IMMEDIATE CAUSE OF DEATH AFTER SURGICAL REPAIR OF

- Slides: 24
IMMEDIATE CAUSE OF DEATH AFTER SURGICAL REPAIR OF ACUTE TYPE “A” DISSECTION Evidence from the Canadian Thoracic Aortic Collaborative 44 th Annual Symposium, The Society for Clinical Vascular Surgery Las Vegas, Nevada RS Mc. Clure MD University of Calgary Aortic Surgeon Calgary AB Canada
• The Author’s Have No Disclosures
• Co-Authors & Participating Institutions • Maral Ouzounian, MD, Ph. D University of Toronto • Munir Boodhwani, MD University of Ottawa • Ismail El-Hamamsy, MD, Ph. D University of Montreal QC • Michael W. A. Chu, MD Western University London ON • Zlatko Pozeg, MD University of Manitoba Winnipeg MB • Francois Dagenais, MD University of Laval Quebec City QC • Jehangir J. Appoo, MDCM • Khokan Sikdar , MSc, MAS, Ph. D • R Scott Mc. Clure MD SM University of Calgary Queen’s University Toronto ON Ottawa ON Calgary AB Kingston, ON
BACKGROUND • For acute type A dissection, surgery confers best chance at survival • Despite this, perioperative mortality remains high • • • (17 – 22% - based on large data registries) Perioperative risk factors for mortality have been described Data on actual cause of death remains sparse
PURPOSE This study aimed to characterize the inciting events that cause death during surgical repair of acute type A dissection • PREMISE • Characterizing the cause of death may help guide focused modifications to surgical & perioperative techniques to better outcomes
