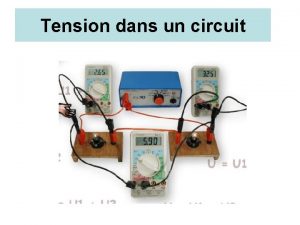
Headaches Alan Chan MD 12 16 prevalence Tension

- Slides: 24
Headaches Alan Chan, MD
• • 12 -16 % prevalence Tension most common Cluster HA men > women All other types women > men • International Headache Society (IHS) classification updated in 2004 • HA, cranial neuralgia, facial pain syndromes.
HA • Migraine – 2/3 unilat, 1/3 bilat or global; crescendo pattern, pulsating; 4 -72 hr; +/aura • Tension – bilat, pressure/tightness variable; indeterminate length • Cluster – unilat, quick and explosive; patient active; < 3 hr; ipsilat facial symptoms – tearing, nasal congestion, Horner’s, rarely focal neuro symptoms
Ddx – less common • • • Paroxysmal hemicrania Idiopathic stabbing headache Cold-stimulus headache Benign cough headache Benign exertional headache Headache associated with sexual activity
Other HA • Secondary HA – associated with trauma, vascular disorder, nonvascular intracranial disorder, substance use or withdrawal, infection, metabolic disorder, other facial or cranial structures
Get some hx • Triggers – Diet, stress, hormones, sensory stimuli, change in habit or environment • Important questions in history – frequency of severe headache (difficult to function) – frequency of milder HA – frequency of taking analgesics – change in HA
Image if… • recent significant change in pattern, frequency, or severity • worsening despite therapy • focal neurological signs/symptoms • HA with exertion, cough, or sexual activity • Orbital bruit • Onset after age 40
Migraine • episodes of severe HA typically with nausea +/- photo/phonophobia

Pathophysiology - NOT vascular dilatation of blood vessels • Primary neuro dysfunction leading to premonitory symptoms, aura, HA, and postdrome • Central process either brainstem or cortical spreading depression – causes aura, activates trigeminal nerve afferent fibers, alter blood brain barrier (BBB) permeability
• trigeminovascular system – activity leading to stimulation releases vasoactive neuropeptides of substance P, calcitonin gene-related protein (CGRP, which is a profound endogenous vasodilator), neurokinin A, activation of arachadonic acid cascade • sensitization – neurons get progressive more sensitive to nociceptive and non-nociceptive stimulation
More… • Genetics – approx 3 x risk in patients with relatives who had migraines. Non-Mendelian pattern of inheritance • Prodrome – 60% of people with migraine; can occur 1 -2 days prior to HA onset. Includes depression, irritability, constipation, euphoria, food craving, increased yawning. • Aura – 25%; typically visual like scotoma, but can be sensory, verbal, or motor • Headache – typically unilateral and throb/pulse • Postdrome – exhausted, sudden head mvt causes pain
Diagnosis – without aura • Headache attacks last 4 to 72 hours • Headache has at least two of the following characteristics: unilateral location; pulsating quality; moderate or severe intensity; aggravation by routine physical activity • During headache at least one of the following occurs: nausea and/or vomiting; photophobia and phonophobia • At least five attacks occur fulfilling the above criteria • History, physical examination, and neurologic examination do not suggest any underlying organic disease
Aura • At least one of the following characteristics without motor weakness: – Fully reversible visual symptoms including positive features (eg, flickering lights, spots, or lines) and/or negative features (eg, loss of vision) – Fully reversible sensory symptoms including positive features (eg, pins and needles) and/or negative features (eg, numbness) – Fully reversible dysphasic speech disturbance • Aura has at least two of the following characteristics: – Homonymous visual symptoms and/or unilateral sensory symptoms – At least one aura symptom develops gradually over ≥ 5 minutes and/or different aura symptoms occur in succession over ≥ 5 minutes – Each symptom lasts ≥ 5 and ≤ 60 minutes
Complications • Chronic (>15 days a month for > 3 months in absence of drug overuse) • Status migrainosus - > 72 hr and debilitating • Persistent aura without infarction – aura > 1 wk • Migrainous infarction – deficit > 1 hr and positive imaging • Migraine triggered seizure
Acute therapy • NSAIDs, combo Tylenol/ASA/caffeine, triptans, ergots like dihydroergotamine (DHE), opioids (but weak evidence only for butorphanol nasal and worry about abuse and transformation into chronic daily HA), IV metoclopramide.
