Gynecology skills training The Dept of clinical medicine

![l l The appropriate sized speculum is selected. [3] The speculum is slowly inserted l l The appropriate sized speculum is selected. [3] The speculum is slowly inserted](https://slidetodoc.com/presentation_image_h2/031987f8dfb102116c2111ab42839cae/image-26.jpg)
![l l The appropriate sized speculum is selected. [3] The speculum is slowly inserted l l The appropriate sized speculum is selected. [3] The speculum is slowly inserted](https://slidetodoc.com/presentation_image_h2/031987f8dfb102116c2111ab42839cae/image-27.jpg)


- Slides: 44
Gynecology skills training The Dept. of clinical medicine , yangzhou medical college
l l l 1. gynecologic examination("bimanual exam) 2. culdocentesis 3. cervical smea
l The examination can be uncomfortable. During the pelvic exam the vaginal wall is assessed for rugae, texture and weak spots. In addition to a thorough pelvic exam, other tests may ordered to further determine the cause of symptoms that are concerning. During the pelvic exam, samples of vaginal fluids may be taken to screen for sexually transmitted infections or other infections.
l Some clinicians combine a routine pelvic exam along with other preventative procedures like a breast examination and pap smear.
l The pelvic exam begins with an explanation of the procedure. The woman is asked to put on an examination gown, get on the examination table, lay on her back with her feet in stirrups. Sliding down toward the end of the table is the best position for the clinician to do a visual examination. A pelvic exam begins with an assessment of the reproductive organs that can be seen without the use of a speculum. Many women may want to 'prepare' for the procedure. Douching before the exam is discouraged because cells needed from the cervix to assess for cervical cell abnormalities may be washed out.
l One possible reason for delaying an exam is if it is to be done during menstruation, but this is a preference of some women and not a requirement of the clinician. The woman will probably will be asked to put on an examination gown and lay down on the examination table. A girl or woman may ask to have another woman in the examination room during the exam. The clinician may want to perform pelvic examination and assessment of the vagina because there are unexplained symptoms of vaginal discharge, pelvic pain, unexpected bleeding, or urinary problems.
l l l The typical external examination begins with making sure that a woman is in a comfortable position and her privacy respected. If a woman is obese, different positioning and assistance may be required to keep tissue from blocking the view of the perineal area. [3] The pubic hair is inspected for pubic lice and hair growth patterns. Sparse hair patterns can exist in older and in some Asian women. [3]
l The labia majora are evaluated. Their position and symmetry are assessed. The expected finding in older women is that the labia majora can be thinner and smaller. The examiner is looking for ulcers, inflammation, warts and rashes. If drainage is present from these structures, its color, location and other characteristics are noted. Infection control is accomplished by frequent glove changes. [3]
l l The labia minora are then evaluated. They should appear moist, smooth in texture and pink. The presence of tearing, inflammation and swelling is noted. Thinner and smaller labia minora are an expected finding in older women. T he clitoris is assessed for size, position, symmetry, and inflammation. [3]
l The urethral opening is inspected. No urine should leak when the woman is asked to cough. Urine leakage may indicate stress incontinence and the weakening of pelvic structures. The opening should be midline, pink, and smooth. The presence of inflammation, or discharge which may indicate an infection. Excoriation can be present in obese women due to urinary incontinence. [3]
l The vaginal opening is inspected for position, presence of the hymen, and shape. The presence of bruising, tearing, inflammation and discharge. Pelvic examinations are usually procedures that are designed to obtain objective, measurable descriptions of what is observed. If sexual abuse is suspected, questions regarding this is discussed after the examination and not during it. When the woman is requested to 'bear down', the presence of prolapsed structures are documented. Prolapsed structures can appear when abdominal pressure increases or they can hang free without bearing down.
l l The perineum, the space between the vagina and the anus is inspected. It should be smooth, firm and free of disease. Scars from episiotomies are visible on women who have had the procedure during childbirth. [3][9] The anus is assessed for lesions, inflammation or trauma. It should appear dark, continuous and moist. In an obese women, excoriation may be present due to fecal incontinence
l Before inserting the speculum, the vaginal wall, urethra, Skene's glands and Bartholin's glands are palpated through the vaginal wall. During the internal exam, the examiner describes the procedure while doing the assessment, making sure that the woman can anticipate where she will feel the palpations

l l l The woman is first informed that the examiner will insert their finger into the vagina. The palpation of the vagina is done by evaluating the condition of the vaginal walls. These should feel smooth, consistent and soft. The rugae can also be assessed by palpation. [3] The woman is again asked to bear down while the examiner continues the internal examination. The presence of bulging is assessed. [3] The position of the urethra is assessed by palpation with a finger through the vaginal wall. [3]
l l The Skene's glands, located on each side of the urethra are palpated to produce secretion from the glands. The Bartholin glands are also assessed internally by gently squeezing them with one finger placed externally, on the posterior labia majora and the other finger in the vagina.
