Infant Food Allergies Where Are We Now Janice









![Summary of 2008 AAP Guidelines for Allergy Management [Greer et al 2008] There is Summary of 2008 AAP Guidelines for Allergy Management [Greer et al 2008] There is](https://slidetodoc.com/presentation_image/1eb6855674d77c6a433fb4974cc9df02/image-27.jpg)









- Slides: 51
Infant Food Allergies Where Are We Now? Janice Joneja Ph. D. , RD
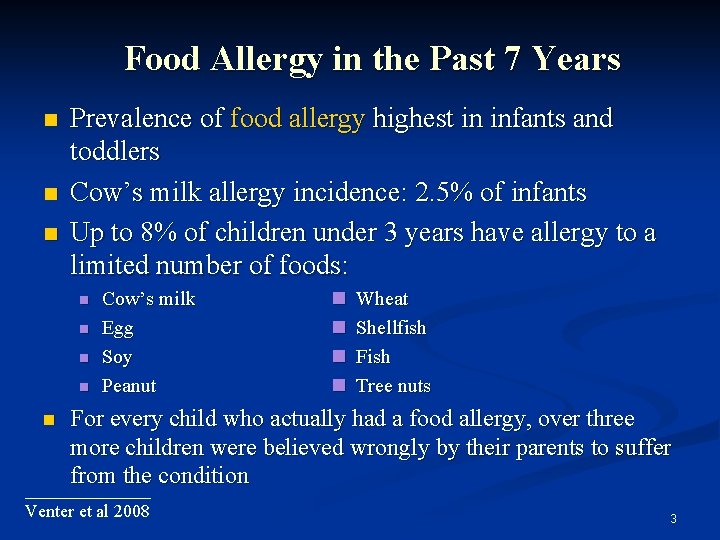
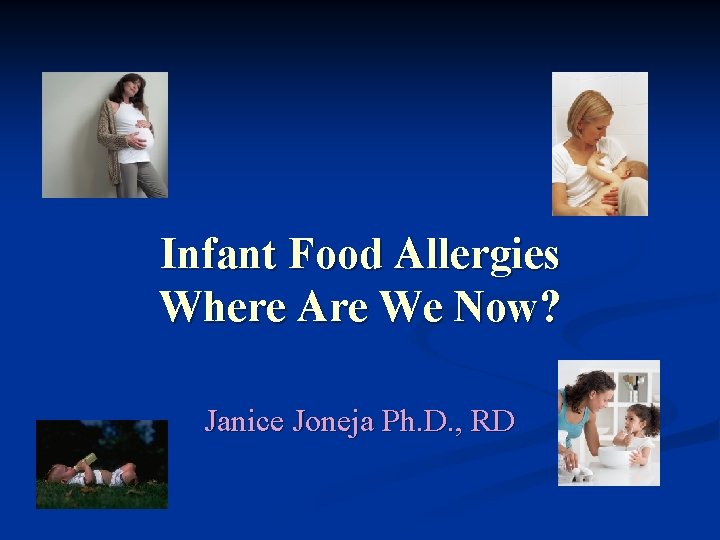
Food Allergy in the Past 7 Years Nearly 4% of North Americans have food allergies, many more than recorded in the past Incidence of food allergy much higher in children (>8%) than adults (<2%) Prevalence of peanut allergy doubled in American children younger than 5 years of age in the years 2002 - 2007 2
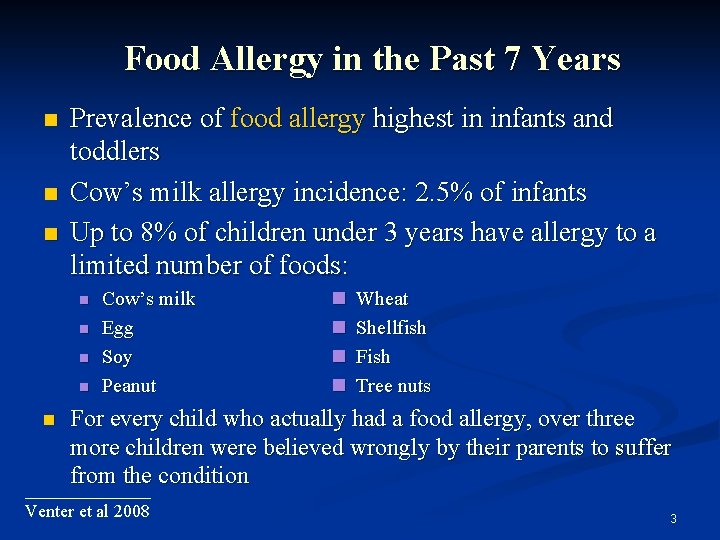
Food Allergy in the Past 7 Years Prevalence of food allergy highest in infants and toddlers Cow’s milk allergy incidence: 2. 5% of infants Up to 8% of children under 3 years have allergy to a limited number of foods: Cow’s milk Egg Soy Peanut Wheat Shellfish Fish Tree nuts For every child who actually had a food allergy, over three more children were believed wrongly by their parents to suffer from the condition _______ Venter et al 2008 3
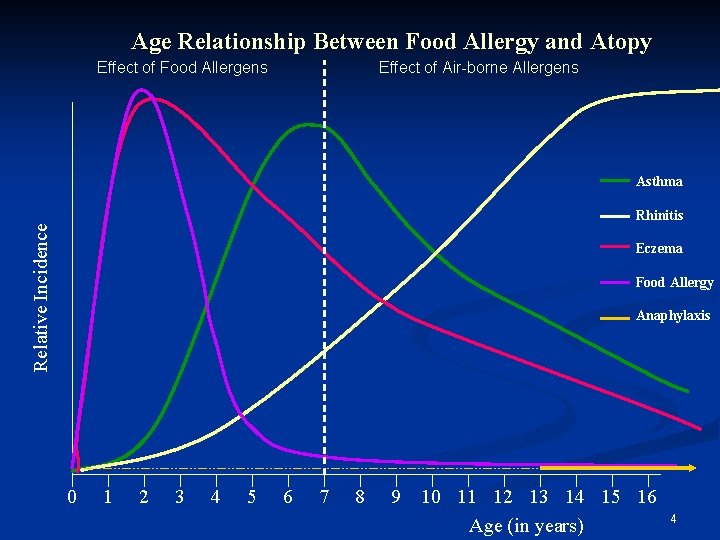
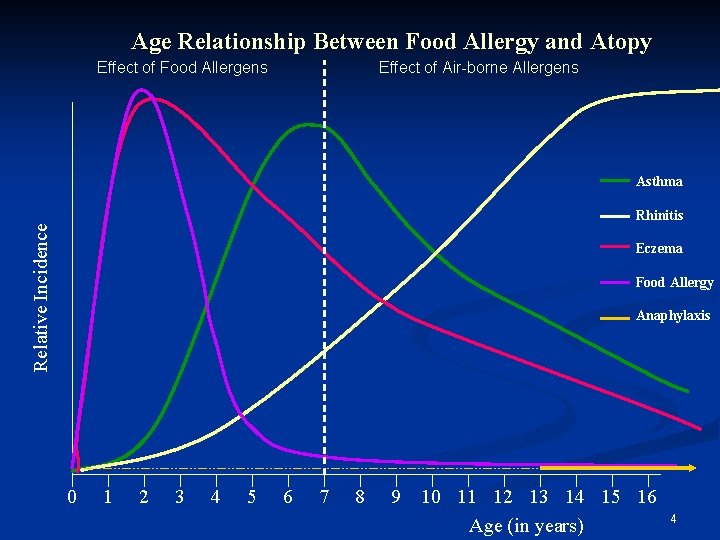
Age Relationship Between Food Allergy and Atopy Effect of Food Allergens Effect of Air-borne Allergens Asthma Relative Incidence Rhinitis Eczema Food Allergy Anaphylaxis 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Age (in years) 4

