HYSTRECTOMY Definition Hysterectomy Is the surgical removal of
- Slides: 17
HYSTRECTOMY
Definition: • Hysterectomy: Is the surgical removal of the uterus Types: . Emergency: to control life-threatening bleeding or hemorrhage, and in the event of intractable pelvic infection or irreparable rupture of the uterus. Planned : performed for removing fibroids.
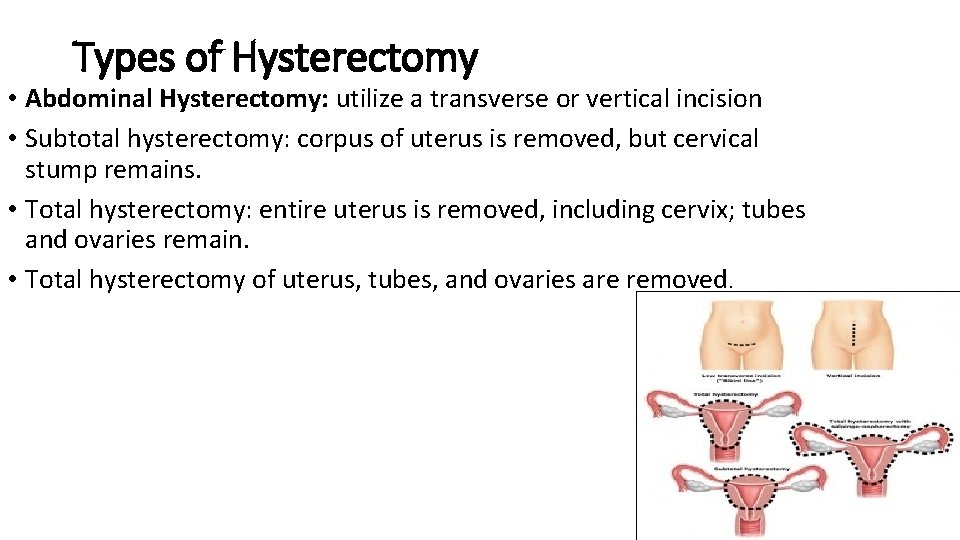
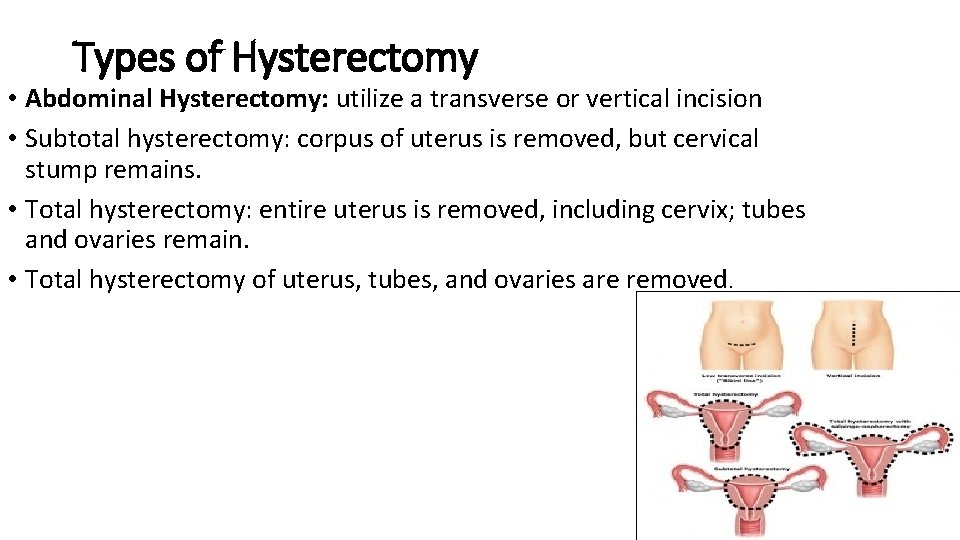
Types of Hysterectomy • Abdominal Hysterectomy: utilize a transverse or vertical incision • Subtotal hysterectomy: corpus of uterus is removed, but cervical stump remains. • Total hysterectomy: entire uterus is removed, including cervix; tubes and ovaries remain. • Total hysterectomy of uterus, tubes, and ovaries are removed.
