whole system person-centred care

3 Technology creates value through better utilising the workforce and supporting their decision making Automates and improves previously manual tasks reducing errors and allowing skills to be redeployed Increases access to information allowing mining of big data and reduction of transaction costs Mc. Kinsey & Company Printed 21/01/2015 15: 19 GMT Standard Time Expanding access to limited specialist skills allowing both enhancement of specialization without compromising access Last Modified 17/11/2015 12: 10 GMT Standard Time Allowing patients and carers to play a much greater role effectively expanding and reducing cost of the workforce | 26

3 Digital tools can dramatically empower self-care, provided they meet key patient needs Increasingly sophisticated features… § Automatic adherence monitoring via Bluetooth™ Top reasons to continue using health techno-logy include time, cost and convenience, % Saved me time Was free § Behavioral analytics engine generating alerts based on phone usage More convenient than ’non-tech’ Made me feel in control of my health Help me achieve my health goals Printed 21/01/2015 15: 19 GMT Standard Time § Geolocation to support care for dementia patients Last Modified 17/11/2015 12: 10 GMT Standard Time . . however convenience and clinician endorsement remain key Other Main endorsement preference, % Other 1 Family/friends § Facilitated self-care plan generation based on EHR data 9 10 45 A health professional you knew SOURCE: Mc. Kinsey research; Mc. Kinsey Digital Health Survey 2014 (EMEA) 36 The NHS 81% Mc. Kinsey & Company | 27

3 The awareness vs adoption gap for digital tools is starting to close 2014 2015 Percentage of consumers who are aware of product 1 Growth from 2014 to 2015 78% Health bracelets Senior remote alert apps 60 25 149% Health chips 22 72% believe scheduling a medical appointment online is more effective than by phone >70% are now using digital channels for medical education 63% of consumers would prefer a single app that could hold all of their data (including medical records)2 1 Includes respondents who have heard about product but are not familiar, as well as respondents who are familiar 2 Mc. Kinsey Consumer Health Insights Survey 2014 (questions was not asked in the 2015 survey) SOURCE: Mc. Kinsey Consumer Health Insights Survey 2015 Mc. Kinsey & Company | 28 Printed 21/01/2015 15: 19 GMT Standard Time % of consumers who are interested in buying or have already bought 93% Last Modified 17/11/2015 12: 10 GMT Standard Time Awareness of consumer health tools

3 Evidence for value from digital interventions Supply efficiency (reduce unit costs) ▪ ▪ EHR ▪ Digital lean: – Patient flow management – Barcoding – RFID – Procurement – e-Rostering ▪ Doctor performance transparency tools 3 ▪ Electronic booking and reminders ▪ Vital sign tracking ▪ Remote monitoring ▪ EHR ▪ ▪ Community Care~12% ▪ E-triage, telephone triage, teleconsultations and physician web messaging ▪ EHR incl. eprescriptions ▪ Online booking Booking reminders ▪ E-referrals Teleconsultations Mental Health ~12% ▪ ▪ Mobile working ▪ EHR Centralised booking system ▪ Geographic assignment of patients and routes ▪ E-rostering ▪ Procurement ▪ Transparency ▪ RFID Care coordination and screening ▪ Remote ▪ Automated monitoring reminders ▪ ▪ EHR ▪ Centralised electronic booking ▪ ICT-based or facilitated interventions ▪ E-rostering Self-care; Electronic monitoring of patients mood ▪ Transparency ▪ Procurement Behaviour tracking apps ▪ E-learning portals Primary prevention ▪ Automated reminders ▪ Remote consultations ▪ Incentive programmes ▪ Behaviour tracking apps Mc. Kinsey & Company | 29 Printed 21/01/2015 15: 19 GMT Standard Time Demand levers (reduce volume) Primary Care ~25% Share of total spend Last Modified 17/11/2015 12: 10 GMT Standard Time Acute Care ~50% XX%

4 Digital interventions’ net improvement potential reaches 10% 3 Relevance for patient focused digital health Supply efficiency (reduce unit costs) Primary Care ~25% ~12% Community Care Transparency on outcomes 1 Connected EHRs Demand levers (reduce volume) Mental Health~12% Mental Savings potential (1. 3 - 2. 3%) (0. 1%) 4. 7 -7. 8% Printed 21/01/2015 15: 19 GMT Standard Time (1. 7 - 2. 5%) Shift to lower cost channels (e-triage, phone triage, digital consultation) (0. 9 - 2. 1%) (x%) Saving as percent of total HC expenditure (0. 7 - 0. 8%) Patient self services Automation of hospitals Low Workforce efficiency (1. 0 – 1. 1%) Care coordination and screening (0. 8 – 1. 7%) 1. 0 -2. 5% Primary prevention Last Modified 17/11/2015 12: 10 GMT Standard Time Acute Care ~50% High (0. 2 – 0. 8%) 6. 2 -10. 3% Mc. Kinsey & Company | 30

3 Step changes on the horizon Radiologist Last Modified 17/11/2015 12: 10 GMT Standard Time Hospital porter Pharmacist Doctor Printed 21/01/2015 15: 19 GMT Standard Time Anesthetist Surgeon Mc. Kinsey & Company | 31
 Innovating for people
Innovating for people Nc hfma
Nc hfma Marina henke
Marina henke Wv hfma
Wv hfma Nc hfma
Nc hfma Pow code of conduct
Pow code of conduct Sports medicine definition
Sports medicine definition Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Nicolaus schwerk
Nicolaus schwerk What was nicolaus copernicus job
What was nicolaus copernicus job Nicolaus copernicus theory
Nicolaus copernicus theory Slovakia christmas dinner
Slovakia christmas dinner Where was nicolaus copernicus born
Where was nicolaus copernicus born Nicolaus copernicus
Nicolaus copernicus Nicolaus copernicus contribution
Nicolaus copernicus contribution Introduction of health care delivery system
Introduction of health care delivery system Accenture project management methodology
Accenture project management methodology Uic healthcare administration
Uic healthcare administration Visual analytics in healthcare
Visual analytics in healthcare Integrated healthcare law
Integrated healthcare law Midas health analytics
Midas health analytics Advancing knowledge in healthcare
Advancing knowledge in healthcare Legal principles in healthcare
Legal principles in healthcare Conybio healthcare products
Conybio healthcare products Fluoroquinalone
Fluoroquinalone Delaware healthcare commission
Delaware healthcare commission Indivirtus
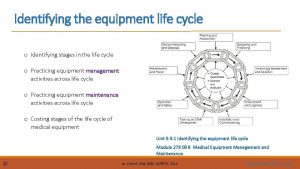
Indivirtus Healthcare equipment lifecycle
Healthcare equipment lifecycle Support services career pathway
Support services career pathway Sirius security
Sirius security Affinity healthcare group recruiting
Affinity healthcare group recruiting Emory radiology eclh
Emory radiology eclh Introduction to healthcare data analytics
Introduction to healthcare data analytics