Historical Perspective Sensitization to food allergens was thought to be the start of the “allergic march” Food allergy Atopic dermatitis/eczema Asthma Rhinitis Reducing sensitization to foods was therefore considered the essential first step in allergy prevention 5
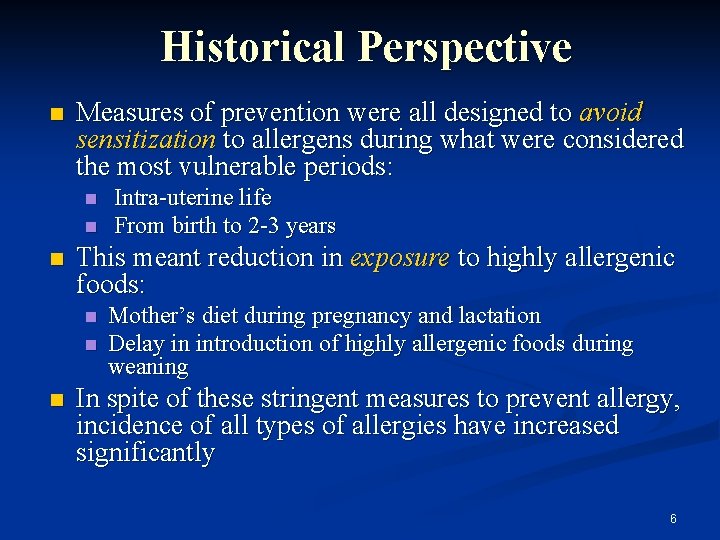
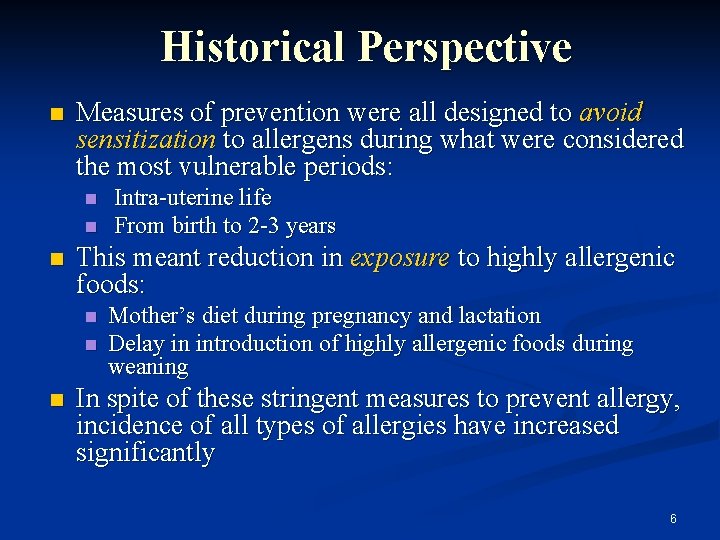
Historical Perspective Measures of prevention were all designed to avoid sensitization to allergens during what were considered the most vulnerable periods: This meant reduction in exposure to highly allergenic foods: Intra-uterine life From birth to 2 -3 years Mother’s diet during pregnancy and lactation Delay in introduction of highly allergenic foods during weaning In spite of these stringent measures to prevent allergy, incidence of all types of allergies have increased significantly 6
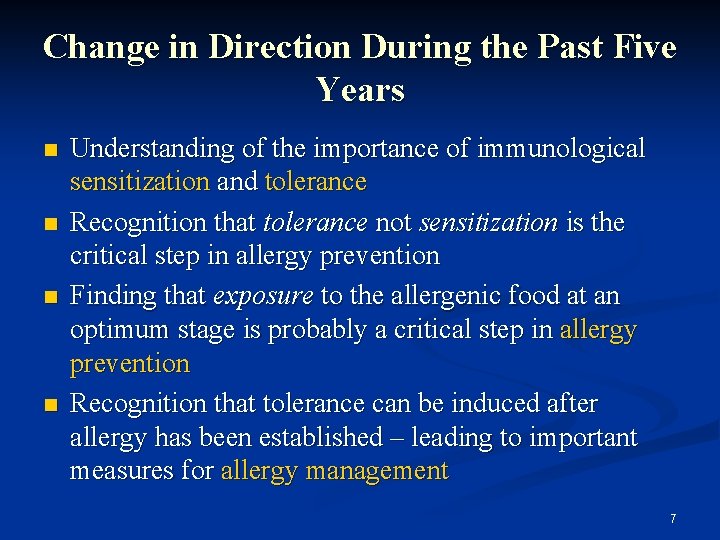
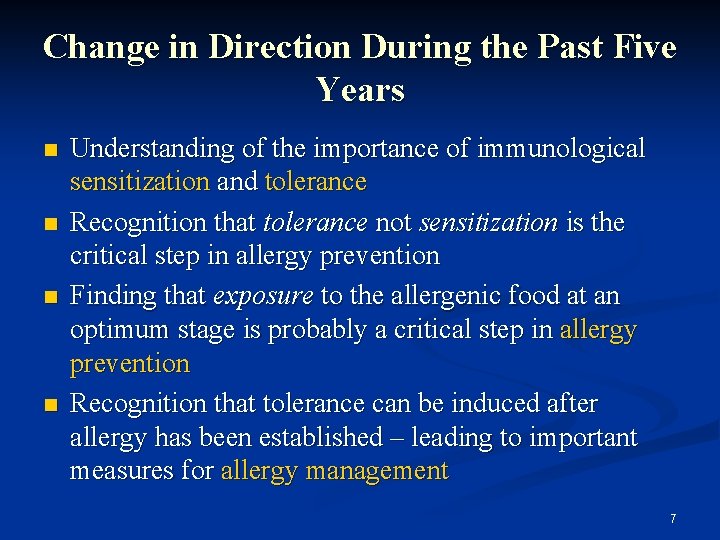
Change in Direction During the Past Five Years Understanding of the importance of immunological sensitization and tolerance Recognition that tolerance not sensitization is the critical step in allergy prevention Finding that exposure to the allergenic food at an optimum stage is probably a critical step in allergy prevention Recognition that tolerance can be induced after allergy has been established – leading to important measures for allergy management 7
Allergy is a Response of the Immune System Our immune systems are designed to protect the body from invasion by foreign materials All foods contain proteins – derived from plants and animals – all of which are foreign to the human body In order food to be absorbed, metabolized, and utilized by the body, the immune system needs to be “educated” that the foreign material is safe ____ Herz 2008 8

