GP Supervision Understand Minimise Your Risks GP Supervisors






- Slides: 49

GP Supervision: Understand & Minimise Your Risks GP Supervisors Australia
Webinar Housekeeping: Muting and Background Noise • We will mute your ability to speak with us until question time • We are recording this webinar to share with other supervisors • Your continued attendance will be taken as permission given
• Webinar Housekeeping: How to ask a question Chat function: type your question – Click on then click on Margo – Type your question in the text box – For comments, click • Dr. Baker will raise the question with the Presenter
About GPSA is the national representative body that unites GP Supervisors by promoting recognition for supervision work through open and accountable advocacy. “We are the voice of GP Supervision making the next generation of family doctors” “We are making GP Supervision rewarding, respected and recognised” “We are working to recruit and retain quality supervisors” - Advocate for Supervisors with relevant health sector policy makers, & Govt. - Work with and listen to, and support our members - Negotiate the National Terms and Conditions between Supervisors and Registrars on behalf of Supervisors

Moderator: Dr. Patricia Baker Chair of GPSA • GAICD MBBS FRACGP • Chair GP Supervisors Australia • Principal Keperra Family Practice, QLD • Board North Brisbane Medicare Local & QLD Faculty Board RACGP • Strong background in medical boards and organisations. • Interest in indigenous and preventative health as well as health education
Guest Presenter: Ms. Julie Brooke Cowden Claims Manager (Solicitor) MDA National • BSc & BLaws (LLB) Macquarie University; Master Laws (LLM) Sydney 2005. • Specialist Accreditation in Personal Injury (Defendant) Litigation, 2000 • Adjunct Lecturer with the University of Notre Dame Australia’s School of Medicine in Sydney • Member Concord Repatriation General Hospital’s Human Research Ethics Committee 10 years • Specialised work with Doctors on: • Complaints • Claims • Performance & disciplinary issues • Conduct and health matters • Medicare investigations & audits • Pharmaceutical Services investigations • Coronial investigations & inquests

Guest Observer: The Hon. Senator Fiona Nash • Elected to the Australian Senate in 2004, • Since 1 July 2005 for the Nationals, NSW • Assistant Minister for Health • Interests: education, health, food security to safe environmental practices • Deputy Leader of the Nationals in the Senate, with party experience as branch chairman, state executive, delegate to Federal Council, and National Party Whip in the Senate • Bachelor of Arts (Liberal Studies) Mitchell College, Bathurst
Outline • Definition, role and responsibilities of the GP Supervisor • General knowledge questions • Issues relating to GP Supervision • When things go wrong – case scenarios • Risk management measures • Checklist • Q & A
Definitions “A GP Supervisor is a General Practitioner who establishes and maintains an educational alliance that supports the clinical, educational and personal development of a Registrar” Wearne et al 2012
Definitions • In a general practice setting, a GP Supervisor may be supervising: – Medical students – Prevocational doctors doing general practice terms e. g. PGPPP – GP Registrars – IMGs working towards a Fellowship in General Practice who are not on a Registrar training program
What do Effective GP Supervisors Do? “… promote reflection and give feedback based on direct observation to facilitate clinical deliberate practice” “… attend to the Registrar’s wellbeing and make it safe for the registrar to reveal and address the weaknesses in his or her knowledge, skills and emotional responses to practice” Wearne et al 2012 p 1169
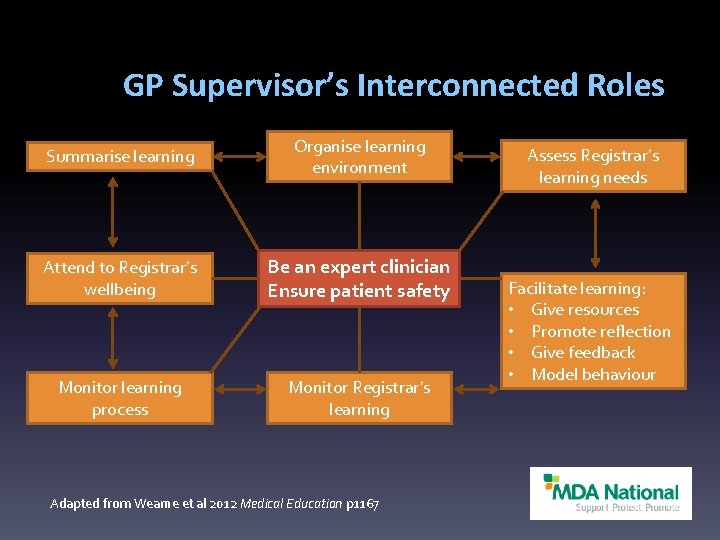
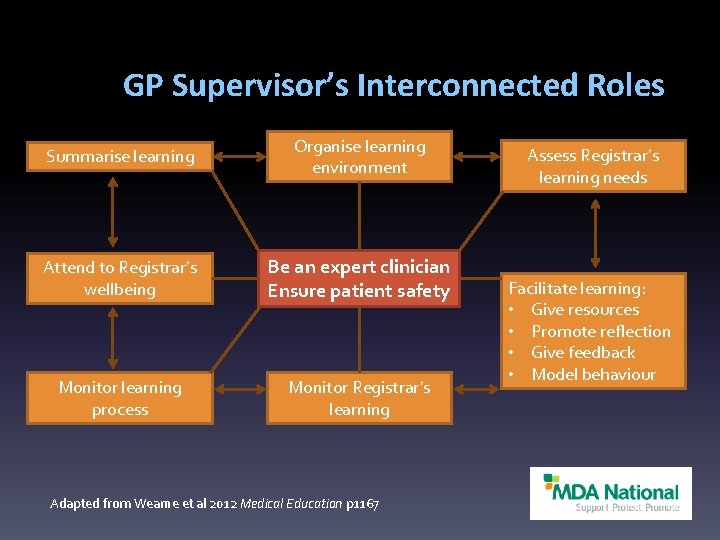
GP Supervisor’s Interconnected Roles Summarise learning Organise learning environment Attend to Registrar’s wellbeing Be an expert clinician Ensure patient safety Monitor learning process Monitor Registrar’s learning Adapted from Wearne et al 2012 Medical Education p 1167 Assess Registrar’s learning needs Facilitate learning: • Give resources • Promote reflection • Give feedback • Model behaviour