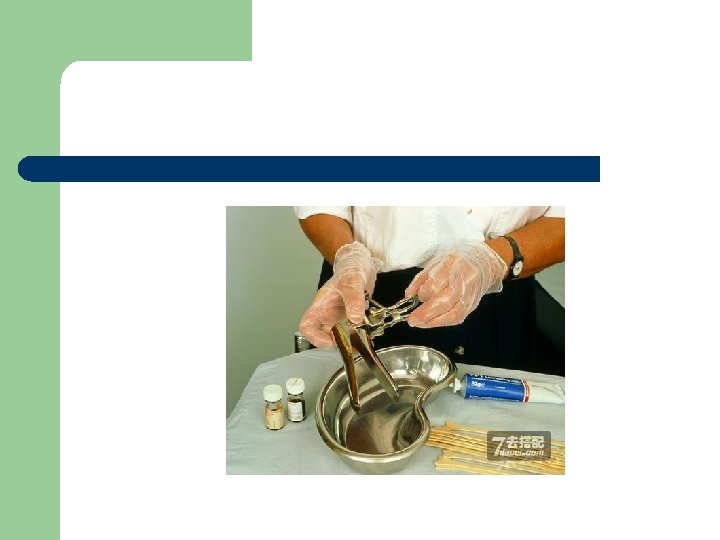
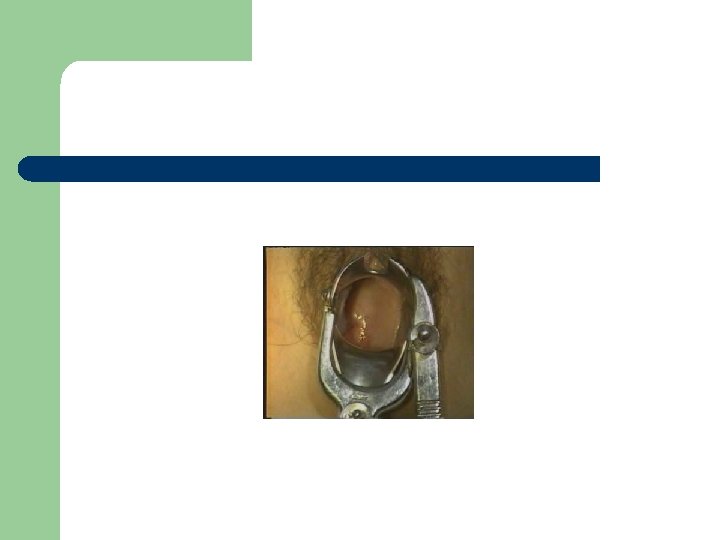
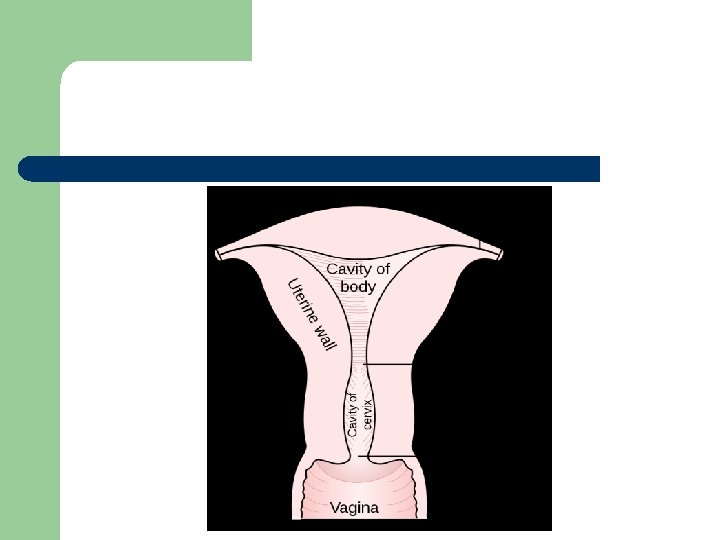
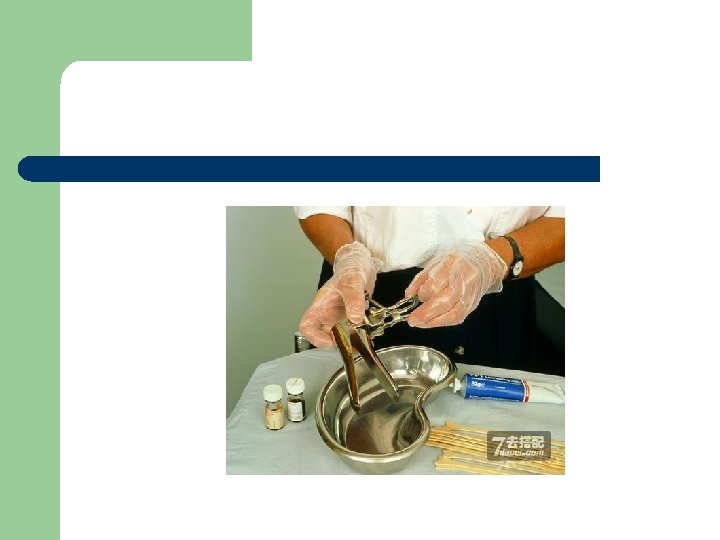
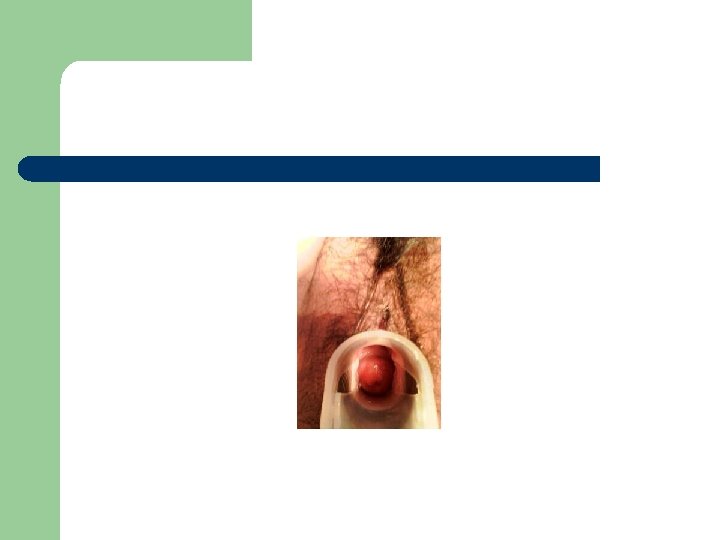
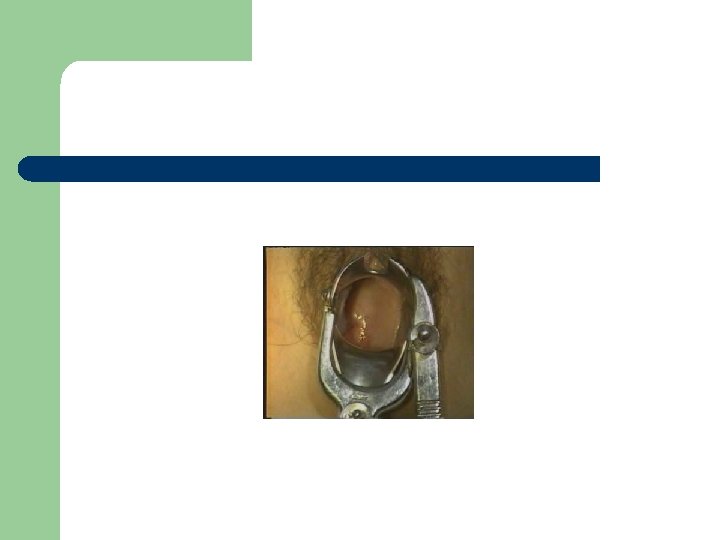
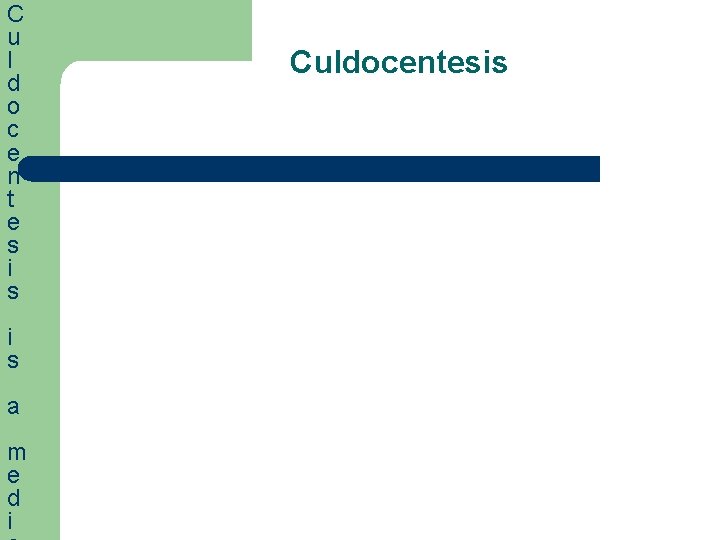
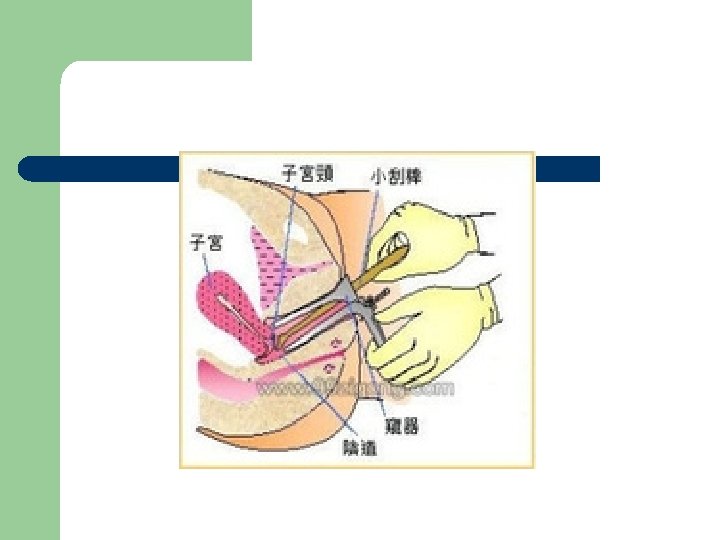
l At this point of the pelvic exam, the examiner will insert the speculum to visualize other internal structures: the cervix, uterus, and ovaries. [3][10] If this is the first pelvic exam of the woman, the examiner will show the speculum to the woman, explain its use and answer any questions.