Education of the Immune System Involves a complex series of immunological reactions controlled by T cell lymphocytes (T cells) T helper (Th) cells detect foreign proteins (antigens) in any form T cells then trigger a series of immunological reactions, mediated by cytokines (the “control chemicals” of the immune system) _____ Joneja 2007 9
T-helper Cell Subclasses There are two subclasses of T-helper cells Th 1 Th 2 Each Th cell type produces its own specific set of cytokines The types of cytokines generated determine the resulting immune response Th 1 principally INF- Th 2 principally IL-4 10
Role of T-helper Cell Subtypes Th 1 triggers the protective response to a pathogen such as a virus or bacterium Ig. M, Ig. G, Ig. A antibodies are produced Th 2 is responsible for the allergic (hypersensitivity) reaction Ig. E antibodies are produced 11
T cells involved in Oral Tolerance T cell response depends on the type of T helper cell that is activated Latest research indicates that T cells that produce a cytokine called TGF- are important in inducing oral tolerance Sometimes called Th 3 cells T cells that produce IL-10 and IL-13 may also be involved in tolerance These also regulate immune response to resident microflora, preventing the usual immune inflammatory response to microorganisms __________ Strobel and Mowat 2006 12

Oral Tolerance “Education” of the T cells to not respond to that food protein when it enters via the oral route – called oral tolerance Contrasts with the active immune responses needed to protect the gut against continual bombardment by invading pathogens and their products (toxins, etc) Also contrasts with the reduced responsiveness to the millions of microorganisms that are permanent residents of the large bowel T cells involved in these processes are called regulator T cells (Treg) 13
Prevention of Food Allergy in Clinical Practice Significant change in directives within the past 5 years: Previously: Avoidance of allergen to prevent sensitization (allergen-specific Ig. E) Current: Active stimulation of the immature immune system to induce tolerance of the antigens in food ________ Rautava et al 2005 14
Factors Predictive of Allergy: High and Low risk Groups Many factors investigated as possible predictive markers for allergy Only significant variable in studies: Family history of allergy (all types) High risk for allergy: One first degree relative with diagnosed allergy (Ig. E-mediated) of any type First-degree relative: parent or sibling 15

Does Atopic Disease Start in Fetal Life? Fetal cytokines are skewed to the Th 2 type of response Suggested that this may guard against rejection of the “foreign” fetus by the mother’s immune system Ig. E occurs from as early as 11 weeks gestation and can be detected in cord blood _______ Jones et al 2000 16

Does Atopic Disease Start in Fetal Life? (continued) At birth neonates have low INF- and tend to produce the cytokines associated with Th 2 response, especially IL-4 So why do all neonates not have allergy? 17

Does Atopic Disease Start in Fetal Life? (continued) New research indicates that the immune system of the mother may play a very important role in expression of allergy in the neonate and infant Ig. G crosses the placenta; Ig. E does not Certain sub-types of Ig. G (Ig. G 1; Ig. G 3) can inhibit Ig. E response 18
Significance in Practice Food proteins demonstrated to cross the placenta and can be detected in amniotic fluid Exposure to small quantities of food antigens from mother’s diet thought to tolerize the fetus, by means of Ig. G 1 and Ig. G 3, within a “protected environment” 19

Immune Response of the Allergic Mother Atopic mother’s immune system may dictate the response of the fetus to antigens in utero The allergic mother may be incapable of providing sufficient Ig. G 1 and Ig. G 3 to downregulate (depress) fetal Ig. E There is no convincing evidence that sensitization to specific food allergens is initiated prenatally 20
Diet During Pregnancy Current directive: the atopic mother should strictly avoid her own allergens and replace the foods with nutritionally equivalent substitutes There are no indications for mother to avoid other foods during pregnancy A nutritionally complete, well-balanced diet is essential Authorities recommend avoidance of excessive intake of highly allergenic foods such as peanuts and nuts to prevent “allergen overload”, but there is no scientific data to support this ________ Kramer et al 2006 21
Breast-feeding and Allergy Studies indicating that breast-feeding is protective against allergy report: A definite improvement in infant eczema and associated gastrointestinal complaints when baby is exclusively breast-fed Reduced risk of asthma in the first 24 months of life _________ Kirjavainen et al 2002 22
Breast-feeding and Allergy Other studies are in conflict with these conclusions: Some report no improvement in symptoms Some suggest symptoms get worse with breastfeeding and improve with feeding of hydrolysate formulae Japanese study suggests that breast-feeding increases the risk of asthma at adolescence Why the conflicting results? ________ Miyake et al 2003 23

Immunological Factors in Human Milk that may be Associated with Allergy: Cytokines and Chemokines Atopic mothers tend to have a higher level of the cytokines and chemokines associated with allergy in their breast milk Those identified include: IL-4 IL-5 IL-8 IL-13 Some chemokines (e. g. RANTES) Atopic infants do not seem to be protected from allergy by the breast milk of atopic mothers ______________ Snijders et al 2007 KOALA study 24
Immunological Factors in Human Milk that may be Associated with Allergy: TGF- 1 Cytokine, transforming growth factor- 1 (TGF 1) promotes tolerance to food components in the intestinal immune response TGF- 1 in mother’s colostrum may influence the type and intensity of the infant’s response to food allergens A normal level of TGF- 1 is likely to facilitate tolerance to food encountered by the infant in mother’s breast milk and later to formulae and solids _______ Rigotti et al 2006 25

Implications of Research Data Exclusive breast-feeding with exclusion of mother’s and baby’s allergens will reduce signs of allergy in the first 1 -2 years; specifically: Cow’s milk allergy Eczema Reduction or prevention of early food allergy by breast-feeding does not seem to have long-term effects on the development of asthma and allergic rhinitis Other benefits of breast-feeding far outweigh any possible negative effects on allergy: exclusive breast-feeding for 4 -6 months is strongly encouraged 26
![Summary of 2008 AAP Guidelines for Allergy Management Greer et al 2008 There is Summary of 2008 AAP Guidelines for Allergy Management [Greer et al 2008] There is](https://slidetodoc.com/presentation_image/1eb6855674d77c6a433fb4974cc9df02/image-27.jpg)
Summary of 2008 AAP Guidelines for Allergy Management [Greer et al 2008] There is no convincing evidence that women who avoid highly allergenic foods, or other foods during pregnancy and breast-feeding lower their child’s risk of allergies For high-risk for allergy infants (one firstdegree relative with established allergy), exclusive breast-feeding for at least 4 months prevents or delays the occurrence of atopic dermatitis (eczema), cow’s milk allergy, and wheezing in early childhood _______ Greer et al 2008 __________ Sicherer and Burks 2008 27
Preventive Effect of Breast-feeding: KOALA Study Longer duration of breastfeeding is associated with lower risk for eczema in non-atopic mothers Slightly lower risk for mothers with allergy but no asthma Longer duration of breastfeeding reduced risk for wheezing in infants: possibly due to reduction in respiratory infections There is a lack of evidence that exclusive or prolonged breast-feeding has any positive effect on the development of asthma in older children ______________ Snijders et al 2007 KOALA study 28
Summary of 2008 AAP Guidelines continued In infants at high risk for allergy who are not exclusively breast-fed for 4 -6 months there is modest evidence that the onset of atopic disease (allergy), especially eczema, may be delayed or prevented by the use of hydrolyzed formulas There is no good evidence that soy-based infant formulas have any preventive effect on the development of allergy 29