METHODS • 9 Canadian centers within the Canadian Thoracic Aortic Collaborative (CTAC) participated in the study • Retrospective study design • All patients 18 years or older who died in the perioperative period following surgical repair of an acute type A dissection between Jan 2007 – Dec 2013 were included • Patients diagnosed with an acute type A dissection but did not undergo surgical repair were excluded
METHODS Primary Outcome of Interest • Cause of death following surgical repair of acute type A dissection • Cause of death classified into 1 of 7 predetermined categories 1. Cardiac Death 2. Stroke 3. Hemorrhage 4. Other Organ Ischemia (Peripheral, Renal, Visceral) 5. Multi-organ Failure 6. Sepsis 7. Other Causes
METHODS • Single aortic surgeon from each site reviewed data and determined primary cause of death • If multiple categories may have contributed final outcome surgeon selected single inciting event most likely responsible for death • Clinical & operative variables were analyzed to delineate potential modifiable factors for mortality
STATISICAL ANALYSIS • Descriptive statistics for continuous variables (mean ± SD) • Independent t-tests (normally distributed continuous variables) • Wilcoxon Signed rank test (non-normally distributed continuous variables) • Chi-square or Fisher’s exact test (associations between clinical characteristics & cause of death for categorical variables)
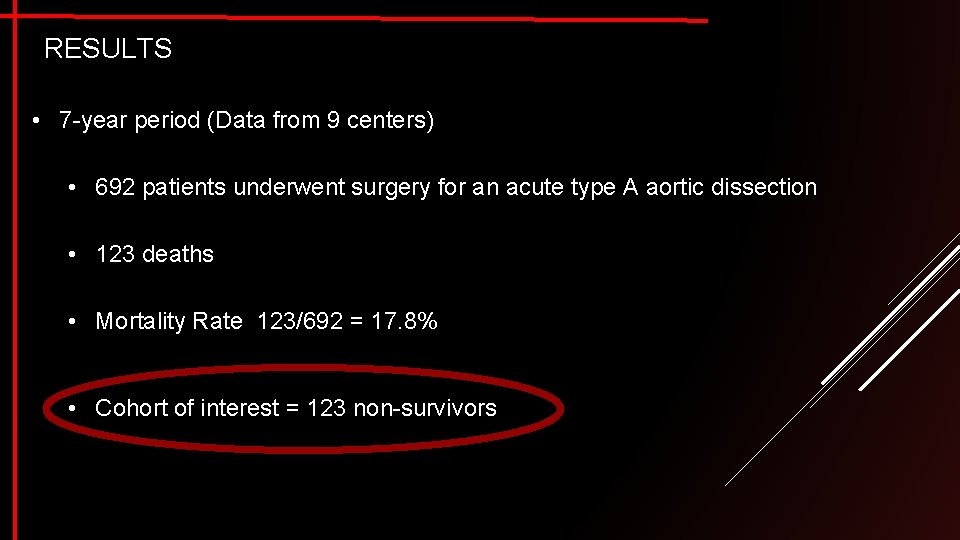
RESULTS • 7 -year period (Data from 9 centers) • 692 patients underwent surgery for an acute type A aortic dissection • 123 deaths • Mortality Rate 123/692 = 17. 8% • Cohort of interest = 123 non-survivors
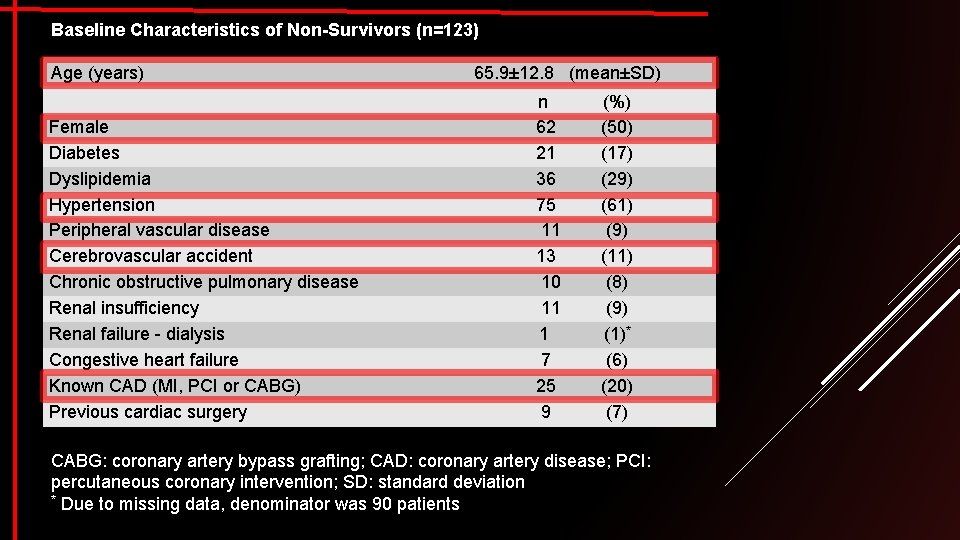
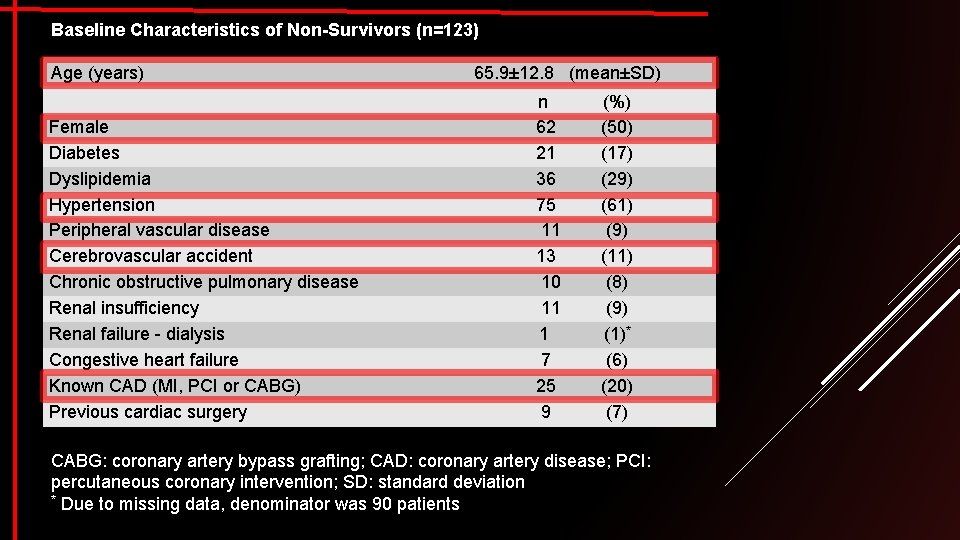
Baseline Characteristics of Non-Survivors (n=123) Age (years) Female Diabetes Dyslipidemia Hypertension Peripheral vascular disease Cerebrovascular accident Chronic obstructive pulmonary disease Renal insufficiency Renal failure - dialysis Congestive heart failure Known CAD (MI, PCI or CABG) Previous cardiac surgery 65. 9± 12. 8 (mean±SD) n 62 21 36 75 11 13 10 11 1 7 25 9 (%) (50) (17) (29) (61) (9) (11) (8) (9) (1)* (6) (20) (7) CABG: coronary artery bypass grafting; CAD: coronary artery disease; PCI: percutaneous coronary intervention; SD: standard deviation * Due to missing data, denominator was 90 patients
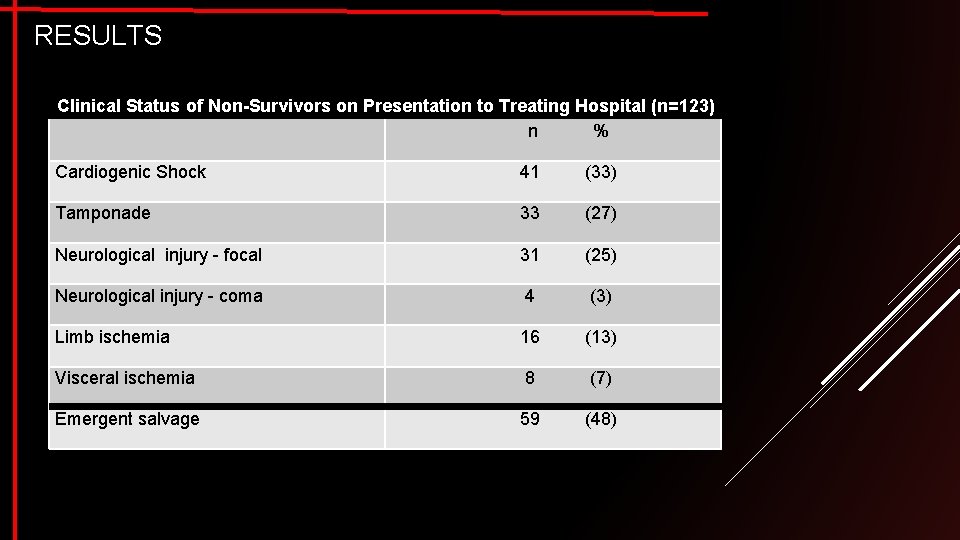
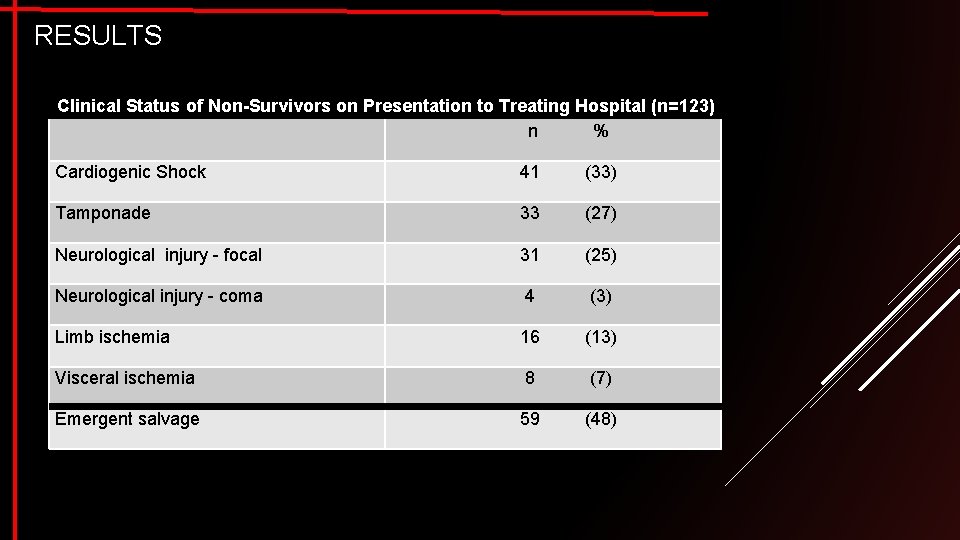
RESULTS Clinical Status of Non-Survivors on Presentation to Treating Hospital (n=123) n % Cardiogenic Shock 41 (33) Tamponade 33 (27) Neurological injury - focal 31 (25) Neurological injury - coma 4 (3) Limb ischemia 16 (13) Visceral ischemia 8 (7) Emergent salvage 59 (48)
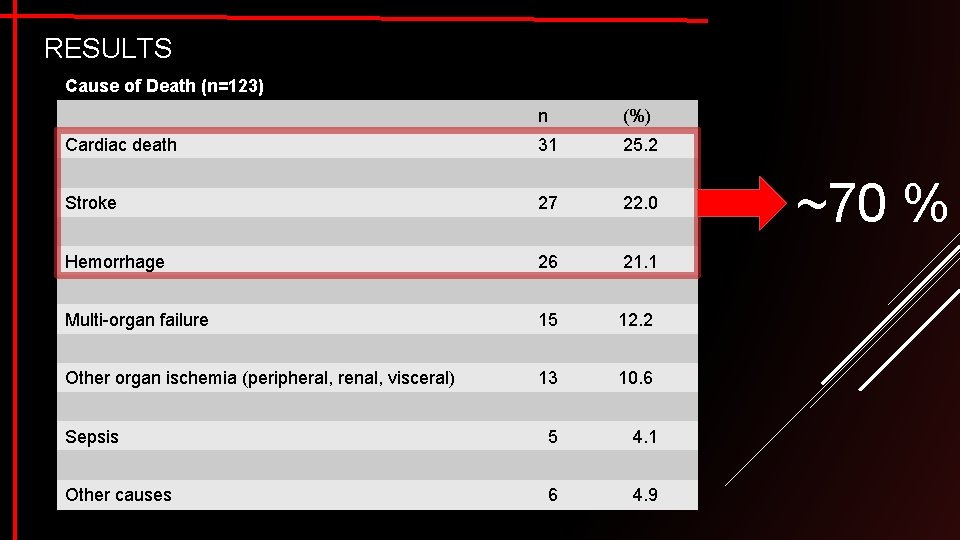