Responsibilities of the GP Supervisor • Discuss the supervised doctor’s role & responsibilities • Clarify the supervised doctor’s skill level & abilities • Establish triggers & guidelines – confirm when the supervised doctor must seek advice and/or assistance • Ensure that feedback is regularly provided & encourage ongoing dialogue • Develop strategies to minimise risk • Recognise and manage conflict & other problems early
Expectations of the Medical Board The Medical Board of Australia’s (MBA) Good medical practice- a code of conduct for doctors in Australia states that good medical practice, with regard to teaching and supervising, involves: – 10. 2. 1: Seeking to develop the skills, attitudes and practices of an effective teacher, whenever you are involved in teaching – 10. 2. 2: Making sure that any doctor or medical student for whose supervision you are responsible receives adequate oversight and feedback
Expectations of the Medical Board In relation to assessing colleagues, the MBA’s code of conduct notes that in order to achieve the highest standards of practice, doctors should: – 10. 3. 1: Be honest, objective and constructive when assessing the performance of colleagues, including students. Patients will be put at risk if you describe as competent someone who is not
Expectations of the Medical Board Finally, the MBA’s code of conduct provides guidance specifically with respect to medical students. It is suggested that supervising doctors: – 10. 4. 1 Treat students with respect and patience – 10. 4. 2 Make the scope of the student’s role in patient care clear to the student, to patients and to other members of the healthcare team – 10. 4. 3 Inform patients about the involvement of medical students, obtaining their consent for student participation, while respecting their right to choose not to consent
GP Supervision – General Knowledge Questions Quiz and discussion
1. Apart from appropriate professional indemnity insurance, are there any other insurance requirements for those working as GP Supervisors (on site or remotely)? A. Yes, notification in writing is required and extra premium payable B. Yes, notification in writing is required but no extra premium payable C. No D. Only if doing remote supervision Answer = C
2. Are supervised doctors (on Registrar policies) covered to perform a procedure their supervisor/s is not covered to perform? A. Yes B. No C. Only if the Registrar is directly supervised (observed) whenever the procedure is performed D. Only if the Registrar has previously obtained qualifications, skills and training in the procedure Answer = B

3. Are GP Supervisors legally liable for what their Registrars do? A. Yes B. No C. Only if the supervisor was aware of the situation and did not intervene appropriately D. Only if the supervisor was unaware of the situation but should have been aware, i. e. was providing an inadequate level of supervision Answer = A
4. Can GP Supervisors undertaking remote supervision (i. e. supervising a doctor who is not working in the same physical location as they are) also be held liable for the actions of the supervised doctor? A. Yes B. No Answer = A
5. Are patients seeing GP Registrars in your Practice informed that they are being treated by a supervised doctor or doctor undertaking further training? A. Always B. Mostly C. Only if it comes up or the patient asks D. Not generally E. I do not know
Possible issues arising from Supervision • Blind spots • Failing to make the supervised doctor aware of the circumstances in which they must or should contact their Supervisor • Not providing regular feedback or review, or being inaccessible to discuss the supervised doctor’s issues or concerns • Failing to promptly and/or transparently deal with errors when they occur
“Blind Spots” • “Blind spots” are an unawareness of incompetence which can result in help not being sought when it is needed, potentially placing patients at risk • This is more risky in somewhat isolated work environments like General Practice • It is important to remember that Supervisors can also have blind spots Byrnes 2012, Kamien 2004, Kruger & Dunning 1999, Wearne 2005, Wearne 2011