Preventive Effect of Hydrolyzed Infant Formulae No evidence of any reduction in allergy with hydrolyzed formula compared to breastfeeding Limited evidence that prolonged feeding with hydrolyzed formula compared to cow’s milk reduces incidence of CMA and eczema No evidence that hydrolyzed formulas have any effect on the development of rhinitis and asthma later Extensively hydrolyzed cow’s milk (Ehf) formulas marginally better than partially hydrolyzed whey (Phf) in prevention _________________ Osborn and Sinn 2009 Cochrane Review _____________ Von Berg et al GINI Study 2009 30
Infant Formulae for the Allergic Baby Current Recommendations Cow’s milk based formula if there are no signs of milk allergy Partially hydrolysed (phf) whey-based formula if there are no signs of milk allergy in high risk for allergy group Extensively hydrolysed (ehf) casein based formula if milk allergy is proven _________ Greer et al AAP 2008 Von Berg et al 2007 31
Recommendations for Introduction of Solids to High Risk for Allergy Infants Little evidence that delaying the introduction of complementary foods beyond 4 -6 months of age prevents allergy Introduction of solid foods should be individualized Foods should be introduced one at a time in small amounts Mixed foods containing various potential food allergens should not be given unless tolerance to each ingredient has been assessed __________ Greer et al AAP 2008 ___________ Thygaran and Burks 2008 32
Introduction of Solid Foods in Relationship to Celiac Disease Results suggest that in high risk for celiac disease infants introduction of gluten-containing grains before 3 months or after 7 months increases incidences of development of CD 1 Introduction of gluten while breast-feeding offers protection or delays onset of celiac disease in at-risk infants 2 Recommendations: Introduce gluten grains in small amounts between 4 and 6 months while infant is breastfed Continue breast-feeding for a further 2 -3 months Similar results for wheat allergy 3 ________ 1 Norris et al 2005 _______ 2 Guandalini 2007 ______ 3 Poole et al 2006 33