![l l The appropriate sized speculum is selected 3 The speculum is slowly inserted l l The appropriate sized speculum is selected. [3] The speculum is slowly inserted](https://slidetodoc.com/presentation_image_h2/031987f8dfb102116c2111ab42839cae/image-26.jpg)
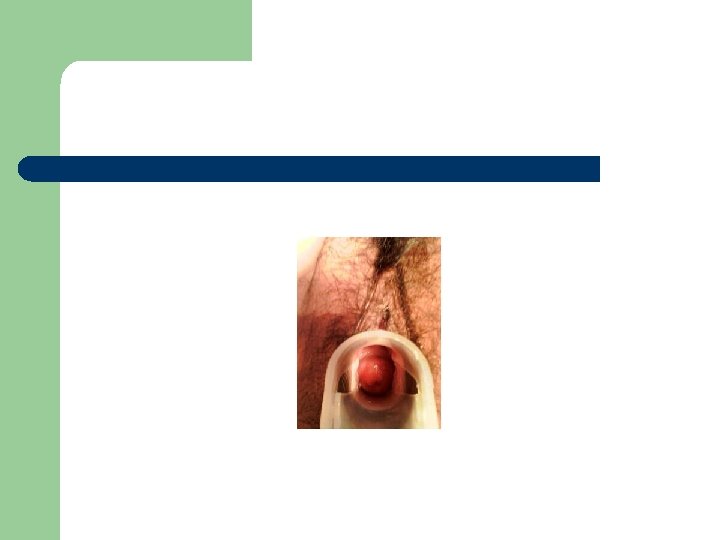
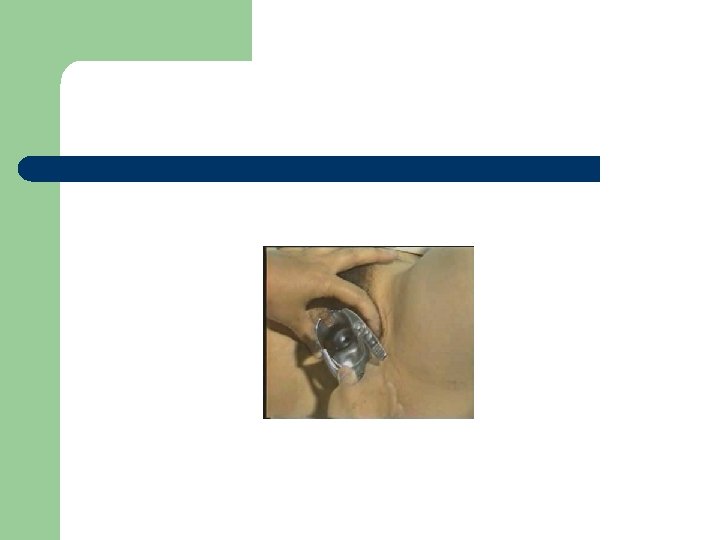
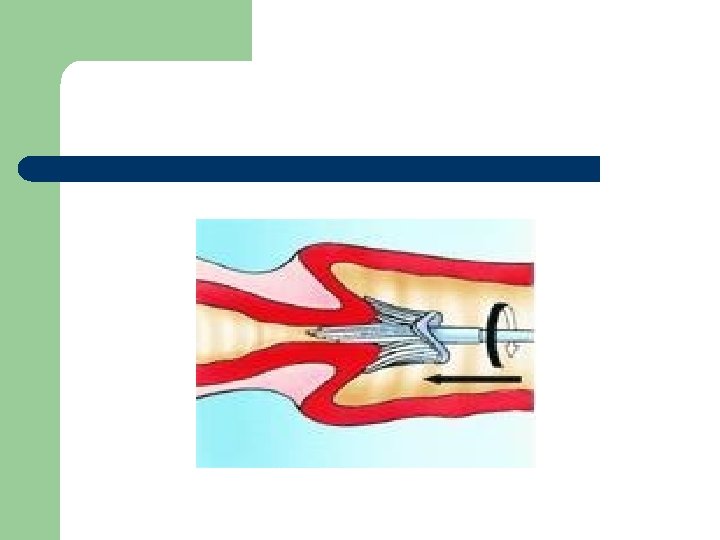
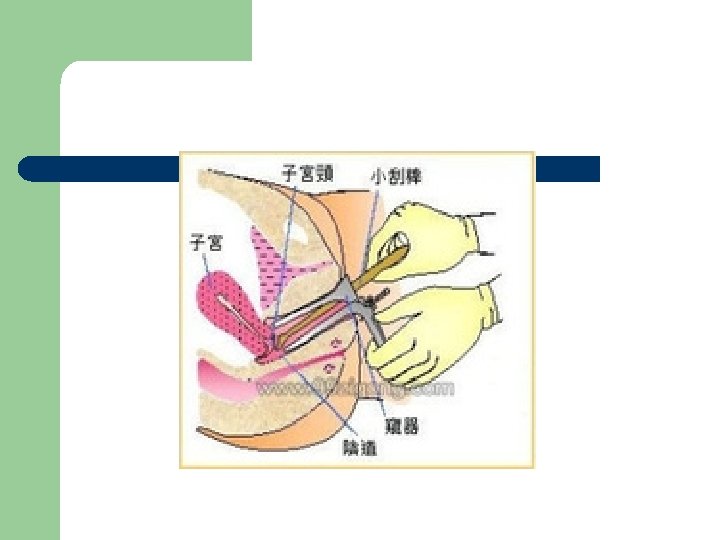
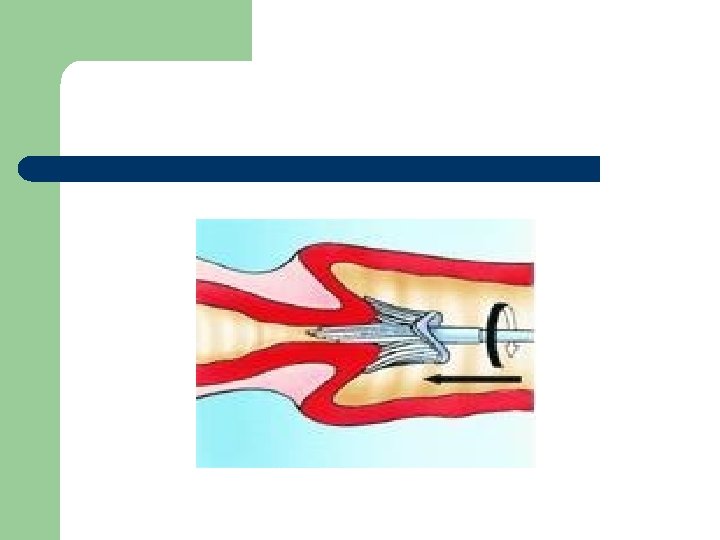
l l The appropriate sized speculum is selected. [3] The speculum is slowly inserted in its collapsed state at a forty-five degree angle to match the slope of the vagina. The blades are then expanded until the cervix comes into view. If the speculum is transparent, the vaginal walls can be seen. The cervix is then assessed. It should look moist, round, pink, and centered to the middle. The secretions of the cervix should be clear or whitish with no odor. The presence or absence of polyps, ulcers, and inflammation are noted. The appropriate sized speculum is selected. The speculum is slowly inserted in its collapsed state at a forty-five degree angle to match the slope of the vagina. The blades are then expanded until the cervix comes into view.