Criteria to Contact the GP Supervisor • Establishing criteria prompting supervised doctors to contact their Supervisors is an important strategy to reduce patient risk • Criteria can include: – Diagnostic, e. g. recognition of a seriously ill child – Therapeutics, e. g. particular procedural skills – Transfer of care – Management of sentinel or adverse events • It is helpful to have a general template or list which is provided and discussed at the beginning of the placement RACGP 2008
Case Scenario 1 - Competency Dr Sam (supervised Doctor), Lucy, and Dr Watts (GP Supervisor) • Lucy, a 16 y. o, comes in on Monday morning with a sore arm, which she injured at netball. She is tired and headachy, with an elevated temperature • Dr Sam observes several lesions on Lucy’s left arm, which look like hives. Lucy says they are itchy and sore, so Dr Sam prescribes an antihistamine, and asks her to return if she is worse, or not improving • Lucy returns on Thursday morning, as she is feeling feverish and unwell. On examination, Dr Sam notes that there is a band-like rash in her left arm, characteristic of shingles This case study is based on an actual event but details have been changed to protect the privacy of those involved
Case Scenario 1 - Competency • Dr Sam checks MIMS, noting that antiviral treatment should ideally be given within 48 hours, but can be administered up to 72 hours after the rash first appears • Dr Sam decides that antiviral therapy is not warranted, as he assumes that the rash has been present for more than 3 days. He recommends over the counter analgesia and that Lucy also apply topical lotions to the lesions • 6 weeks later, Lucy’s mother contacts the Practice claiming that Lucy was treated inappropriately, as she was not given antiviral medication. Lucy has ongoing severe pain, and has apparently developed post-herpetic neuralgia
Case Scenario 1 - Competency What should Dr Watts do? • Check the clinical notes • Speak with Dr Sam, to find out what happened, and ascertain the reasons as to why this incident occurred • Contact Lucy’s mother, to apologise, and listen to her concerns • Advise her insurer, and seek their guidance as to how to manage this issue. For example, Dr Watts may: – Arrange to meet with Lucy and her mother, to discuss their concerns in person – Prepare a response should a written complaint be received – Consider whetherapeutic relationship should continue, particularly if a claim for damages is made
Case Scenario 1 - Competency What if: - Dr Sam says to Dr Watts that: • The Practice is much busier than he had expected, and sometimes he feels completely overwhelmed • He has felt unable to approach her whenever he has any issues or concerns regarding patients, as it is clear she dislikes interruptions when she is consulting • When he has spoken with her, on a number of occasions she has dismissed his questions and told him to go and read Murtaugh instead Dr Watts decides she needs some advice from her insurer
Case Scenario 1 - Competency Advice from Dr Watts’ insurer may include: • Talk to Dr Sam about the level of supervision he feels is needed • If unable to reach agreement, discuss his supervision needs with the medical educator from his training provider • Randomly review 10 files of patients who have seen Dr Sam over the previous 2 months. – If significant concerns remain about the appropriateness of Dr Sam’s management, Dr Watts should consider changing their supervision requirements • Sending in copies of the clinical notes to the insurer, as a file will need to be opened
Case Scenario 2 - Mandatory Notification