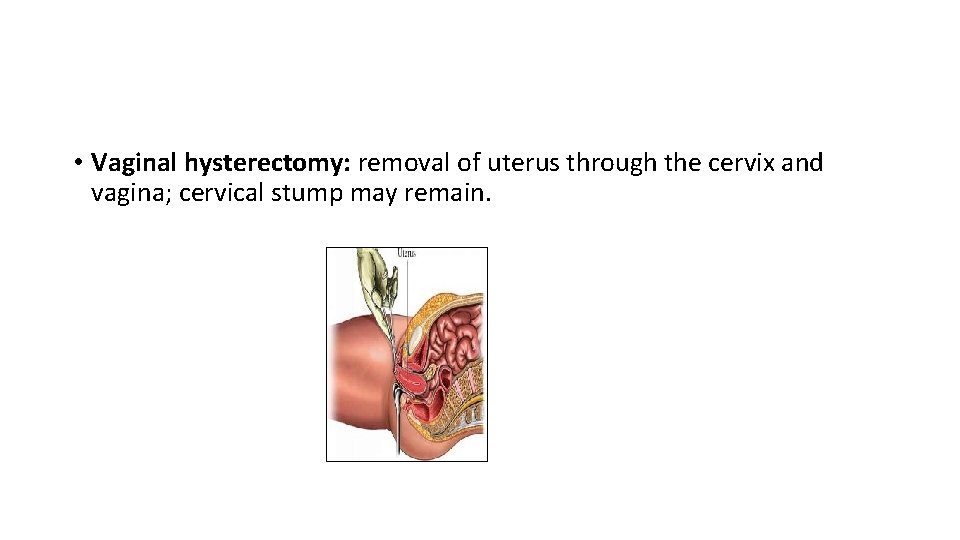
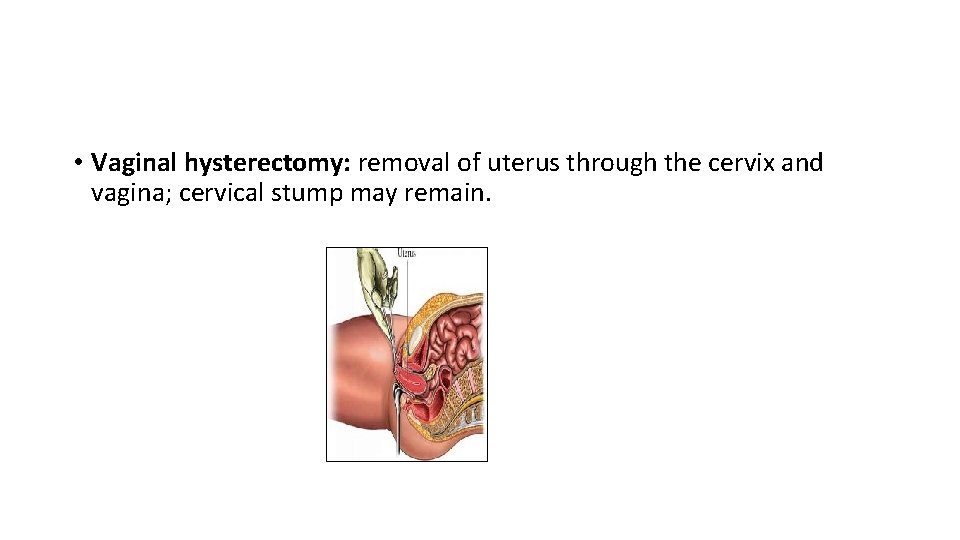
• Vaginal hysterectomy: removal of uterus through the cervix and vagina; cervical stump may remain.
• Laparoscopic supracervical hysterectomy: laparoscopic removal of the uterus but the cervix is remaining.
Indications: • • • Uterine fibroids about 30% of cases Endometriosis and adenomyosis about 20% of cases Dysfunctional uterine bleeding Uterine prolepses Chronic pelvic pain about 10% of cases Cancer of the vagina, cervix, uterus, ovaries, or fallopian tub.
Complications: • Incision/pelvic infection. • Hemorrhage. • Urinary tract injury. • Bowel obstruction. • Thrombophlebitis/deep vein thrombosis (DVT)
Pre-operative Nursing Care: • Explain procedure and reason for hysterectomy, what the procedure involve, and what to expect postoperatively are explained. • Patient must remain NPO from midnight the night before surgery and must void before surgery. • An enema is administered before surgery to evacuate the bowel and prevent contamination and trauma during surgery. • Vaginal irrigation is performed before surgery with normal saline solution and skin preparation is done if ordered. • Preoperative medication is given to help the patient relax. (eg, morphine) • Check the patient recored. • Check the history of OCP, to administer Hormonal Replacement post oprative. • Wear elastic stocking pre operative to prevent DVT.
Post-Operative Nursing Care: • Assess vital sign, upon arrival then Q 30 min. times 1 then Q 1 hr. times 1 then Q 2 hrs. times 4 then Q 4 hrs. and intake and output • Assess for complication as infection, pneumonia, hemorrhageshock, and thrombophlebitis. After 24 hours of postoperative. • Auscultate chest for breathing sound • Observe the incision q 4 hrs or as order • Bowel management: Auscultate bowel sound q 6 hrs to 8 hrs by encouraging her to move out of bed, prevent increase in intraabdominal pressure which will cause bleeding by avoiding constipation by Administer medications: stool softeners, mineral oil, laxatives, as indicated. stool softner and laxatives , until peristalsis begins, food and fluid intake promote resumption of normal bowel elimination.