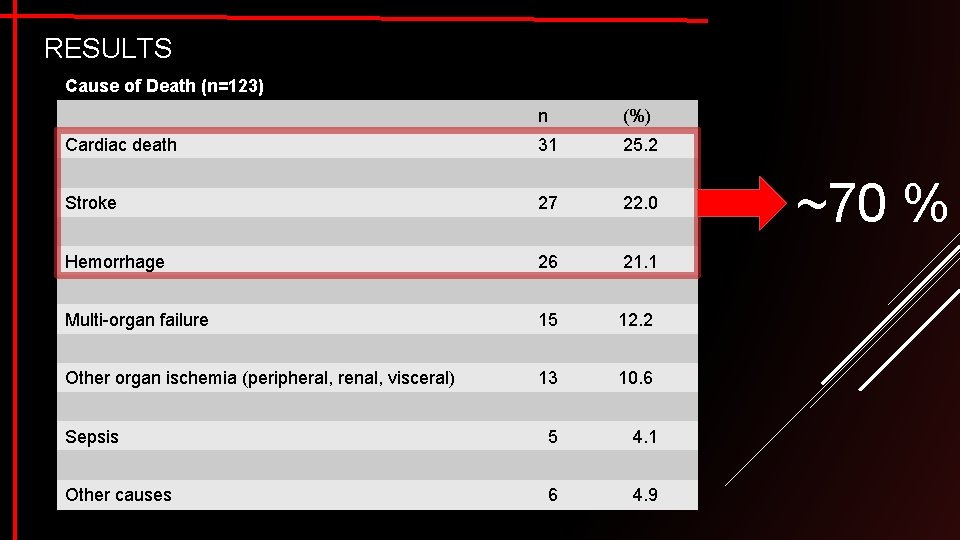
RESULTS Cause of Death (n=123) n (%) Cardiac death 31 25. 2 Stroke 27 22. 0 Hemorrhage 26 21. 1 Multi-organ failure 15 12. 2 Other organ ischemia (peripheral, renal, visceral) 13 10. 6 Sepsis 5 4. 1 Other causes 6 4. 9 ~70 %
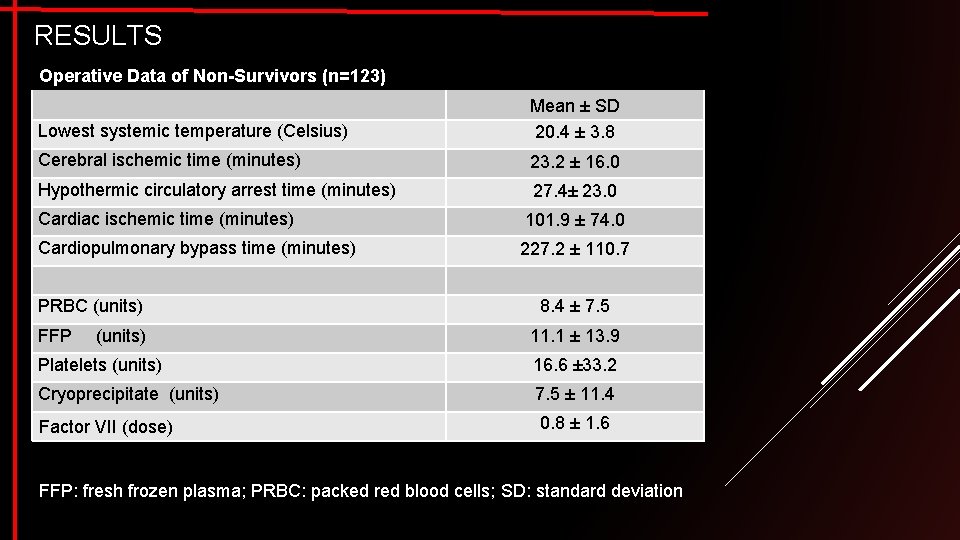
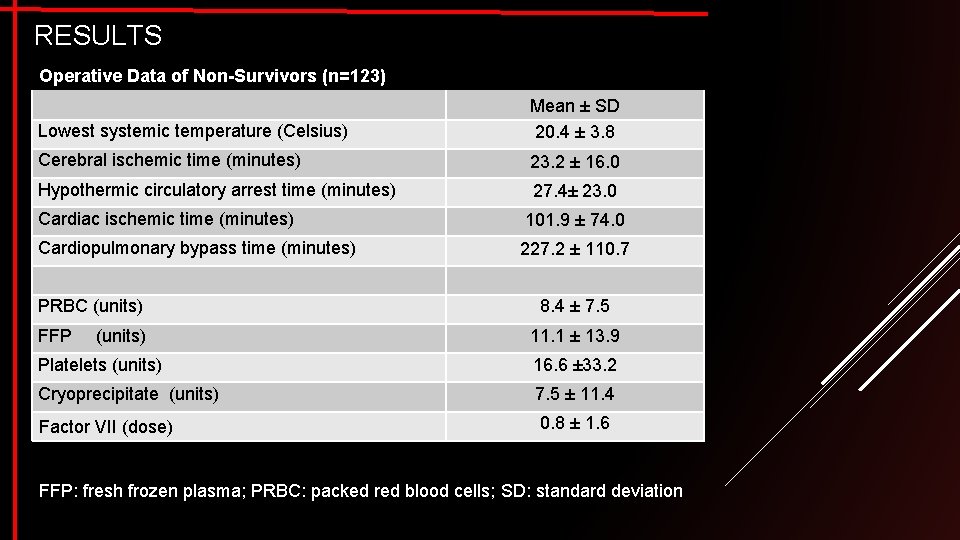
RESULTS Operative Data of Non-Survivors (n=123) Lowest systemic temperature (Celsius) Mean ± SD 20. 4 ± 3. 8 Cerebral ischemic time (minutes) 23. 2 ± 16. 0 Hypothermic circulatory arrest time (minutes) 27. 4± 23. 0 Cardiac ischemic time (minutes) 101. 9 ± 74. 0 Cardiopulmonary bypass time (minutes) 227. 2 ± 110. 7 PRBC (units) FFP (units) 8. 4 ± 7. 5 11. 1 ± 13. 9 Platelets (units) 16. 6 ± 33. 2 Cryoprecipitate (units) 7. 5 ± 11. 4 Factor VII (dose) 0. 8 ± 1. 6 FFP: fresh frozen plasma; PRBC: packed red blood cells; SD: standard deviation
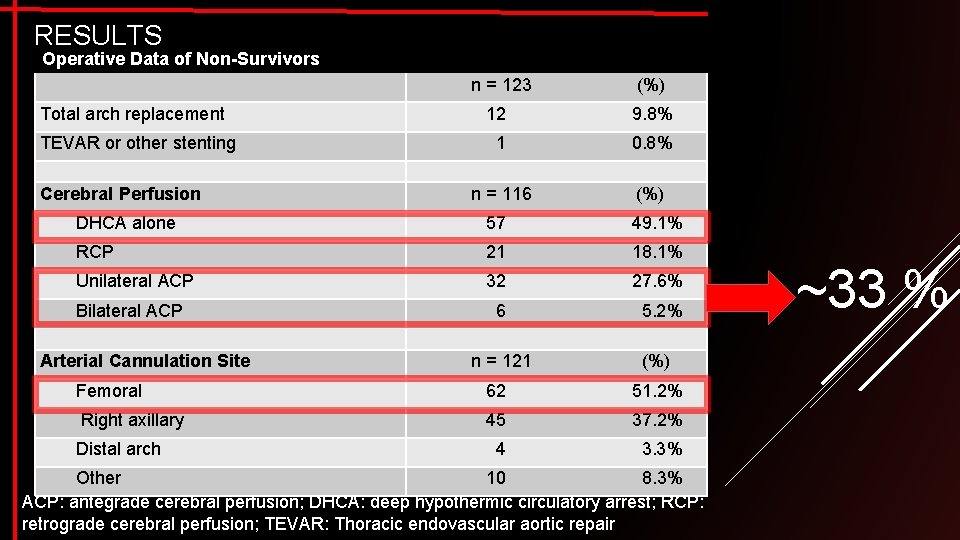
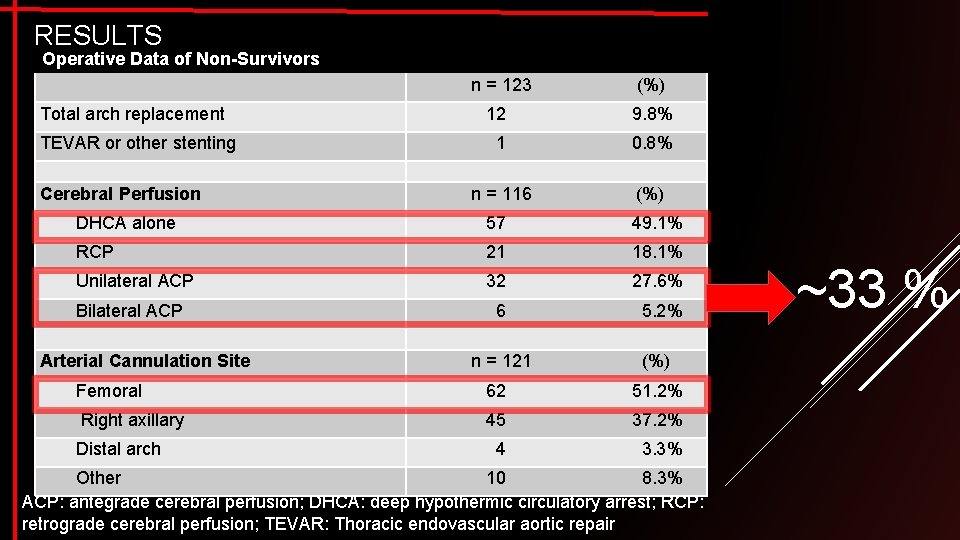
RESULTS Operative Data of Non-Survivors Total arch replacement TEVAR or other stenting Cerebral Perfusion n = 123 (%) 12 9. 8% 1 0. 8% n = 116 (%) DHCA alone 57 49. 1% RCP 21 18. 1% Unilateral ACP 32 27. 6% 6 5. 2% Bilateral ACP Arterial Cannulation Site n = 121 (%) Femoral 62 51. 2% Right axillary 45 37. 2% 4 3. 3% Distal arch Other 10 8. 3% ACP: antegrade cerebral perfusion; DHCA: deep hypothermic circulatory arrest; RCP: retrograde cerebral perfusion; TEVAR: Thoracic endovascular aortic repair ~33 %