Case Scenario 2 - Mandatory Notification Supervisor reporting Registrar • Dr Chu receives a phone call from a local Pharmacist, querying a script written by the Practice’s GP Registrar for methotrexate, 20 mg orally, once daily, for severe rheumatoid arthritis • The Pharmacist asks whether this should be once weekly, rather than daily • As the Registrar has already left for the day, Dr Chu checks the very brief patient notes, which state that this new patient has methotrexate 20 mg daily, and needs a new script • Dr Chu confirms with the Pharmacist that the correct dose is weekly This case study is based on an actual event but details have been changed to protect the privacy of those involved
Case Scenario 2 - Mandatory Notification • When Dr Chu asks the registrar the following day about the issue with dosing identified by the Pharmacist, the Registrar maintains that the 20 mg daily dose she prescribed was correct • Although the Registrar concedes that she did not check MIMs, she is not concerned when Dr Chu points out that oral Methotrexate should be prescribed weekly, not daily • The Registrar is dismissive of Dr Chu’s concerns, and says she cannot see any problems with her management • Dr Chu has significant concerns about the Registrar’s insight and clinical competence, particularly as a similar, but less serious issue has arisen in the last month • What is Dr Chu required to do ?
Case Scenario 2 - Mandatory Notification Under Section 140 of the National Law, registered health practitioners are required to report ‘notifiable conduct’ to AHPRA Notifiable conduct is defined as occurring in circumstances where the practitioner has: - a) Practised whilst intoxicated by alcohol or drugs; or b) Engaged in sexual misconduct in connection with their clinical practice; or c) Placed the public at risk of substantial harm during their practise of medicine, because of an impairment; or d) Placed the public at risk of harm because they have practised in a way that constitutes a significant departure from accepted professional standards
Case Scenario 2 - Mandatory Notification • It is Dr Chu’s belief that the Registrar’s conduct placed this particular patient at significant risk of harm • Further, given the registrar’s lack of insight, Dr Chu was concerned that other patients may also be at risk • Dr Chu phoned his insurer, who agreed that there was a reasonable basis for him to have formed the belief that the registrar’s conduct fell within the definition of ‘notifiable conduct, ’ under s 140 of the National Law • Accordingly, Dr Chu contacted AHPRA, and reported the Registrar’s conduct
Case Scenario 3– Unprofessional Conduct Breach of patient privacy and confidentiality
Case Scenario 3 –Unprofessional Conduct Breach of patient privacy and confidentiality • Dr Placid is an IMG, who has very little experience in the General Practice setting. He has come to Dr Smith’s small rural practice, to complete his first term. • Although he requires significant supervision, Dr Placid is very keen to learn and wants to make a good impression. • After a couple of months, Dr Placid’s clinical skills have significantly improved, and he appears to have embraced life in the rural community.
Case Scenario 3– Unprofessional Conduct Breach of patient privacy and confidentiality • The annual B & S ball rolls around, and Dr Placid informs Dr Smith that he will be attending. Dr Smith reminds him that he needs to be careful about how he behaves, as most of the attendees will be patients of the practice • Although Dr Placid is feeling a little sore and sorry the day after, he appears otherwise unaffected by the events of the previous night • However, after lunch, the Practice Manager comes into Dr Smith’s office and says that Muriel is on the phone, and she wants to complain about Dr Placid’s behaviour at the B & S ball
Case Scenario 3– Unprofessional Conduct Breach of patient privacy and confidentiality • Dr Smith picks up the phone, with some trepidation. Muriel is very angry, and says that Dr Placid disclosed to her grandson and his friends at the B&S ball that she had asked for a referral to a Plastic Surgeon, to have breast implants and a lift • Muriel claims Dr Placid was drunk at the time. She is distressed about facing her family, and the likely reaction she will receive from her friends at bingo. She wants Dr Placid to be struck off and dismissed from the practice • What should Dr Smith do?