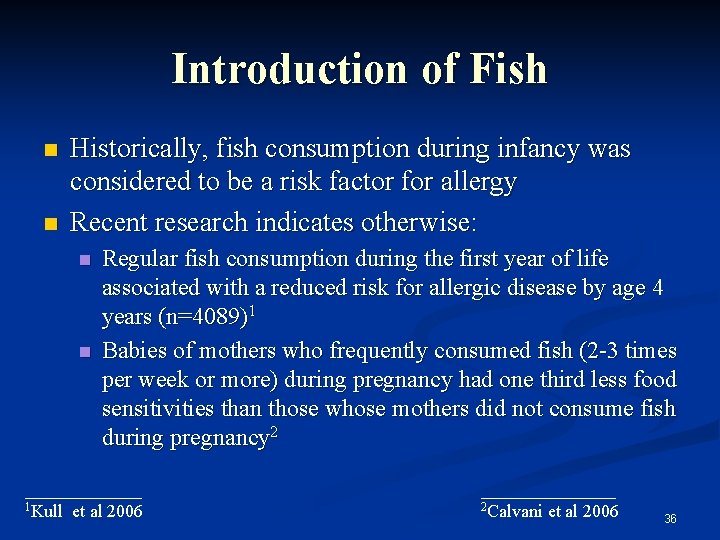
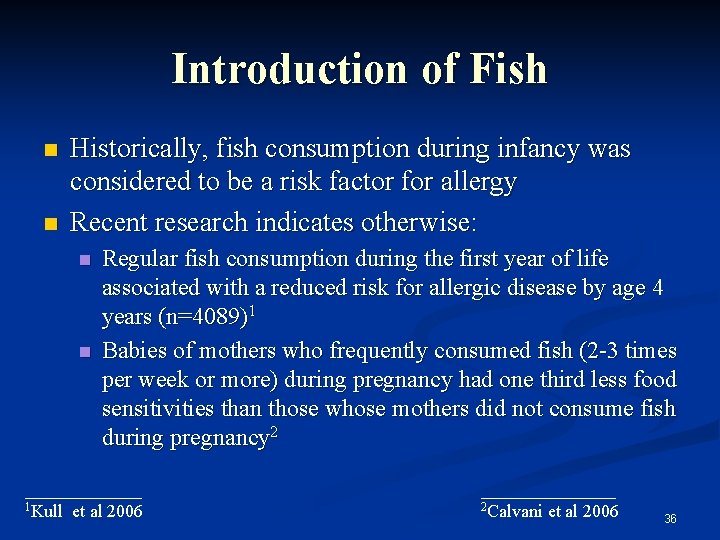
Introduction of Peanuts Directives from pediatric societies (1998 - 2007) recommended avoidance of peanuts by mothers during pregnancy and lactation, and delaying introduction of peanuts until after 2 or even 3 years of age Research indicates that incidence of peanut allergy in children rose dramatically in the years following release of these directives Recent research suggests: Avoidance of peanuts reduced development of tolerance Early exposure leads to reduced incidence of peanut allergy _________ Hourihane et al 2007 34
Introduction of Peanuts Study (n=10, 786) among primary school age Jewish children in UK and Israel Prevalence of peanut allergy (PA): 1. 85% 0. 17% Median monthly consumption of peanut in infants aged 8 – 14 months: In UK: In Israel: 0 7. 1 g Difference not due to atopy, genetic background, social class, or peanut allergenicity Israeli infants consume peanuts in high quantities during the first year of life _______ Du Toit et al 2008 35
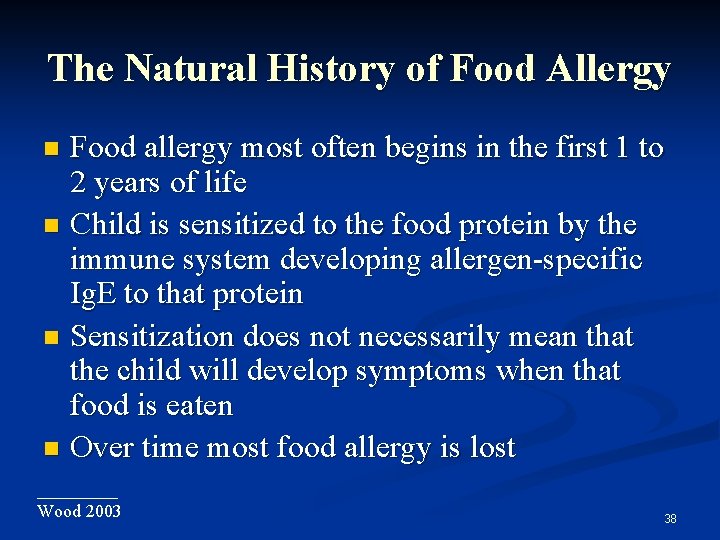
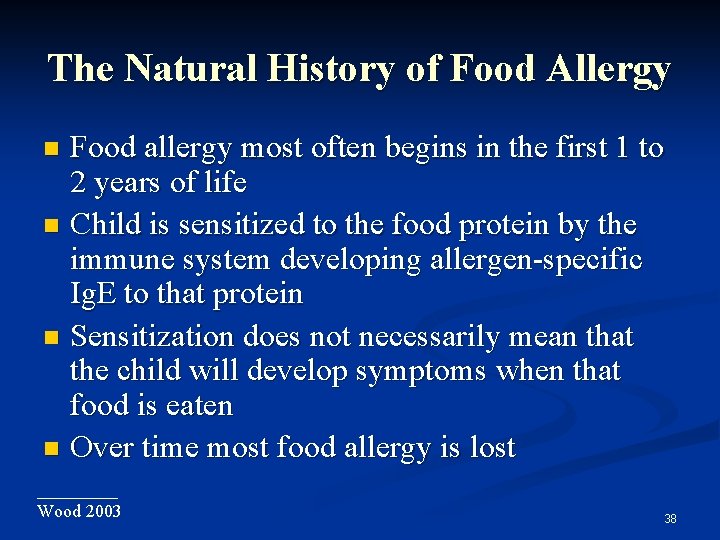