![l l The appropriate sized speculum is selected 3 The speculum is slowly inserted l l The appropriate sized speculum is selected. [3] The speculum is slowly inserted](https://slidetodoc.com/presentation_image_h2/031987f8dfb102116c2111ab42839cae/image-27.jpg)
l l The appropriate sized speculum is selected. [3] The speculum is slowly inserted in its collapsed state at a forty-five degree angle to match the slope of the vagina. The blades are then expanded until the cervix comes into view. If the speculum is transparent, the vaginal walls can be seen. The cervix is then assessed. It should look moist, round, pink, and centered to the middle. The secretions of the cervix should be clear or whitish with no odor. The presence or absence of polyps, ulcers, and inflammation are noted. The appropriate sized speculum is selected. The speculum is slowly inserted in its collapsed state at a forty-five degree angle to match the slope of the vagina. The blades are then expanded until the cervix comes into view.
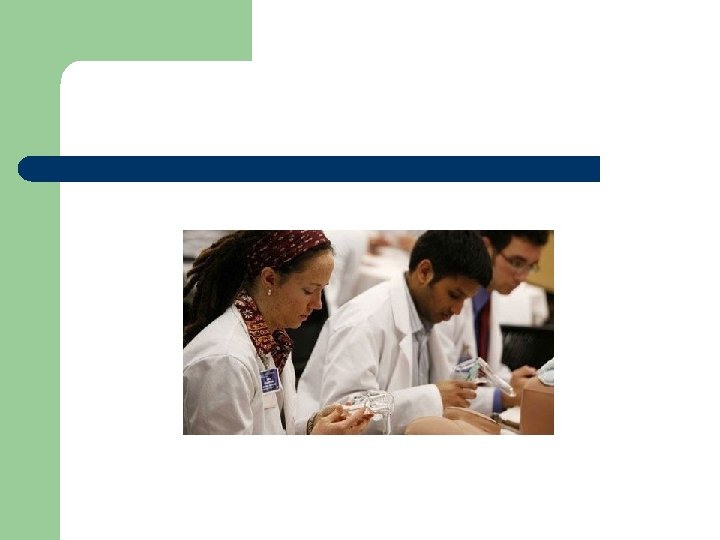
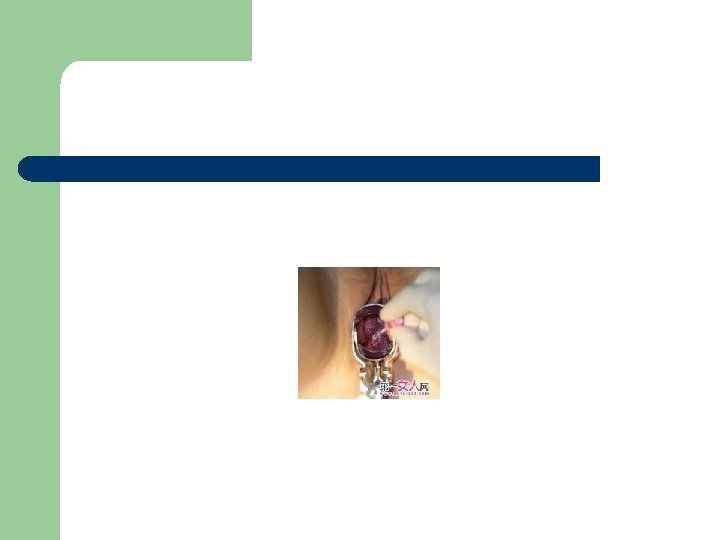
l A swab or cytobrush will be used to collect or scrape cervical cells off of the surface of the cervix to be evaluated for changes. Other vaginal swabs can be taken at this time to test for sexually transmitted diseases.
l A swab or cytobrush will be used to collect or scrape cervical cells off of the surface of the cervix to be evaluated for changes. Other vaginal swabs can be taken at this time to test for sexually transmitted diseases.