Case Scenario 3– Unprofessional Conduct Breach of patient privacy and confidentiality • Dr Smith asks Muriel to come in and have a chat with him, so he can apologise in person • He then calls Dr Placid into his office, and asks him to explain what happened. Dr Placid confirms that he disclosed confidential information about his recent consultation with Muriel when he was feeling tipsy. He is mortified and extremely apologetic about his behaviour • After some discussion, they agree that Dr Placid will notify his insurer, and seek their advice about the wording of an appropriate letter of apology to Muriel. • Dr Smith then has a long chat with Muriel, who reluctantly accepts Dr Placid’s apology.
Case Scenario 3– Unprofessional Conduct Breach of patient privacy and confidentiality
Risk Management Tips for GP Supervisors • Clarify the supervised doctor’s roles and responsibilities • Encourage a positive feedback environment, focussing on improving learning and patient safety • Be aware of the supervised doctor’s and your own “blind spots” understandings. • Offer timely feedback which not only covers strengths and weaknesses, but is corrective • Reflect and discuss learning gaps, and reinforce
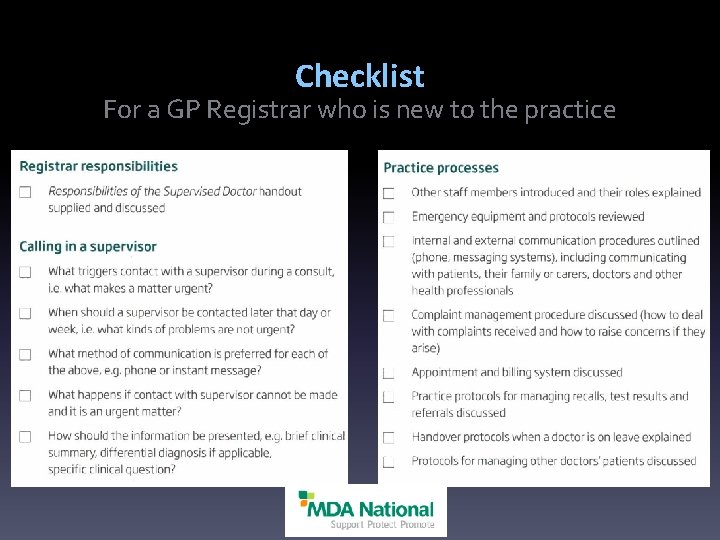
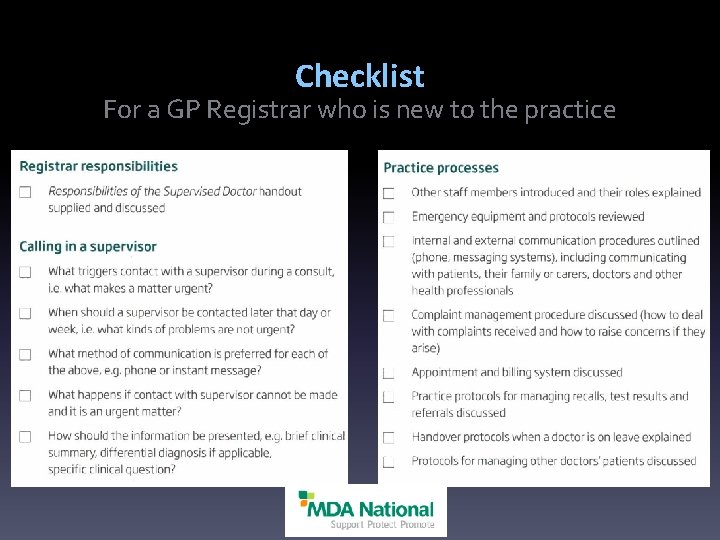
Checklist For a GP Registrar who is new to the practice
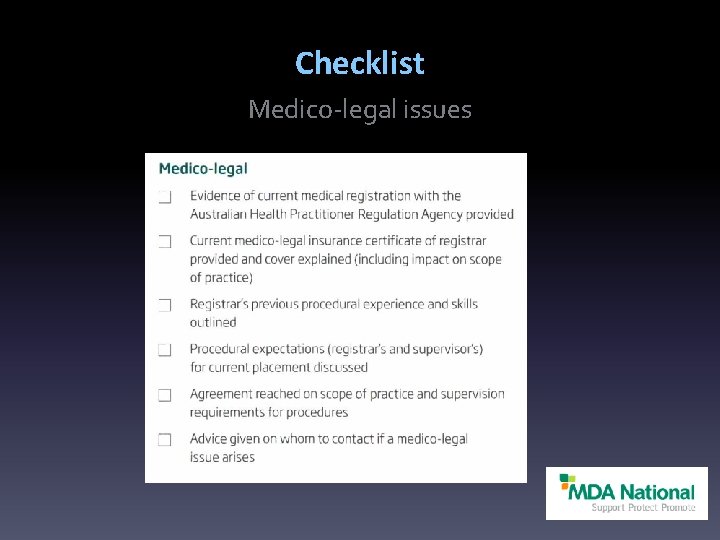
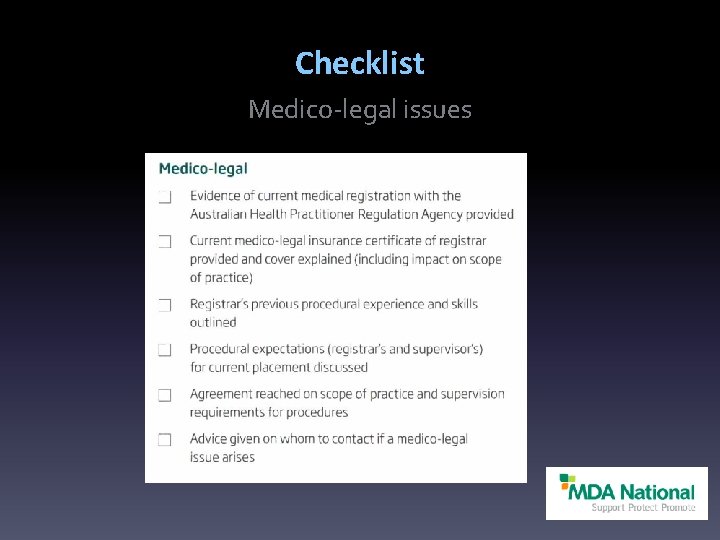
Checklist Medico-legal issues