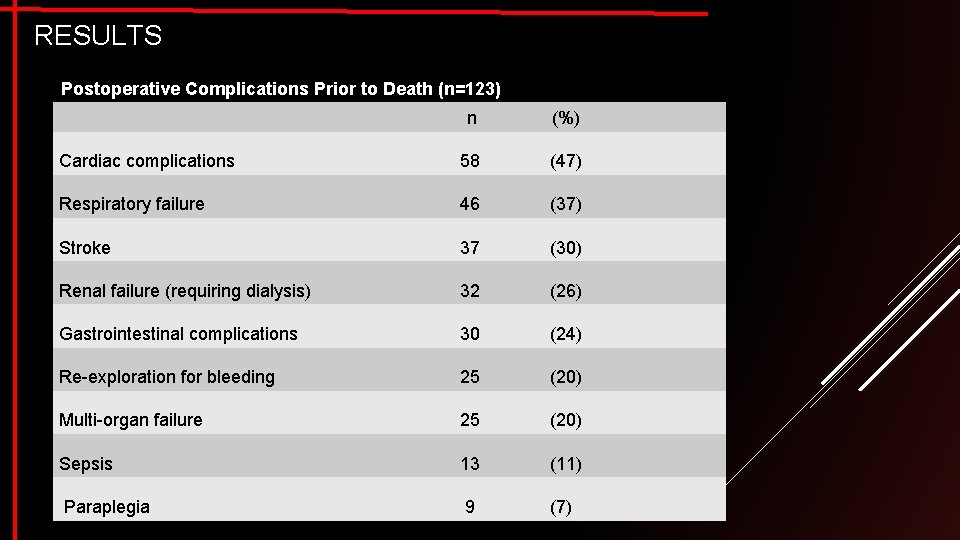
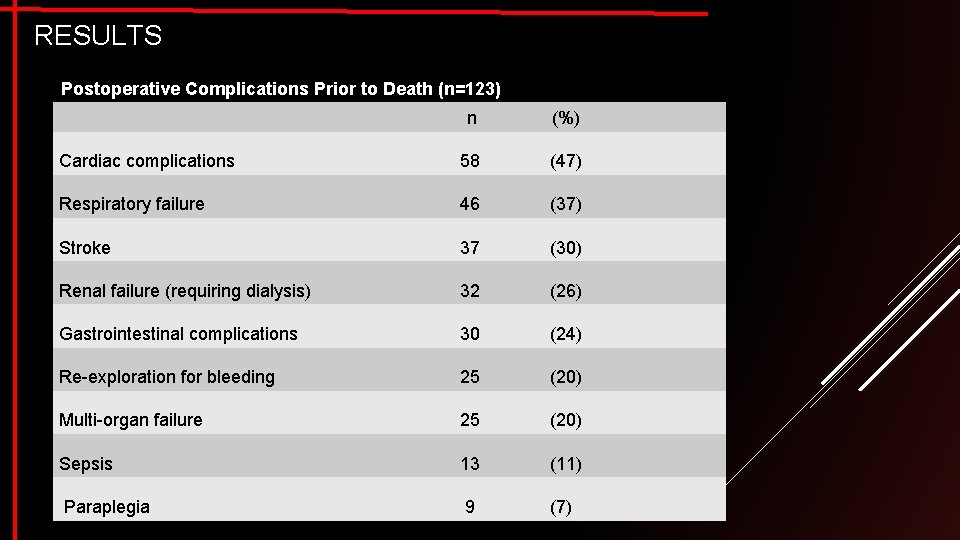
RESULTS Postoperative Complications Prior to Death (n=123) n (%) Cardiac complications 58 (47) Respiratory failure 46 (37) Stroke 37 (30) Renal failure (requiring dialysis) 32 (26) Gastrointestinal complications 30 (24) Re-exploration for bleeding 25 (20) Multi-organ failure 25 (20) Sepsis 13 (11) Paraplegia 9 (7)
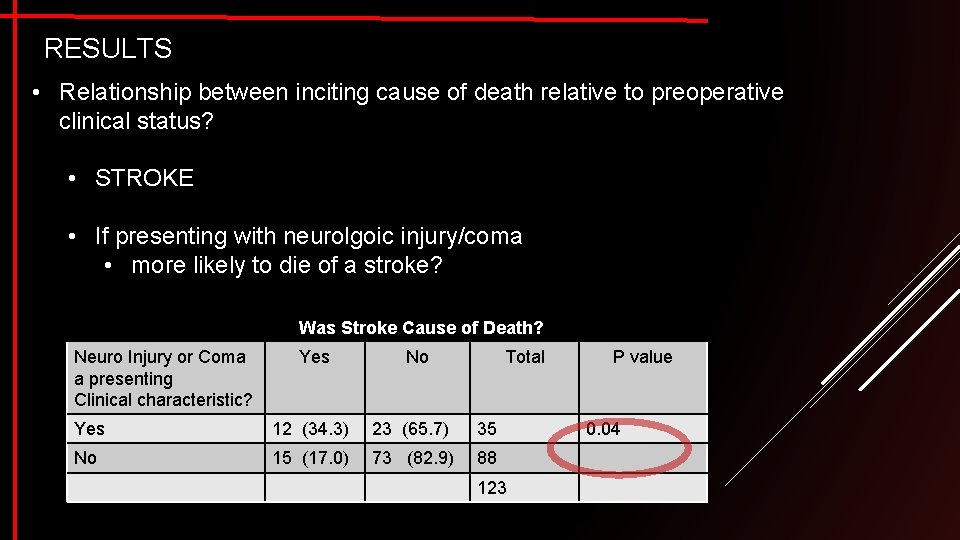
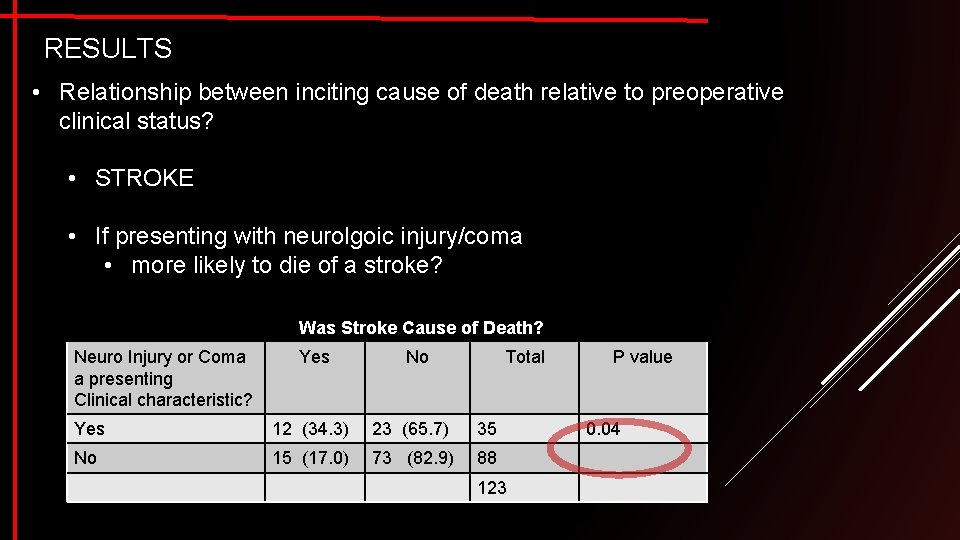
RESULTS • Relationship between inciting cause of death relative to preoperative clinical status? • STROKE • If presenting with neurolgoic injury/coma • more likely to die of a stroke? Was Stroke Cause of Death? Neuro Injury or Coma a presenting Clinical characteristic? Yes No Total Yes 12 (34. 3) 23 (65. 7) 35 No 15 (17. 0) 73 (82. 9) 88 123 P value 0. 04
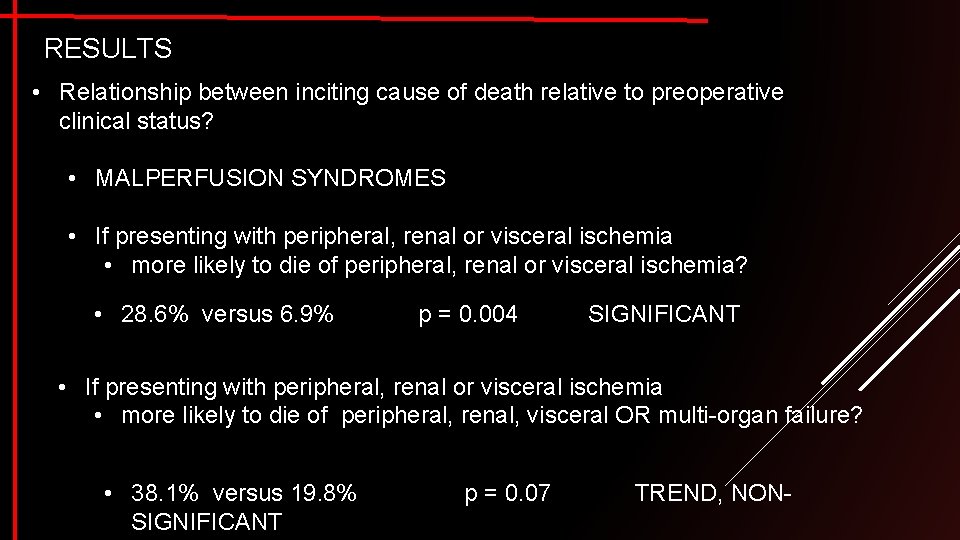
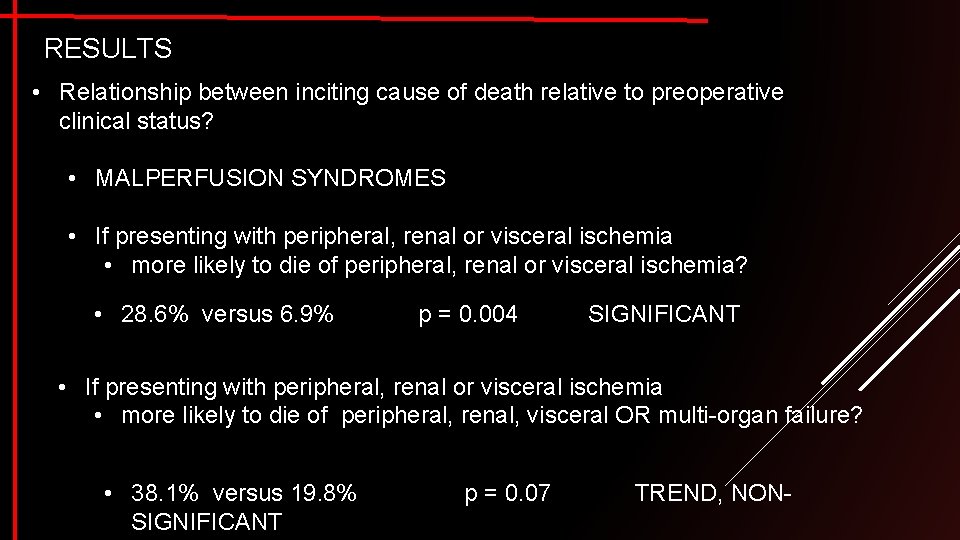
RESULTS • Relationship between inciting cause of death relative to preoperative clinical status? • MALPERFUSION SYNDROMES • If presenting with peripheral, renal or visceral ischemia • more likely to die of peripheral, renal or visceral ischemia? • 28. 6% versus 6. 9% p = 0. 004 SIGNIFICANT • If presenting with peripheral, renal or visceral ischemia • more likely to die of peripheral, renal, visceral OR multi-organ failure? • 38. 1% versus 19. 8% SIGNIFICANT p = 0. 07 TREND, NON-