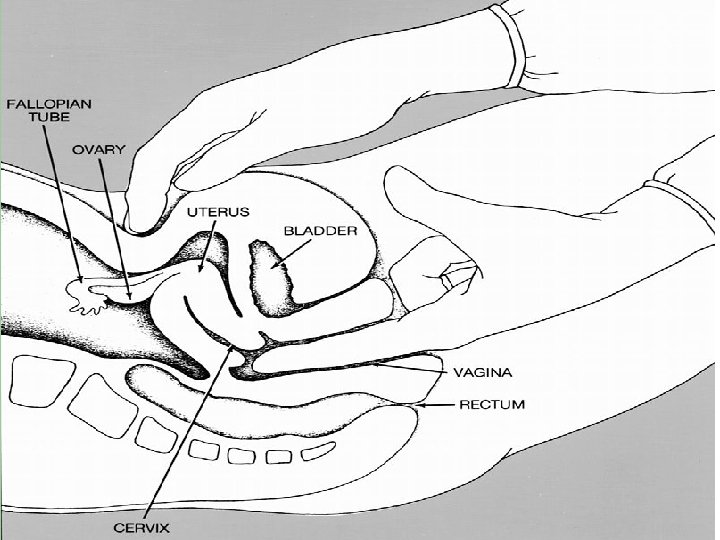
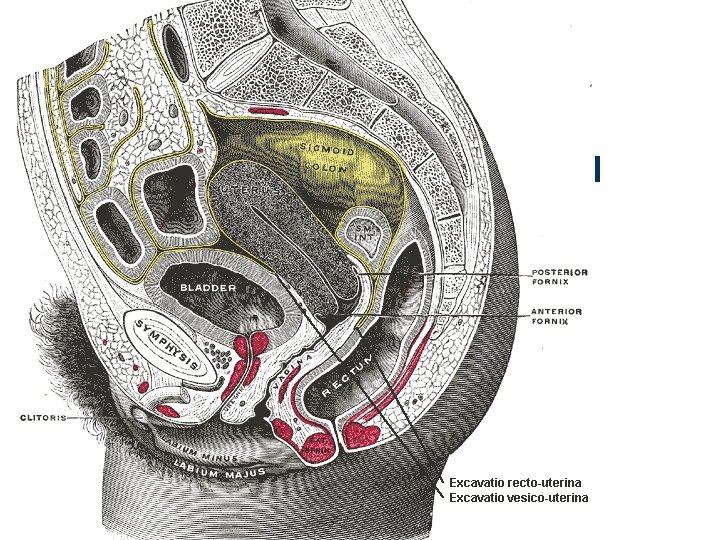
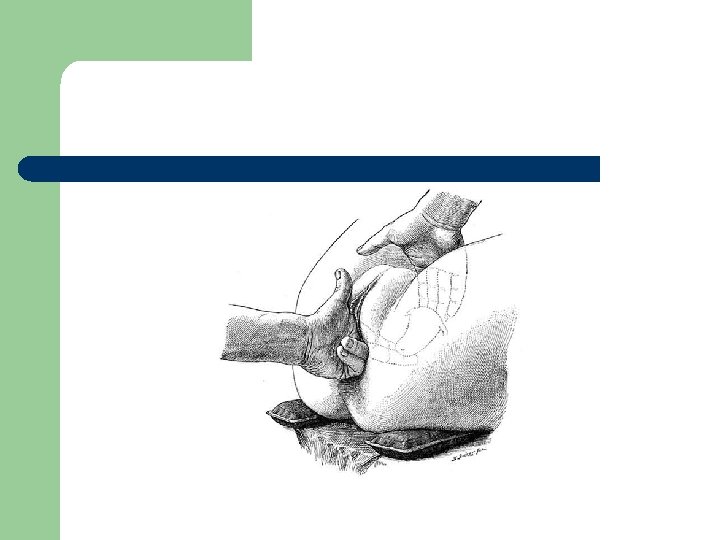
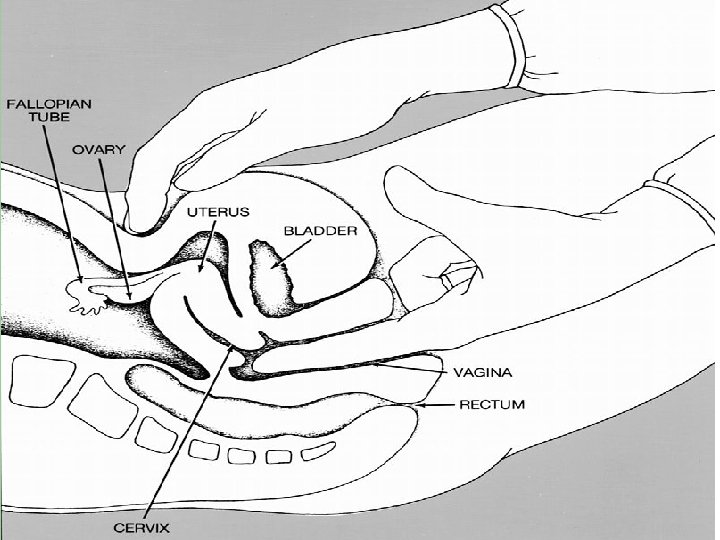
l l The next part of the pelvic exam is the Bimanual palpation and begins after the speculum is removed. The examiner informs and explains this part of the exam. Two fingers are used to palpate the cervix. [3] The cervix and fornices are assessed for mobility and the presence of lumps. [3] The uterus is palpated and evaluated to determine its position by leaving the fingers of one hand in the vagina while pressure to the abdomen is applied with the other hand. If the body tissue is too thick due to obesity, an ultrasound may be performed instead
l l The ovaries can be palpated through the abdomen. They should be mobile, about the size of an almond but can vary in texture. Sometimes the ovaries cannot be palpated. If the examiner can feel the fallopian tubes, this is not a normal finding. The examiner removes their hands and puts on clean gloves to assess the rectum, and explains this part of the exam to the woman. The rectum is assessed by having one finger in the vagina and the other in the rectum. The rectum should be smooth.