References Australian Medical Association. Supervision and Assessment of Hospital Based Postgraduate Medical Trainees 2012 Byrnes P. Are they safe in there? Aust Fam Physician. 2012; 41: 26– 9 Kamien J. Educating the good GP. Aust Fam Physician. 2004; 33: 1027– 9 Kennedy E & Heard S. Making mistakes in practice: developing a consensus statement. Aust Fam Physician. 2001; 30: 295– 9 Kruger J & Dunning D. Unskilled and unaware of it. J Pers Soc Psychol. 1999; 77: 1121– 34 The RACGP. Companion Standards for General Practice Education and Training: Trainers and Training Posts 2005 (Version 2) 2008 Wearne S. General Practice supervision at a distance – is it remotely possible? Aust Fam Physician. 2005; 34: 31– 3 Wearne S. In-practice and distance consultant on-call General Practitioner supervisors for Australian General Practice? Med J Aust. 2011; 195: 224– 8 Wearne S, Dornan T et al. General Practitioners as supervisors in postgraduate clinical education: an integrative review. Medical Ed. 2012; 46: 1161– 73

Questions?

Don’t forget to join MDA National Insurance
GPSA is Here to Help • Contact us with your concerns – CEO Margo Field: ceo@gpsupervisorsaustralia. org. au • 0407 700 353 – Chair Dr. Patricia Baker: chair@gpsupervisorsaustralia. org. au • 0414 869 674 – www. gpsupervisorsaustralia. org. au (awesome website!) • Refer any Supervisors you know • Next webinar: Infrastructure Training Grant Applications • Newsletters coming up • Best Practice Guides
Thank you and Good night! • Thank you to our sponsor MDA National Insurance • Thank you to the Hon. Senator Fiona Nash, Assistant Minister for Health and her friendly staff. • Thank you for participating