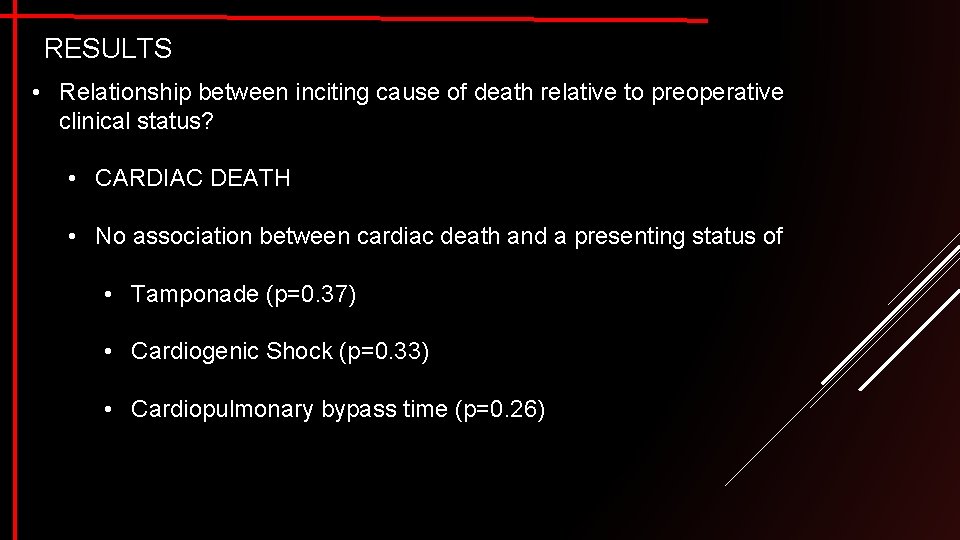
RESULTS • Relationship between inciting cause of death relative to preoperative clinical status? • CARDIAC DEATH • No association between cardiac death and a presenting status of • Tamponade (p=0. 37) • Cardiogenic Shock (p=0. 33) • Cardiopulmonary bypass time (p=0. 26)
RESULTS • Relationship between stroke death relative to surgical techniques? • No associations identified • Duration of circulatory arrest time (p=0. 93) • Antegrade cerebral perfusion relative to alternative strategies (p=0. 36) • Lowest systemic temperature (p=0. 54)
Conclusion • Operative mortality following surgical repair of acute type A dissection remains high • Stroke, hemorrhage & cardiac failure were the cause of death in nearly 70% of all cases • To improve outcomes, emerging surgical, endovascular & hybrid technologies should target these 3 areas • Cerebral perfusion and cannulation strategies are quite varied across the country. Although the reason is surely multi-factorial, these are modifiable factors. Standardized methods could have a positive impact

Thank You Calgary Thoracic Aortic Program www. aorta. ca
Limitations • Retrospective study design • Study only captures non-survivor cohort • Potential for misclassification
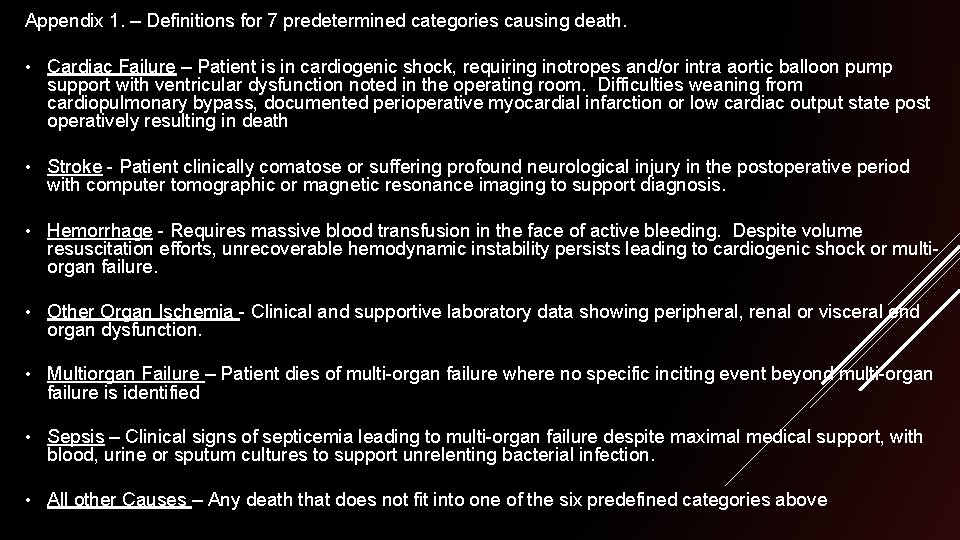