Introduction of Fish Historically, fish consumption during infancy was considered to be a risk factor for allergy Recent research indicates otherwise: Regular fish consumption during the first year of life associated with a reduced risk for allergic disease by age 4 years (n=4089)1 Babies of mothers who frequently consumed fish (2 -3 times per week or more) during pregnancy had one third less food sensitivities than those whose mothers did not consume fish during pregnancy 2 _______ 1 Kull et al 2006 ________ 2 Calvani et al 2006 36

Introduction of Fish Study (n= 5, 000); 20. 9% developed eczema by 1 year: Babies who were fed fish before nine months of age were 24% less likely to develop eczema by age 1 year Omega-3 content of fish did not seem to influence the outcome The age at which egg and milk were introduced did not affect development of eczema Breast-feeding did not have any significant impact on development of eczema ______ Alm et al 2009 ______________ Hibbeln et al 2007 ALSPAC study 37
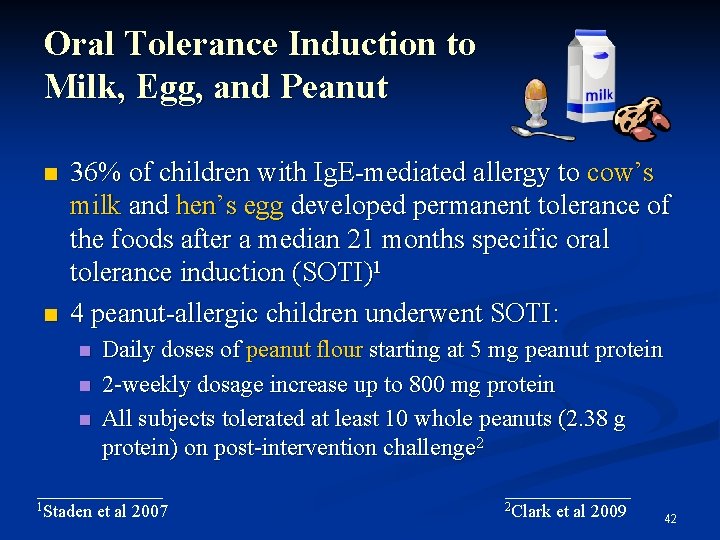
The Natural History of Food Allergy Food allergy most often begins in the first 1 to 2 years of life Child is sensitized to the food protein by the immune system developing allergen-specific Ig. E to that protein Sensitization does not necessarily mean that the child will develop symptoms when that food is eaten Over time most food allergy is lost _____ Wood 2003 38