Preventive Tx – can take as long as 2 -3 months to see benefit. • Treat if >2 a month that last > 3 days of disability, contraindication to acute tx, > 2 times a week use of acute tx, presence of uncommon conditions • Nonselective beta blockers – propranolol studied the most • TCA (better for mixed migraine and tension HA) like amitriptylline as others not studies as much; limited evidence for fluoxetine • Anticonvulsants - divalproex sodium and sodium valproate, limited evidence for gabapentin • NSAIDs – only naproxen with modest effect, but overuse syndrome • Serotonergic agent – ergot like DHE
• Keep a headache diary of related activities and triggers!
Cluster Headache • trigeminal autonomic cephalalgias, which are short, unilat, severe with autonomic symptoms (ptosis, miosis, lacrimation, conjunctival injection, rhinorrhea, nasal congestion)
• • Prevalence - <1 % Dx – very typical. < 3 hrs Tx – Acute – O 2, triptans, octreotide, lidocaine (intranasal), ergot • Preventive – CCB like verapamil, glucocorticoids, lithium (limited evidence), topiramate • Others less used – pizotifen (anti serotonergic), valproic acid, capsaicin, ergot, melatonin, indomethacin, triptans
Tension type headache (TTH) • Most common • Types – infrequent episodic (< 1 /month), freq episodic (1 -14/month), and chronic (> 15 days a month) • PP – multifactorial. Normally innocuous stimuli are interpreted as pain in the dorsal horn neurons. Some genetic role. Women slightly more than men. Blacks less than whites.
Dx – usually non descript! • TTH is characterized by having at least two of the following four features: • The location of the pain is bilateral in either the head or neck • The quality of the pain is steady (eg, pressing or tightening) and nonthrobbing • The intensity of the pain is mild to moderate • There is no aggravation of the headache by normal physical activity
• In addition to these criteria, there must be at least 10 headache episodes fulfilling all other ICHD-2 criteria, which include the following: • The duration of pain is between 30 minutes to 7 days • The headache is not attributable to another disorder
Tx • Acute – early tx, some may require a higher dose, avoid overuse, consider preventive. Tylenol, NSAIDs, ASA. Add some caffeine, but may get side effects. Butalbital and opioids generally not recommended. • Preventive – TCAs, Serotonin-NE reuptake inhibitors like venlafaxine, behavioral like CBT, relaxation, biofeedback
References • Uptodate. com • Snow V, Weiss K, Wall EM, et al. Pharmacologic Management of Acute Attacks of Migraine and Prevention of Migraine Headache. Ann Int Med. 2002. 137(10): 840 -849. • Clinch CR. Evaluation of Acute Headaches in Adults. Am Fam Physician. 2001. 63(4): 685693. • Tepper SJ, Spears RC. Acute Treatment of Migraine. Neuro Clinics 2009. 27(2): 417 -427
 Period prevalence vs point prevalence
Period prevalence vs point prevalence Prevalence defination
Prevalence defination Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Apsasia
Apsasia Bé thì chăn nghé chăn trâu
Bé thì chăn nghé chăn trâu Dr alan chan
Dr alan chan Dr alan chan
Dr alan chan Spin coat
Spin coat Transference and counter transference
Transference and counter transference Energi bebas permukaan
Energi bebas permukaan Prevalence ratio
Prevalence ratio Bates method eye
Bates method eye Incidence and prevalence meaning
Incidence and prevalence meaning Prevalence calculation
Prevalence calculation Contoh soal attack rate
Contoh soal attack rate Mortality formula
Mortality formula Adhd prevalence by country
Adhd prevalence by country Incidence vs incidence rate
Incidence vs incidence rate Prevalence
Prevalence Prevalence
Prevalence Calculate prevalence rate
Calculate prevalence rate Incidence vs prevalence
Incidence vs prevalence Point prevalence rate adalah
Point prevalence rate adalah Uuuu_limited
Uuuu_limited