C u l d o c e n t e s i s a m e d i Culdocentesis


l T h e P a p a n i c o l a o u t e
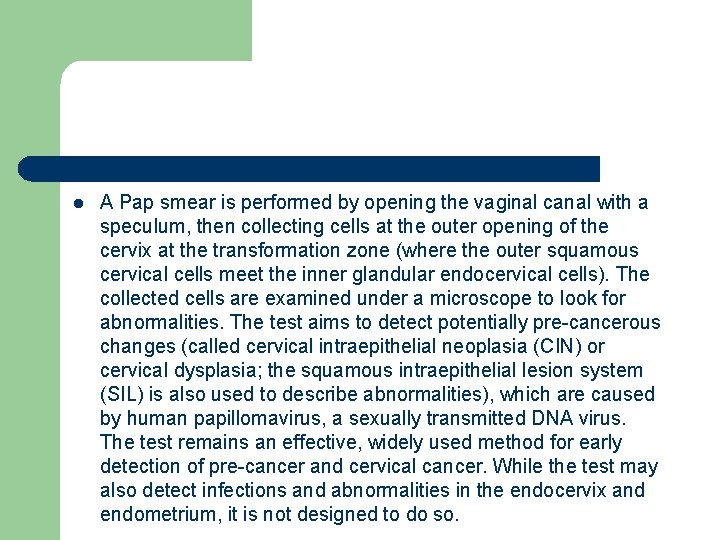
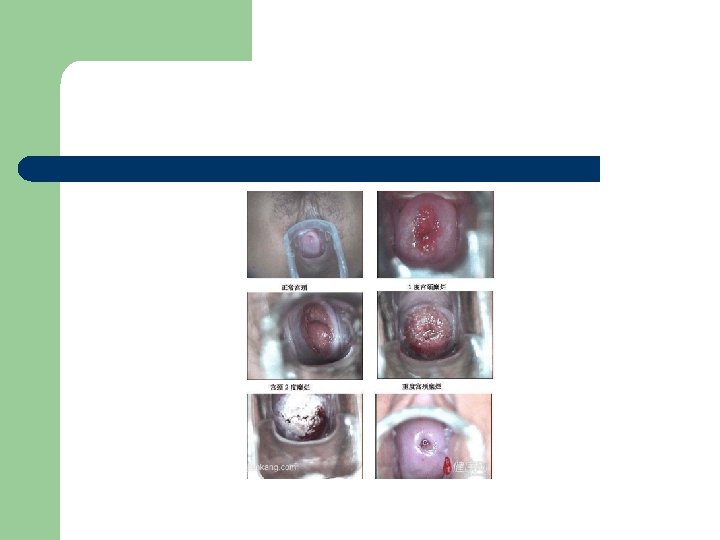
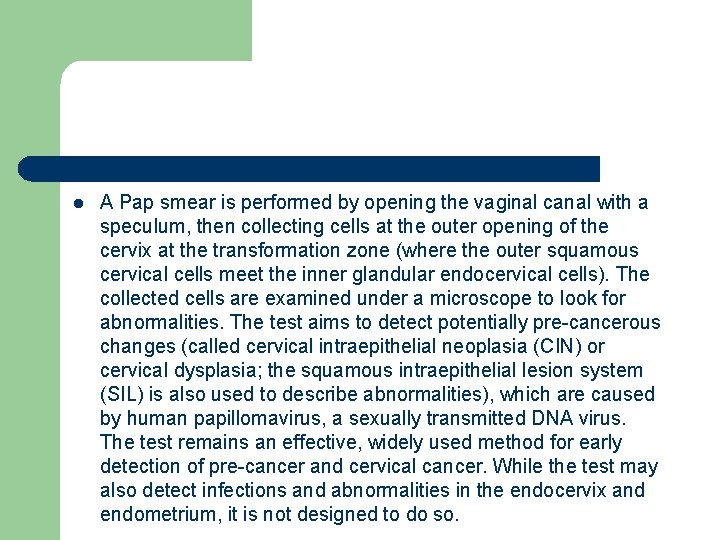
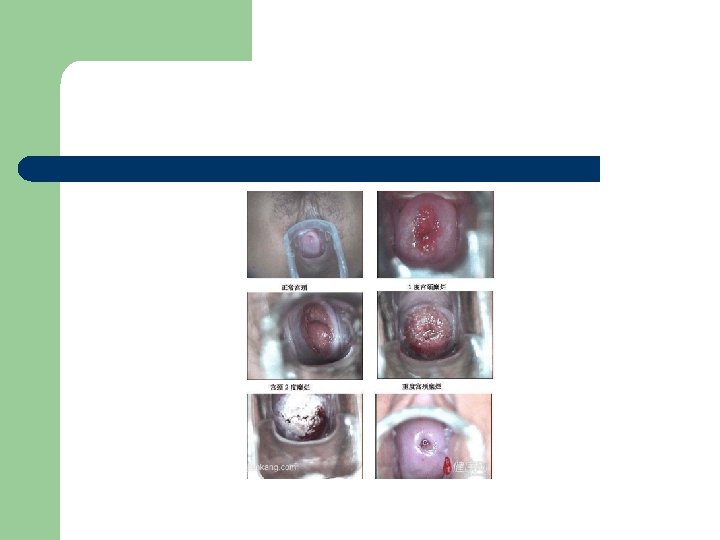
l A Pap smear is performed by opening the vaginal canal with a speculum, then collecting cells at the outer opening of the cervix at the transformation zone (where the outer squamous cervical cells meet the inner glandular endocervical cells). The collected cells are examined under a microscope to look for abnormalities. The test aims to detect potentially pre-cancerous changes (called cervical intraepithelial neoplasia (CIN) or cervical dysplasia; the squamous intraepithelial lesion system (SIL) is also used to describe abnormalities), which are caused by human papillomavirus, a sexually transmitted DNA virus. The test remains an effective, widely used method for early detection of pre-cancer and cervical cancer. While the test may also detect infections and abnormalities in the endocervix and endometrium, it is not designed to do so.