Prognosis Most children outgrow early food allergy John’s Hopkins Children’s Center USA Milk allergy outgrown: Egg allergy outgrown: 20% by 4 years 42% by 8 years 79% by 16 years 4% by 4 years 37% by 10 years 68% by 16 years Allergy to some foods more often than others persists into adulthood: Peanut Tree nuts Seeds Shellfish Fish _______ Skripak et al 2007 39

Induction of Oral Tolerance to a specific food can be induced by oral administration of the offending food by process of “low dose continuous exposure” Designated (SOTI: specific oral tolerance induction) Starting with very low dosages Gradually increasing daily dosage up to the equivalent of the usual daily intake Followed by daily maintenance dose _________ Niggemann et al 2006 _______ Calvani et al 2010 40

Desensitization to Cow’s Milk 18 children with confirmed CMA >4 years of age underwent SOTI Starting dose 0. 05 ml cow’s milk Increased to 1 ml on first day Increasing dosage weekly up to a daily dose of 200250 ml Results: 16/18 tolerated 200 -250 ml milk Length of process median 14 weeks (range 11 -17 weeks) Tolerance has been maintained for >1 year ________ Zapatero et al 2008 41
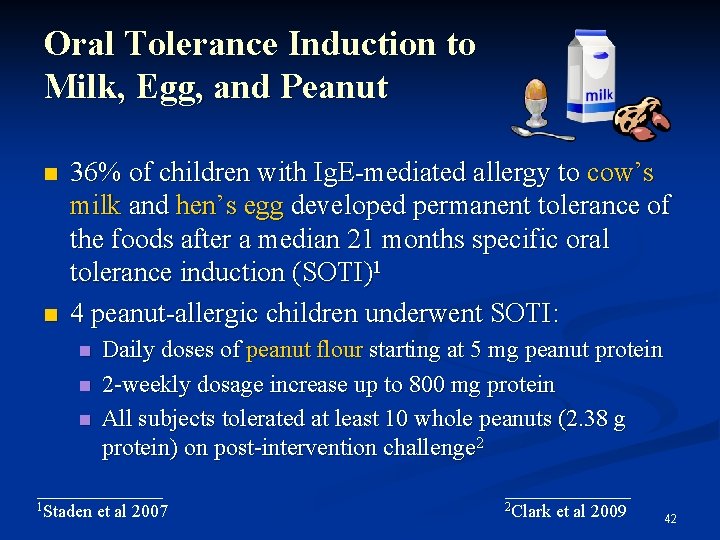
Oral Tolerance Induction to Milk, Egg, and Peanut 36% of children with Ig. E-mediated allergy to cow’s milk and hen’s egg developed permanent tolerance of the foods after a median 21 months specific oral tolerance induction (SOTI)1 4 peanut-allergic children underwent SOTI: Daily doses of peanut flour starting at 5 mg peanut protein 2 -weekly dosage increase up to 800 mg protein All subjects tolerated at least 10 whole peanuts (2. 38 g protein) on post-intervention challenge 2 _______ 1 Staden et al 2007 _______ 2 Clark et al 2009 42
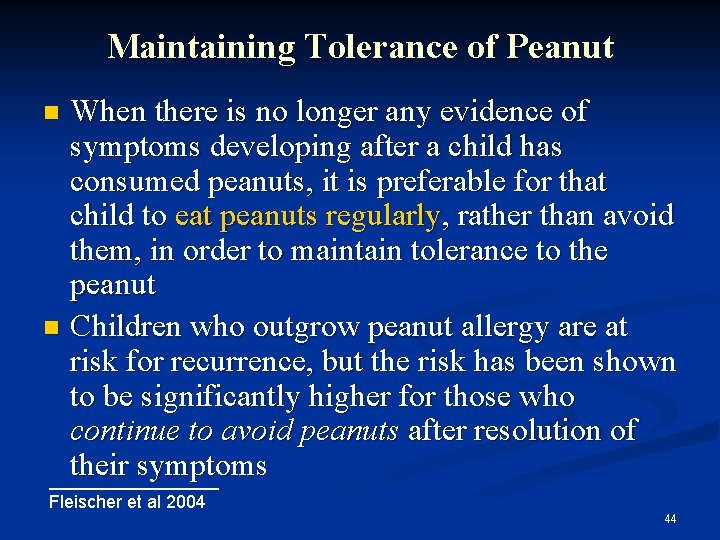
Progression of Peanut Allergy Peanut allergy, like many early food allergies, can be outgrown In 2001 pediatric allergists in the U. S. reported that about 21. 5 per cent of children will eventually outgrow their peanut allergy 1 Those with a mild peanut allergy, as determined by the level of peanut-specific Ig. E in their blood, have a 50% chance of outgrowing the allergy 2 Only about 9% of patients are reported to outgrow their allergy to tree nuts 3 _________ 1 Skolnick et al 2001 2 Fleischer et al 2003 3 Fleischer et al 2005 43
Maintaining Tolerance of Peanut When there is no longer any evidence of symptoms developing after a child has consumed peanuts, it is preferable for that child to eat peanuts regularly, rather than avoid them, in order to maintain tolerance to the peanut Children who outgrow peanut allergy are at risk for recurrence, but the risk has been shown to be significantly higher for those who continue to avoid peanuts after resolution of their symptoms _________ Fleischer et al 2004 44
Probiotics and Allergy Prevention Probiotics and prebiotics may change the colonic microflora of the neonate Theory: Change from Th 2 to Th 1 response in the neonatal period is required to reduce potential for allergy This change is mediated by contact with micro-organisms Non-allergic children have a predominance of lactobacilli and bifidobacteria Atopic children tend to have more clostridia and lower levels of bifidobacteria Probiotics could be used to change the “atopic” to a more “non-atopic flora” ______ Ozdemir 2010 45
Studies on Probiotics in Allergy Prevention Some studies indicate a positive outcome in reducing the incidence of allergy: Lactobacillus F 19 in cereals fed to infants from 4 to 13 months of age reduced the incidence of eczema 1 Other studies showed no effect: Bifidobacterium + Lactobacillus rhamnosus daily for the first 6 months in at risk infants had no effect compared to placebo 2 __________ 1 West et al 2009 __________ 2 Soh et al 2009 46