Appendix 1. – Definitions for 7 predetermined categories causing death. • Cardiac Failure – Patient is in cardiogenic shock, requiring inotropes and/or intra aortic balloon pump support with ventricular dysfunction noted in the operating room. Difficulties weaning from cardiopulmonary bypass, documented perioperative myocardial infarction or low cardiac output state post operatively resulting in death • Stroke - Patient clinically comatose or suffering profound neurological injury in the postoperative period with computer tomographic or magnetic resonance imaging to support diagnosis. • Hemorrhage - Requires massive blood transfusion in the face of active bleeding. Despite volume resuscitation efforts, unrecoverable hemodynamic instability persists leading to cardiogenic shock or multiorgan failure. • Other Organ Ischemia - Clinical and supportive laboratory data showing peripheral, renal or visceral end organ dysfunction. • Multiorgan Failure – Patient dies of multi-organ failure where no specific inciting event beyond multi-organ failure is identified • Sepsis – Clinical signs of septicemia leading to multi-organ failure despite maximal medical support, with blood, urine or sputum cultures to support unrelenting bacterial infection. • All other Causes – Any death that does not fit into one of the six predefined categories above
 Underlying cause and immediate cause
Underlying cause and immediate cause Cadaveric spasm and rigor mortis difference
Cadaveric spasm and rigor mortis difference Base excision repair
Base excision repair Base excision repair
Base excision repair After me after me after me
After me after me after me If any man comes after me
If any man comes after me What was an immediate cause of the 1789 french revolution
What was an immediate cause of the 1789 french revolution Immediate cause of ww1
Immediate cause of ww1 Immediate cause of world war 2
Immediate cause of world war 2 The effects of the french revolution
The effects of the french revolution Immediate cause of french revolution
Immediate cause of french revolution World war 2 brain pop
World war 2 brain pop Imprinting biology example
Imprinting biology example Greylag goose egg-retrieval behavior
Greylag goose egg-retrieval behavior Proximate vs ultimate causation
Proximate vs ultimate causation Eldridge moores cause of death
Eldridge moores cause of death Yana novotna cause of death
Yana novotna cause of death Antonio vivaldi cause of death
Antonio vivaldi cause of death Jacqui saburido cause of death
Jacqui saburido cause of death Manner mechanism and cause of death
Manner mechanism and cause of death Whmis acronym
Whmis acronym What was humpty dumpty's cause of death geometry
What was humpty dumpty's cause of death geometry Masako natsume cause of death
Masako natsume cause of death Daily iodine requirement
Daily iodine requirement Portia may white early life
Portia may white early life