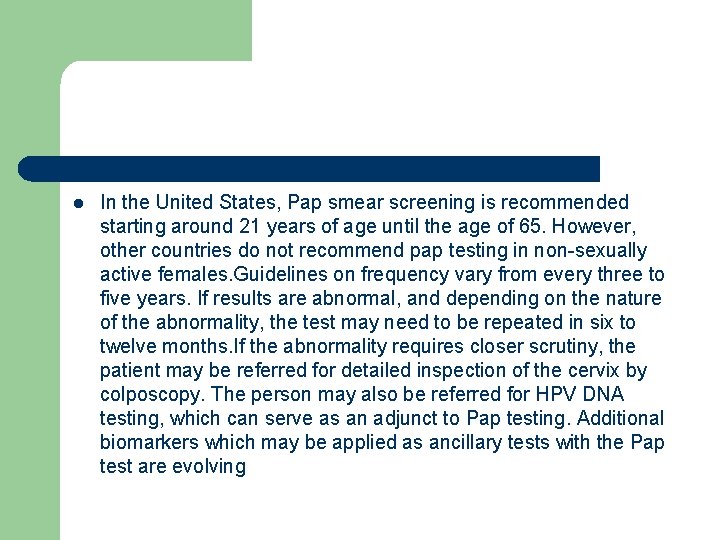
l In the United States, Pap smear screening is recommended starting around 21 years of age until the age of 65. However, other countries do not recommend pap testing in non-sexually active females. Guidelines on frequency vary from every three to five years. If results are abnormal, and depending on the nature of the abnormality, the test may need to be repeated in six to twelve months. If the abnormality requires closer scrutiny, the patient may be referred for detailed inspection of the cervix by colposcopy. The person may also be referred for HPV DNA testing, which can serve as an adjunct to Pap testing. Additional biomarkers which may be applied as ancillary tests with the Pap test are evolving
l l l Abnormal results are reported according to the Bethesda system. They include: Squamous cell abnormalities (SIL) Atypical squamous cells of undetermined significance (ASC-US) Atypical squamous cells – cannot exclude HSIL (ASC-H) Low-grade squamous intraepithelial lesion (LGSIL or LSIL) High-grade squamous intraepithelial lesion (HGSIL or HSIL) Squamous cell carcinoma
 Ninewells hospital area 6 outpatients
Ninewells hospital area 6 outpatients Post castration syndrome gynecology
Post castration syndrome gynecology Introduction of obstetrics
Introduction of obstetrics Neuroendocrine syndromes in gynecology
Neuroendocrine syndromes in gynecology Balan medical term
Balan medical term Foetotomy
Foetotomy Gynecology
Gynecology Clinical observation of motor and postural skills
Clinical observation of motor and postural skills Clinical skills definition
Clinical skills definition Dept nmr spectroscopy
Dept nmr spectroscopy Department of agriculture consumer services
Department of agriculture consumer services Finance departments
Finance departments Worcester electrical inspector
Worcester electrical inspector Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Mn dept of education
Mn dept of education Dept of finance and administration
Dept of finance and administration Dept. name of organization
Dept. name of organization Ohio employment first
Ohio employment first Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Vaginal dept
Vaginal dept Gome dept
Gome dept Gome dept
Gome dept Gome dept
Gome dept Gome dept
Gome dept Hoe dept
Hoe dept Lafd interview
Lafd interview Oviposition
Oviposition Dept of education
Dept of education Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Dept a
Dept a Central islip fire department
Central islip fire department Rowan county medicaid transportation
Rowan county medicaid transportation Dept of education
Dept of education Bromocicloesano
Bromocicloesano Pt dept logistik
Pt dept logistik Nys department of homeland security
Nys department of homeland security La dept of revenue
La dept of revenue Geaux biz login
Geaux biz login Oxford dept of continuing education
Oxford dept of continuing education Nebraska dept of agriculture
Nebraska dept of agriculture Ee dept iitb
Ee dept iitb Dept ind onegov
Dept ind onegov Albany county department of social services
Albany county department of social services Fda clinical investigator training course
Fda clinical investigator training course