Current Status of Probiotics in Allergy Prevention Beneficial effects of probiotic therapy depends on: Type of bacteria selected Dosage of the bacteria delivered to the digestive tract Method of delivery of the bacteria to the GI tract (in formulae; in cereals) Age of the individual Length of duration of delivery Conclusion at the current state of research: Probiotics cannot be recommended generally for primary prevention of atopic disease _______ Ozdemir 2010 a 47

Take Home Message Allergy prevention emphasizes inducing tolerance rather than avoiding sensitization Beginning of tolerance to foods may occur in utero or during breast-feeding Restriction of maternal diet to avoid highly allergenic foods during pregnancy or lactation is contraindicated Unless either mother or baby is allergic to them 48

Take Home Message Management of established food allergy includes: Accurate identification of the allergenic food(s) Careful avoidance of the food allergens – especially if there is any risk of anaphylaxis Avoidance of unnecessary food restrictions 49
Take Home Message Provision of complete balanced nutrition by substituting foods of equal nutritional value Monitoring the child’s response at intervals to determine when the food allergy has been outgrown Maintenance of tolerance by feeding tolerated foods regularly 50
Invitation to Further Information www. allergynutrition. com Joneja, J. M. Vickerstaff Dealing with Food Allergies in Babies and Children Bull Publishing Company, Boulder, Colorado. October 2007 51
 Mikael ferm
Mikael ferm Boutonniere nodes
Boutonniere nodes Arthritis and food allergies
Arthritis and food allergies Chronic allergies icd 10
Chronic allergies icd 10 Beta glucan allergies
Beta glucan allergies Docteur simonis citadelle
Docteur simonis citadelle Now i see it now you don't
Now i see it now you don't Unit 2 food food food
Unit 2 food food food Food chain sequence
Food chain sequence Janice merigo
Janice merigo Janice gorzynski smith
Janice gorzynski smith Janice earns $3 750
Janice earns $3 750 Nadya mandel
Nadya mandel Janice toyoshima
Janice toyoshima Qian janice wang
Qian janice wang Janice hermann
Janice hermann Hemocode test
Hemocode test Janice seinfeld
Janice seinfeld Janice weinberg
Janice weinberg First nations
First nations Janice pilch
Janice pilch Janice miner holden
Janice miner holden Janice singh
Janice singh Interpretivsm
Interpretivsm Graded repetitive arm supplementary program
Graded repetitive arm supplementary program Janice adair
Janice adair Janice smith
Janice smith Andrea is a very good student. the probability
Andrea is a very good student. the probability Fearless by janice galloway
Fearless by janice galloway Pearl sydenstricker buck
Pearl sydenstricker buck Dr janice tung
Dr janice tung Majapahit coins
Majapahit coins Youtube. com
Youtube. com Janice zimmerman md
Janice zimmerman md Janice mirikitani desert flowers poem
Janice mirikitani desert flowers poem Janice lapsansky
Janice lapsansky Hue luu
Hue luu Janice weinberg
Janice weinberg What is visitor pre registration in picme
What is visitor pre registration in picme Infant industries apush
Infant industries apush Infant motrin coupon
Infant motrin coupon Reflex child development
Reflex child development Infant botulism
Infant botulism For sale infant shoes never worn
For sale infant shoes never worn Pallor cyanosis
Pallor cyanosis Kenmore park infant and nursery school
Kenmore park infant and nursery school Phoenix infant academy
Phoenix infant academy Drdp essential view
Drdp essential view Femoral pulse in child
Femoral pulse in child Saguaro infant care and preschool
Saguaro infant care and preschool Infant hip
Infant hip Infant death rate
Infant death rate