• Bladder management : • Note voiding pattern and monitor urinary output. • Provide routine voiding measures: privacy, normal position, running water in sink, pouring warm water over perineum • Provide and encourage good perianal cleansing and catheter care (when present). educing risk of ascending urinary tract infection (UTI). • Vaginal packing removal after 24 hours • Apply dry heat to promote healing • Patient should be kept in Supine Position and Avoid high-Fowler’s position and pressure under the knees or crossing of legs. Because it creates vascular stasis by increasing pelvic congestion and pooling of blood in the extremities, potentiating risk of thrombus formation. • Identify dietary needs. Give foods high in protein and iron. Facilitates healing and tissue regeneration and helps correct anemia when present.
• Ensure that patient turn, cough, and deep breathing at least every 2 hrs to aid in respiratory excursion and to prevent stasis • Teach the patient to use a pillow over abdominal sutures to aid abdominal muscles and decrease the pressure associated with coughing. • Keep patient in low flower’s or flat position to prevent increased intraabdominal pressure, and avoid placing client in high- fowler’s position and placing pressure under the knee to prevent stasis and pooling of blood in the extremities • Avoid sitting with knee bent and crossing legs • Apply antiembolic stocking and assist in passive and active exercise at least every 4 hrs to enhance circulation and to aid venous return • Encourage ambulation as soon as possible
• Promote micturition at regular intervals when catheter is removed • Check for homan’s sign “calf tenderness or pain” at least once shift to assess for Thrombophlebitis • Change perineal pads as needed, observing vaginal discharge described color, amount and odor. • Administer antibiotic and hormone replacement therapy as order. • Assess the dressing for the sign of bleeding and infection
• Encourage adequate fluid and food as soon as tolerated and peristalsis resume. • Offer prune juice once peristalsis is resumed • Discuss emotional liability with patient – family and expectation for the grieving process include sadness and depression, assure patient- family that the ability to cope and remain in control in due course • Help family – friend to understand patient need for repeated reassurance of their love, concern, and availability, encourage them to support her attractiveness and her self-esteem, explore cultural attitude regarding the female role in order to learn it’s probable effect the patient perceptions.
Discharge Education: • Instruct her to ambulate at regular intervals • Avoid sitting for prolonged period at home or when traveling because of the possibility of blood pooling in the lower extremities, which increases the risk of thromboembolism and increase intra-abdominal pressure so increase stress on the wound. • Instructs her to care for incision and teach the sign of infection as redness, swelling, pain, discharge or increase in vaginal drainage, foul odor. • Eat 3 balance meals a day, including 6 -8 glass of water • Explain to avoid heavy lifting and vigorous activities for 6 weeks after surgery. • Avoid Situational Low Self-Esteem: Development of a negative perception of self-worth in response to current situation by Providing time to listen to her concerns and fears. • Sexual relation support Assess patient’s information regarding sexual anatomy, using positions that avoid pressure on abdominal incision, using vaginal lubricant will Help the patient return to desired or satisfying sexual activity.
• Explain to avoid constipation and straining at stool • Avoid sexual intercourse for 4 to 6 weeks or as indicated by doctors. • Discuss changes regarded sexual functioning, such as shortened vagina and possible dyspareunia because of dryness and offer suggestion for her as use water soluble jell. • Avoid douching, tampons, or anything in vagina for 4 to 6 weeks or as indicated by physician • Follow up and maintaining regular gynecological examinations.
Warning signs to come back to hospital immediately : • You have bright red vaginal bleeding that soaks one or more pads in an hour, or you have large clots. • You have foul-smelling discharge from your vagina. • You are sick to your stomach or cannot keep fluids down. • You have signs of infection, such as: • • • Increased pain, swelling, warmth, or redness. Red streaks leading from the incision. Pus draining from the incision. Swollen lymph nodes in your neck, armpits, or groin. A fever.
• You have pain that does not get better after you take pain medicine. • You have loose stitches, or your incision comes open. • You have signs of a blood clot, such as: • Pain in your calf, back of knee, thigh, or groin. • Redness and swelling in your leg or groin. • You have trouble passing urine or stool, especially if you have pain or swelling in your lower belly. • You have hot flashes, sweating, flushing, or a fast or pounding heartbeat.
 Most common site of ureteric injury during hysterectomy
Most common site of ureteric injury during hysterectomy Indications of hysterectomy
Indications of hysterectomy Cesarean hysterectomy steps
Cesarean hysterectomy steps Disadvantages of laparoscopic hysterectomy
Disadvantages of laparoscopic hysterectomy Hysterectomy
Hysterectomy Surgical audit examples
Surgical audit examples Horizontal mattress
Horizontal mattress Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Glasgow thang điểm
Glasgow thang điểm Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Môn thể thao bắt đầu bằng từ đua
Môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực